Introduction
In-transit metastasis (ITM) is a cutaneous or
subcutaneous metastasis that develops between the primary lesion
and regional lymph nodes, and is seen in approximately 4-10% of
patients with malignant melanoma (MM) (1). ITMs are associated with poor
prognosis. ITM negatively impacts patients' quality of life, and
its treatment is essentially palliative (2). When patients develop multiple ITMs,
especially after lymph node dissection, it is difficult to control
the exudate and bleeding from ITMs. Newly-developed therapies
[i.e., BRAF/MEK inhibitors and immune checkpoint inhibitors (ICIs)]
have improved the prognosis of many patients with MM (3-5).
However, a substantial population of patients do not respond to
even these medications. In Japan, local injection of interferon-β
(IFN-β) has been used for years as adjuvant therapy licensed for
MM. Nevertheless, the evidence of IFN-β effectiveness for ITM
remains low, and the use of IFN has decreased following launches of
ICIs and molecular-targeted agents. Herein, we report a case of MM
with multiple ITMs that did not respond to a PD-1 inhibitor, but
went into remission upon local injection of IFN-β.
Case report
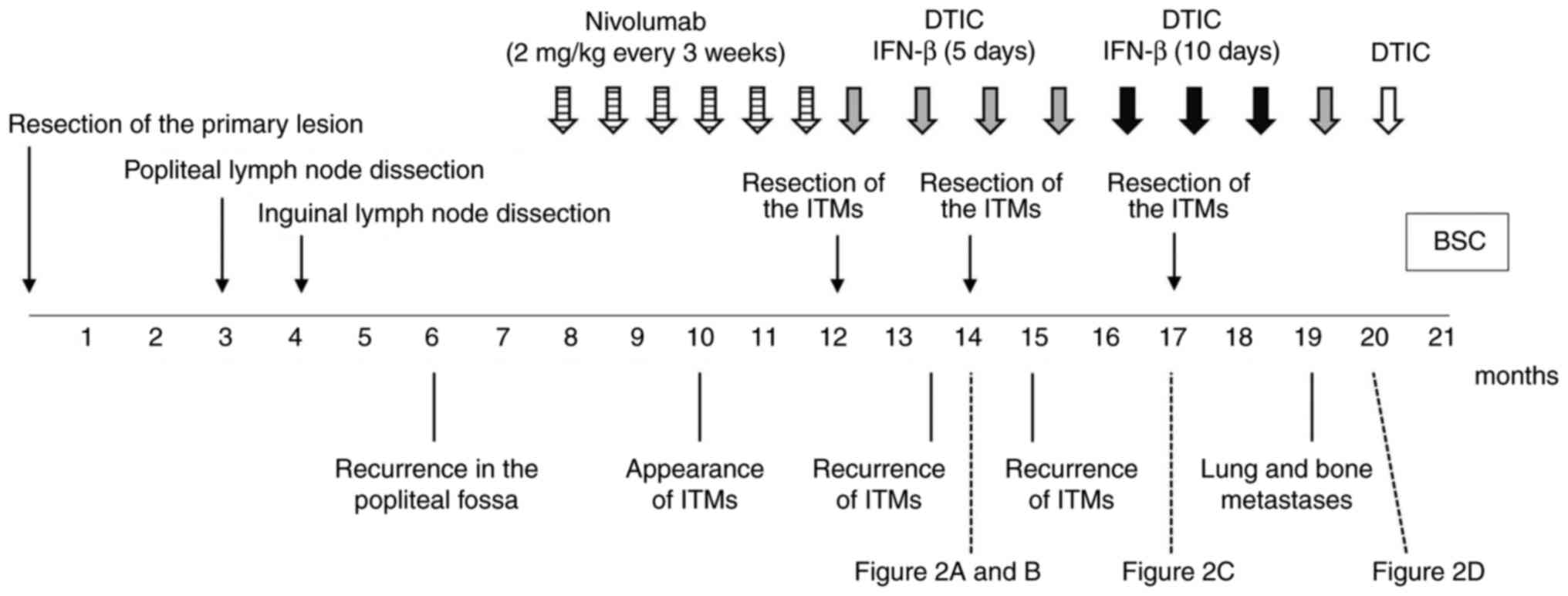
An 81-year-old man presented with acral lentiginous
melanoma on his right sole. The clinical course of the patient is
shown in Fig. 1. The primary lesion
was resected, but the tumour spread to the popliteal and inguinal
lymph nodes without any distant metastasis. No BRAF mutation was
detected in the tumour, and PD-L1 expression was not examined. He
received 2 mg/kg nivolumab every 3 weeks for the recurrence
following popliteal and inguinal lymph node dissections. However,
ITMs appeared and increased. Moreover, colitis as an immune-related
