Introduction
Breast cancer frequently metastasizes to the liver,
bone and lung (1) and only 8% of
breast carcinomas are reported to metastasize to the uterus
(2). Furthermore, only 3.8% of
breast metastases to gynecological organs consist of metastases to
the uterus (2). Metastasis of
extragenital cancer to the female genital organs is uncommon and
frequently involves metastasis to the ovaries (3). Metastases to the uterus from
extragenital cancers are rare [3.7% of metastatic tumors to the
female genital tract from extragenital cancers (2,4)] and
are frequently caused by cancers of the gynecological organs,
rather than extragenital sites (4). In addition, the most common type of
primary cancer that causes uterine metastasis is breast cancer,
accounting for 42.9% of uterine metastases, followed by colon
cancer (17.5%) and stomach cancer (11.1%). In addition, the results
of a previous study demonstrated that the uterine myometrium is
more likely to be involved than the uterine endometrium (4). Metastasis to the myometrium remains
asymptomatic; however, abnormal genital bleeding is a common
symptom of metastasis when the endometrium has a role.
The most common type of breast carcinoma that
metastasizes to the uterus is invasive lobular carcinoma (ILC)
(5). After invasive ductal
carcinoma (IDC), ILC is the second most common type of breast
cancer, comprising of 10% of all invasive breast cancers (3). The results of a previous study
