Introduction
When an abnormality occurs during the course of
pregnancy, such as premature birth, the placenta is submitted for a
pathological examination to identify the underlying cause. In some
cases, malignant tumors are detected in the placenta. The placental
metastasis of maternal malignancy is very rare. Previous case
reports of metastatic tumors in the placenta included malignant
melanoma, breast cancer, lung cancer, hematological malignancies,
gastric cancer, and ovarian cancer (1,2).
Most gynecological malignancies diagnosed during pregnancy are
cervical and ovarian cancer (1).
Endometrial cancer is often associated with estrogen, and so mostly
occur in peri- or postmenopausal woman. However, endometrial cancer
occurs in 5% of women <40 years of age. Smoking, family history,
obesity and unstable menstruation are strong risk factors for
endometrial cancer in individuals that are <40 years old. It is
rare to observe endometrial cancer during or before pregnancy. Most
patients diagnosed with endometrial cancer during pregnancy are
first-trimester, which is attributable to spontaneous abortions by
dilatation and curettage (3,4). A
previous report has indicated that the symptoms of spontaneous
abortion are often genital bleeding, which may be caused by damage
of chorionic villi due to the the presence of endometrial cancer
(3). Endometrial cancer before
pregnancy adversely affects the intrauterine environment and
implantation. Therefore, it is very rare to be able to deliver a
surviving baby in a pregnancy where the mother is diagnosed with
endometrial cancer. In some cases, endometrial cancer can be
diagnosed postpartum. As a histopathological type, the proportion
of grade 1 to 2 endometrioid adenocarcinoma is high (5). To the best of our knowledge, the
placental metastasis of endometrial cancer has not yet been
reported. In pregnancies where the individual has cancer and in
nonpregnant patients, the former has a worse prognosis and worse
response to therapy (6).
Additionally, the diagnosis of cancer during pregnancy is often
delayed due to pregnancy-specific changes. For example, the breast
is well developed following hormonal changes during pregnancy, such
that the sensitivity of mammography decreases (6). Certain reports indicate that
pregnancy does not affect the prognosis of patients with