adverse event associated with nivolumab was observed. The treatment
was switched to dacarbazine (DTIC) (100 mg/day for 5 days every 4
weeks) and local injections of IFN-β (3 million IU/day for 5 days
every 4 weeks) after the treatment with nivolumab for 4 months. The
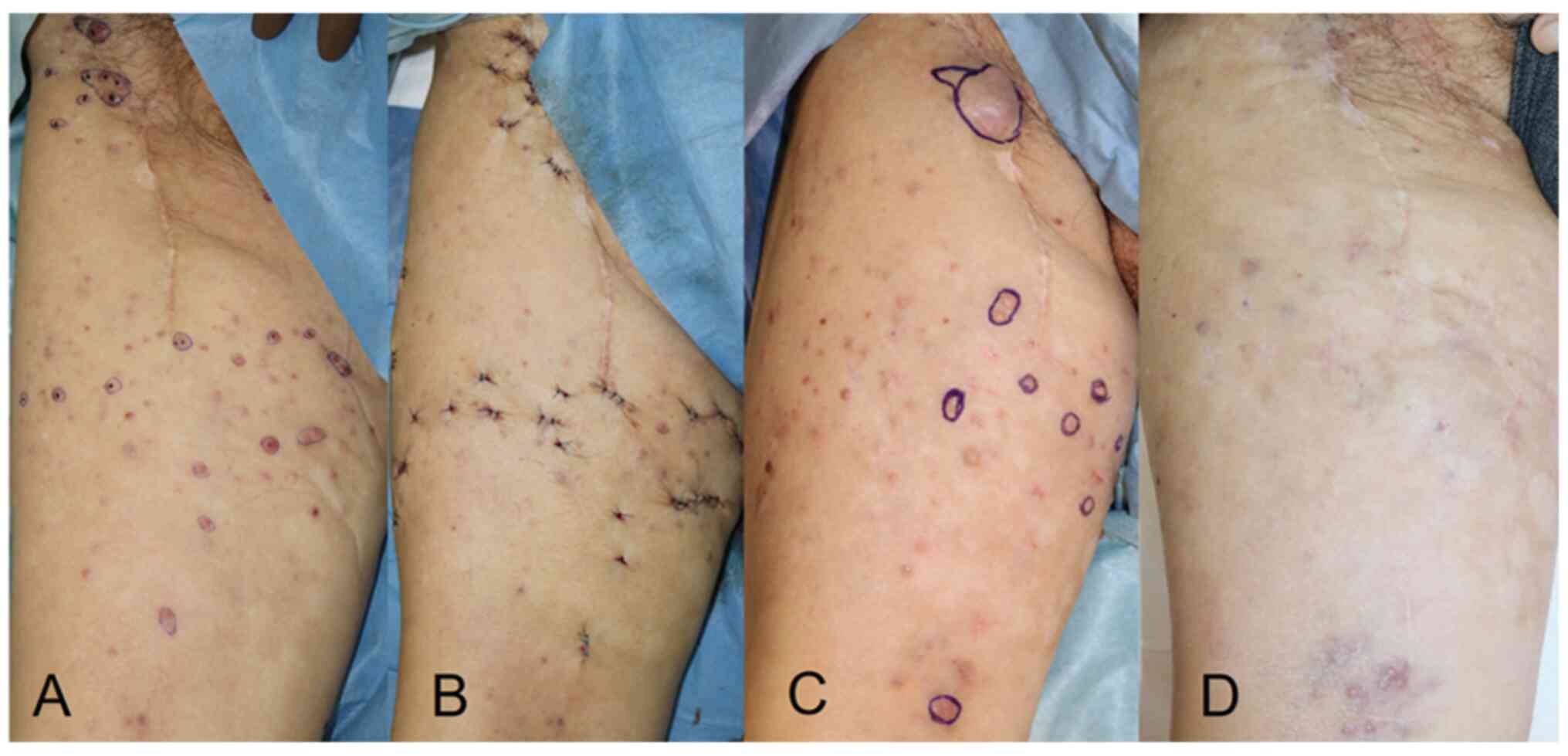
ITMs were resected twice (Fig. 2A
and B) during the treatment, but
recurred within a month. Because no distant metastasis was
detected, local control of tumours was important to improve the
patient's quality of life. Other ICIs were not considered advisable
due to the side effects developed with nivolumab. In contrast, no
serious adverse events were observed with local injections of
IFN-β. The local injections of IFN-β were increased from 5 to 10
consecutive days and administered every 4 weeks, followed by a
third resection of ITMs (Fig. 2C).
Thereafter, ITMs were markedly suppressed and no longer needed to
be resected (Fig. 2D). However,
lung and bone metastases appeared 4 months after the increase in
IFN-β, and then the treatment was switched to the best supportive
care.
Discussion
It has been reported that IFN-α contributed to
recurrence-free survival in patients with MM (6). A case of MM with ITMs treated with
intravenous IFN-β has also been reported (7). However, there is little evidence for
the efficacy of local IFN injection for ITMs. An in-vitro study
revealed that human IFN-β inhibited proliferation of melanoma cells
and induced apoptosis in a dose-dependent fashion (8). In our patient, increasing the amount
of IFN-β led to good control of ITMs without visible skin
impairment, bleeding, or exudation, suggesting a remarkable
anti-tumour effect of the increase in dose of IFN-β.
