Introduction
Primary testicular lymphoma (PTL) is an uncommon and
aggressive form of extra-nodal non-Hodgkin's lymphoma (NHL),
accounting for 1-2% of all NHL cases in patients aged >60 years
(1). The most common histological
subtype is the diffuse large B-cell lymphoma (DLBCL), which is
characterized by a high aggressiveness, rapid growing mass and
extranodal tropism, comprising a bilateral involvement in 6-10% of
cases (2). Typical clinical
manifestations include the presence of a firm and painless
testicular mass, although orchitis-like symptoms could be present.
In addition, despite non-disease-specific, hydrocele is observed in
43% of patients with primary and secondary testicular lymphoma
(1,3). Despite PTL involves testes only at
the beginning of the disease, the involvement of other sites at the
time of diagnosis is common, in particular central nervous system
(CNS) skin, lung and pleura (4).
On echotomography, PTL is indistinguishable from other neoplastic
and non-neoplastic lesions (5). As
result, diagnosis is obtained via histological confirmation
post-orchiectomy, which permits the staging of the disease and the
subsequent therapy choice (6).
Case report
A 54-year-old patient presented to our attention at
the Hospital ‘Sacro Cuore di Gesù’ Fatebenefratelli (Benevento,
Italy) in October 2021, complaining severe erectile dysfunction
(International Index of Erectile Function questionnaire score
<7) in addition to a bilateral and rapid increase in volume and
consistency of testes, in absence of painful manifestations. Other
non-urological symptoms included gingivitis, mastoiditis, headache
and dysgeusia. No recent traumatic or septic issues were reported
in the anamnesis. Among comorbidities, patient suffered from
hypertension and gastroesophageal reflux disease (GERD), which
however was in treatment with amlodipine 10 mg and Omeprazole 40 mg
per day. The patient was negative for Hepatitis B and C Viruses
(HBV and HCV) as well as Human Immunodeficiency Virus (HIV).
Physical examination excluded hydrocele, showing a significant
increase of both testis volume, with a wooden consistency and
immobility compared to the scrotal plane. Ultrasound scan (US)
examination confirmed the increased size of testes, revealing a
completely subverted structure due to the presence of coarse and
confluent hypo-echogenic areas, enhancing at the colour-Doppler
modality. Blood samples were obtained, reporting a mild
hypotestosteronaemia (179 ng/dl, normal values 350-890 ng/dl) and
increased LDH (348 IU/l, normal values 80-300 IU/l), while
alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA) and human
chorionic gonadotropin (hCG) were within normal ranges (4.13 ng/ml,
4.34 ng/ml and 2.1 mIU/ml, respectively; normal values: <6
ng/ml, <5 ng/ml and <5 mIU/ml, respectively). Regarding blood
count, renal and liver function, the patient reported no pathologic
values with 8.16x103/µl white blood cells,
4.55x106/µl red blood cells, 13.8 g/dl of haemoglobin
and 225x103/µl platelets; creatinine was 0.96 mg/dl
while aspartate aminotransferase (AST) and alanine aminotransferase
(ALT) were 16 U/l and 26 U/l, respectively. Finally, uric acid was
4.7 mg/dl (Table I). According to
physical and US examinations, the patient underwent a bilateral
radical orchiectomy, as indicated by the European Association of
Urology guidelines on testicular cancer, due to the evident tumoral
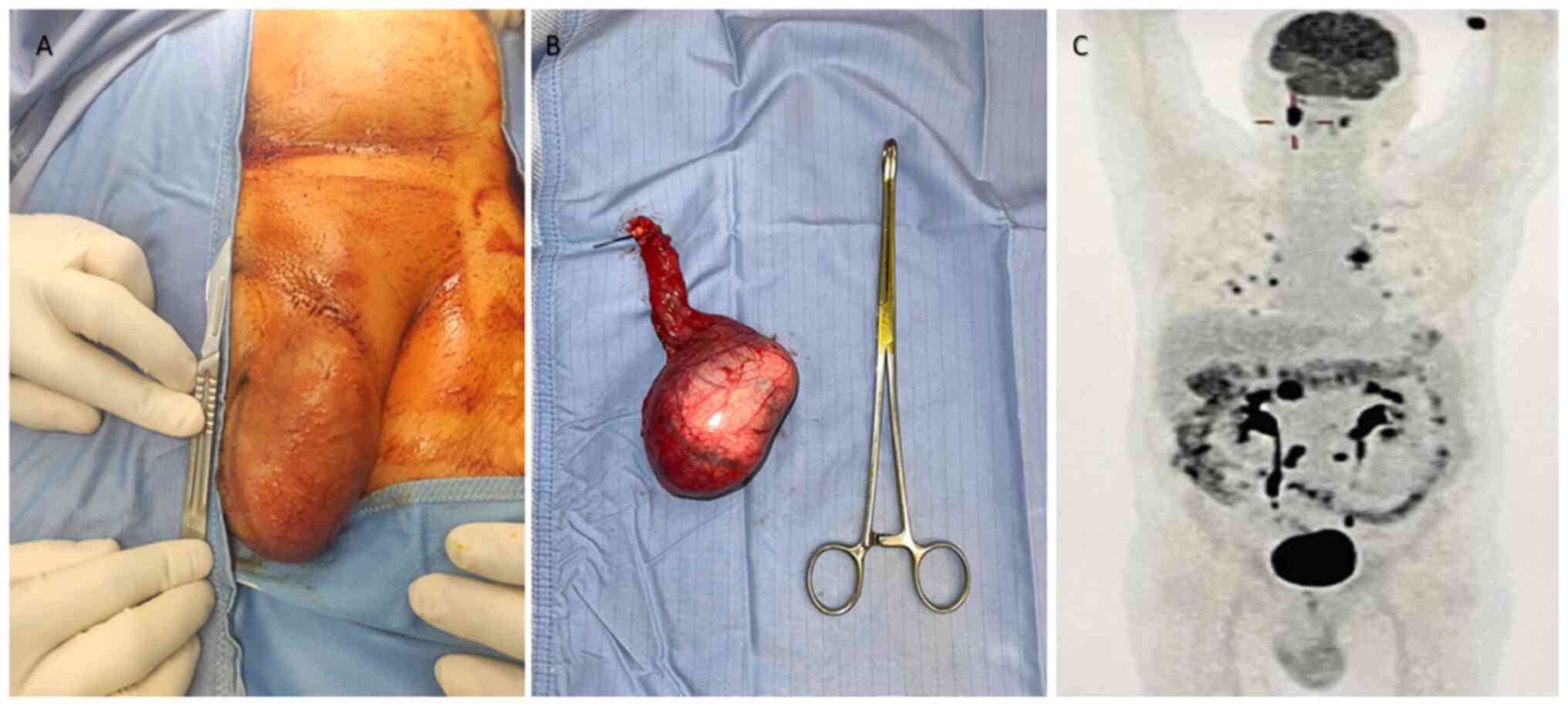
aspect of the testicular masses (7,8). At
the surgical table, testes were measured (left testis 10x7x5 cm;
right testis 12x8x7 cm) and examined, showing parenchyma completely
replaced by whitish-yellow plurinodular and confluent formations
(Fig. 1). The subsequent
histopathological analysis reported the presence of medium and
large size multilobed lymphoid cells, with poor cytoplasm and
occasional eosinophilic central nucleoli. No infiltration or
congestion of the cord was reported bilaterally. The
immunophenotypic profiling revealed a lymphoid proliferation CD
20+, Bcl +/-, CD3- and CD5-, consistent with medium-large cells
B-derived non-Hodgkin Lymphoma diagnosis. 18F-FDG PET/CT scan,
which was performed in the postoperative staging of the disease,
showed multiple avid lesions (>10) located at lungs (SUV max
15.1), pleura (SUV max 11.6), pancreatic head (SUV max 19.4). Nodal
involvement comprehended caval (SUV max 4.1), celiac (SUV max 2.3),
aortic (SUV max 16.9) and renal (SUV max 15.4) lymph nodes.
Finally, several hyperaccumulations were found in the mandibular
(SUV max 18.4) and maxillary (SUV max 5.7) region, bilaterally. A
probably reactive hyperaccumulation was found in surgical locations
(scrotal and inguinal region) (SUV max 4.4). The patient was
subsequently addressed to the haematologist and oncologist for
further evaluations. Lumbar puncture was performed to exclude CNS
involvement. Skin involvement, after dermatological consultation,
was excluded as well, while testosterone replacement therapy was
administered with 1,000 mg of intramuscular testosterone
undecanoate every 12 weeks.
 | Table IBlood sample values of the patient
before surgery. |
Table I
Blood sample values of the patient
before surgery.
