Introduction
Distinct surgical approaches for managing the same
disease have several advantages and disadvantages when compared to
each other. These factors may be related to the technical features
and/or surgical team's comfort in performing the technique; yet, in
any comparison, patient outcome measures are the highest priority.
Any approach used in surgical oncology may become very popular for
a limited period unless it has not been proven safe, feasible, and
good for short, mid, and long-term patient outcomes. Single-port
laparoscopic surgery (SPLS) is currently a popular option in
gynecologic surgery. SPLS is a form of advanced, minimally invasive
laparoscopic surgery that uses a specialized technique where one
small incision provides laparoscopic access for optics and
instruments. Recently, some reports have demonstrated the
feasibility and safety of SPLS and the improvements in outcome over
conventional laparoscopy in terms of pain, recovery time, cosmesis,
and duration of hospital stay (1-6).
However, SPLS is not widely available due to the technical
difficulty of the procedure. It can be thought that inserting
several instruments through the same incision impedes the proper
working of the devices. The surgeon and the assistant must maneuver
in a very small space outside the abdomen, which can result in hand
collisions (7). On the other hand,
in single-port surgery, no other port exists for scope placement
and the ability to move the scope is significantly limited by other
instruments (8). Therefore, the
objective of this study was to overcome these technical challenges.
Inserting a small diameter port (3 mm) associated with a trocar in
the left medial part of the iliac crest could make this approach
more comfortable geometrically. To our knowledge, this is the first
report regarding this new technique.
Materials and methods
This retrospective study included 25 patients who
underwent laparoscopic cystectomy at our institution between March
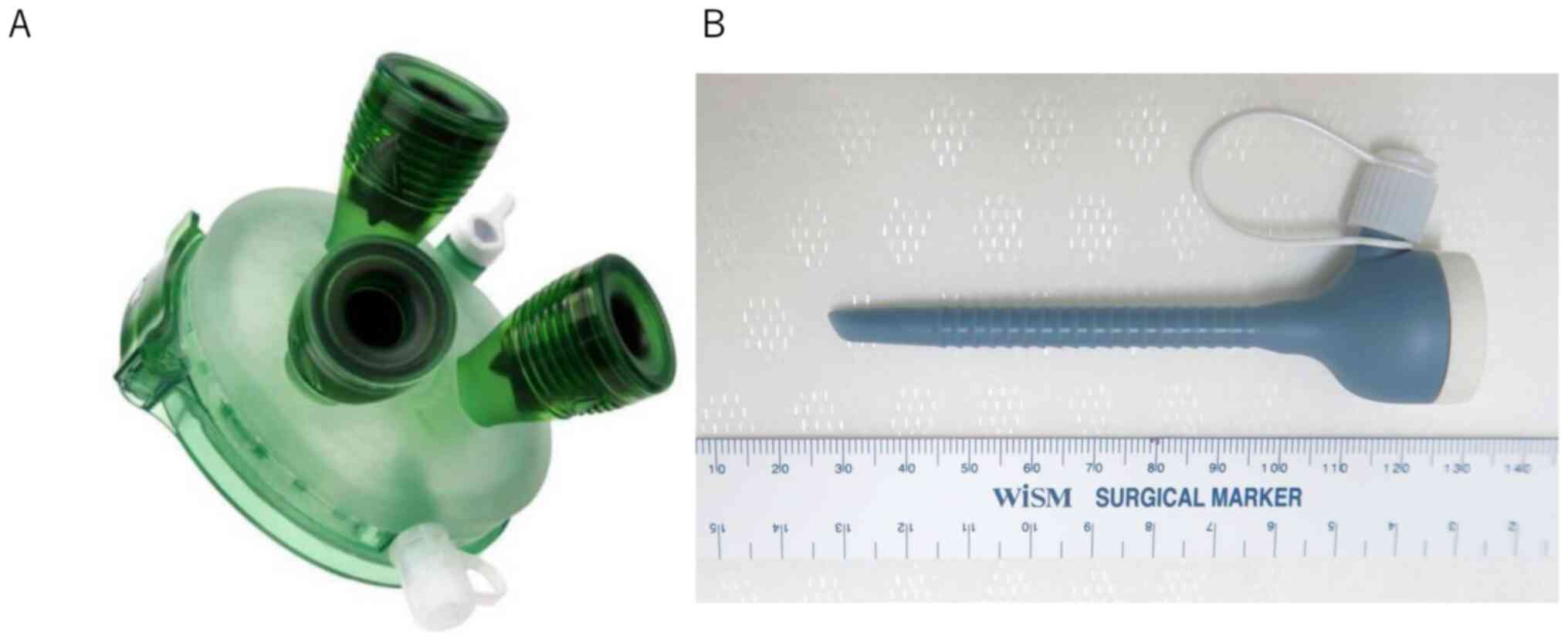
2015 and February 2020. Single-port procedures were performed with
devices manufactured specifically for single-port procedures used
in gynecologic surgery (GelPOINT® Mini Medical Leaders)
(Fig. 1). Written informed consent
for this operation was obtained from all patients or their
parents/guardians (for patients <18 years old). This work was
approved by the Institutional Review Board, Shimane University (IRB
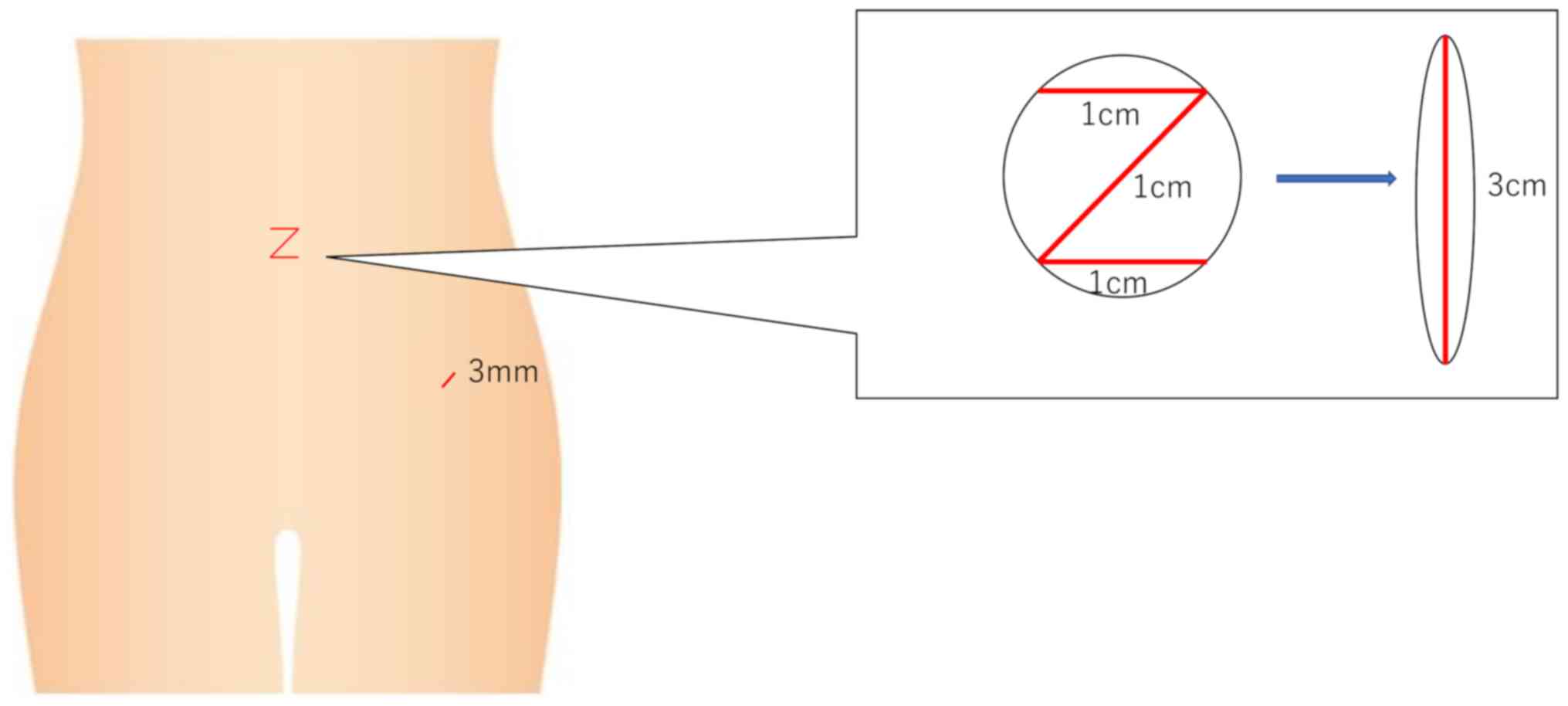
no. 201912120-1). After making a 3-cm Z-shaped intra-umbilical skin
incision (Fig. 2), the gel port is
inserted into the peritoneal cavity through the umbilicus
associated with 2 trocars. In order to facilitate movement of
surgeon's hands without collisions, a small incision (3 mm) is
performed in the left medial part of the iliac crest and a
bladeless trocar (Versa One®) is inserted into this
incision (Fig. 2). The main outcome
measures chosen for the current analysis were total operation time,
estimated blood loss during surgery, and changes in hemoglobin
level. Data collected from the hospital database included age, body
mass index, previous surgeries, preoperative symptoms, operation
time, blood loss, and length of hospital stay.
