Introduction
Bone metastases occur in 60-84% of metastatic
cancers and are the most common cause of cancer-related pain
(1). Primary tumors that are
responsible for the majority of cases are cancers of prostate,
kidney, thyroid gland, lung and breast (2). Usually, bone metastases are
associated with incurable diseases with significant morbidity and
severe pain (3). In patients with
bone metastases, radiotherapy has appeared to be efficient in
palliation of pain (4). Local
field radiotherapy is a safe option for relieving pain caused by
localized bone metastases. All fractionation schemes: 30 Gy in 10
fractions, 20 Gy in 5 fraction and 8 Gy in single fraction are
considered effective and widely accepted (5,6). In
oligometastatic setting of the disease, defined as single or few
(up to five) metastases (7),
stereotactic body radiotherapy (SBRT) may be considered (5).
Multiple locations of painful bone metastases occur
in many patients. Half-body irradiation (HBI) is an alternative to
local field radiotherapy. It shortens treatment time and its pain
palliation is effective (8-10).
Historically, HBI was categorized into upper HBI (UHBI), lower HBI
(LHBI) and mid-body irradiation (MBI) (11). For UHBI, the inferior margin of the
radiation field corresponded to the bottom of the 4th lumbar
vertebra. For LHBI, the superior margin corresponded to the
inferior one for UHBI, while the inferior margin extended to
mid-ankles and MBI that consisted of a field that reached from the
top of the diaphragm to the bottom of the obturator foramina
(11). Such treatment is
advantageous as it allows to deal with multiple lesions
simultaneously within a short period of time. On the other hand,
wide field radiotherapy leads to frequent irradiation of healthy
tissue and therefore may cause acute and long-term toxicity.
Nowadays, more conformal techniques, such as
volumetric modulated arc therapy (VMAT) or tomotherapy with 3D
planning, are available, which allows to irradiate smaller fields
and avoid unaffected bones. Thus, it helps to reduce doses in
organs at risk and may decrease the incidence of acute toxicity
(8). The safest and most effective
single HBI doses are 6 Gy for UHBI and 8 Gy for both LHBI and MBI
(12). Lately, fractionated
schemes: 15 Gy/5 fractions/5 days, 8 Gy/2 fractions/1 day and 12
Gy/4 fractions/2 days have been reported to relieve pain in 91% of
cases (13). A response to
treatment is usually prompt and manifests itself with relieved
pain, observed as early as within 48 h following the initiation of
the treatment (11,12). In UHBI, the main organs at risk are
lungs affected by post-radiation pneumonitis, especially when the
dose absorbed to a lung was above 6 Gy (14). Irradiation of great volume of the
digestive system leads to nausea, vomiting and diarrhea, being the
most common acute complications of HBI (4). Hospitalization may be required for
hydration and administration of antiemetics. Myelosuppression is
another common HBI-induced toxicity. Patients undergoing HBI
demonstrate more hematologic toxicity in comparison to those who
undergo a local field treatment alone, with approximately 10% of
patients presenting leukopenia, anemia or thrombocytopenia
(15).
Although HBI radiotherapy utilizes modern techniques
which aim at reducing doses to organs at risk, there are only
limited data regarding the effectiveness and side-effects of such
treatment. The objective of our study was to evaluate efficiency of
upper and lower half body irradiation (UHBI, LHBI) in reduction of
pain in patients with painful multiple bone metastases, treated
with VMAT HBI.
Materials and methods
Study population
Our retrospective analysis covered the period from
July 2018 to July 2020. The study group included 22 patients
treated with HBI in Regional Cancer Center, Copernicus Memorial
Hospital of Lodz (Łódź, Poland). All patients were referred to
radiotherapy department with multiple painful bone metastases in
cases where pain could not be controlled with analgesics drugs and
were qualified to palliative radiotherapy. Patients were qualified
to HBI treatment when pain was present in more than 5 localizations
and standard palliative treatment could not be performed quickly
and there was no further systemic therapy planned. In most cases of
patients that were qualified to HBI, number of bone metastases was
not given in imaging results, and were described as multiple or
uncountable. All the patients have been admitted to hospital one
day prior to the treatment. Before hospitalization, all the
patients have undergone computed tomography (CT) scanning for the
elective treatment. Upon admission, the patients rated pain in 11
points (0-10) according to the verbal numeric pain score (VNPS).