demonstrated that ILC frequently metastasizes to distant lesions
(3), and ILC frequently
metastasizes to the peritoneum, ovaries and gastrointestinal tract
(6).
The present report described the case of a
66-year-old female patient who developed uterine metastasis 23
years following the primary treatment of invasive breast cancer,
who presented with abnormal genital bleeding.
Case report
A 66-year-old female (gravida 5, para 3) was
referred to the Gynecology Department of Osaka City University
Hospital (Osaka, Japan) due to abnormal genital bleeding lasting
for 2 months. The patient experienced menopause at the age of 56
years. The patient was also diagnosed with right invasive lobular
breast cancer at the age of 43 years and received right breast
resection and chemotherapy (detailed treatment is unknown due to a
lack of medical records). The patient was further diagnosed with
recurrence on the right breast and multiple bone metastases at the
age of 60 years and was subsequently treated with aromatase
inhibitors followed by tamoxifen citrate. At 23 years after the
primary surgery (age, 66 years), the patient presented with
abnormal genital bleeding lasting for 2 months. Gynecological
examination revealed a small amount of bloody vaginal discharge and
an enlarged uterine cervix. The uterine corpus was also enlarged
and mobility was restricted. It was not possible to palpitate the
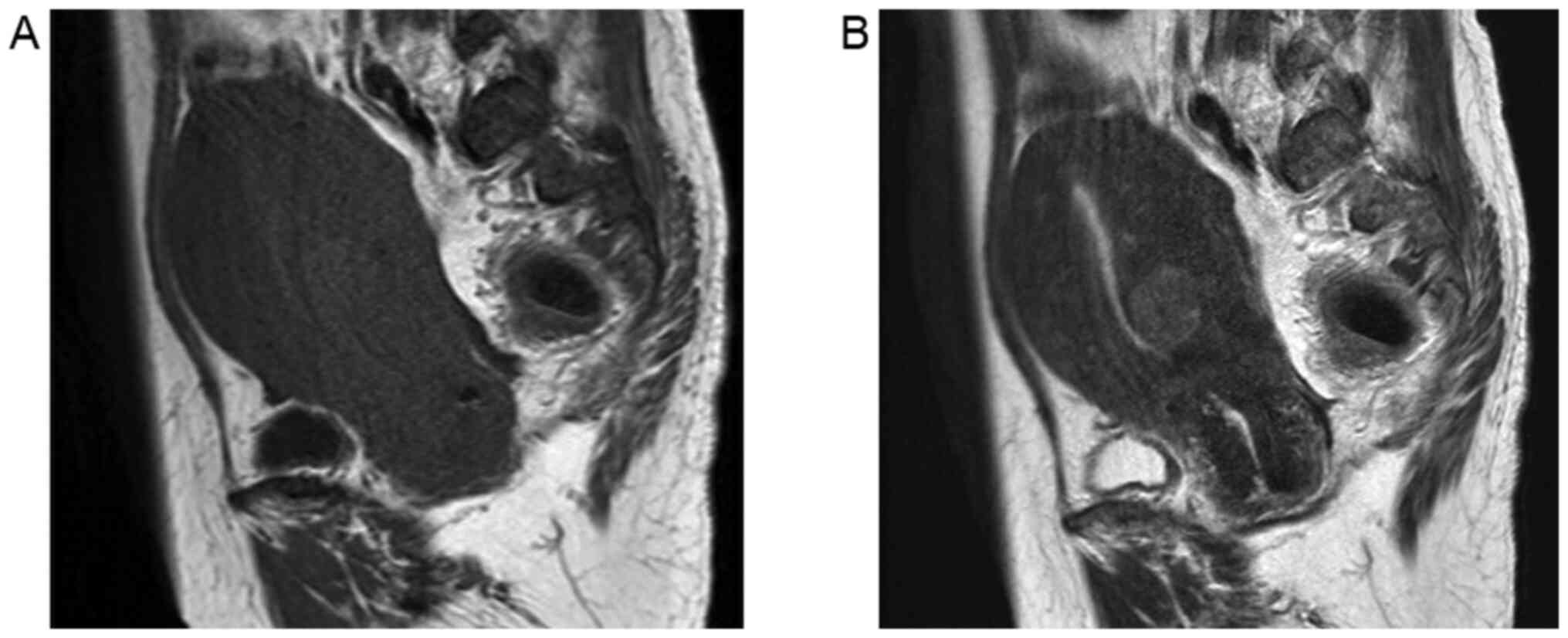
bilateral adnexa. Magnetic resonance imaging of the pelvis revealed
that the thickness of the endometrium was 7 mm and there was no
notable mass in the endometrium (Fig.
1). The myometrium of the uterus was enlarged, which appeared
to be due to the presence of adenomyosis. Furthermore, a 15-mm
degenerated myoma was present on the posterior myometrium. Computed
tomography scan of the chest and abdomen revealed multiple bone
metastases, which had previously been reported, and no evidence of
metastasis to the other organs. Uterine cervical cytology revealed
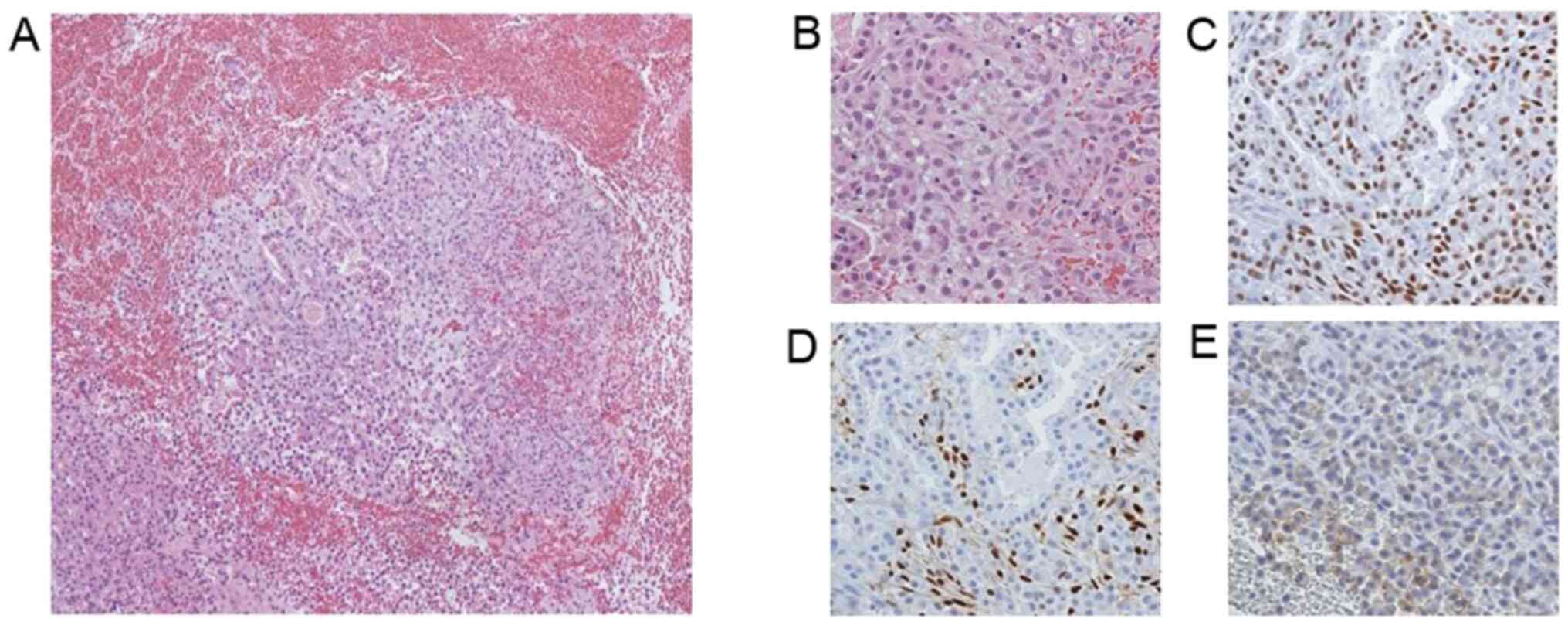
no malignancy. Biopsy of the endometrium and routine staining for
estrogen receptor (ER; ++), progesterone receptor (PR; +/-) and
human epidermal growth factor receptor 2 (HER2; +/-) revealed
adenocarcinoma. It was therefore difficult to differentiate whether
this was metastasis from breast cancer or primary endometrial
adenocarcinoma (Fig. 2). Abdominal
total hysterectomy, bilateral salpingo-oophorectomy, partial
omentectomy and biopsy of the peritoneum were subsequently
performed. Multiple millet-sized metastases were observed at the
peritoneum, mesentery, surface of the intestines, omentum and
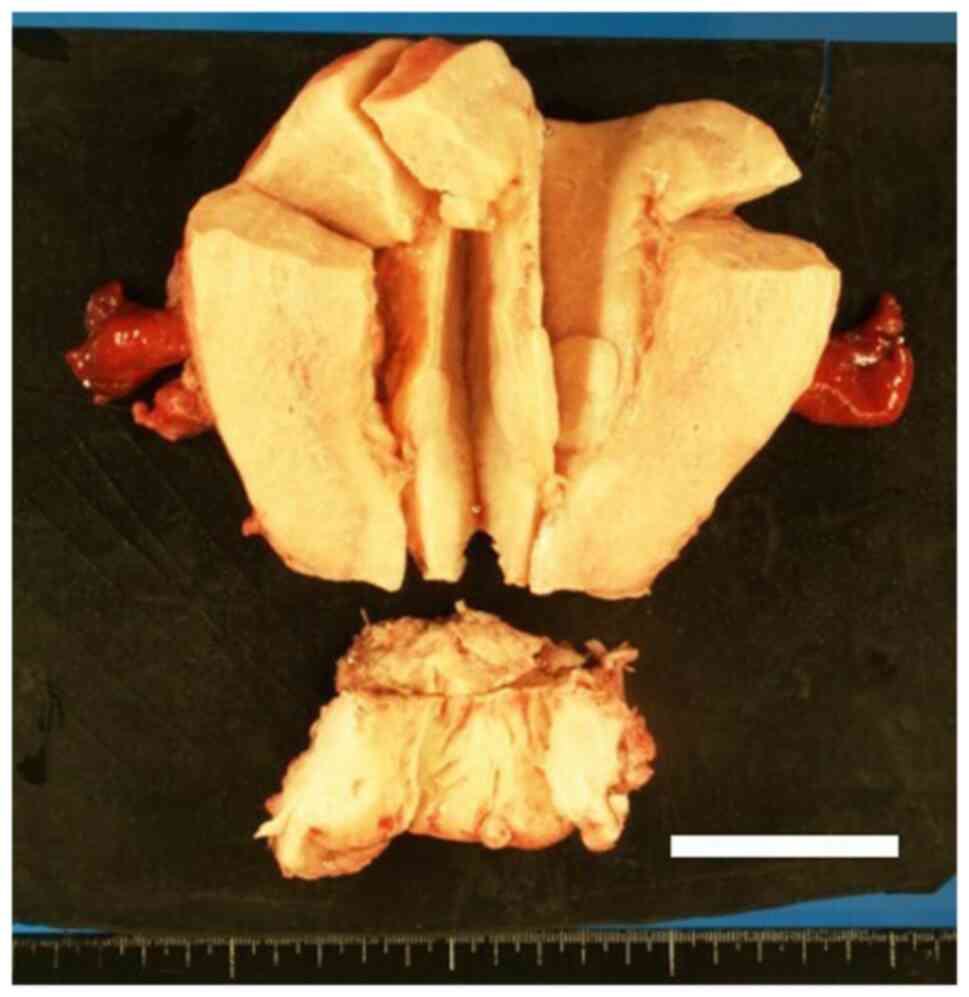
diaphragm. On gross inspection following specimen removal, diffuse
enlargement of the myometrium and irregular surface of the
endometrium were revealed (Fig.
