Introduction
Fibromatosis, also termed desmoid tumor or
aggressive fibromatosis (AF), is a clonal proliferative tumor that
emerges from mesenchymal cells in the fascia and musculoaponeurotic
structures and belongs to a small subset of soft tissue lesions
(1,2). It is a rare soft tissue tumor that
accounts for ~0.03% of all tumors and <3% of all soft tissue
tumors, with a general population incidence of 2-4 per million
individuals per year (3). Although
the causes of this condition remain unclear, a connective tissue
proliferation disease has been proposed as a possible cause. AF in
adults has been linked to inherited diseases (Gardner's syndrome),
pregnancy (particularly second pregnancy) and female sex hormones.
However, these links do not apply to children (4). The majority of the cases are sporadic
and genetically linked to Wnt/b-catenin pathway gene mutations,
with a smaller percentage related to APC gene mutations (5). Syndromic cases are typically
associated with intra-abdominal diseases and familial adenomatous
polyposis (6). Regardless of the
fact that fibromatosis does not metastasize and has a good survival
prognosis, patients suffer significant morbidity as a result of the
tumor's invasive progression and the possibility of a high
recurrence rate ranging from 15 to 77% (6,7). The
aim of the present study was to report a case series of
extra-abdominal recurrent AF.
Patients and methods
Study design
The present study was a single-center retrospective
case-series of patients with recurrent AF. The present study was
approved by the Sulaimani University Ethics Committee (2023/no.
20). All patients or the parents of patients (for cases <18
years old) provided signed consent for their data to be published.
The cases were managed at a single private facility. Throughout the
previous 7 years (January 2016 to January 2023), the patients were
evaluated, treated and followed-up.
Study participants
The socio-demographic and clinical data of the
patients were obtained from the electronic health records of the
Orthopedic Clinic at Smart Health Tower (Sulaimani, Iraq), which
included age, sex, occupation, previous medical history, previous
surgical history, smoking status, family history, radiation
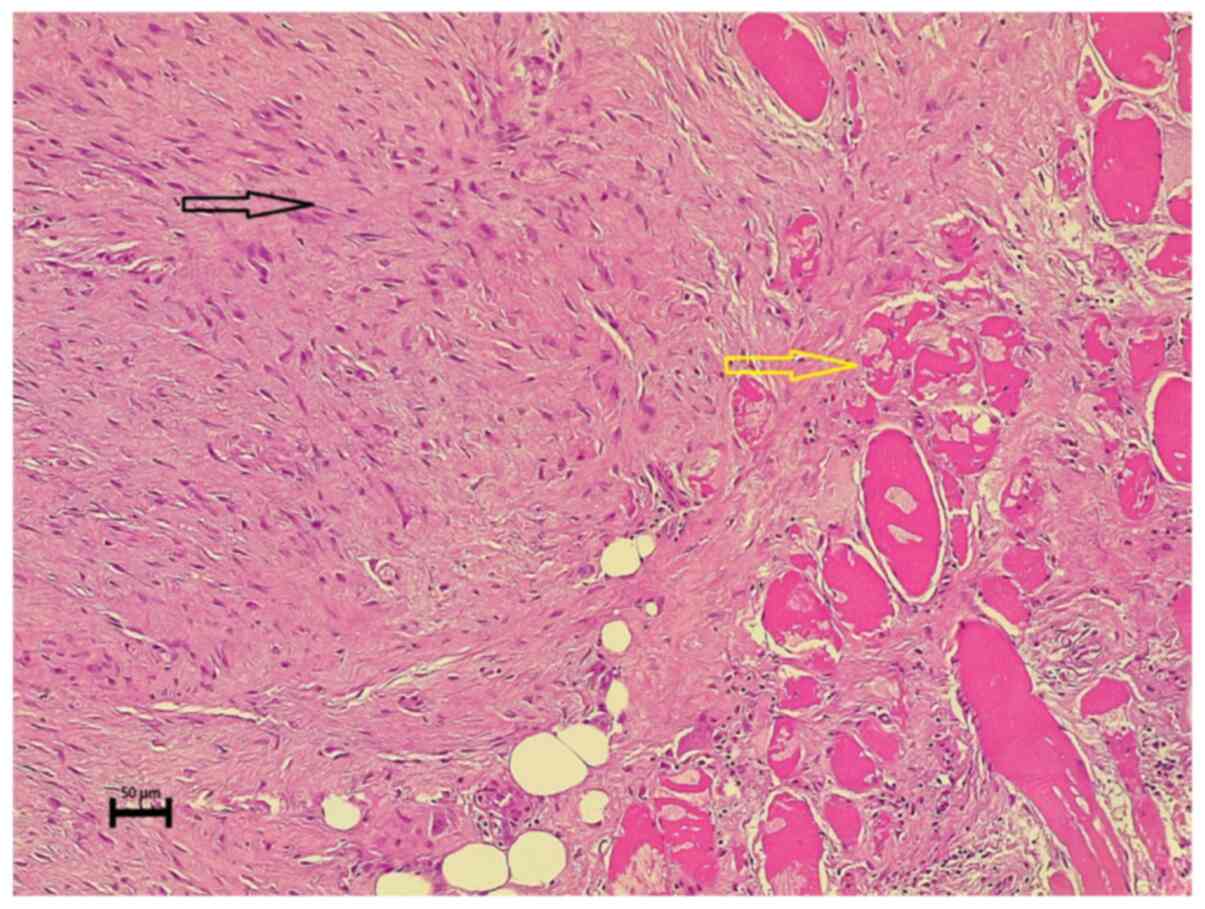
exposure history and a histopathological examination (Fig. 1), and details of the
characteristics of primary and recurrent tumors.
