Introduction
Mandibular lesions are classified as odontogenic and
non-odontogenic based on the cell of origin. A lesion associated
with an impacted tooth frequently indicates an odontogenic origin.
Non-odontogenic lesions, however, develop from osseous origin and
are not tooth related (1,2).
Most malignant neoplasms of the mandible are
secondary to tumor invasion from the surrounding mucosa of the oral
cavity (3,4). Metastatic disease may involve the
mandible. The most common sites of origin include the kidneys,
lungs and the breasts (3,4). Primary intraosseous malignant
neoplasm of the mandible is a very rare entity and has been
hypothesized to originate from the remnants of odontogenic
epithelium and has no initial connection with the oral mucosa
(3,4). For the diagnosis of primary
intraosseous malignant neoplasm of the mandible, tumor invasion or
metastasis to the mandible from another oral cavity or distant
location must be excluded (2,4).
There have only been a small number of reports on
primary mandibular neoplasm in the literature (5-9).
There are few publications regarding fluorodeoxyglucose (FDG)
positron emission tomography (PET)/CT for primary intraosseous
neoplasms of the mandible (10-12),
due to the rarity of the disease.
The aim of the present study was to evaluate the
value of FDG PET/CT for primary mandibular neoplasm. Therefore,
patients with primary malignant neoplasm of the mandible were
identified from the Picture Archiving and Communication System
database, and FDG PET/CT imaging and all clinical documents were
reviewed.
Materials and methods
Ethics and patients
The present retrospective study was approved by the
Institutional Review board at New Jersey Medical School, Rutgers
University (NJ, USA). Relevant cases were identified by searching a
computerized database containing 6,500 patients with cancer who
underwent PET/CT imaging at the Advanced Imaging Center, Rutgers
New Jersey Medical School (NJ, USA) between January 2010 and June
2020. A total of 10 patients, who had FDG PET/CT for primary
mandible lesions or neoplasms, were selected for the study based on
the following inclusion criteria: i) Histopathologically confirmed
malignant intraosseous neoplasms of the mandible prior to FDG
PET/CT; ii) exclusion of other neoplasms, especially in the head
and neck by medical history; iii) comprehensive examinations; and
iv) laboratory and image evaluations. A total of 6,490 patients
with known neoplasm at other locations (such as the tonsils,
tongue, larynx, lungs and colorectum), metastatic mandible lesions
or radiation-induced mandibular necrosis were excluded from the
study.
Prior to FDG PET/CT, 7 patients had diagnostic
imaging using contrast-enhanced neck CT. All eligible subjects had
available histopathological investigations, clinical and image
follow-up data following PET/CT.
FDG PET/CT scan
Combined PET/CT was performed using a PET/CT scanner
(Discovery LS; GE Healthcare) and the standard techniques. The
patients had fasted for at least 6 h prior to examination and their
blood glucose level was <250 mg/dl. The patients received 15 mCi
intravenous FDG administration, immediately followed by oral
administration of 500 ml diluted Gastrografin. Spiral low-dose CT
(80 mA; 140 kV; 4 mm section thickness) was performed with the
cranio-caudal direction covering the areas from the vertex to the
mid-thigh for the purpose of attenuation correction and anatomic
localization, 60 min later. Thereafter, emission scan was conducted
in a reverse direction.
Image analysis
Diagnostic CT images were interpreted by the
radiologists specialized in head and neck imaging. MIM image
software (v6.9.4; MIM Software, Inc.) was used for PET/CT image
display and analysis. The whole-body maximum-pixel-intensity
projection was used for visual evaluation. Maximum standardized
uptake value (SUVmax) of the lesions was recorded. All
the selected images were re-interpreted by the investigator for
accuracy of previous dictation reports.
Histopathological and/or cytopathological diagnosis
was inferred from the electronic medical documents, Epic and
Logician.
The performance of FDG PET/CT was evaluated based on
the association of the image findings with histopathological
results, and the sensitivity, specificity and accuracy of FDG
PET/CT were calculated for primary mandible and/or distant
metastatic lesions.
