Introduction
Microwave ablation (MWA) is a promising non-vascular
interventional technique, with clear efficacy in local control. For
the treatment of small primary and secondary hepatic tumors (<3
cm), MWA may be comparable to surgical resection (1-4).
Furthermore, numerous clinical trials have indicated that
trans-arterial chemoembolization (TACE) combined with MWA may
significantly improve the rate of complete necrosis of tumors and
prolong the survival of patients (5,6).
However, for special lesions, such as those adjacent to the
diaphragm, blood vessels, or the biliary or intestinal tract, MWA
may also have a series of complications, which should be paid more
attention to. For hepatic tumors adjacent to the diaphragm, there
have been reports of complications, such as diaphragmatic
perforation and hernia, biliary pleural fistula and biliary
bronchial fistula caused by MWA thermal injury (7,8). The
present study reports on a rare iatrogenic complication of hepatic
artery-pulmonary artery fistula (HA-PAF) after MWA of a hepatic
tumor adjacent to the diaphragm.
Case report
A 60-year-old male with a surgical history of colon
cancer presented with progression of solitary liver metastasis
after multiple courses and lines of chemotherapy. The patient did
not have any symptoms. Physical examination did not reveal any
abnormalities. Routine hematological, biochemical and coagulation
functions were within the normal range. The levels of tumor markers
[CEA (normal limit, <5.0 ng/ml), 120 ng/ml; CA19-9 (normal
limit, <37.0 U/ml), 62.0 U/ml; CA125 (normal limit, <35.0
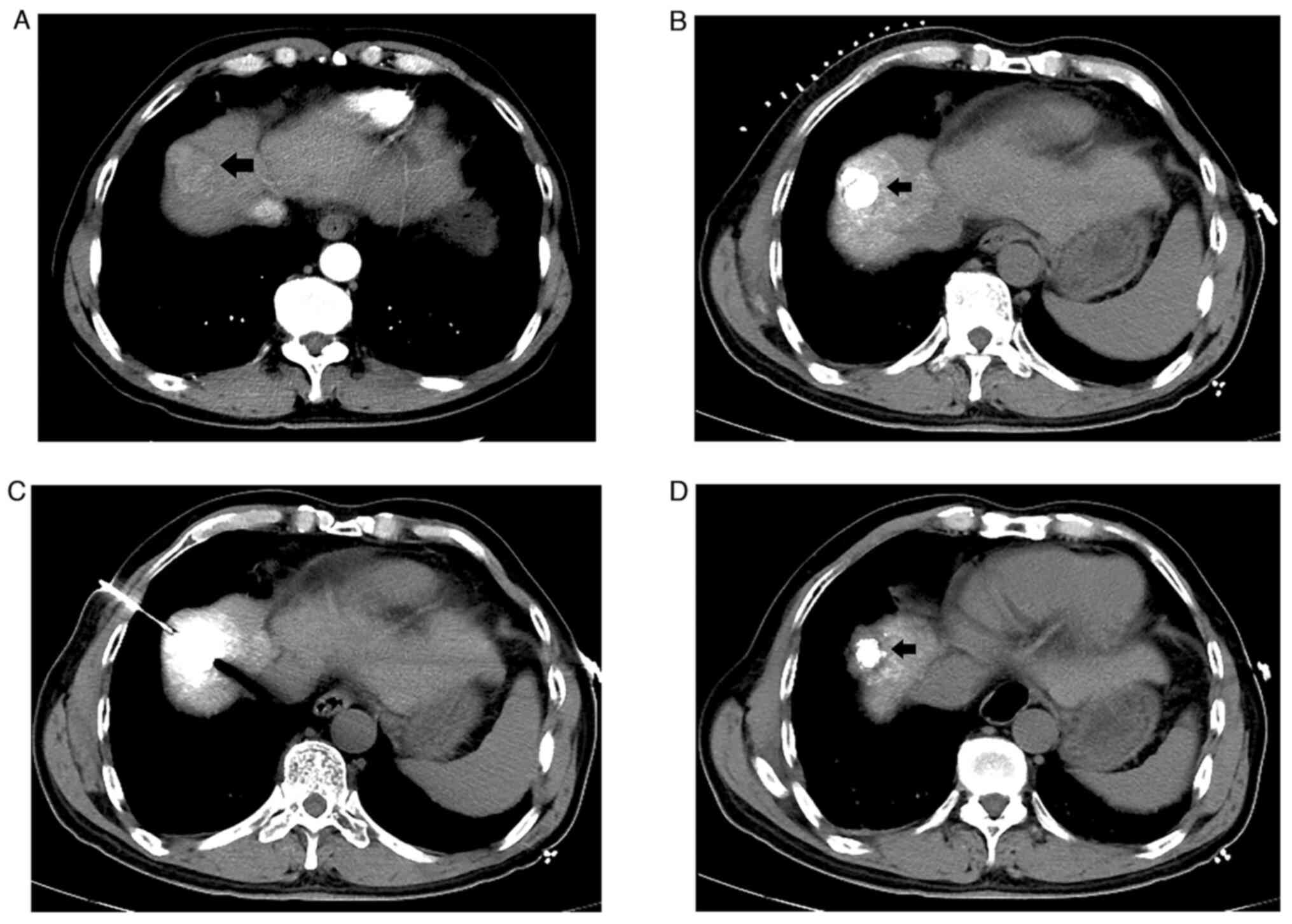
U/ml), 78.2 U/ml] were higher than normal. Abdominal
contrast-enhanced computed tomography (CT) indicated a round-like
mass of ~3.0x2.5 cm in hepatic segment VIII abutting the diaphragm,
with obvious enhancement of the lesion in the arterial phase
(Fig. 1A). Considering
chemotherapy resistance, the decision to perform local
interventional therapy was made after a multi-disciplinary
discussion.