endometrial cancer; however, it is unclear how endometrial cancer
affects pregnancy or how pregnancy affects endometrial cancer
(5). We herein describe a case in
which a pathological examination of the placenta led to a diagnosis
of endometrial carcinoma.
Case presentation
Placental pathology of endometrial
carcinoma
A 34-year-old Japanese woman presented to a local
clinic with infertility. An examination at the clinic revealed no
thickening of the endometrium; therefore, the patient was treated
with clomiphene citrate, received gonadotropin therapy, and
underwent artificial insemination. However, she did not become
pregnant. One year later, she underwent frozen-thawed embryo
transfer with a hormone replacement therapy cycle regimen
(estradiol patch, vaginal progesterone 300 mg/day) and became
pregnant. The patient was referred to another hospital for an
epidural birth. Although the progression of the pregnancy was
uneventful, the patient presented to the hospital with scant
bleeding in the 21st (21+2) week of gestation. A shortened cervical
length and uterine contractions were detected. Therefore, the
patient was admitted to the hospital with a diagnosis of threatened
premature delivery and was administered ritodrine. The patient was
diagnosed with the premature rupture of membranes and transferred
to our hospital at 21 weeks and 6 days gestation. No obvious
abnormalities were observed in the fetus, placenta (attached to the
posterior wall of the uterus), or umbilical cord. Tocolytic agents
(ritodrine and magnesium sulfate) and prophylactic antibiotics were
administered. Labor pain occurred on the 23rd (23+3) week of
gestation, and a female fetus weighing 524 g was delivered
vaginally. Apgar scores at one and five minutes were two and seven,
and umbilical artery pH was 7.2. The placenta was 262 g with no
major macroscopic abnormalities. Since this was a preterm birth,
the placenta was submitted for a pathological examination, which
revealed metastatic adenocarcinoma (Expression of estrogen receptor
was observed, but clear cell carcinoma was suspected because
immunohistochemistry analysis showed positive for PAX8 and HNF1B;
the tumor was also negative for CD10, Glypican, AMACR and p53). No
significant inflammatory cell infiltration was noted in the
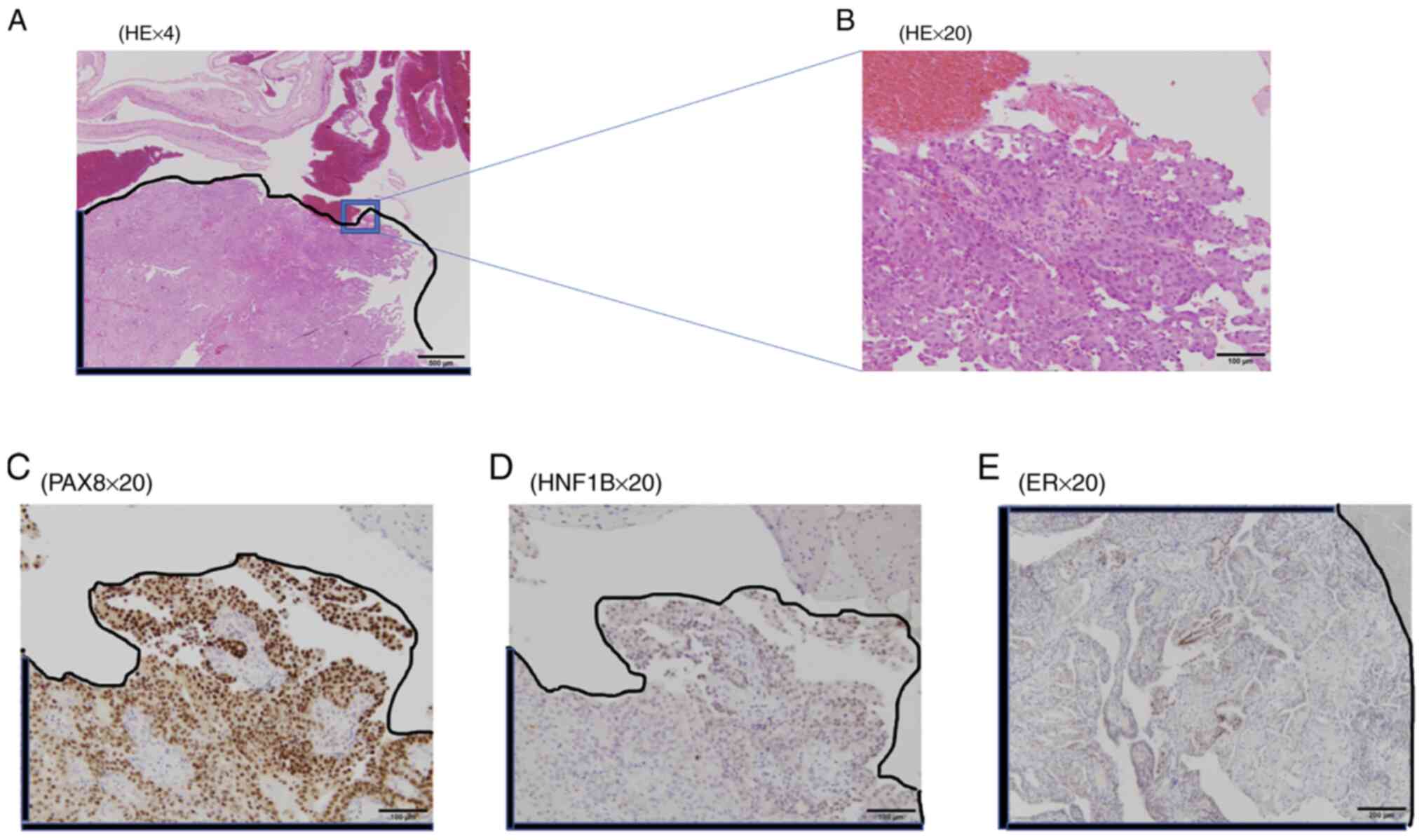
placenta or umbilical cord. (Fig.
1A-E).