Results and Discussion
A total of 25 patients who underwent laparoscopic
ovarian cystectomy using our new technique were included in this
study. The mean patient was 27.8 (range, 15-39) years. The mean
total surgery time was 67.2 (range, 50-1,030) min. The mean blood
loss was 10.1 (range, 0-100) ml. The mean postoperative hospital
stay was 4.2 (range, 3-8) days (Table
I). No intraoperative or postoperative complications occurred
in any of the patients.
 | Table IPatient demographics (n=25). |
Table I
Patient demographics (n=25).
| Variable | Value |
|---|
| Age, years | |
|
Mean | 27.8 |
|
Range | 15-39 |
| Surgery time,
min | |
|
Mean | 67.2 |
|
Range | 50-103 |
| Bleeding volume,
ml | |
|
Mean | 10.1 |
|
Range | 0-100 |
| Postoperative
hospital stay, days | |
|
Mean | 4.2 |
|
Range | 3-8 |
The percent of cases of benign disease being managed
with SPLS has increased dramatically in recent years (1-6).
It has been reported that SPLS has several advantages compared to
conventional laparoscopy in the gynecologic field, such as less
post-operative pain, less recovery time, better cosmesis, and less
hospital stay (1-6).
SPLS is also useful for specimen removal because of the large
umbilical port site (2,3). However, SPLS has a major systemic
limitation: It involves crowding of all the working instruments
within one incision. As a result of this, visualization may be
obscured and hand collisions may occur between the surgeon and
assistant during the procedure. These technical problems cause
lower surgical accuracy and longer operation time compared to
conventional laparoscopy. Another limitation is that SPLS is a
difficult procedure, at least initially; it becomes easier with
increasing experience of the surgeon and development of instruments
(8). When related to inadequate
training and experience, these challenges may increase the risk of
intraoperative injury. To overcome the technical difficulties of
SPLS, newly developed approaches have been introduced in our
hospital since 2015. A small incision (3 mm) is performed in the
left medial part of the iliac crest and a bladeless trocar (Versa
One®) is inserted into this incision (Fig. 2). A 3-mm bipolar forceps are
included in this trocar. This ensures adequate distance between the
incisions of umbilicus as well as abdominal wall, facilitating easy
movement of the surgeon's hands without collisions. As a result,
even younger and/or less experienced doctors can perform this
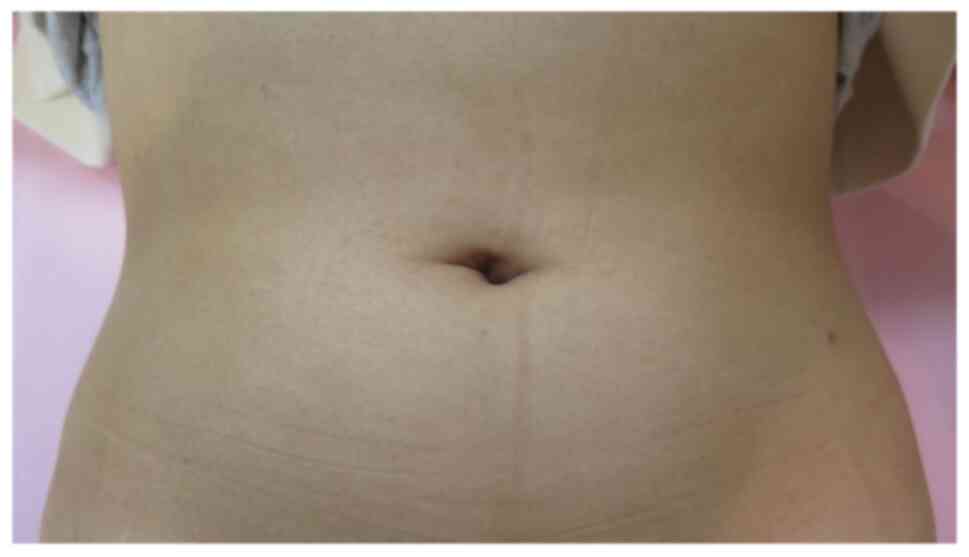
procedure safely and easily. On the other hand, due to the addition
of a small diameter port, there is practically no scar at the wound
site, making SPLS cosmetically a superior option (Fig. 3).
