Introduction
In general, surgery to improve swallowing includes
laryngeal elevation, cricopharyngeal myotomy, pharyngeal flap
surgery, and arytenoid adduction. A combination of these procedures
is performed depending on the pathophysiology of each case. With
respect to operative indications, the patient's condition and
prognosis are the most important eligibility factors, because
postoperative rehabilitation is also necessary to improve
swallowing function. Cricopharyngeal myotomy is often combined with
other swallowing improvement procedures, especially with laryngeal
elevation. It is often performed simultaneously through an external
cervical incision in the same surgical fields. However, only
cricopharyngeal myotomy may be indicated in specific diseases such
as Wallenberg's syndrome and neuromuscular diseases in which there
is failure to open the esophageal inlet. Endoscopic cricopharyngeal
myotomy (ECPM), reported by Halvorson and Kuhn (1) and Pitman and Weissbrod (2), may be considered for such cases.
ECPM is a safe and minimally invasive technique, but
it has not become widely used. In 2011, Chitose et al
improved on this technique and reported a method in which the
incised mucosa is sutured at the end to close the posterior
pharyngeal space (3). We have
performed this procedure in a few cases in our institution. In one
of these cases, it was difficult to insert the Weerda distending
operating laryngoscope (Karl Storz, Tuttlingen, Germany) in the
proper position, and repeated manipulation resulted in the
application of excessive force to the pharyngeal mucosa, causing
mucosal damage. Furthermore, when resecting the cricopharyngeal
muscle, the pharyngeal venous plexus bled, and the amount of
bleeding was even greater, making it impossible to stop the
bleeding with a laser and forceps in that operative field.
Ultimately, hemostasis was achieved through an external cervical
incision.
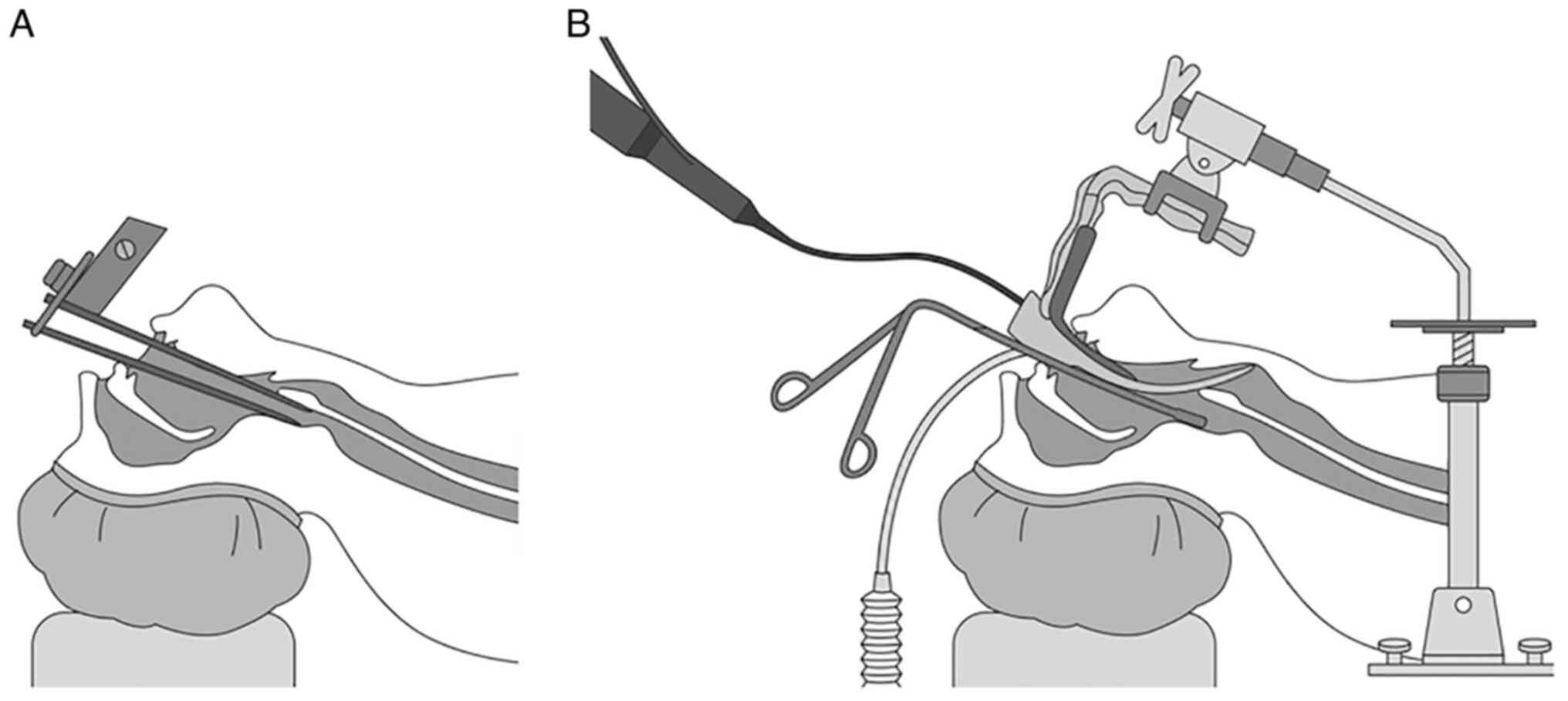
Recently, endoscopic laryngopharyngeal surgery
(ELPS) using a curved rigid laryngoscope (Sato's Curved rigid
laryngoscope, Nagashima Medical Instruments Company, Tokyo, Japan)
has been used for the treatment of superficial cancer of the
hypopharynx (4). The curved rigid
laryngoscope expands the hypopharynx more widely than the
diverticuloscope and does not compress the pharyngeal mucosa.
Therefore, damage to the oral and pharyngeal mucosa is unlikely to