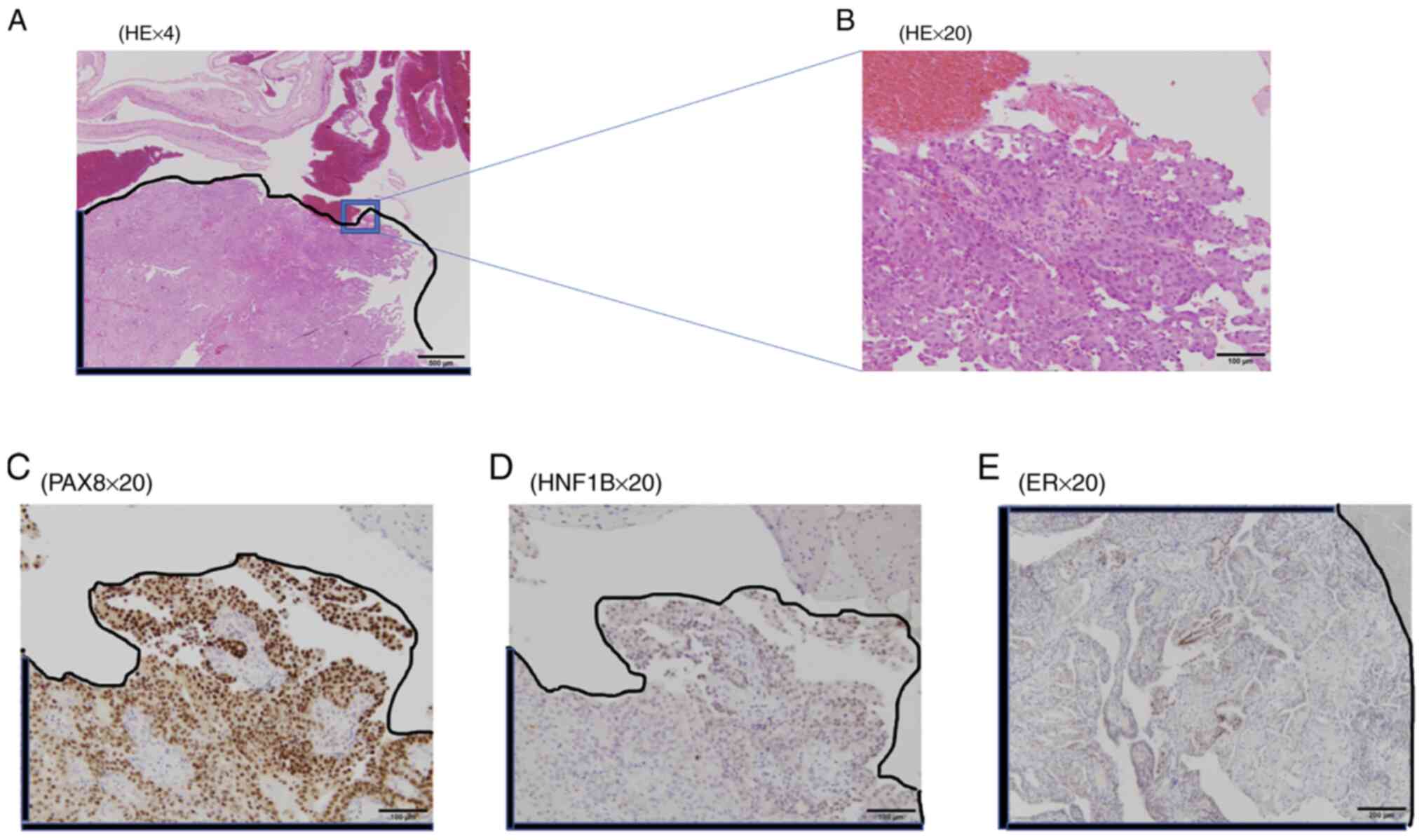 | Figure 1Histopathological findings of a
resected placenta specimen. The tumor site is indicated by a black
line. Microscopically, at (A) x4 and (B) x20 magnifications, a
10-mm neoplastic lesion in a section of the placenta exhibited
metastatic adenocarcinoma. The tumor grew with a solid and luminal
structure, and metastatic adenocarcinoma was suspected. Clear cell
carcinoma was additionally suspected as immunohistochemistry
analysis demonstrated that samples were positive for (C) PAX8 and
(D) HNF1B (magnification, x20). PAX8 demonstrated strong positive
staining in ~50% of the tumor. HNF1B was weakly positive in ~5% of
the tumor. The tumor was however negative for CD10, Glypican, AMACR
and p53. (E) ER demonstrated strong positive staining in ~10% of
the tumor (magnification, x20). HE, hematoxylin and eosin; PAX8,
paired box 8; HNF1B, hepatocyte nuclear factor 1β; ER, estrogen
receptor. |
Diagnosis of endometrial
carcinoma
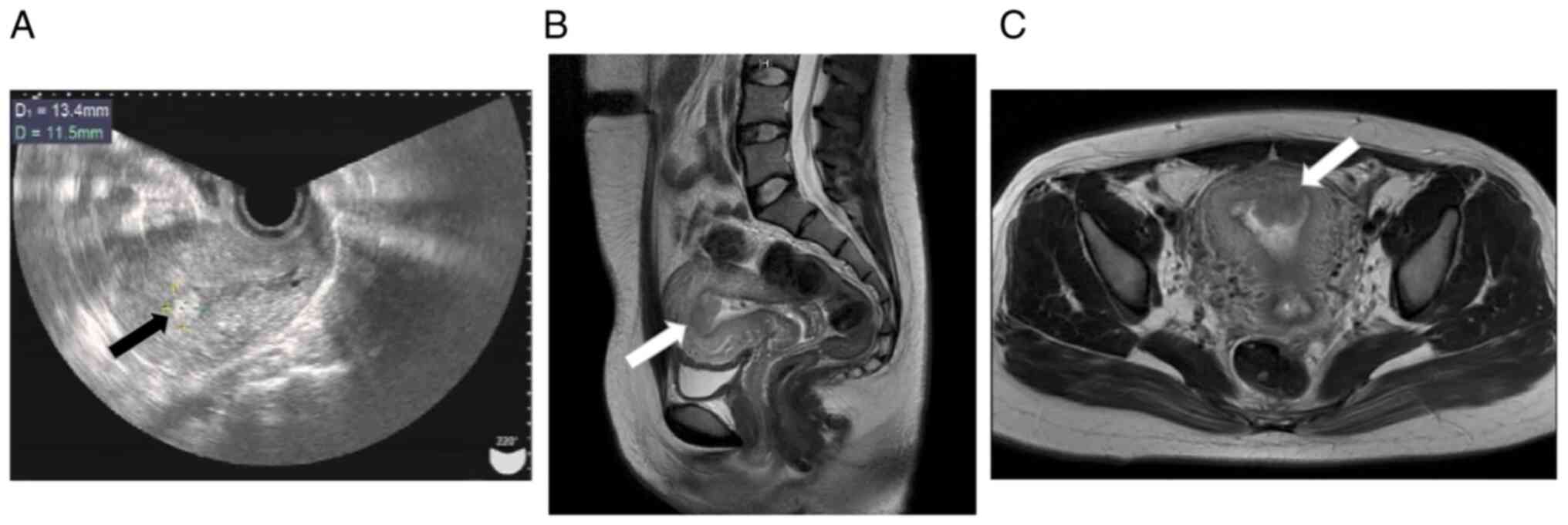
One month postpartum, a high echoic mass of 1.5 cm
was detected in the endometrial cavity by transvaginal
ultrasonography, and endometrial cancer was suspected. (Fig. 2A). Cytological findings of the
uterine cervix were negative for intraepithelial lesions and
malignancy, and endometrial cytology was also negative. Biopsy of
the lesion revealed adenocarcinoma, and the final diagnosis was
endometrial cancer. A 4-cm mass was detected in the endometrial
cavity by contrast-enhanced magnetic resonance imaging. (Fig. 2B and C) Contrast-enhanced computed tomography