First, TACE was performed to label and embolize the
hepatic tumor, using iodized oil (Laboratoire Andre Guerbet) as an
embolic agent. Subsequently, MWA was performed percutaneously under
the guidance of CT. The tumor exhibited intra-tumoral high-density
iodized oil deposition (Fig. 1B)
on a preprocedural CT scan. Under local anesthesia and conscious
sedation, a single, 17-G, internally cooled antenna (MTC-3C MWA
system, Vison Medical, Inc.) was introduced into the tumor via the
right lower lung and diaphragm (Fig.
1C). The microwave power was set at 40 W and the ablation
duration was 8 min. A follow-up CT scan obtained immediately after
MWA indicated complete ablation with good ablative margin (Fig. 1D). The patient recovered smoothly
and reported slight chest tightness and shortness of breath after
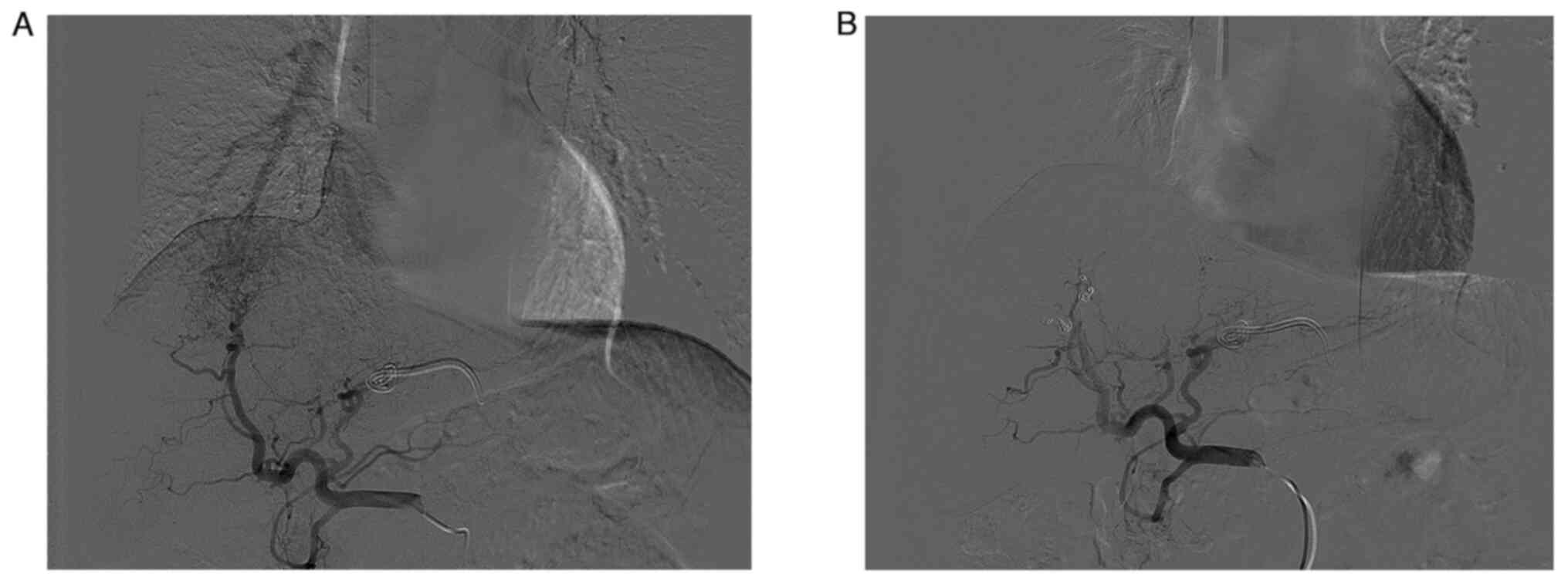
discharge. One month later, a transhepatic arterial chemoinfusion
was performed as scheduled and the hepatic angiography revealed a
fistula between the right hepatic artery and the right lower
pulmonary artery (Fig. 2A).