Results
Patient characteristics
A total of 10 patients and 16 scans were analyzed in
the present study (Table I). There
were 7 males and 3 females, with a mean age of 69 years (range,
29-82 years). For the first FDG PET/CT scans, 9 patients were for
staging and 1 was for restaging following surgery. A total of 6 out
of 10 patients had follow-up restaging images after the first scan.
The diagnosis of primary intraosseous neoplasms of the mandible was
verified using FDG PET/CT, which excluded other primary lesions or
tumors in all the patients.
 | Table ICharacteristics of patients with
primary malignant neoplasms of the mandible. |
Table I
Characteristics of patients with
primary malignant neoplasms of the mandible.
| | PET/CT findings | |
|---|
| Patient number | Age, years | Sex | Scan number | Pre-PET pathology and
indication | Prior
contrast-enhanced neck CT | Outcome | SUV | Regional lymph
nodes | Distant
metastasis | Treatment | Final pathology | F/U |
|---|
| 1 | 81 | M | 2 | SCC staging | None | R. mandible
destruction | 8.8 | No | No | Mandibulectomy and
RT | SCC LN (-) | 1 PET/CT in 1 year,
neg |
| 2 | 64 | M | 2 | SCC staging | L. mandible lesion
and L. neck nodes | L. mandible
destruction | 14.7 | L. neck | No | Mandibulectomy and
RT | SCC LN (+) | 1 PET/CT in 1 year,
neg |
| 3 | 84 | F | 2 | SCC staging | R. mandible lesion
and R. LN | R. mandible
destruction with ST involvement | 28 | R. neck | No | None | SCC LN (+) | Restaging PET/CT,
worse |
| 4 | 68 | F | 1 | SCC staging | R. mandible lesion
and R. neck LN | R. mandibular
destruction with ST invasion | 11 | No (no LN
uptake) | No | Segmental
mandibulectomy and R. neck dissection | SCC LN (-) | None |
| 5 | 82 | F | 2 | SCC staging | None | R. mandible
destruction with ST invasion | 9.4 | No | No | Keytruda therapy for
8 m | SCC LN (-) | Restaging PET/CT,
decreased extent and uptake. SUV 3.8 |
| 6 | 59 | M | 1 | SCC staging | R. mandible lesion
with ST component, small R. LN | R. mandible
destruction with ST invasion | 15 9.3 | R. neck. 1.2 cm with
SUV 5.0 L. neck LN | No Spleen | No Chemo for | SCC LN (+) DLBCL | None Restaging |
| 7 | 76 | M | 2 | DLBCL staging | None | L. mandible lytic
lesion with ST involvement | | | | 4 months | LN (+) | PET/CT, worse with
new intracranial lesion |
| 8 | 77 | M | 1 | Adenocarcinoma
staging | R. mandible lesion.
No LN | R. mandible lytic
lesion | 7.0 | R. neck LN, 1.1 cm
with SUV 7.1 | No | Chemo | Adenocarcinoma LN
(+) | None |
| 9 | 68 | M | 1 | Plasmocytoma
staging | L mandible lesion and
LN | Lytic L. mandible
lesion with FOM involvement | 35 | L. neck LNs | R. ilium | Chemo and RT | Plasmocytoma LN
(+) | None |
| 10 | 29 | M | 2 | Ameloblastic
fibrosarcoma restaging | L. mandibulectomy. No
LN | RLL lung lesion, 2
cm | 9.8 | No | R. lung | RLL
segmentectomy | Metastatic
fibrosarcoma | Repeat PET/CT in 3
months, neg |
All of the 10 patients had histopathological
confirmed primary mandible neoplasms, including 6 squamous cell
carcinoma, 1 diffuse large B-cell lymphoma, 1 adenocarcinoma, 1
plasmacytoma and 1 ameloblastic fibrosarcoma. A total of 6 patients
had a primary lesion on the right, with 4 on the left.