There are some limitations to our study. First, a
small number of patients were included in our study, making it
difficult to draw a clear-cut conclusion about the findings.
Therefore, further investigation with a larger study population is
required. Moreover, the surgical outcomes of procedures performed
by only one surgeon were analyzed. Therefore, it may be difficult
to extrapolate our findings. Consequently, further randomized
controlled trials are necessary.
In conclusion, by using Z shape intra-umbilical skin
incision and including an additional small diameter port,
interference of forceps as well as hand collision among surgeons is
prevented. We hope that as the chief technical difficulties in this
procedure have been overcome, SPLS will be an increasingly
widespread minimally invasive procedure in the gynecologic
field.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KN and SR drafted the manuscript. KN and SR confirm
the authenticity of all the raw data. TI, MI, SS, HY, KS, YY, SR,
SKu and HS performed the operation and statistical analysis. KN
participated in the design of the study. SKy conceived the study,
participated in its design and coordination, and helped in drafting
the manuscript. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from all
patients or their parents/guardians (for patients <18 years
old). The present study was approved by the Institutional Review
Board of Shimane University (approval no. 201912120-1).
Patient consent for publication
Consent was obtained from a patient for the
publication of corresponding images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Jung YW, Kim SW and Kim YT: Recent
advances of robotic surgery and single-port laparoscopy in
gynecologic oncology. J Gynecol Oncol. 20:137–144. 2009.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Jung YW, Choi YM, Chung CK, Yim GW, Lee M,
Lee SH, Paek JH, Nam EJ, Kim YT and Kim SW: Single port
transumbilical laparoscopic surgery for adnexal lesions: A single
center experience in Korea. Eur J Obstet Gynecol Reprod Biol.
155:221–224. 2011.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yim GW, Jung YW, Paek J, Lee SH, Kwon HY,
Nam EJ, Kim S, Kim JH, Kim YT and Kim SW: Transumbilical
single-port access versus conventional total laparoscopic
hysterectomy: Surgical outcomes. Am J Obstet Gynecol. 203:26.e1–e6.
2010.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Escobar PF, Bedaiwy MA, Fader AN and
Falcone T: Laparoendoscopic single-site (LESS) surgery in patients
with benign adnexal disease. Fertil Steril. 93:2074.e7–e10.
2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fader AN and Escobar PF: Laparoendoscopic
single-site surgery (LESS) in gynecologic oncology: Technique and
initial report. Gynecol Oncol. 114:157–161. 2009.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lee YY, Kim TJ, Kim CJ, Kang H, Choi CH,
Lee JW, Kim BG, Lee JH and Bae DS: Single-port access
laparoscopic-assisted vaginal hysterectomy: A novel method with a
wound retractor and a glove. J Minim Invasive Gynecol. 16:450–453.
2009.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Paek J and Kim SW: Single-port access
laparoscopic surgery in gynecology: Technical tips, advanced
gynecologic endoscopy. Darwish A (ed). In Tech, 2011. Available
from: http://www.intechopen.com/books/advanced-gynecologic-endoscopy/single-port-access-laparoscopic-surgery-in-gynecology-technical-tips.
|
|
8
|
Lee M, Kim SW, Nam EJ, Yim GW, Kim S and
Kim YT: Single-port laparoscopic surgery is applicable to most
gynecologic surgery: A single surgeon's experience. Surg Endosc.
26:1318–1324. 2012.PubMed/NCBI View Article : Google Scholar
|