The patients were also asked to rate the maximum and average pain
experienced in the last month period. All patients provided written
informed consent to undergo the treatment.
Treatment
Hospitalization lasted 3 days, and the treatment
procedure was performed on the second day. According to the
protocol used in our center, inclusion criteria for HBI were the
following: diagnosed cancer with multiple, symptomatic bone
metastases, ECOG PS 0-4, WBC ≥3,000/µl, PLT ≥100,000/µl, Hgb level
above 8.5 g/dl and submission of a written informed consent to
undergo the treatment. The patients were prehydrated intravenously.
On the day of irradiation, the patients were administrated steroids
(dexamethasone 8 mg i.v.), antiemetics (metoclopramide 10 mg i.m.),
and additionally, anti-diarrheal drugs (loperamide 2 mg p.o. every
8 h) when LHBI was performed. The treatment procedure was conducted
in the supine position, with hands above the head when UHBI was
planned.
Clinical target volume (CTV) was delineated by a
radiation oncologist, comprising the whole bone tissue extending
from lumbar vertebrae to cervical vertebrae, depending on the
metastases localized most superiorly and most inferiorly.
CTV varied from C2-C7 to L1-L4 and was evaluated by
the attending physician. The skull was not delineated if there were
no metastases. In LHBI, borders extended from the mid-length of the
femur to the most inferiorly located metastasis if there were no
more metastases in lower extremities. With regards to UHBI, the
border extended as far as L1-L4 vertebrae, depending on how much
superiorly the metastasis was localized. The patients who were
qualified for both UHBI and LHBI, received simultaneous planning
and treatment with at least a two-week interval. Planning target
volume (PTV) was created by adding a four-five mm margin to CTV.
Organs at risk that were delineated included: the heart, lungs,
kidneys, spinal cord and liver in UHBI and kidneys, rectum, spinal
cord and bladder in LHBI. The dose prescribed to PTV was 6 Gy in
one fraction in UHBI and 8 Gy in one fraction in LHBI. When both
UHBI and LHBI were planned, the dose of LHBI changed and ranged
from 6 to 8 Gy, depending on the decision of the attending
physician.
All patients' plans were prepared with the use of
the VMAT technique. Aimed dosimetry constraints were at least 90%
of the prescribed dose covering the whole PTV and organs at risk
with mean doses smaller than 2.5 Gy for kidneys, 3 Gy for the
rectum, bladder and heart, 4 Gy for the liver and 4 Gy for lungs.
Image verification with kV images was performed before each arc.
Plans for all 22 patients were subject to a dosimetric
analysis.
Follow-up
During a follow-up visit one month after finishing
the treatment, the patients were asked once again to rate the pain
on the day of the visit as well as the maximum and average pain
experienced within the last month. Of 22 patients, 3 were lost to
the follow-up, so the influence of HBI radiotherapy on severity of
pain was assessed on the base of data obtained from 19 patients.
Characteristics of the study group are presented in Table I. De-escalation of pain on the day
of interview, manifesting itself with the value of 0-1 in the VNPS
Scale was considered a complete response, whereas relieved pain,
characterized with at least 2 points less than before the
treatment, was regarded as a partial response.
 | Table ICharacteristics of the study
group. |
Table I
Characteristics of the study
group.
| Characteristic | Value |
|---|
| Median age at time of
treatment, years | 68 (IQR, 61-75) |
| Sex | |
|
Female | 7 (37%) |
|
Male | 12 (63%) |
| Localization of
primary tumor | |
|
Prostate | 10 (53%) |
|
Breast | 7 (37%) |
|
Bladder | 1 (5%) |
|
Unknown
primary | 1 (5%) |
| Treatment
performed | |
|
UHBI | 8 (42%) |
|
LHBI | 5 (26%) |
|
UHBI +
LHBI | 6 (32%) |
| ECOG performance
status | |
|
0-1 | 7 (37%) |
|
2-3 | 12 (63%) |
Statistical analysis
All statistical analyses were performed using
Statistica 13.1 software (Statsoft). The Wilcoxon signed-rank test
was used to compare VNPS before and after the treatment in the
whole group of patients. P<0.05 was considered to indicate a
statistically significant difference.