occur. Moreover, along with greater flexibility, there is less
restriction of the movement of surgical instruments and less
interference between instruments (Fig.
1). Surgical instruments such as electrocautery and suction
coagulators can be inserted and can stop bleeding more reliably
than a CO2 laser, even in cases of massive bleeding. We
have performed ECPM using a curved rigid laryngoscope for patients
with laryngeal palsy after skull base surgery. A new method of ECPM
is presented, and its advantages and applications are
discussed.
Case report
Methods
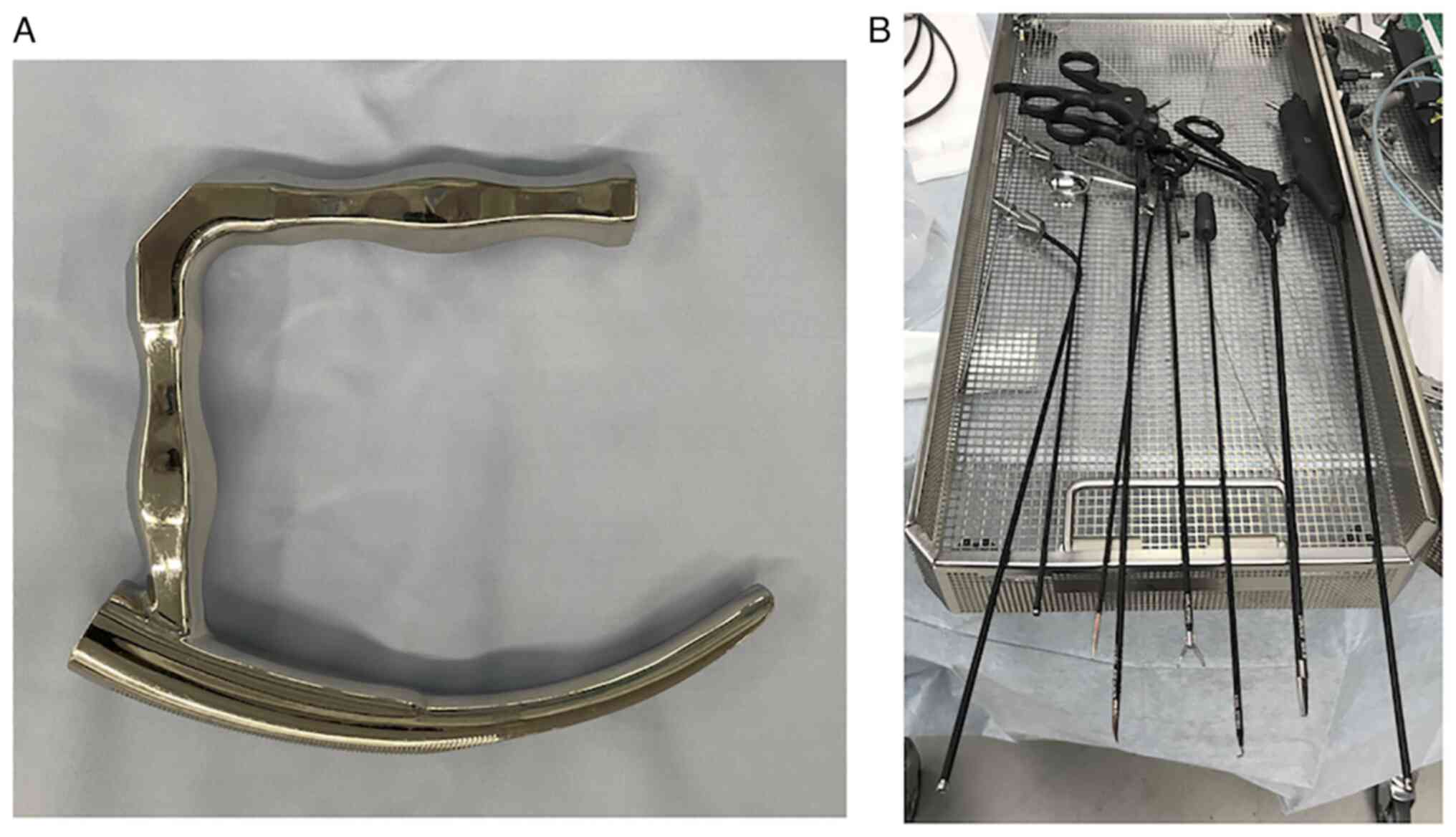
The instruments used were a curved rigid
laryngoscope (Sato's Curved rigid laryngoscope, Nagashima Medical
Instruments Company), apical curved video scope (ENDOEYE FLEX,
Olympus, Tokyo, Japan), electrocautery scalpel, bipolar forceps,
grasping forceps, suction coagulator (Karl Storz, Tuttlingen,
Germany), apical flexible electrocautery scalpel (KD600 apical
flexible electrocautery scalpel, Olympus), and electrocautery body
(High-Frequency Surgery Equipment VIO 3, ERBE, Tübingen, Germany).
The electrocautery body setting was in cut mode Dry 60W/effect 4
and soft coag mode 30W/effect 3. Fig.