did not show any distant metastasis, and tumor markers (CEA, CA125,
and CA19-9) were negative.
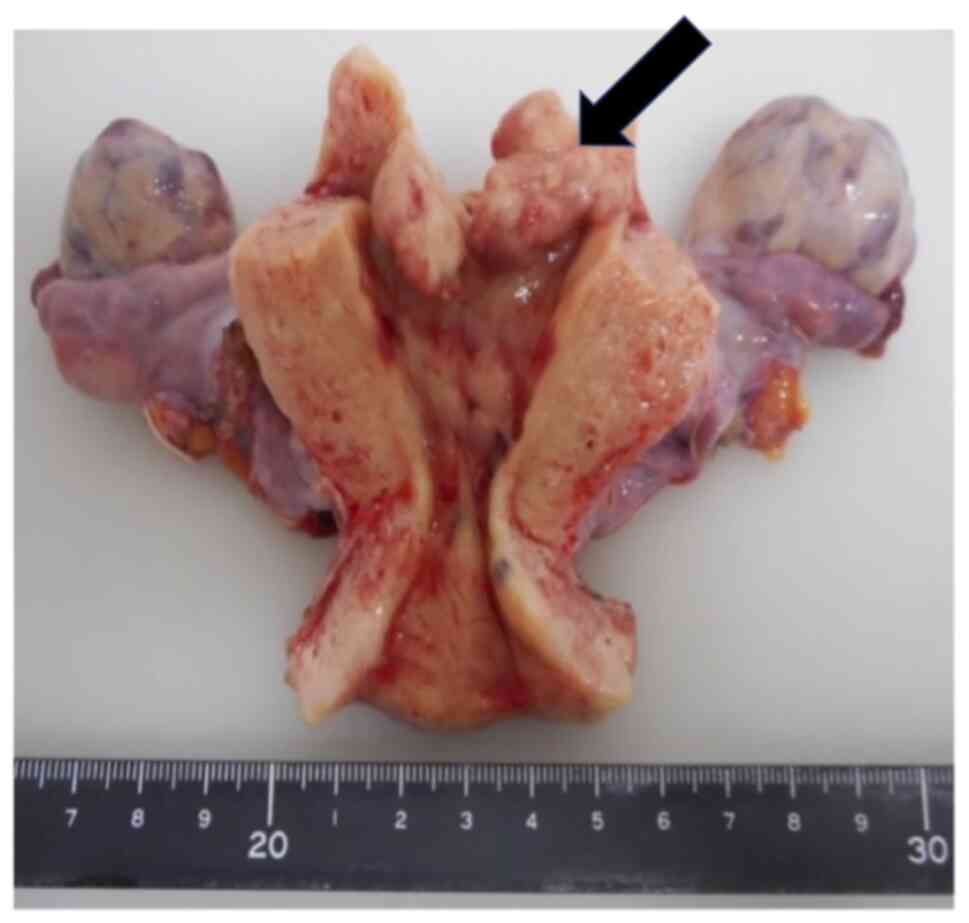
The patient was diagnosed with endometrial cancer
(stage I suspected), and underwent abdominal total hysterectomy,
bilateral salpingo-oophorectomy, partial omentectomy, and pelvic
lymph node dissection based on suspected clear cell carcinoma in
the preoperative diagnosis (intraoperative consultation,
endometrioid carcinoma, grade 2, invasion involving less than
one-half of the myometrium) (Fig.
3).
The postoperative diagnosis was endometrial cancer
stage 1A (pT1aN0M0, endometrioid carcinoma, grade 2, negative
peritoneal lavage cytology, positive lymphatic vessel invasion,
negative blood vessel invasion, and myometrium invasion of 3 mm
with endometrial thickness of 20 mm). There has been no evidence of
disease one year after surgery and the patient is being followed
up.
Discussion
The incidence of malignancy during pregnancy ranges
between 0.05 and 0.1% (1). Common
malignancies during pregnancy include melanoma, ovarian cancer,
cervical cancer, leukemia, and breast cancer, whereas endometrial
cancer is rare (2). In recent
years, the number of cases of endometrial cancer in patients
younger than 40 years and those with an advanced maternal age due
to assisted reproductive technology has been increasing. Therefore,
the rate of malignancy during pregnancy has also increased. A risk
factor for endometrial cancer is the excessive and unopposed
exposure of the endometrium to estrogen, such as obesity and