Subsequently, the HA-PAF was successfully occluded by
trans-arterial embolization using three microcoils
(MWCE-18S-3/2-TORNADO; COOK Inc.). Control hepatic arteriography at
the end of the procedure indicated complete occlusion of the
fistula (Fig. 2B). The
postoperative course was uneventful and the patient was discharged
with symptomatic improvement three days later.
Discussion
HA-PAF, an abnormal communication between the
hepatic artery and pulmonary artery, is a rare complication of MWA.
To the best of our knowledge, so far, only one case report has
presented a similar case, but no effective treatment was given
(9). The early clinical symptoms
are usually insidious and easily ignored by patients and
clinicians. Imaging examinations (CT, magnetic resonance or
ultrasound) frequently fail to detect the fistula, whereas only
hepatic arteriography is able to confirm the diagnosis. When the
pulmonary artery pressure increases gradually, the patient has an
obvious cough, expectoration, chest tightness and dyspnea. If not
treated in time, serious complications may occur, such as
hemoptysis and heart failure, and they may even be life-threatening
(10,11).
The formation of HA-PAF may be congenital or
acquired, the latter being mainly caused by chronic inflammation,
accidental trauma or iatrogenic collateral thermal damage. Thermal
damage is caused by hyperthermic ablation (MWA), which is caused by
heating the targeted tissue to >60˚C, leading to acute
coagulative necrosis. In the present case, the cause of a HA-PAF
was considered as follows: On the one hand, MWA performed with a
high-power setting and long duration give rise to a large ablation
area involving the diaphragm and lung tissue. Due to the local
weakness of the thermal damaged tissue, delayed perforation and
abnormal communication between blood vessels may occur after
long-term respiratory movement. On the other hand, the tumor is
located in the hepatic dome adjacent to the right diaphragm. The
puncture path passes through the lung tissue and diaphragm,
resulting in mechanical injury. Furthermore, iodized oil has good
thermal conductivity, which may increase the temperature in the
ablation area by improving heat conduction, causing heat
accumulation and expansion of the ablation area.
Considering the high risk of thermal injury to the
diaphragm around the tumor after MWA, precautionary measures should
be taken to avoid collateral damage to adjacent organs. Results of
a previous study suggested that the establishment of artificial
ascites and/or pleural effusion was equivalent to the formation of
a barrier zone, which may separate the adjacent blood vessels,
liver and diaphragm from thermal ablation (12-14).
The barrier zone may reduce heat energy conduction and avoid
thermal injury, thereby protecting the diaphragm, lung tissues and
its internal blood vessels. However, for patients who underwent
surgical resection of liver tumors, or had peritonitis, it is
difficult to establish artificial pleural effusion or ascites due
to the peritoneal or pleural adhesions (12-14).
While the patient of the present study underwent laparotomy prior
to microwave therapy, microwave therapy with artificial pleural
effusion or artificial ascites should have been opted for.
The ablation area may not completely cover the
tumor, resulting in tumor residue. Thus, for hepatic tumor adjacent
to the diaphragm, clinicians should be aware of the risk and
potential complications of diaphragm injury. In addition, patients
should be followed up regularly after MWA and provided with more
attention to changes in their conditions. When there are symptoms
of pulmonary hypertension, such as weakness, dizziness, chest
tightness, shortness of breath and dyspnea, clinicians should be
promptly alerted to the presence of HA-PAF and hepatic
arteriography is required to make a clear diagnosis.