For histopathological analysis, the sections
(5-µm-thick) were paraffin-embedded and fixed with 10% neutral
buffered formalin at room temperature for 24 h. The sections were
then stained with hematoxylin and eosin (Bio Optica Co.) for 1-2
min at room temperature. They were then examined under a light
microscope (Leica Microsystems GmbH).
Inclusion and exclusion criteria
The present study included all patients with
extra-abdominal recurrent AF. Patients who do not return for
follow-up are excluded from the study. An extensive literature
review was performed to identify related articles. Studies
published in predatory journals (not properly peer-reviewed) and
those with minimal improvement or persistent symptoms were
excluded. Predatory journals were defined according to Kscien's
criteria (8).
Analysis of patient data
The data were collected and organized using
Microsoft Excel 2019. The Statistical Package for Social Sciences
25.0 software (IBM Corp.) was used to qualitatively analyze
(descriptive analysis) the data. The data are presented as
frequencies, mean, median and range.
Results
A total of 9 patients with recurrent AF were
included in the present study. The demographic data and clinical
characteristics of the patients with primary tumors are presented
in Table I. The patients varied in
age from 7 to 60 years of age, with a mean and median age of 29 and
30 years, respectively. In total, two thirds of the cases (n=6;
66.67%) were female. A negative previous medical history was
reported in 7 cases (77.7%), and diabetes and hypertension were
reported in 1 case (11.1%); migraines were also reported in 1 case
(11.1%). The previous surgical history was negative in 4 cases
(44.4%), 2 cases had a history of cesarean section (22.2%), 1 case
had a history of hemorrhoidectomy (11.1%), and another one had a
history of pilonidal sinus disease. Overall, only 1 case (11.1%)
had a family history of breast fibromatosis. The upper extremities
were the site of primary tumors in 3 cases (33.3%), the lower
extremities in 3 cases (33.3%), the chest wall in 2 cases (22.2%)
and the lower back in 1 case (11.1%). The most common symptom of
the primary tumors was pain at the tumor site (n=8; 88.9%). All
primary tumors were surgically removed. In primary resection, the
resection margin was positive in 3 cases (33.3%), negative in 2
cases (22.2%) and was undetermined in 4 cases (44.4%). Only 1 case
(11.1%) of surgical site infection was reported. Following primary
tumor excision, only 1 case (11.1%) underwent radiotherapy. Three
cases with a positive resection margin did not undergo adjuvant
radiotherapy, and as primary resection was not performed at
Orthopedic Clinic at Smart Health Tower for these 3 cases
(outpatients), the exact reason for this was not known (patients
may have not agreed to this). Another case rejected adjuvant
radiotherapy following recurrent resection.
 | Table IThe demographic data and clinical
characteristics of the patients with primary tumors. |
Table I
The demographic data and clinical
characteristics of the patients with primary tumors.