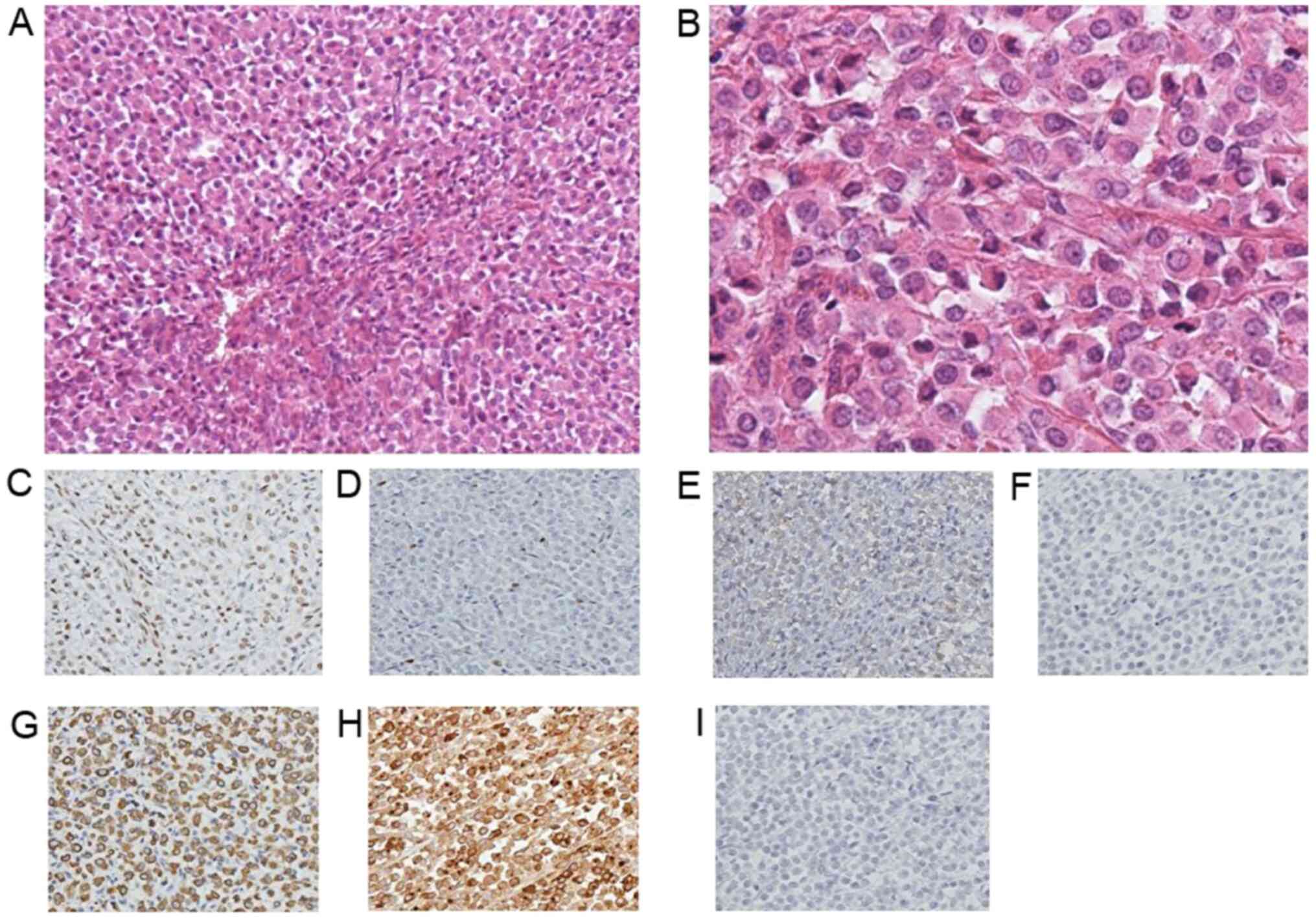
3). As displayed in Fig. 4,
the results of the pathological examination revealed diffuse
invasion of breast lobular cancer to the cervical stroma,
myometrium, cardinal ligament, bilateral adnexa, omentum and
peritoneum. Immunohistochemical analysis demonstrated ER (++), PR
(+/-), HER2 (+/-), CD10 (-), CAM5.2 (+), gross cystic disease fluid
protein-15 (GCDFP; +) and E-cadherin (-). Negative staining for
CD10 indicated that the tumor had not originated from the
endometrium. Positive staining for GCDFP indicated that the tumor
had originated from the breast and negative staining for E-cadherin
suggested that the tumor was lobular carcinoma, rather than ductal
carcinoma. The patient has since been treated with fulvestrant,
toremifene citrate and tegafur, and the current patient survival
duration is 2 years and 8 months.