2 shows the curved rigid laryngoscope and surgical instruments,
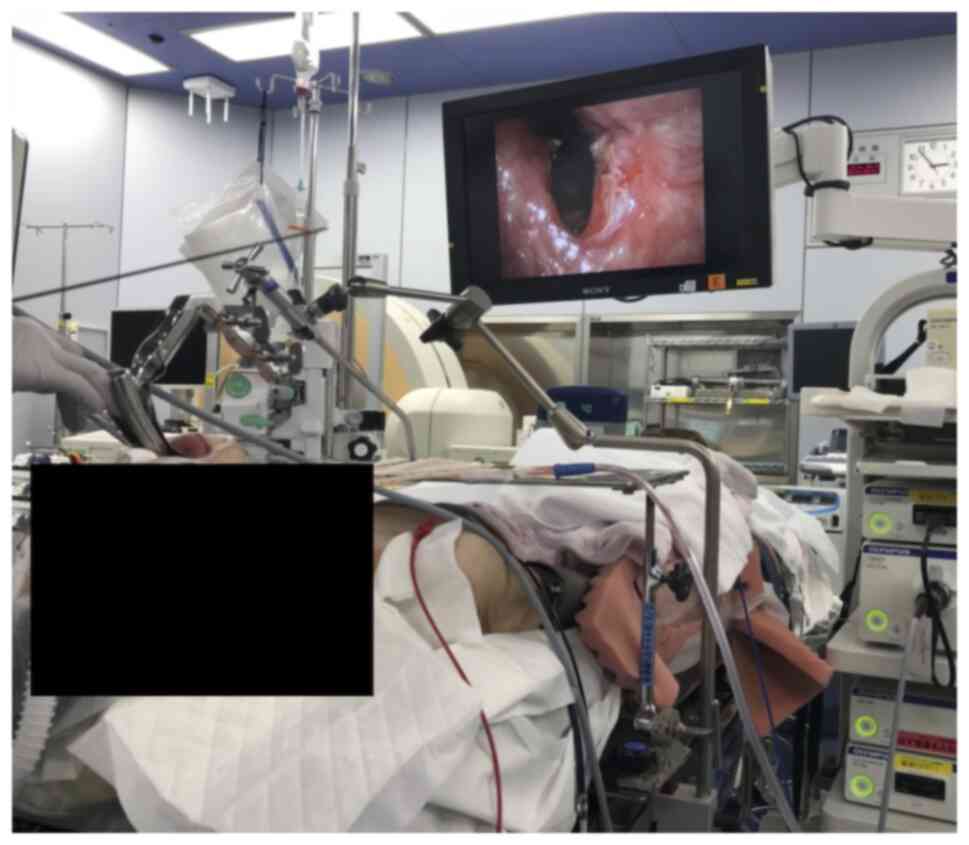
and Fig. 3 shows the surgical
situation regarding the curved rigid laryngoscope.
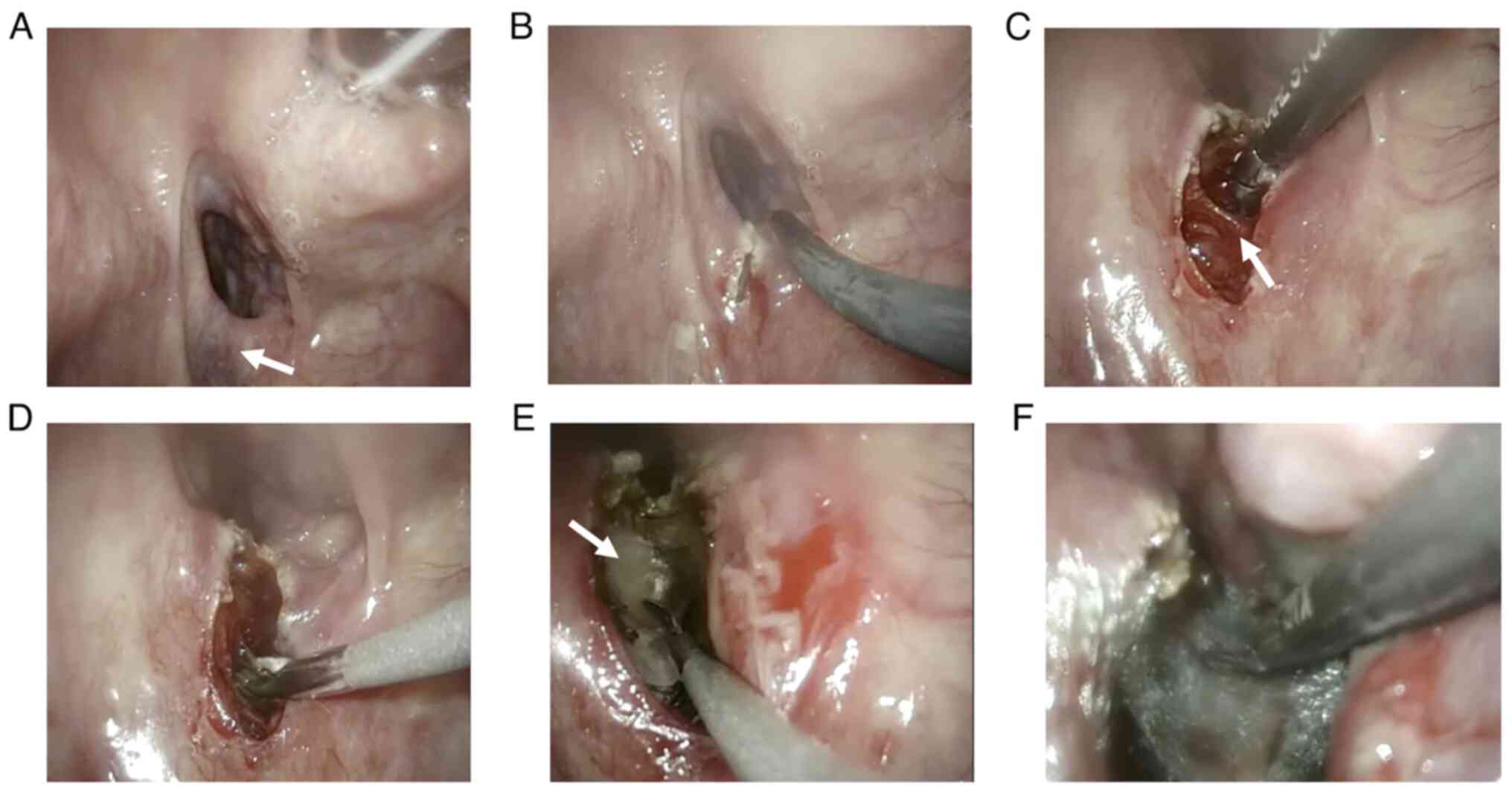
The surgical technique was as follows. First, the
pharynx was expanded with a curved rigid laryngoscope, and then the
clear field of view for identifying the cricopharyngeal muscle was
developed by the apical curved videoscope. The cricopharyngeal
muscle could be recognized as a submucosal ridge on the posterior
wall of the esophageal inlet. (Fig.
4A). Subsequently, a mucosal incision was made with an
electrocautery scalpel (Fig. 4B),
and the submucosa and dorsal surface of the cricopharyngeal muscle
were dissected by bipolar forceps. The cricopharyngeal muscle was
identified and freed from the surrounding area (Fig. 4C). The next step was cutting the
cricopharyngeal muscle. Bipolar cautery should be used as much as
possible before cutting muscle. Because the cricopharyngeal muscle
has a venous plexus, its blood flow varies from person to person.
The cricopharyngeal muscle is a transverse muscle, so resection
should proceed until the transverse muscle is no longer present
(Fig. 4D). Buccopharyngeal fascia,
the sparse connective tissue beyond the cut muscle, should be
preserved as much as possible (Fig.
4E). After the resection, hemostasis was confirmed, and a
polyglycolic acid (PGA) sheet was cut into small pieces and applied
with fibrin glue (Fig. 4F).