nulliparity; therefore, pregnancy is a protective factor. The
patient is overweight (Body Mass Index is 27.9 kg/m2)
and has had menstrual disorders since junior high school
student.
In the present case, endometrial cancer may have
been present before or during pregnancy. We identified dozen of
cases of endometrial carcinoma during pregnancy; however, more than
50% were detected at the time of dilatation and curettage for
first-trimester spontaneous abortions (3-5).
Other cases were diagnosed after childbirth. Although the reason
why endometrial cancer coexists with pregnancy currently remains
unknown, the partial resistance of the endometrium to progesterone
has been proposed (3,6). In most cases, the histopathology of
endometrial cancer during pregnancy is endometrioid carcinoma
(4,5). The present case became pregnant by
frozen-thawed embryo transfer with a hormone replacement therapy
cycle regimen; therefore, the intra-uterine concentration of
progesterone was high. A high progesterone status during pregnancy
may have suppressed the growth of endometrioid carcinoma. Since the
placenta was attached to the posterior wall of the uterine and
located at a different position to the site of cancer, the
pregnancy continued.
The underlying reason for the premature rupture of
membranes was inhibited uterine growth and increased intrauterine
pressure caused by cancer in the uterus. Previous cases of maternal
to placental metastasis included malignant melanoma, gastric
cancer, leukemia, breast cancer, lung cancer, and ovarian cancer
(7-9).