Results
Dosimetric analysis
Thirteen UHBI plans were prepared: 6 of patients
were planned for UHBI alone and 7 were planned for both UHBI and
LHBI for which the total number of both plans was created to assess
doses in PTVs and OARs, before implementing the treatment. All
patients received the dose of 6 Gy prescribed to UHBI PTV volume.
Plans consisted of 6 arcs in six patients, 5 arcs in two patients,
4 arcs in four patients and 3 arcs for one patient. The mean
minimum absorbed dose that covered 90% of the PTV volume (D90) was
5.89±0.33 Gy and the mean minimum absorbed dose that covered 95% of
the PTV volume (D95) was 5.68±0.21 Gy. The mean dose in PTV was
6.08±0.09 Gy with the mean volume that absorbed 90% of the
prescribed dose (5.4 Gy)-V90 of 98.30±2.20%. Lungs were the main
organs at risk taken into account during an audit of UHBI treatment
plans. The mean doses administered to the left and right lungs were
4.09±0.47 Gy and 4.02±0.46 Gy, respectively. Other OARs that were
delineated and in which the mean dose was checked included: the
spinal cord with the mean dose of 5.79±0.94 Gy, the liver with the
mean dose of 3.69±0.72 Gy and the heart with the mean dose of
2.50±0.70 Gy.
LHBI plans were prepared for 16 patients: 9 were
qualified for LHBI alone and 7 were qualified for sequential
treatment with UHBI and LHBI for which the total number of both
plans was created. Eleven patients were prescribed a dose of 8 Gy,
3 patients-a dose of 6 Gy and 2 patients-a dose of 7 Gy prescribed
to LHBI PTV. A dosimetric analysis in the homogenous group of 11
plans with a prescribed dose of 8 Gy was conducted. The plans
consisted of 6 arcs in two patients, 5 arcs in two patients, 4 arcs
in two patients and 3 arcs in five patients. The mean D90 was
7.77±0.16 Gy and D95 was 7.64±0.25 Gy. The mean dose prescribed to
PTV was 8.04±0.09 Gy with the mean volume that absorbed 90% of the
prescribed dose (7.2 Gy)-V90 of 99.51±0.61%. The rectum, spinal
cord and urinary bladder were organs at risk, taken into account
during an audit of LHBI treatment plans. The mean doses applied to
the rectum, spinal cord and urinary bladder were respectively:
3.41±0.95, 4.51±1.93, and 3.80±0.96 Gy.
Pain palliation
The median age of 19 patients included in the
analysis was 68 (IQR 61-75) years. Primary tumors included prostate
cancer diagnosed in 10 cases, breast cancer diagnosed in 7 cases,
and bladder cancer detected in 1 case. An primary tumor of the
unknown origin was diagnosed in 1 case. Eight patients were treated
with LHBI, 5 patients-with UHBI and 6 patients-with both UHBI and
LHBI (Table I).