Discussion
Mazur et al (2) reported that the most frequently
affected female genital tract by metastatic disease from
extragenital cancers is the ovaries (75%), followed by the vagina
(5.8%), endometrium (3.8%), cervix (3.4%) and vulva (2%) (2). Of note, the breast and
gastrointestinal tract are the most common origins of primary
tumors that subsequently metastasize to the female genital tract
(4). When uterine metastasis is
diagnosed, the most frequent origin of the primary tumor is breast
cancer (42.9%) (4). Furthermore,
results of a previous study demonstrated that 63.5% of uterine
corpus metastasis cases involved the myometrium alone, 32.7% of the
cases involved both the myometrium and endometrium and 3.8% of the
cases involved the endometrium alone (2).
The ovaries are frequently involved in the spread of
metastatic cancer cells (2). The
rich vasculature and well-developed lymph network of the ovaries
provide a favorable environment for the implantation of cancer
cells. Of note, both the pH levels and oxygen pressure in the
stroma of the ovaries are favorable for the growth and development
of cancer cells (7,8). Retrograde lymphatic spreading of an
ovary-originating primary tumor causes metastasis to the uterus in
~60% of patients; however, cases of metastases to the uterus
without affected ovaries are rare and may be caused by hematogenous
spread (4).
Breast cancer is the most common malignancy in
females. A total of >2 million breast cancer cases are diagnosed
per year and breast cancer leads to >600,000 cancer-associated
mortalities worldwide (9). Due to
advances in breast cancer treatments and early diagnoses, the
breast cancer survival rate is improving (10). Consequently, the number of females
living with metastatic breast cancer has increased (11).
The two most frequent histological subtypes of
breast cancer are IDC and ILC (3).
A total of ~76% of all breast cancers are categorized as IDC, and
~8% of all breast cancers are categorized as ILC (3). Although the incidence rate remains
low, ILC frequently metastasizes to the female genital tract
(4). Frequent metastasis of ILC is
caused by reduced levels of expression of the cellular adhesion
molecule E-cadherin, which is not observed in IDC (12). ILC is also characterized by reduced
sensitivity to neoadjuvant chemotherapy compared with IDC (13).
Tamoxifen is a widely-established oral drug for the
treatment of ER-positive breast cancer. Tamoxifen acts as a
selective ER modulator in the breast; however, it also behaves as
an estrogen agonist on the endometrium, resulting in increased
levels of carcinogenesis (14).
Thus, patients with breast cancer who are treated with tamoxifen
may suffer from uterine metastases, as well as primary endometrial
cancer.
Abnormal genital bleeding is the most common initial
manifestation of primary endometrial cancer and is also the first
symptom of endometrial metastases (4). Abnormal genital bleeding occurs when
the endometrium or the cervix is involved in tumor development and
progression. Thus, patients with a previous history of breast
cancer and treatment with tamoxifen who present with abnormal
genital bleeding must be examined for primary endometrial cancer
and metastatic uterine cancer.