Furthermore, many cases of placental metastasis were advanced
cancers. To the best of our knowledge, the placental metastasis of
endometrial cancer has not yet been reported. A previous study
showed that placental metastasis occurred via blood vessels
(9). In the present case, the
placenta was closely located to the site of cancer in the
peripheral tissues, which allowed for its migration or attachment
to the placenta.
Metastasis to not only the placenta, but also to the
fetus may occur, and this may be attributed to the immature fetal
immune system (8). Therefore,
metastasis to the fetus also needs to be considered. At this time,
it does not recognize obvious abnormalities in the pelvis by
ultrasonography, but we will continue to follow up.
Lynch syndrome accounts for 2% of all endometrial
cancer cases (10). Since our
patient was young and has a family history of rectal cancer
(father), it is important to consider the possible diagnosis of
Lynch syndrome. Follow-up assessments are needed for both the
patient and the child. However, NGS method was not performed due to
lack of her consent; Therefore, we plan to begin colorectal
surveillance with the possibility of Lynch syndrome in mind.
In previous cases of placental metastasis,
metastatic lesions were not observed macroscopically, similar to
the present case.
In conclusion, the study confirms the need to
perform a histopathological examination of the placenta in the
abnormal course of pregnancy, especially in all cancers coexisting
with pregnancy and shows that careful observation of the potential
development of hormone-dependent tumors during assisted
reproductive procedures is needed.
Acknowledgements
The authors would like to thank Dr Takumi Kakimoto
(Department of Pathology, Tokushima University Hospital) for
conducting pathological evaluations.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
requests.
Authors' contributions
MN, ES, TK, MI, TI and TM were involved in the
conception and design of the current study. TM wrote the
manuscript. MN, MI and TI supervised the study. TM and MN confirm
the authenticity of all the raw data. All authors have read and
approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Institutional
Review Board of The University of Tokushima Hospital. Written
informed consent was obtained from the patient.
Patient consent for publication
Consent for publication was obtained from the
patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Skrzypczyk-Ostaszewicz A and Rubach M:
Gynaecological cancers coexisting with pregnancy-a literature
review. Contemp Oncol (Pozn). 20:193–198. 2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pavlidis N, Peccatori F, Lofts F and Greco
AF: Cancer of unknown primary during pregnancy: An exceptionally
rare coexistence. Anticancer Res. 35:575–579. 2015.PubMed/NCBI
|
|
3
|
Zhou F, Qian Z, Li Y, Qin J and Huang L:
Endometrial adenocarcinoma in spontaneous abortion: Two cases and
review of the literature. Int J Clin Exp Med. 8:8230–8233.
2015.PubMed/NCBI
|
|
4
|
Saciragic L, Ball CG, Islam S and
Fung-Kee-Fung M: Incidental endometrial carcinoma diagnosed at
first trimester pregnancy loss: A case report. J Obstet Gynaecol
Can. 36:1010–1013. 2014.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Shiomi M, Matsuzaki S, Kobayashi E, Hara
T, Nakagawa S, Takiguchi T, Mimura K, Ueda Y, Tomimatsu T and
Kimura T: Endometrial carcinoma in a gravid uterus: A case report
and literature review. BMC Pregnancy Childbirth.
19(425)2019.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Hoellen F, Reibke R, Hornemann K, Thill M,
Luedders DW, Kelling K, Hornemann A and Bohlmann MK: Cancer in
pregnancy. Part I: Basic diagnostic and therapeutic principles and
treatment of gynecological malignancies. Arch Gynecol Obset.
285:195–205. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Altman JF, Lowe L, Redman B, Esper P,
Schwartz JL, Johnson TM and Haefner KH: Placental metastasis of
maternal melanoma. J Am Acad Dermatol. 49:1150–1154.
2003.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Oga S, Hachisuga M, Hidaka N, Fujita Y,
Tomonobe H, Yamamoto HY and Kato K: Gastric cancer during pregnancy
with placental involvement: Case report and review of published
works. Obstet Gynecol Sci. 62:357–361. 2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Honda M, Yamada M, Kumasawa T, Samejima T,
Satoh H and Sugimoto M: Recurrence of ovarian cancer with placental
metastasis: A case report. Case Rep Oncol. 10:824–831.
2017.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pellat A, Netter J, Perkins G, Cohen R,
Coulet F, Parc Y, Svrcek M, Duval A and André T: Lynch syndrome:
What is new? Bull Cancer. 106:647–655. 2019.PubMed/NCBI View Article : Google Scholar : (In French).
|