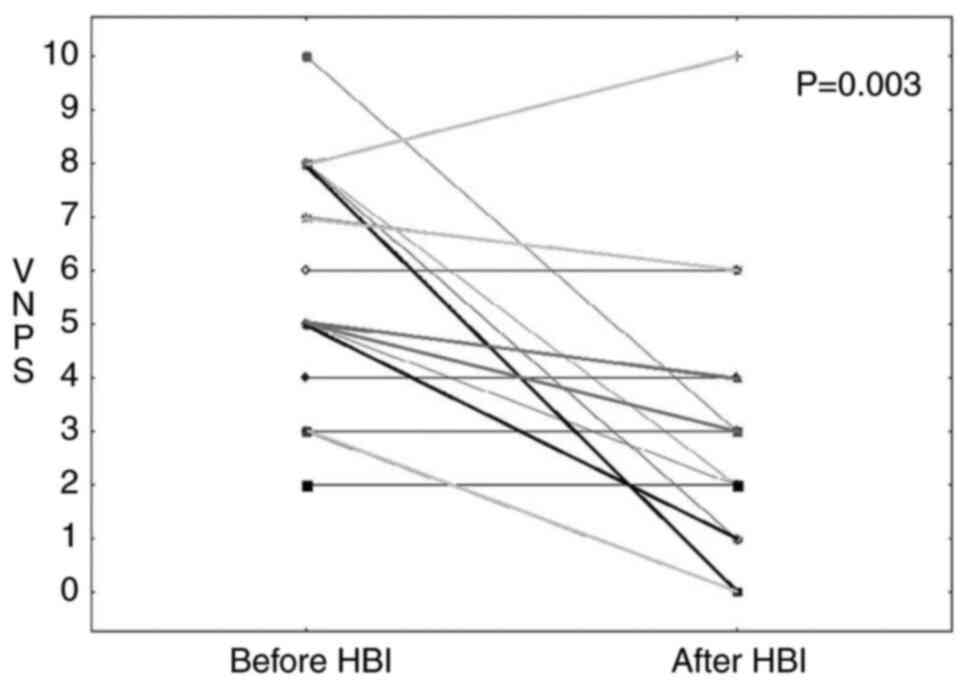
The median pain, measured in the VNPS on the day
prior to the treatment was 5 (IQR 3-8) and 3 (IQR 1-4) on the day
of the follow-up visit (P=0.003) (Fig.
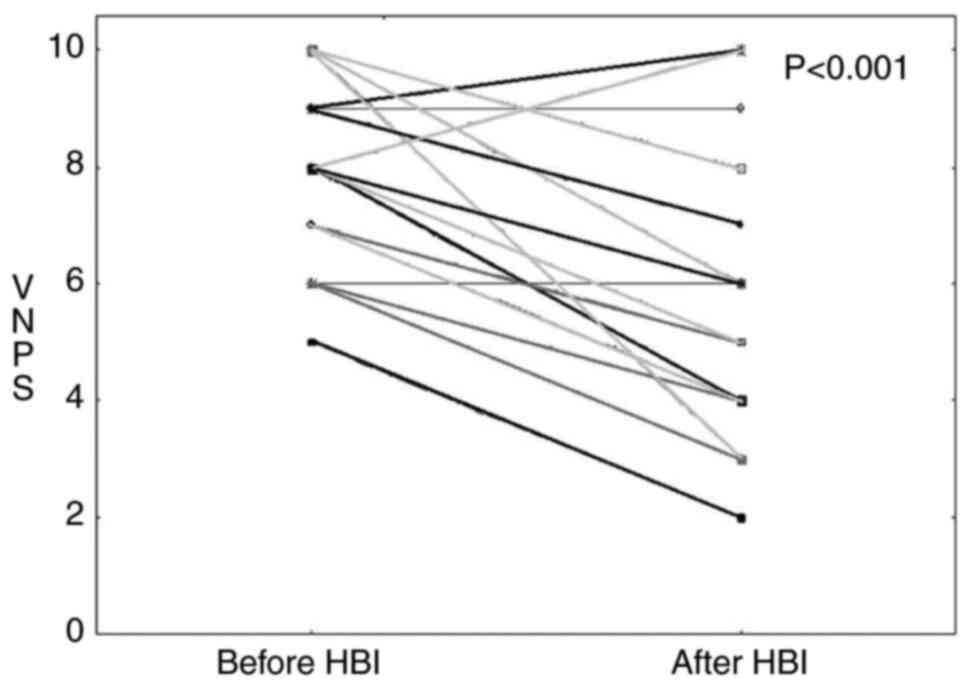
1). The median VNPS of the maximum pain in the last month
before the treatment was 8 (IQR 7-10) and 5 (IQR 4-7) on the
follow-up visit (P<0.001) (Fig.