Case presentation
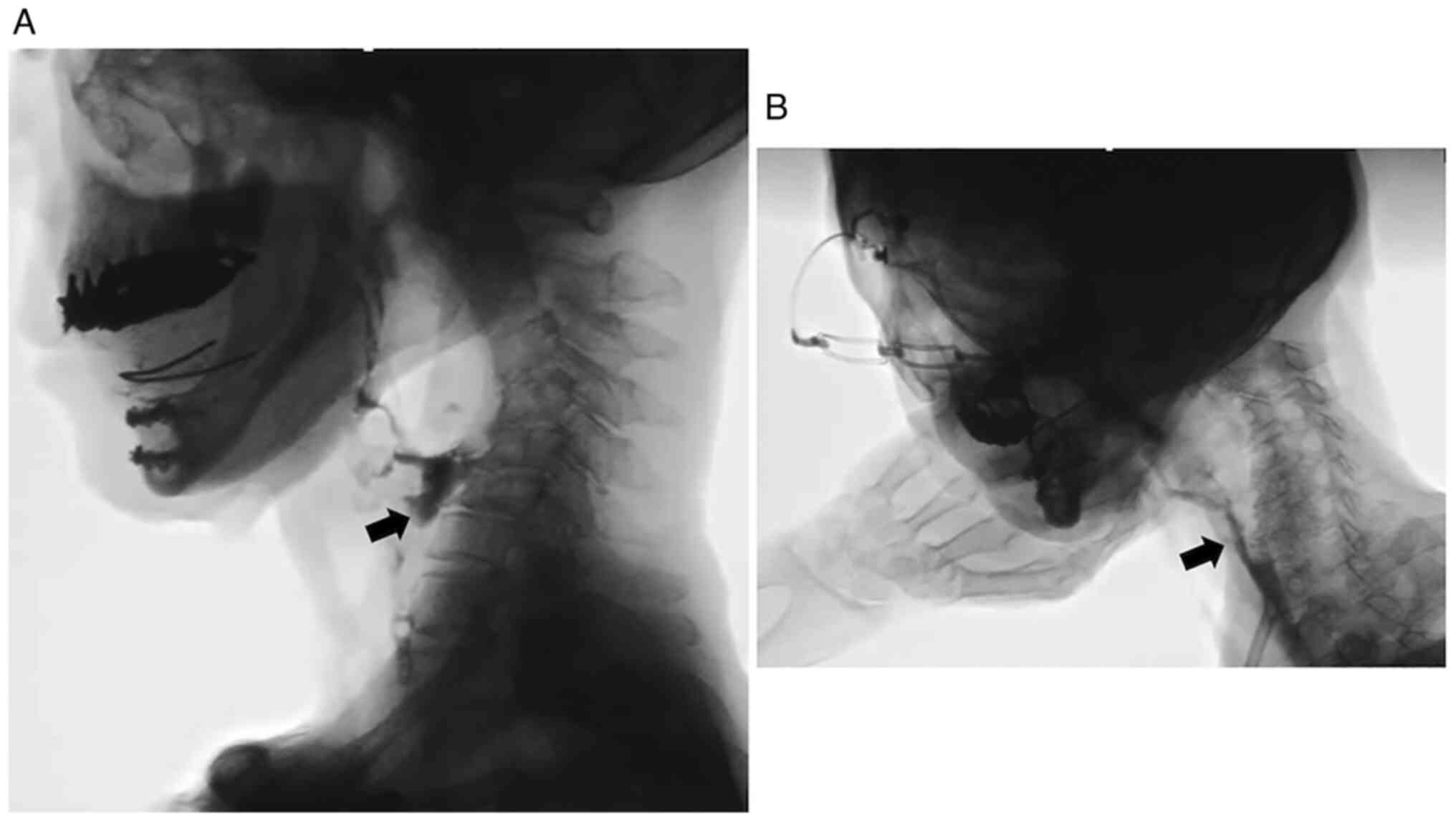
The patient, an 80-year-old woman, presented with
laryngeal paralysis due to inferior cranial nerve palsy after skull
base nerve sheath tumor surgery and consequent dysphagia and
visited Nagoya University Hospital in December 2017. The patient
showed significant residue on preoperative videofluorography (VF)
after swallowing some thickened water (Fig. 5A). No compensatory swallowing
technique of any kind was effective. The possible causes of this
swallowing disorder were as follows: Decreased pharyngeal pressure;
failure of opening of the esophageal inlet; and failure of
cricopharyngeal muscle relaxation. Considering her age and physical
condition, a less invasive and time-saving procedure was needed.