FDG PET/CT findings
All the untreated primary mandible neoplasms
demonstrated high FDG avidity on the PET imaging, with a mean
SUVmax, 14.8±9.3 (range, 7.0-35). Most mandible lesions
extended beyond the bones and involved perimandibular soft tissue,
and 2 invaded the ipsilateral floor of the month. The results were
suggestive of high FDG avidity and high sensitivity of PET/CT in
detection of primary mandible tumors. Contrast-enhanced diagnostic
CT imaging of the neck in 7 out of 10 patients showed similar bone
lesion as FDG PET; however, PET images could define the involvement
of soft tissue compared with that for contrast-enhanced diagnostic
CT. In 7 patients with diagnostic CT prior to FDG PET/CT, soft
tissue involvement or invasion was well documented on only 1 report
(patient 6).
On the integrated CT appearance, all mandible tumors
showed lytic/destructive or mixed lytic/sclerotic lesions. There
was no pure sclerotic or osteoblastic lesion in any of the
patients.
PET/CT for N and M staging
While N staging of the disease is solely based on
the size of lymph nodes from anatomic images, defined as positive
for those >1 cm (2), FDG PET
imaging showed improved sensitivity and specificity compared with
that for contrast-enhanced diagnostic CT for N staging. A total of
6 out of 10 patients had ipsilateral lymph node metastases on the