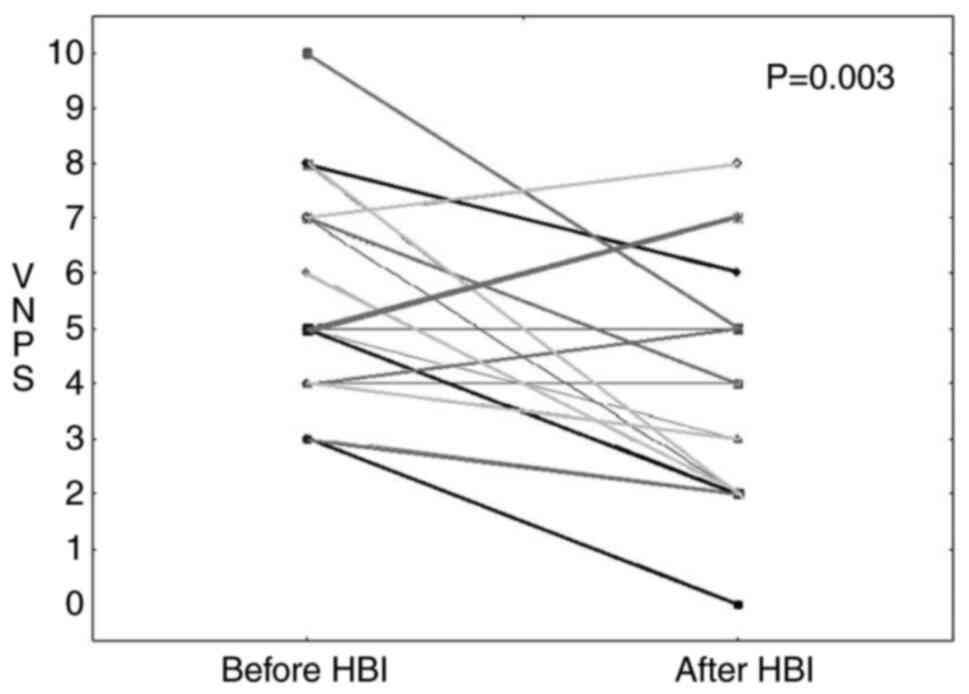
2). The median VNPS of the average pain calculated in the last
month before the treatment was 5 (IQR 4-7) and 3 (IQR 2-5) on the
day of the follow-up visit (P=0.003) (Fig. 3). A short-term complete response
was noted in 31.6% of patients (6 out of 19) and a partial response
was observed in 52.4% of patients (10 out of 19).
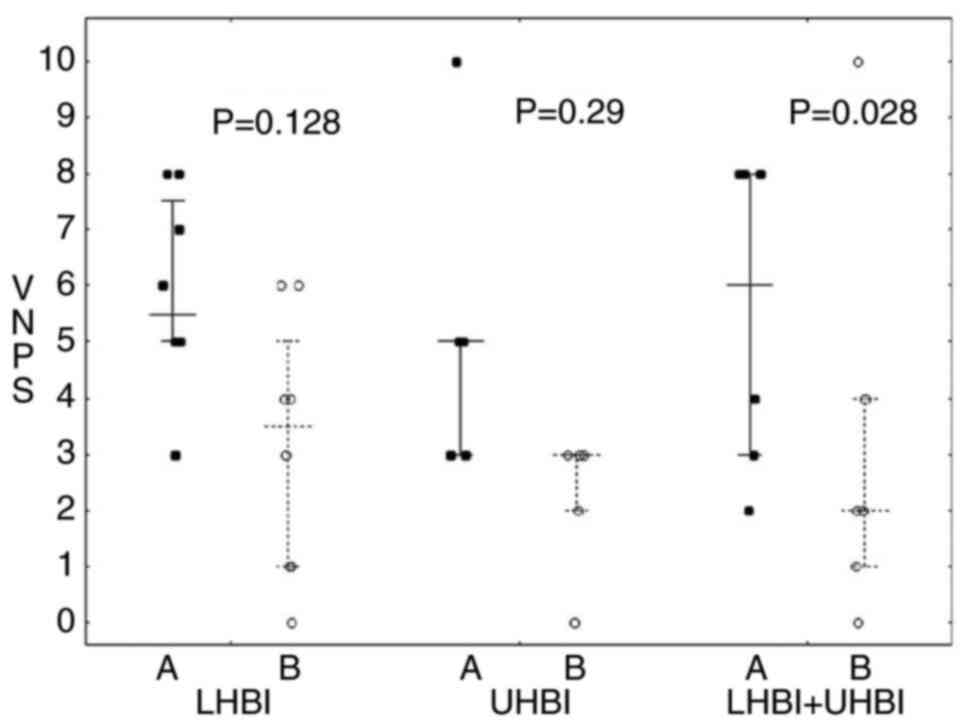
The VNPS of pain on the day before the treatment in
the UHBI group (n=5) was 5 (IQR 3-5) and 3 (IQR 2-3) on the day of
the follow-up (P=0.068). The median VNPS of the maximum pain in the
last month before the treatment in the UHBI group was 7 (IQR 6-8)
and 6 (IQR 4-6) on the follow-up visit (P=0.068). The median VNPS
of the average pain in the last month reported in the UHBI group
before the treatment was 4 (IQR 4-5) and 4 (IQR 4-5) on the
follow-up day (P=0.29). In the LHBI group (n=8), the VNPS of pain
on the day before the treatment was 5.5 (IQR 5-7.5) and 3.5 (IQR
1-5) on the follow-up day (P=0.028). The maximum pain reported in
this group in the last month before the treatment was 9 (IQR
7.5-10) and 5.5 (IQR 4.5-8.5) on the follow-up day (P=0.028). The
average pain in the last month before the treatment was 5.5 (IQR
5-7) and 3.5 (IQR 2.5-6) on the follow-up procedure (P=0.128). In
the group of patients with both UHBI and LHBI (n=6), the VNPS on
the day before the treatment was 6 (IQR 3-8) and 2 (IQR 1-4) during
the follow-up visit (P=0.144). According to the VNPS, the maximum