Therefore, ECPM with the ELPS technique was selected based on our
previous experience.
The patient was kept off food and drink for one week
postoperatively. During this period, the patient was managed on
tube feeding and peripheral parenteral nutrition (PPN). Swallowing
training was initiated when no leakage and no mediastinal
complications were seen on the first VF study after surgery. The
patient underwent rehabilitation, including Shaker exercise, chin
push-pull maneuver, and head rotation position swallowing, for one
month. Improvement of swallowing function was observed after one
month of rehabilitation. The residue almost disappeared on
thickened liquid swallowing (Fig.
5B), and the time for meals was shorter than before
surgery.
Discussion
ECPM was performed using a curved rigid laryngoscope
in a patient with impaired opening of the upper esophageal
sphincter (UES) without any postoperative complications, and
residue reduction after swallowing was confirmed. This procedure
was developed based on the report of ECPM by Chitose et al
(3). In our institution, we have
experienced difficulties in surgical field development and
postoperative complications with Chitose's method. We had
considerable experience with ELPS using a curved rigid laryngoscope
for superficial pharyngeal cancer. The curved laryngoscope is
placed slightly cephalad of the vocal cords, and the hypopharynx is
expanded by raising the curved laryngoscope forward. This allows
the hypopharynx to be widely expanded, and the entire area can be
observed, even the esophageal inlet. The cricopharyngeal muscle can
be seen as a circular ridge at the esophageal inlet. Therefore, we
decided to use the curved rigid laryngoscope for ECPM. Using the
curved rigid laryngoscope, it was possible to develop a wider
surgical field than when using the Weerda distending operating
laryngoscope.
The major difference between the present technique
and Chitose's method (3) is the
suture of the pharyngeal mucosa after cricopharyngeal myotomy. The
posterior pharyngeal space is exposed after cricopharyngeal
myotomy. The posterior pharyngeal space is connected to the
dangerous space that connects the deep cervical spaces to the
mediastinum, and infection or abscess can be fatal. Pitman and
Weissbrod also recommended preservation of the buccopharyngeal
fascia, which is the shallow layer of the posterior pharyngeal
space, to prevent connection to this dangerous space (2). In this technique, the operative field
is wider than that with the microscope used in conventional ECPM,
and the use of a videoscope with a movable tip makes it possible to
observe the tissue from multiple directions. Connective tissue
attached to the cricopharyngeal muscle can be recognized more
clearly, and connective tissue from the back surface of the
cricopharyngeal muscle to the buccopharyngeal fascia can be
recognized and preserved more reliably than with conventional
techniques. Therefore, only the cricopharyngeal muscle can be
reliably resected, and the pharyngeal venous plexus can be
recognized in advance, allowing resection while preparing for
hemostasis. In the unlikely event of bleeding, surgical instruments
such as electrocautery and suction coagulators can be inserted to
stop the bleeding more reliably than a CO2 laser.
Furthermore, Chitose et al (3) reported that the mucosal suture was
sutured perpendicular to the direction of the cut so that the
esophageal inlet was wider. In the present case, we tried to
minimize the opening of the posterior pharyngeal space with our
procedure and to fix the PGA sheet with fibrin glue after
cricopharyngeal myotomy. Since the surgical field for this
procedure is originally dirty, we believe that it makes more sense
to leave it open rather than closed, so as not to trap saliva and
bacterial flora. However, in terms of further widening the entrance
after resection and controlling wound scarring, we believe that
suturing to enlarge the resection area is a worthwhile technique.