initial PET/CT staging scan, and all were verified by surgical
pathology. A total of 7 patients had contrast-enhanced diagnostic
neck CT prior to PET/CT. While diagnostic CT and FDG PET/CT had
similar findings for regional lymphadenopathy in 4 out of 7
patients, there were 3 patients with whom the diagnostic neck CT
and FDG PET had discordant findings. For patient 4, the diagnostic
neck CT, on the same day as PET/CT, showed right mandibular lesion
and two 1.3 cm ipsilateral right level IB lymph nodes, suspicious
for metastases based on the size criteria. However, there was no
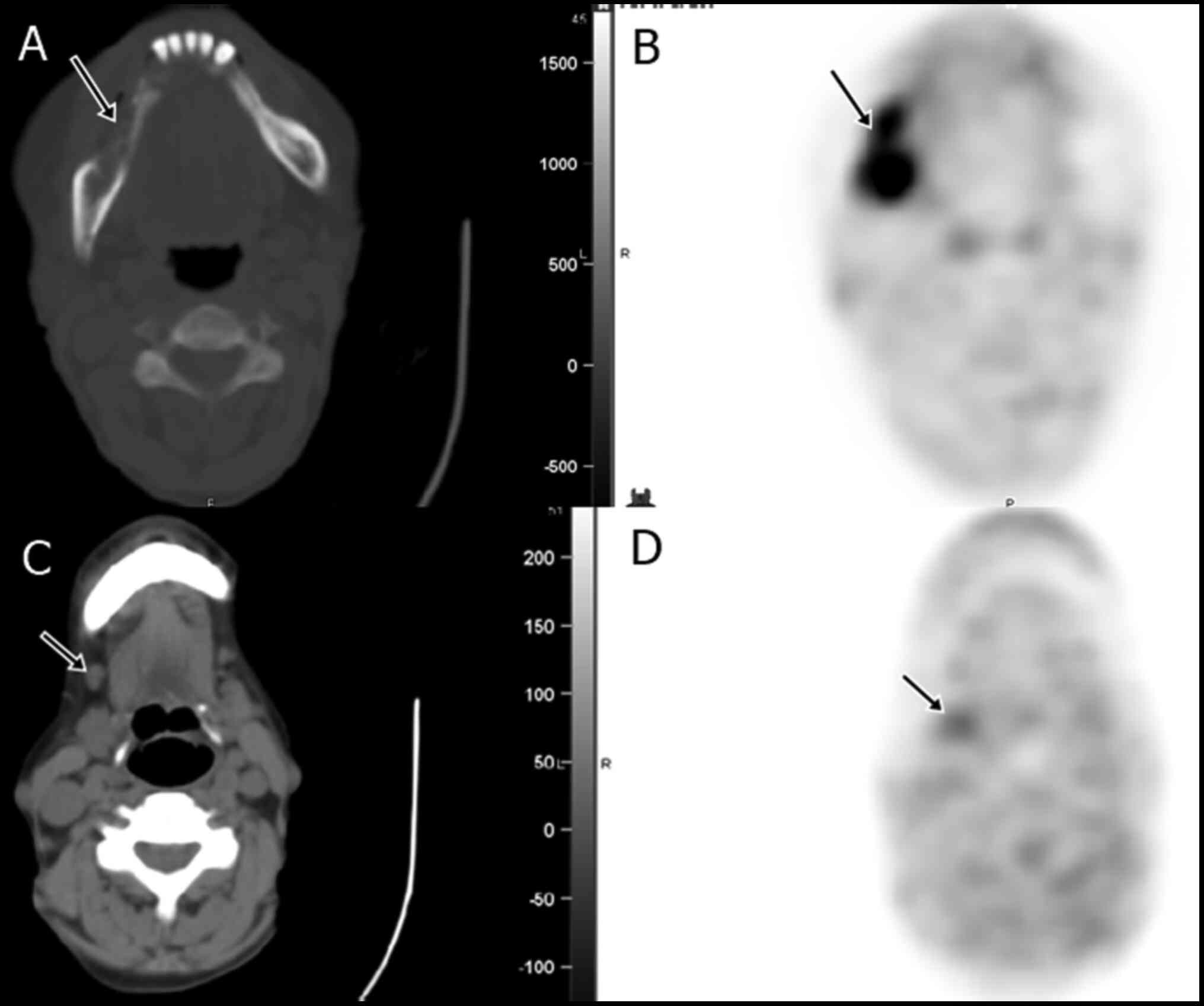
FDG uptake of the lymph nodes on FDG PET/CT (Fig. 1). Surgical pathology from
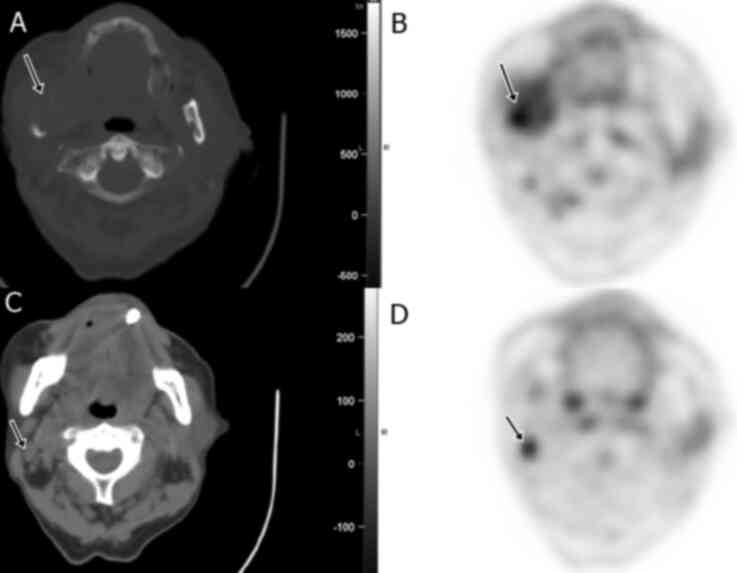
dissection was negative in both lymph nodes. However, for patients
6 and 8, the diagnostic CT did not report lymphadenopathy, but the
FDG PET/CT scan revealed a 1.2 cm and 1.1 cm right level II lymph
node, with moderate to intense uptake (SUV, 5.0 and 7.1
respectively), consistent with nodal metastases, which were
confirmed by surgical histopathological examinations (Fig. 2, for patient 8). Therefore, in
these three cases, diagnostic CT was false positive for one case
and false negative for 2 cases, but there was no false positives or
negatives for FDG PET/CT.