pain in the last month prior to the treatment was 8 (IQR 7-9) and 4
(IQR 3-7) after the treatment (P=0.059). The VNPS of the average
pain during the last month before HBI in this group was 6 (IQR 5-8)
and 2 (IQR 2) during the follow-up visit (P=0.028). Table II and Fig. 4 demonstrate the total value in all
subgroups.
 | Table IISummary of the palliation effect in
all subgroups. |
Table II
Summary of the palliation effect in
all subgroups.
| VNPS | UHBI (n=5) | LHBI (n=8) | UHBI + LHBI
(n=6) |
|---|
| VNPS of pain at the
day of the questionnaire | | | |
|
Before
treatment | 5 (IQR, 3-5) | 5.5 (IQR, 5-7.5) | 6 (IQR, 3-8) |
|
At
follow-up | 3 (IQR, 2-3) | 3.5 (IQR, 1-5) | 2 (IQR, 1-4) |
|
P-value | 0.068 | 0.028 | 0.144 |
| VNPS of maximum pain
during the last month | | | |
|
Before
treatment | 7 (IQR, 6-8) | 9 (IQR, 7.5-10) | 8 (IQR, 7-9) |
|
At
follow-up | 6 (IQR, 4-6) | 5.5 (IQR,
4.5-8.5) | 4 (IQR, 3-7) |
|
P-value | 0.068 | 0.028 | 0.059 |
| VNPS of average pain
during the last month | | | |
|
Before
treatment | 4 (IQR, 4-5) | 5.5 (IQR, 5-7) | 6 (IQR, 5-8) |
|
At
follow-up | 4 (IQR, 4-5) | 3.5 (IQR, 2.5-6) | 2 (IQR, 2) |
|
P-value | 0.29 | 0.128 | 0.028 |
A retrospective analysis revealed grade 3 toxicity
in one patient with breast cancer and metastases to bones, treated
with UHBI. She needed to be admitted to hospital as well as
administered transfusion of packed red blood cells. No other
patient in this group demonstrated toxicity of grade 3 or
higher.