In conclusion, the present study reported a rare
case of HA-PAF as an iatrogenic complication due to MWA thermal
injury that was successfully managed by trans-arterial
embolization. This may be an important observation for improving
post-surgery monitoring and management after MWA in the clinic.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BL and XGL were involved in the design and
conception of the study and confirmed the authenticity of all the
raw data. BL analyzed and interpreted the data, and was involved in
drafting the manuscript. BL and XGL performed the treatment,
acquired the data and critically revised the manuscript. XGL
supervised the conduct of this report. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were in accordance with the ethical standards of the
institutional and/or national research committee and with the 1964
Helsinki declaration and its later amendments or comparable ethical
standards.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of this report and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mironov O, Jaberi A and Kachura JR:
Thermal ablation versus surgical resection for the treatment of
stage T1 hepatocellular carcinoma in the surveillance,
epidemiology, and end results database population. J Vasc Interv
Radiol. 28:325–333. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Biederman DM, Titano JJ, Bishay VL,
Durrani RJ, Dayan E, Tabori N, Patel RS, Nowakowski FS, Fischman AM
and Kim E: Radiation segmentectomy versus TACE combined with
microwave ablation for unresectable solitary hepatocellular
carcinoma up to 3 cm: A propensity score matching study. Radiology.
283:895–905. 2017.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Knott EA, Ziemlewicz TJ, Lubner SJ,
Swietlik JF, Weber SM, Zlevor AM, Longhurst C, Hinshaw JL, Lubner
MG, Mulkerin DL, et al: Microwave ablation for colorectal cancer
metastasis to the liver: A single-center retrospective analysis. J
Gastrointest Oncol. 12:1454–1469. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Radosevic A, Quesada R, Serlavos C,
Sánchez J, Zugazaga A, Sierra A, Coll S, Busto M, Aguilar G, Flores
D, et al: Microwave versus radiofrequency ablation for the
treatment of liver malignancies: A randomized controlled phase 2
trial. Sci Rep. 12(316)2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zaitoun MMA, Elsayed SB, Zaitoun NA,
Soliman RK, Elmokadem AH, Farag AA, Amer M, Hendi AM, Mahmoud NEM,
Salah El Deen D, et al: Combined therapy with conventional
trans-arterial chemoembolization (cTACE) and microwave ablation
(MWA) for hepatocellular carcinoma >3-<5 cm. Int J
Hyperthermia. 38:248–256. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zhao J, Wu J, He M, Cao M, Lei J, Luo H,
Yi F, Ding J, Wei Y and Zhang W: Comparison of transcatheter
arterial chemoembolization combined with radiofrequency ablation or
microwave ablation for the treatment of unresectable hepatocellular
carcinoma: A systemic review and meta-analysis. Int J Hyperthermia.
37:624–633. 2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Huang ZM, Zuo MX, Gu YK, Lai CX, Pan QX,
Yi XC, Zhang TQ and Huang JH: Bronchobiliary fistula after ablation
of hepatocellular carcinoma adjacent to the diaphragm: Case report
and literature review. Thorac Cancer. 11:1233–1238. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Livraghi T, Meloni F, Solbiati L and Zanus
G: Collaborative Italian Group using AMICA system. Complications of
microwave ablation for liver tumors: Results of a multicenter
study. Cardiovasc Intervent Radiol. 35:868–874. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Qin Y, Zhang J and Li S: Hepatic
artery-pulmonary artery fistula. Ann Thorac Surg.
114(e77)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Sockrider M, Roessel L, Fagan KA and
Gillespie M: Diagnosis and treatment of pulmonary hypertension. Am
J Respir Crit Care Med. 203:P14–P15. 2021.
|
|
11
|
Maron BA, Abman SH, Elliott CG, Frantz RP,
Hopper RK, Horn EM, Nicolls MR, Shlobin OA, Shah SJ, Kovacs G, et
al: Pulmonary arterial hypertension: Diagnosis, treatment, and
novel advances. Am J Respir Crit Care Med. 203:1472–1487.
2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Delmas L, Koch G, Cazzato RL, Weiss J,
Auloge P, Dalili D, de Marini P, Gangi A and Garnon J: Artificial
ascites using the guidewire technique during microwave ablation in
the liver dome: Technique and analysis of fluid repartition. Abdom
Radiol (NY). 46:4452–4459. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang Y, Zhang L, Li Y and Wang W: Computed
tomography-guided percutaneous microwave ablation with artificial
ascites for problematic hepatocellular tumors. Int J Hyperthermia.
37:256–262. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Qi H, Zhang H, Wan C, Xie L, Song Z and
Fan W: CT-guided microwave ablation through the lungs for treating
liver tumors near the diaphragm. Oncotarget. 8:79270–79278.
2017.PubMed/NCBI View Article : Google Scholar
|