None of the 10 patients had image workups for
distant metastasis prior to FDG PET/CT. In 3 out of 10 patients
with the first FDG PET/CT scan, distant metastatic disease was
detected in the spleen, ilium and lung, respectively. Another
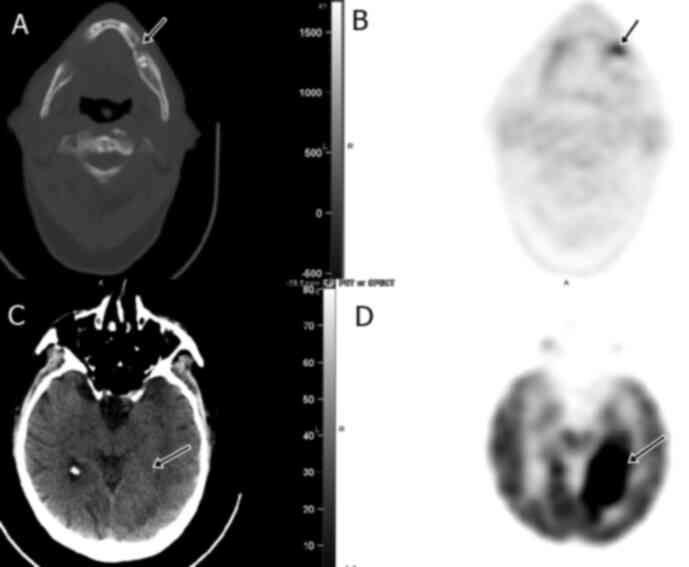
patient developed intracranial metastasis on the restaging scan
(Fig. 3, patient 7). Overall, the
FDG PET/CT scan identified 4 distant metastases from the 10
patients, which were either unknown or not documented prior to
PET/CT. From the 4 distant metastatic lesions, 2 (lung and brain)
were verified by surgical pathology and another (spleen lesion) was
confirmed by biopsy.
PET/CT for restaging
A total of 6 out of 10 patients had a 2nd FDG PET/CT
scan for restaging with or without treatment. A total of 3
patients, who had surgical resections (2 mandibulectomy and 1 lung
segmentectomy), were negative on the restaging scans, 1 patient had
worse disease and new intracranial metastasis after 4-months of
chemotherapy, 1 patient had improvement of the disease extent and
FDG uptake after 8-months Keytruda treatment, and 1 had worsening
primary neoplasm and local nodal disease 6 months later without any
treatment.
Overall PET/CT performance
Combining all of the 16 FDG PET/CT scans from the 10
patients, sensitivity, specificity, and accuracy for primary
mandible and/or distant metastatic lesions were 100% (13/13), 100%
(3/3) and 100% (16/16), respectively.
For N staging of the initial scans, FDG PET/CT
sensitivity, specificity and accuracy were 100% (5/5), 100% (4/4)
and 100% (9/9), compared with that for diagnostic CT, 75% (3/4),
50% (1/2) and 67% (4/6), respectively.
Discussion
A variety of benign and malignant neoplasms may
originate in the mandible. Primary malignant mandibular neoplasm is
very rare, with only a few case reports regarding image diagnosis
in the literature (1-4).
In the present study, the most common malignant tumor of the
mandible was squamous cell carcinoma, consistent with previous
studies (13-15).
Primary intraosseous malignant neoplasms affect men more than women
and is more frequent in the 6th and 7th decades of life (16,17).
In the present study, 7 out of 10 patients were men and 8 out of 10
were >60 years old, with a mean age of 69 years.
The posterior mandible has been the most common site
of tumor occurrence. Image exanimation is often the first
evaluation of the suspected mandibular lesion (1,4). A
lesion that is surrounded by bone can be regarded as of
intraosseous origin. Radiographical lesions usually show a fully
enclosed, irregular pattern of bone destruction with ill-defined
margin (2). However, image
findings are non-specific with similar appearance in a wide range
of pathology. The recommended treatment is radical surgery and neck
dissection (2-4).
In general, prognosis is poor (15).
The patient data analyzed in the present study
demonstrated that FDG PET/CT was a valuable image modality for
staging and restaging primary mandibular neoplasm. There was high
FDG avidity of all primary and metastatic lesions. FDG PET/CT could
define perimandibular soft tissue involvement, detect regional
lymph node and distant metastases with 100% accuracy. In numerous
patients with primary mandibular lesions, there was hyperemia of
the adjacent soft tissue and muscles, which might demonstrate
contrast enhancement on the diagnostic CT and could not be
distinguished from tumor extension. The uptake intensity of the
soft tissue/muscles adjacent to the mandibular tumor on the PET
image could assist with identifying soft tissue involvement or
invasion. Compared to contrast-enhanced diagnostic CT, FDG PET/CT
also provided superior N staging. There were three patients with
discordant findings between the diagnostic CT and FDG PET/CT
images, and surgical pathology verified that FDG uptake in these
lymph nodes was more liable than the size criteria for N-staging.