Discussion
Our retrospective study shows that VMAT-based HBI is
effective in palliation of pain, with relief in all measured scales
of pain. Our findings are similar to results by another authors
(8-10,12,13,16)
are consistent with two prospective trials, where pain relief was
reported in 76 and 73% of patients undergoing HBI (9,12).
However, in both trials, radiotherapy was applied in less conformal
techniques. One retrospective analysis of 3D conformal radiotherapy
with HBI, conducted in a large group (fractionation: 4 fractions of
3 Gy bind up to the total dose of 12 Gy) was presented, where pain
reduction was observed in 76.3% of patients (16). To our knowledge, this is the first
report of HBI delivered with highly conformal VMAT technique. In
general, VMAT allows to deliver a prescribed dose to PTV,
simultaneously protecting normal tissues outside PTV, as the high
gradient of a dose at borders of PTV allows to reduce doses in
OARs.
There is a number of studies on dose reduction in
OARs due to the use of VMAT (17,18).
Our dosimetric analysis showed that the VMAT technique, allows to
reduce doses applied to lungs to 4 Gy, for 6 Gy prescribed to PTV.
Therefore, potential escalation of dose to PTV can be safely
achieved. The risk of radiation-induced pneumonitis, which tends to
increase when a dose absorbed to a lung is higher than 6 Gy, is now
lower (14). What is more, with
the application of conformal techniques, doses to all OARs are
reduced in comparison to those prescribed to PTV (8).
In our group, we did not report grade 1-2 toxicity
due to lack of full retrospective data, which is a limitation of
this study. It is the grade 1-2 toxicity that is considered a
common adverse event of HBI (4,15).
However, despite another limitation of our study that doses in
ileum were not analyzed, a reduced radiation dose applied to the
gastrointestinal system may potentially reduce the number of
adverse events during the treatment. Results of our study confirmed
that the VMAT technique has another benefit. It also ensures
homogeneity of the dose delivered to PTV. This allows to treat all
metastatic locations with the same effective dose. On the other
hand, VMAT, being a highly conformal technique, needs image
verification before each fraction, which may be problematic in
highly symptomatic patients, treated with numerous arcs. Designing
a treatment for our patients was not difficult; however, it was
one-fraction treatment. Maintaining the same therapeutic position
can be difficult for a greater number of fractions.
A small-sized group of patients and only one-month
follow-up period are limitations of this analysis as well as only
grade 3 toxicity reported. Due to these limitations, further relief
of pain and grade 1-2 toxicity of this treatment remains unknown.
Another limitation of this report is that exact analgesics doses
and previous pharmacotherapy was analyzed and correlated with pain
level and HBI effectiveness. Yet, VMAT HBI appeared to be clearly
effective. Prospective trials followed by an analysis of toxicity
are needed to clarify advantages of conformal techniques in
HBI.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
AK was involved in conception and design,
acquisition and analysis of data, and was a major contributor in
writing the manuscript. AK and LG confirm the authenticity of all
the raw data BT analyzed and interpretated the data, and was
involved in drafting the manuscript. AO, NT, BTK, JŁB and PM
performed treatment, acquired the data and critically revised the
manuscript critically. JF and LG revised the manuscript critically,
were involved in writing the manuscript, conception and design of
the study, and gave final approval of the version to be published.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Consent was not required for this retrospective
study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mercadante S: Malignant bone pain:
Pathophysiology and treatment. Pain. 69:1–18. 1997.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Tubiana-Hulin M: Incidence, prevalence and
distribution of bone metastases. Bone. 12 (Suppl 1):S9–S10.