| Value | Result | Normal range |
|---|
| WBC,
x103/µl | 8.16 | 4.8-10.8 |
| RBC,
x106/µl | 4.55 | 4.2-5 |
| Haemoglobin,
g/dl | 13.8 | 12-17.5 |
| Platelets,
x103/µl | 225 | 130-400 |
| Creatinine,
mg/dl | 0.96 | 0.72-1.25 |
| AST, U/l | 16 | 0-34 |
| ALT, U/l | 26 | 0-55 |
| Uric acid, mg/dl | 4.7 | 3.4-7 |
| LDH, IU/l | 348 | 80-300 |
| AFP, ng/ml | 4.13 | <6 |
| CEA, ng/ml | 4.34 | <5 |
| hCG, mIU/ml | 2.1 | <5 |
| Testosterone,
ng/dl | 179 | 350-890 |
According to the Lugano Modification of the Ann
Arbor staging system, the disease stage was estimated to be IV-E,
with a Karnofsky performance status of 100% and ECOG (Eastern
Cooperative Oncology Group) grade 0(9). Deauville criteria score was 2 while
International Prognostic Index (IPI) for DLBCL adjusted for age was
2.
The patient underwent to the R-CHOP protocol
(rituximab 375 mg/m2 plus cyclophosphamide 750
mg/m2, doxorubicin 50 mg/m2, vincristine 1.4
mg/m2 and prednisone 40 mg/m2) every 21 days
for six cycles, as well as 2 cycles of intrathecal methotrexate for
CNS prophylaxis. The decision to perform a high-dose chemotherapy
and/or haematopoietic stem cell transplantation is still under
consideration. The patient is still in follow up, with a current
observation time of 5 months, and remain in stable condition,
pending subsequent re-evaluation with PET/CT scan.
Discussion
PTL is a rare and extremely aggressive disease,
accounting for an annual incidence of 0.26 cases per 100,000
person-years and a median age of presentation of 65 years (10). The staging is similar to other
forms of aggressive NHL and is based on the Ann Arbor system,
requiring PET/CT with the addition of CNS staging. Considering the
particular tropism of this disease for the skin, a thorough
examination is required. Among adverse prognostic factors are
included: age >70 years, B symptoms (fever, drenching night
sweats and loss of >10% of body weight in 6 months), >1
extranodal site, tumour diameter >10 cm and raised LDH (11). Interestingly, despite the large
testicles masses reported in our patient, no B symptoms were
reported in our case. As reported in the literature, 5-year
progression-free survival (PFS) and overall survival (OS) are,
respectively, 59.3 and 85%, for patients who underwent a combined
protocol including R-CHOP (the treatment of choice for III-E and
IV-E Ann Arbor stages), intrathecal chemotherapy and scrotal
radiotherapy (1,11). In particular, prophylactic
intrathecal chemotherapy and scrotal radiotherapy (in cases of
monolateral disease) are indicated in 10-14% of patients considered
at high risk (12). Although the
approval of rituximab for PTL has been saluted as a potential
favourable therapeutic addition, the impact on the outcomes remains
unclear (13). Few other similar
and recent cases are reported in the literature: Yan et al
(14) reported the case of a
63-year-old patient with a CNS relapse after a successful treatment
of an early monolateral PTL; Sia et al (15) reported the case of a younger
patient (56-year old) with a right testicular PTL who underwent to
scrotal radiotherapy after the R-CHOP protocol and intrathecal
methotrexate; Sadiq et al (16) reported the case of a 47-year old
patients with left PTL; finally Batista and Safriadi (17) reported the case of a bilateral PTL
in a 48-year old male, which was treated similarly to our case.
Albeit a relatively low testosterone level is reported, PTL is not
associated with hypotestosteronaemia, albeit the subsequent
treatment could impair the (residual) testicular function. In our
case, the bilateral orchiectomy required the administration of
testosterone replacement therapy. Few limitations have to be
reported in our study. Firstly, we did not have the genetic
analysis of the patient; secondly, the follow-up is still ongoing
and further clinical decision could be further made.
In conclusion, PTL is a rare and aggressive disease,
characterized by a poor prognosis. Despite being traditionally
reported in patients over 60 years, as reported in our case, it
could be seen also in younger patients, with an aggressive and
metastatic and bilateral presentation at the time of the diagnosis.
Its rare incidence and the peculiar behaviour of the malignancy
have made difficult a standardized approach. Considering the
particular tropism to CNS, skin and contralateral testis, a careful
and thorough patient's evaluation is required, utilizing a
multidisciplinary approach in order to overcome the difficulties of
this disease.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
DDD, BB, LN, FC and VV wrote and reviewed the
manuscript. DDD, ARZ, DDB, GN and VV performed surgical treatment
and related post-operative follow up of the patient. ARZ, GN, DDB,
PR and LDL supervised the study. BB, LN, FC, PR, LDL, IS, CA, LC
and GMF conceived the study, collected the data and verified the
authenticity of all the raw data. All authors read and approved the
final manuscript.