Both the clinical history of the patient and
pathological examination, including immunohistochemical analysis,
are required in order to differentiate between metastatic breast
cancer and primary endometrial cancer, as their treatment strategy
and prognosis exhibit marked differences. A key biomarker for the
differentiation of primary endometrial cancer from metastatic
breast cancer is GCDFP. GCDFP is a glycoprotein originally detected
in the cystic fluid following cystic mastopathy and is therefore a
useful immunohistochemical marker to evaluate the potential mammary
origin of a tumor when the primary site remains to be elucidated
(15). In the present case report,
metastatic uterine cancer was successfully diagnosed following
positive immunohistochemical staining for GCDFP.
In conclusion, the present report described the case
of a 66-year-old female who developed uterine metastasis 23 years
after the primary treatment of invasive lobular breast cancer. The
patient also presented with abnormal genital bleeding. Thus, the
present report highlights the importance of considering not only
primary endometrial cancer, but also uterine metastasis from breast
cancer in the diagnostic process. This consideration is crucial
when a patient with breast cancer undergoing hormonal therapy, such
as tamoxifen, presents with abnormal genital bleeding, despite the
rarity of uterine metastases from breast cancer.
Acknowledgements
Not applicable.
Funding
This study was funded by The Osaka Medical Research Foundation
for Intractable Diseases (grant no. 27-2-4).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
YA, TF and TS conceived and designed the study. YA,
TF, KI, MY, MK, TI and TY acquired, analyzed and interpreted the
data. YA, TF and TS drafted and revised the manuscript. TF and TS
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the case details and any associated
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Almagro E, González CS and Espinosa E:
Prognostic factors of early breast cancer. Med Clin (Barc).
146:167–171. 2016.PubMed/NCBI View Article : Google Scholar : (In Spanish).
|
|
2
|
Mazur MT, Hsueh S and Gersell DJ:
Metastases to the female genital tract. Analysis of 325 cases.
Cancer. 53:1978–1984. 1984.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Watkins EJ: Overview of breast cancer.
JAAPA. 32:13–17. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Kumar NB and Hart WR: Metastases to the
uterine corpus from extragenital cancers. A clinicopathologic study
of 63 cases. Cancer. 50:2163–2169. 1982.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Harris M, Howell A, Chrissohou M, Swindell
RI, Hudson M and Sellwood RA: A comparison of the metastatic
pattern of infiltrating lobular carcinoma and infiltrating duct
carcinoma of the breast. Br J Cancer. 50:23–30. 1984.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Arpino G, Bardou VJ, Clark GM and Elledge
RM: Infiltrating lobular carcinoma of the breast: Tumor
characteristics and clinical outcome. Breast Cancer Res.
6:R149–R156. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
7
|
Perisić D, Jancić S, Kalinović D and
Cekerevac M: Metastasis of lobular breast carcinoma to the cervix.
J Obstet Gynaecol Res. 33:578–580. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Razia S, Nakayama K, Tsukao M, Nakamura K,
Ishikawa M, Ishibashi T, Ishikawa N, Sanuki K, Yamashita H, Ono R,
et al: Metastasis of breast cancer to an endometrial polyp, the
cervix and a leiomyoma: A case report and review of the literature.
Oncol Lett. 14:4585–4592. 2017.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Giordano SH, Buzdar AU, Smith TL, Kau SW,
Yang Y and Hortobagyi GN: Is breast cancer survival improving?
Cancer. 100:44–52. 2004.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mariotto AB, Etzioni R, Hurlbert M,
Penberthy L and Mayer M: Estimation of the number of women living
with metastatic breast cancer in the United States. Cancer
Epidemiol Biomarkers Prev. 26:809–815. 2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Li CI, Uribe DJ and Daling JR: Clinical
characteristics of different histologic types of breast cancer. Br
J Cancer. 93:1046–1052. 2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fu D, Zuo Q, Huang Q, Su L, Ring HZ and
Ring BZ: Molecular Classification of Lobular Carcinoma of the
Breast. Sci Rep. 7(43265)2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Barakat RR: Tamoxifen and endometrial
neoplasia. Clin Obstet Gynecol. 39:629–640. 1996.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Darb-Esfahani S, von Minckwitz G, Denkert
C, Ataseven B, Högel B, Mehta K, Kaltenecker G, Rüdiger T, Pfitzner
B, Kittel K, et al: Gross cystic disease fluid protein 15
(GCDFP-15) expression in breast cancer subtypes. BMC Cancer.
14(546)2014.PubMed/NCBI View Article : Google Scholar
|