Though this is possible in our technique, it was difficult in the
present case because of the scar contracture of the mucosa. If the
suture closure can be done with a generous space rather than a
tight suture closure, it will likely prevent bacteria from being
trapped and prevent scarring of the wound and enlargement of the
esophageal inlet. This technique has a wide field of view and easy
access to instruments, making it possible to perform such a
detailed procedure. This is a future issue for our surgical
method.
Furthermore, a better understanding of the anatomy
of the pharyngeal lumen is needed. Especially at the beginning of
cricopharyngeal myotomy, a high rate of bleeding was observed.
Although the bleeding was of venous origin, we had a case in which
hemostasis was difficult to achieve. The cricopharyngeal muscle
contains the pharyngeal venous plexus. The pharyngeal venous plexus
varies from person to person and may be mistaken for a tumor on
imaging, and some reports recommend making a diagnosis with the
venous plexus in mind (5). Massive
bleeding may occur if resection is rushed without awareness of the
pharyngeal venous plexus. If hemostasis is difficult to achieve,
carbonization of the tissue due to cauterization may lead to
delayed wound healing, infection, and surrounding scarring.
Previous reports have also emphasized the importance of minimally
invasive and minimally necessary treatment (2,3).
We believe that this is a relatively easy procedure
to perform if the surgeon is familiar with the curved rigid
laryngoscope technique. The operative field can be expanded widely,
making it easy to manipulate forceps and electrical devices. In
addition, the movable videoscope enables multifaceted observation
of the pharynx, making it easy to recognize the pharyngeal venous
plexus and buccopharyngeal fascia. We also believe that this
technique is not only easier to operate, but also safer than
conventional techniques. However, there is still room for
improvement in the procedure, surgical instruments, and other
aspects, and further accumulation of cases and analysis of
long-term functional outcomes and postoperative complications are
needed. Once established as a technique, cricopharyngeal myotomy
will expand the range of indications and benefit many patients.
Acknowledgements
Not applicable.
Funding
Funding: This research was supported by JSPS KAKENHI (grant no.
19K18766).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
TM conceived and designed the study and prepared the
manuscript. TM, YF, SY, MaS, NN, MH and MiS conducted data
acquisition, data analysis and interpretation. TM, YF, NN and MiS
conducted revision of the manuscript for important intellectual
property. TM and YF confirmed the authenticity of all the raw data.
TM, YF, SY, MaS, NN, MH and MiS read and approved the final
manuscript.
Ethics approval and consent to
participate
Ethics approval is not applicable. Written informed
consent was obtained from the patient for participation in the
study.
Patient consent to participate and
publication
Written informed consent was obtained from the
patient for publication of this study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Halvorson DJ and Kuhn FA: Transmucosal
cricopharyngeal myotomy with the potassium-titanyl-phosphate laser
in the treatment of cricopharyngeal dysmotility. Ann Otol Rhinol
Laryngol. 103:173–177. 1994.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Pitman M and Weissbrod P: Endoscopic
CO2 laser cricopharyngeal myotomy. Laryngoscope.
119:45–53. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chitose S, Sato K, Hamakawa S, Umeno H and
Nakashima T: A new paradigm of endoscopic cricopharyngeal myotomy
with CO2 laser. Laryngoscope. 121:567–570.
2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Satou Y, Omori T and Tagawa M: Treatment
of superficial carcinoma in the hypopharynx. Nihon Jibiinkoka
Gakkai Kaiho. 109:581–586. 2006.PubMed/NCBI View Article : Google Scholar : (In Japanese).
|
|
5
|
Bunch PM, Hughes RT, White EP, Sachs JR,
Frizzell BA and Lack CM: The pharyngolaryngeal venous plexus: A
potential pitfall in surveillance imaging of the neck. AJNR Am J
Neuroradiol. 42:938–944. 2021.PubMed/NCBI View Article : Google Scholar
|