Ethics approval and consent to
participate
Written informed consent for participation was
obtained from the patient. Ethics approval was not required due the
retrospective nature of the work and the absence of procedure
performed outside the normal clinical practice.
Patient consent for publication
Written informed consent for publication of the case
and related images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Cheah CY, Wirth A and Seymour JF: Primary
testicular lymphoma. Blood. 123:486–493. 2014.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Li S, Young KH and Medeiros LJ: Diffuse
large B-cell lymphoma. Pathology. 50:74–87. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Spaziani E, Di Filippo A, Francioni P,
Fiorini F, Di Costanzo R, Ciaschi V, Spaziani M, De Cesare A and
Picchio M: Bilateral hydrocele. Uncommon clinical presentation of
primary testicular lymphoma in the elderly. Clin Ter.
168:e136–e139. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ahmad SS, Idris SF, Follows GA and
Williams MV: Primary testicular lymphoma. Clin Oncol (R Coll
Radiol). 24:358–365. 2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bertolotto M, Derchi LE, Secil M, Dogra V,
Sidhu PS, Clements R, Freeman S, Grenier N, Mannelli L, Ramchandani
P, et al: Grayscale and color Doppler features of testicular
lymphoma. J Ultrasound Med. 34:1139–1145. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wang Y, Li ZM, Huang JJ, Xia Y, Li H, Li
YJ, Zhu YJ, Zhao W, Xia XY, Wei WX, et al: Three prognostic factors
influence clinical outcomes of primary testicular lymphoma. Tumour
Biol. 34:55–63. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Heidenreich A, Paffenholz P, Nestler T and
Pfister D: European association of urology guidelines on testis
cancer: Important take home messages. Eur Urol Focus. 5:742–744.
2019.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Laguna MP, Pizzocaro G, Klepp O, Algaba F,
Kisbenedek L and Leiva O: EAU Working Group on Oncological Urology.
EAU guidelines on testicular cancer. Eur Urol. 40:102–110.
2001.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cheson BD, Fisher RI, Barrington SF,
Cavalli F, Schwartz LH, Zucca E and Lister TA: Alliance,
Australasian Leukaemia and Lymphoma Group; Eastern Cooperative
Oncology Group; European Mantle Cell Lymphoma Consortium. et al:
Recommendations for initial evaluation, staging, and response
assessment of Hodgkin and non-Hodgkin lymphoma: The Lugano
classification. J Clin Oncol. 32:3059–3068. 2014.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Chen B, Cao DH, Lai L, Guo JB, Chen ZY,
Huang Y, Qiu S, Lin TH, Gou Y, Ma N, et al: Adult primary
testicular lymphoma: Clinical features and survival in a series of
patients treated at a high-volume institution in China. BMC Cancer.
20(220)2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ma RZ, Tian L, Tao LY, He HY, Li M, Lu M,
Ma LL, Jiang H and Lu J: The survival and prognostic factors of
primary testicular lymphoma: Two-decade single-center experience.
Asian J Androl. 20:615–620. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Kim J, Yoon DH, Park I, Kim S, Park JS,
Lee SW, Huh J, Park CS and Suh C: Treatment of primary testicular
diffuse large B cell lymphoma without prophylactic intrathecal
chemotherapy: A single center experience. Blood Res. 49:170–176.
2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kridel R, Telio D, Villa D, Sehn LH,
Gerrie AS, Shenkier T, Klasa R, Slack GW, Tan K, Gascoyne RD, et
al: Diffuse large B-cell lymphoma with testicular involvement:
Outcome and risk of CNS relapse in the rituximab era. Br J
Haematol. 176:210–221. 2017.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yan Z, Yao S, Wang Y, Liu Y and Yao Z:
Primary testicular lymphoma with central nervous system relapse was
successfully treated by a chemo-free regimen: A case report and
literature review. Cancer Manag Res. 13:9489–9500. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sia N, Chekrine T, Bourhafour M, Ouadii K,
Bouchbika Z, Benchakroun N, Jouhadi H, Tawfiq N, Benider A,
Marnissi F, et al: Primary testicular lymphoma: A case report and
review of the literature. J Cancer Ther. 13:145–154. 2022.
|
|
16
|
Sadiq M, Ahmad I, Shuja J, Khan ZU and
Ahmad K: Primary testicular diffuse large B-cell lymphoma: A case
report. Egyp J Basic Appl Sci. 4:358–360. 2017.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Batista B and Safriadi F: Bilateral
primary testicular diffuse large B-cell lymphoma: A case report. J
Surg Case Rep. 2021(rjab431)2021.PubMed/NCBI View Article : Google Scholar
|