It is well-known that FDG PET/CT plays a valuable role in M-staging
due to its whole-body acquisition protocol in oncology (2,10).
In the present study, none of the 10 patients had image workups for
distant metastasis prior to FDG PET/CT, which might be due to
scheduled FDG PET/CT, as it scans the whole body. On the initial
staging, three patients were found to have distant metastases in
the lung, spleen and ilium respectively, which were all unexpected
since there was no prior imaging for distant metastasis. Additional
intracranial metastasis was detected from the restaging scan in 1
of these 3 patients. Identification of distant metastases changed
the patient's therapeutic strategy. The results might suggest that
FDG PET/CT was an effective image modality for surveillance,
monitoring therapeutic response and detection of metastatic
disease.
The diagnosis of primary intraosseous cancer of the
mandible requires exclusion of other oral cavity tumors and
different primary neoplasms. The mandibular lesion must be
distinguished from the tumors that metastasize to the jaw from
distant sites, from gingival carcinomas that have invaded the bone
from the surface, and from tumors that originated from maxillary
sinus (1,4). For exclusion of another primary
tumors, whole-body FDG PET/CT may be the best modality to rule out
synchronous lesions or separate primary (18).
Compared to previously published reports regarding
FDG PET/CT for primary malignant intraosseous neoplasms of the
mandible (10-12),
the results from the present study represent the largest number of
cases with FDG PET/CT scans in more varied types of tumor
pathology. Published cases regarding FDG PET/CT in primary
malignant mandibular tumors were all for squamous cell carcinoma.
The current study presented FDG PET/CT image findings in additional
rare primary neoplasms of the mandible: Diffuse large B-cell
lymphoma, adenocarcinoma, plasmacytoma and ameloblastic
fibrosarcoma. FDG PET/CT is well-known for its improved sensitivity
and accuracy in N and M staging than conventional anatomical image
modalities in oncology; however, the current study clearly
demonstrated the value of FDG PET/CT in this special group of
patients, which is similar to other malignant neoplasms, such as
oral cavity cancer, laryngeal cancer, lymphoma and lung cancer
(19).
A notable limitation of the present study is the
small sample size, due to the rarity of the disease, which made
statistical analysis less powerful. In addition, referral and image
selection bias should be considered. Another limitation is the lack
of color fusion PET/CT images for review of the image examples.
In conclusion, the results of FDG PET/CT images from
10 patients with primary intraosseous malignant neoplasms showed
high FDG avidity in all the primary and metastatic lesions,
improved definition of perimandibular soft tissue involvement, more
accurate regional N-staging and M-staging than the
contrast-enhanced diagnostic CT. In addition, whole-body FDG PET/CT
is a valuable image modality for exclusion of synchronous lesions
or separate primary and verification of diagnosis of primary
intraosseous neoplasm of the mandible as well.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Author's contributions
YL was a sole author and performed the study
including the conception and design, acquisition, analysis and
interpretation of data, and preparation of the manuscript. YL also
confirms the authenticity of all the raw data.
Ethics approval and consent to
participate
This retrospective study was approved by the
Institutional Review board at New Jersey Medical School, Rutgers
University (approval no, Pro2018001712), and the requirement for
written informed consent was waived.
Patient consent for publication
Not applicable.
Competing interests
The author declares that they have no competing
interests.
References
|
1
|
Looser KG and Kuehn PG: Primary tumors of
the mandible. A study of 49 cases. Am J Surg. 132:608–614.
1976.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Dunfee BL, Sakai O, Pistey R and Gohel A:
Radiologic and pathologic characteristics of benign and malignant
lesions of the mandible. Radiographics. 26:1751–1768.