1991.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Foley KM: The treatment of cancer pain. N
Engl J Med. 313:84–95. 1985.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lin A and Ray ME: Targeted and systemic
radiotherapy in the treatment of bone metastasis. Cancer Metastasis
Rev. 25:669–675. 2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
De Felice F, Piccioli A, Musio D and
Tombolini V: The role of radiation therapy in bone metastases
management. Oncotarget. 8:25691–25699. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Wu JS, Wong RK, Lloyd NS, Johnston M,
Bezjak A and Whelan T: Supportive Care Guidelines Group of Cancer
Care Ontario. Radiotherapy fractionation for the palliation of
uncomplicated painful bone metastases-an evidence-based practice
guideline. BMC Cancer. 4(71)2004.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Niibe Y and Hayakawa K: Oligometastases
and oligo-recurrence: The new era of cancer therapy. Jpn J Clin
Oncol. 40:107–111. 2010.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Furlan C, Trovo M, Drigo A, Capra E and
Trovo MG: Half-body irradiation with tomotherapy for pain
palliation in metastatic breast cancer. J Pain Symptom Manage.
47:174–180. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Berg RS, Yilmaz MK, Høyer M, Keldsen N,
Nielsen OS and Ewertz M: Half body irradiation of patients with
multiple bone metastases: A phase II trial. Acta Oncol. 48:556–561.
2009.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Pal S, Dutta S, Adhikary SS, Bhattacharya
B, Ghosh B and Patra NB: Hemi body irradiation: An economical way
of palliation of pain in bone metastasis in advanced cancer. South
Asian J Cancer. 3:28–32. 2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Salazar OM, Rubin P, Hendrickson FR,
Poulter C, Zagars G, Feldman MI, Asbell S and Doss L: Single-dose
half-body irradiation for the palliation of multiple bone
metastases from solid tumors: A preliminary report. Int J Radiat
Oncol Biol Phys. 7:773–781. 1981.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Salazar OM, Rubin P, Hendrickson FR,
Komaki R, Poulter C, Newall J, Asbell SO, Mohiuddin M and Van Ess
J: Single-dose half-body irradiation for palliation of multiple
bone metastases from solid tumors. Final Radiation Therapy Oncology
Group report. Cancer. 58:29–36. 1986.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Salazar OM, Sandhu T, da Motta NW, Escutia
MA, Lanzós-Gonzales E, Mouelle-Sone A, Moscol A, Zaharia M and
Zaman S: Fractionated half-body irradiation (HBI) for the rapid
palliation of widespread, symptomatic, metastatic bone disease: A
randomized Phase III trial of the International Atomic Energy
Agency (IAEA). Int J Radiat Oncol Biol Phys. 50:765–775.
2001.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Fowler JF and Travis EL: The radiation
pneumonitis syndrome in half-body radiation therapy. Int J Radiat
Oncol Biol Phys. 4:1111–1113. 1978.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Poulter CA, Cosmatos D, Rubin P, Urtasun
R, Cooper JS, Kuske RR, Hornback N, Coughlin C, Weigensberg I and
Rotman M: A report of RTOG 8206: A phase III study of whether the
addition of single dose hemibody irradiation to standard
fractionated local field irradiation is more effective than local
field irradiation alone in the treatment of symptomatic osseous
metastases. Int J Radiat Oncol Biol Phys. 23:207–214.
1992.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Macchia G, Ferro M, Cilla S, Buwenge M,
Ianiro A, Boccardi M, Picardi V, Ferro M, Arena E, Zamagni A, et
al: Efficacy and safety of 3D-conformal half body irradiation in
patients with multiple bone metastases. Clin Exp Metastasis.
35:747–752. 2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tamaki T, Hirai R, Igari M, Kumazaki Y,
Noda SE, Suzuki Y and Kato S: Dosimetric comparison of
three-dimensional conformal radiotherapy versus volumetric-arc
radiotherapy in cervical cancer treatment: Applying the
central-shielding principle to modern technology. J Radiat Res.
59:639–648. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Sudha SP, Seenisamy R and Bharadhwaj K:
Comparison of dosimetric parameters of volumetric modulated arc
therapy and three-dimensional conformal radiotherapy in
postmastectomy patients with carcinoma breast. J Cancer Res Ther.
14:1005–1009. 2018.PubMed/NCBI View Article : Google Scholar
|