ICIs potently reinvigorate the usual anti-tumour
response that the immune system is capable of, but tumour cells
have managed to evade. However, the overall response rate of ICIs
to ITMs for itself was reported to be 54% in Australia (9), and presumably even lower in Japanese
melanoma which is less commonly accompanied by chromic sun-induced
damage. IFN has multiple immunomodulatory effect, such as
increasing tumour-infiltrating cells, downregulating T-regulatory
cells, modulating the STAT1/3 balance in tumour cells and host
lymphocytes, direct inhibition of cell proliferation, induction of
apoptosis of tumour cells, and inhibition of tumour angiogenesis
(8,10). The synergistic effect of PD-1
inhibitor and IFN-β has been reported in a small size study of
advance melanoma (11). The effect
of IFN-β and PD-1 inhibitor on ITMs in our case appears to be
additive rather than synergistic, because it was observed only
after the increase in dose of IFN-β.
Nevertheless, local IFN-β therapy could be an option
for improving quality of life of patients with ITMs refractory to
ICIs. Moreover, when the ITMs are also refractory to IFN-β,
increasing the dose of IFN-β may lead to better control of the skin
lesions.
Acknowledgements
The authors would like to thank Dr Faiz Kermani
(World Medical Fund, Alsace, France) for his language editing,
writing assistance and support.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YTa, ST, TK and MH made contributions to the
conception and design of the work, and YTa, TK and MH were major
contributors in writing the manuscript. YTe, DM and AT evaluated
the patient data and the therapeutic effects of IFN-β. ST, AT and
MH revised the manuscript. AT and MH supervised treatment of the
patient and confirmed the authenticity of all the raw data. All
authors read and approved the final manuscript.
Ethics approval and consent to
participate
This is a case report retrospectively reviewed and
analyzed without any new interventions. The report does not include
information which may identify the patients, and did not require
ethical committee approval.
Patient consent for publication
Written informed consent was obtained from the
patient's next of kin for publication of this case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Pawlik TM, Ross MI, Thompson JF, Eggermont
AM and Gershenwald JE: The risk of in-transit melanoma metastasis
depends on tumor biology and not the surgical approach to regional
lymph nodes. J Clin Oncol. 23:4588–4590. 2005.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hayes AJ, Clark MA, Harries M and Thomas
JM: Management of in-transit metastases from cutaneous malignant
melanoma. Br J Surg. 91:673–682. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
3
|
Long GV, Hauschild A, Santinami M,
Atkinson V, Mandalà M, Chiarion-Sileni V, Larkin J, Nyakas M,
Dutriaux C, Haydon A, et al: Adjuvant dabrafenib plus trametinib in
stage III BRAF-mutated melanoma. N Engl J Med. 377:1813–1823.
2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Weber J, Mandala M, Del Vecchio M, Gogas
HJ, Arance AM, Cowey CL, Dalle S, Schenker M, Chiarion-Sileni V,
Marquez-Rodas I, et al: Adjuvant nivolumab versus ipilimumab in
resected stage III or IV melanoma. N Engl J Med. 377:1824–1835.
2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Eggermont AM, Chiarion-Sileni V, Grob JJ,
Dummer R, Wolchok JD, Schmidt H, Hamid O, Robert C, Ascierto PA,
Richards JM, et al: Prolonged survival in stage III melanoma with
ipilimumab adjuvant therapy. N Engl J Med. 375:1845–1855.
2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Eggermont AM, Suciu S, Testori A,
Santinami M, Kruit WH, Marsden J, Punt CJ, Salès F, Dummer R,
Robert C, et al: Long-term results of the randomized phase III
trial EORTC 18991 of adjuvant therapy with pegylated interferon
alfa-2b versus observation in resected stage III melanoma. J Clin
Oncol. 30:3810–3818. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Arima M, Iwata Y, Morita Y, Kobayashi T,
Sasaki R, Suzuki K and Matsunaga K: A case of malignant melanoma
with in-transit metastasis that responded to intravenous infusion
of interferon-β. Case Rep Dermatol. 6:74–79. 2014.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kubo H, Ashida A, Matsumoto K, Kageshita
T, Yamamoto A and Saida T: Interferon-beta therapy for malignant
melanoma: The dose is crucial for inhibition of proliferation and
induction of apoptosis of melanoma cells. Arch Dermatol Res.
300:297–301. 2008.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Nan Tie E, Lai-Kwon J, Rtshiladze MA, Na
L, Bozzi J, Read T, Atkinson V, Au-Yeung G, Long GV, McArthur GA,
et al: Efficacy of immune checkpoint inhibitors for in-transit
melanoma. J Immunother Cancer. 8(e000440)2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Di Trolio R, Simeone E, Di Lorenzo G,
Buonerba C and Ascierto PA: The use of interferon in melanoma
patients: A systemic review. Cytokine Growth Factor Rev.
26:203–212. 2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Fujimura T, Hidaka T, Kambayashi Y,
Furudate S, Kakizaki A, Tono H, Tsukada A, Haga T, Hashimoto A,
Morimoto R, et al: Phase I study of nivolumab combined with IFN-β
for patients with advanced melanoma. Oncotarget. 8:71181–71187.
2017.PubMed/NCBI View Article : Google Scholar
|