2006.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Zachariades N: Neoplasms metastatic to the
mouth, jaws and surrounding tissues. J Craniomaxillofac Surg.
17:283–290. 1989.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Weber AL, Bui C and Kaneda T: Malignant
tumors of the mandible and maxilla. Neuroimaging Clin N Am.
13:509–524. 2003.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lopes Dias J, Borges A and Lima Rego R:
Primary intraosseous squamous cell carcinoma of the mandible: A
case with atypical imaging features. BJR Case Rep.
2(20150276)2016.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hu HY, Liu YY, Wang H and Jiang M: Primary
Intraosseous Adenoid Cystic Carcinoma of the Mandible: A
Comprehensive Review With Analysis of 2 Additional Cases. J Oral
Maxillofac Surg. 75:1685–1701. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Kawano K, Ono K, Yada N, Takahashi Y,
Kashima K, Yokoyama S and Yanagisawa S: Malignant calcifying
epithelial odontogenic tumor of the mandible: Report of a case with
pulmonary metastasis showing remarkable response to platinum
derivatives. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
104:76–81. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Schneider LC, Dolinsky HB, Grodjesk JE,
Mesa ML and Doyle JL: Malignant spindle cell tumor arising in the
mandible of a patient with florid osseous dysplasia. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod. 88:69–73. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mintz GA, Abrams AM, Carlsen GD, Melrose
RJ and Fister HW: Primary malignant giant cell tumor of the
mandible. Report of a case and review of the literature. Oral Surg
Oral Med Oral Pathol. 51:164–171. 1981.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Bosch-Barrera J, Arbea L, García-Velloso
MJ, Gil-Bazo I, García-Foncillas J and Panizo C: Primary bone
lymphoma of the mandible and thyroid incidentaloma identified by
FDG PET/CT: A case report. Cases J. 2(6384)2009.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Strobel K, Merwald M, Huellner M,
Zenklusen HR and Kuttenberger J: Osteoblastoma of the mandible
mimicking osteosarcoma in FDG PET/CT imaging. Clin Nucl Med.
38:143–144. 2013.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Takami Y, Aga F, Mitamura K, Norikane T,
Okuda H, Yamamoto Y, Miyake M and Nishiyama Y: A Case of Ewing
Sarcoma of the Mandible on 18F-FDG PET/CT. Asia Ocean J
Nucl Med Biol. 8:84–87. 2020.
|
|
13
|
Woolgar JA, Triantafyllou A, Ferlito A,
Devaney KO, Lewis JS Jr, Rinaldo A, Slootweg PJ and Barnes L:
Intraosseous carcinoma of the jaws: a clinicopathologic review.
Part III: Primary intraosseous squamous cell carcinoma. Head Neck.
35:906–909. 2013.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Wenguang X, Hao S, Xiaofeng Q, Zhiyong W,
Yufeng W, Qingang H and Wei H: Prognostic Factors of Primary
Intraosseous Squamous Cell Carcinoma (PIOSCC): A Retrospective
Review. PLoS One. 11(e0153646)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Suei Y, Tanimoto K, Taguchi A and Wada T:
Primary intraosseous carcinoma: Review of the literature and
diagnostic criteria. J Oral Maxillofac Surg. 52:580–583.
1994.PubMed/NCBI View Article : Google Scholar
|
|
16
|
De Lathouwer C and Verhest A: Malignant
primary intraosseous carcinoma of the mandible. Oral Surg Oral Med
Oral Pathol. 37:77–83. 1974.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Lo Muzio L, Mangini F, De Falco V,
Pennella A and Farronato G: Primary intraosseous carcinoma of the
mandible: A case report. Oral Oncol. 36:305–307. 2000.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lugakingira M, Pytynia K, Kolokythas A and
Miloro M: Primary intraosseous carcinoma of the mandible: Case
report and review of the literature. J Oral Maxillofac Surg.
68:2623–2629. 2010.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Kapoor V, McCook BM and Torok FS: An
introduction to PET-CT imaging. Radiographics. 24:523–543.
2004.PubMed/NCBI View Article : Google Scholar
|