| Patient no. | Age, years | Sex | PMH | PSH | FH | Site | Presentation | Management | Size of tumor
(cm) | Resection
margin | Residual tumor (R)
classification | Complications | Radiotherapy |
|---|
| 1 | 27 | F | -ve | -ve | -ve | Left-side chest
below axilla | Severe left arm
pain | Excision | 4 | +ve | R1 | -ve | -ve |
| 2 | 30 | M | -ve | PNS | -ve | Upper left chest
wall | Upper left side
chest pain radiating to arm | Excision | 8 | +ve | R1 | -ve | -ve |
| 3 | 60 | F | HTN, DM | C/S,
Hemorrhoidectomy | -ve | Medial aspect of
right leg | Mild right leg pain
and numbness | Excision | 9 | -ve | Rxa | -ve | +ve |
| 4 | 46 | F | Migraine | -ve | -ve | Left hand | Mild left-hand
pain, numbness, and weakness | Excision | 3 | Unknown | Rxa | -ve | -ve |
| 5 | 14 | M | -ve | -ve | Breast fibroma | Left paraspinal
(lumbar) area | Mild back pain and
swelling | Excision | 3.4 | +ve | R2 | Infection | -ve |
| 6 | 30 | F | -ve | C/S | -ve | Right arm | Right arm pain,
numbness, and ecchymosis | Excision | 8 | Unknown | R2 | -ve | -ve |
| 7 | 14 | M | -ve | Tonsillectomy | -ve | Left gluteal
area | Mild left gluteal
pain | Excision | 6 | Unknown | R2 | -ve | -ve |
| 8 | 7 | F | -ve | -ve | -ve | Right gluteal
area | Swelling | Excision | N/A | -ve | Rxa | -ve | -ve |
| 9 | 35 | F | N/A | N/A | N/A | Dorsal aspect of
right hand | Swelling | Excision | N/A | Unknown | R1 | -ve | -ve |
The time interval between the primary tumor and the
recurrent presentation was 28 months, ranging from 8 to 84 months.
The clinical characteristics of patients with recurrent tumors are
presented in Table II. In 6 cases
(66.7%), the tumor was located in the upper and lower extremities,
in 2 cases (22.2%) it was located in the chest, and in 1 case it
was located (11.1%) in the back. Pain was the most common
presenting symptom in 6 cases (66.7%), followed by a palpable mass
in 3 cases (33.3%). The recurring tumor was completely surgically
removed in all patients. The resection margin was positive in 4
cases (44.4%), negative in 2 cases (22.2%) and undetermined in the
remaining cases. As regards the post-operative complications of
recurring tumor resection, 1 patient (11.1%) had delayed wound
healing, 1 patient (11.1%) had a surgical site infection and 1
patient (11.1%) had a femoral nerve injury. Following the removal
of the recurrent tumor, 5 patients (55.6%) underwent radiation.
Each patient was subjected to a careful 3-month follow-up for
further recurrences. The follow-up of the cases revealed a good
prognosis in all cases.
 | Table IIThe clinical characteristics of
patients with recurrent tumors. |
Table II
The clinical characteristics of
patients with recurrent tumors.
| Patient no. | Interval between
primary and recurrence (months) | Site of tumor | Presentation | Management | Size of tumor
(cm) | Resection
margin | Residual tumor (R)
classification | Radiotherapy | Complication |
|---|
| 1 | 12 | Left infrascapular
region | Left arm pain | Excision | 7.6 | Positive | R2 | No | Delay wound
healing |
| 2 | 18 | Upper left chest
wall | Swelling | Excision | 4.1 | Negative | R0 | Yes | Negative |
| 3 | 30 | posterior aspect of
right distal thigh and popliteal fossa | Swelling | Excision | N/A | Unknown | Rxa | No | Surgical site
Infection |
| 4 | 8 | Left hand | Severe left-hand
pain, numbness and weakness | Excision | 4.5 | Unknown | Rxa | Yes | Negative |
| 5 | 12 | Left paraspinal
(lumbar) area | Mild back pain and
mass | Excision | N/A | Unknown | R2 | No | Negative |
| 6 | 48 | Right arm | Right arm pain,
numbness, and ecchymosis | Excision | 12 | Positive | R2 | Yes | Negative |
| 7 | 84 | Left gluteal
area | Swelling | Excision | 9.5 | Positive | R2 | Yes | Femoral nerve
injury |
| 8 | 14 | Right gluteal
area | Swelling | Excision | 4.8 | Negative | Rxa | No | Negative |
| 9 | Unknown | Dorsal aspect of
right hand | Painful mass | Excision | 5 | Positive | R1 | Yes | Negative |
Discussion
Under normal physiological conditions, fibroblasts
play a critical role in the healing process and the preservation of
vital organs, such as the lungs, liver, blood vessels, heart and
kidneys; however, when specific cells acquire gene mutations,
neoplasms can form, leading to the emergence of AF (9). The World Health Organization (WHO)
defines AF as an intermediate soft tissue tumor with clonal
fibroblastic proliferation originating from deep soft tissue and
the potential to infiltrate locally (2). Fibromatoses are divided into three
categories based on anatomic location: Intra-abdominal, abdominal
wall and extra-abdominal (10).
Extra-abdominal AFs are rare, slow-growing tumors with a varying
biological behavior (4). The
differentiation between intra-abdominal and extra-abdominal AFs is
therapeutically essential due to variations in etiology, biological
behavior and morbidity associated with surgical excision (6).
The peak incidence of AF occurs between the ages of
25 and 35 years, with a predominance observed in females (11). The most common symptom is a
painless, growing mass; however, symptoms such as neurologic
problems, joint stiffness, or gastrointestinal discomfort may also
emerge as a result of tumor growth (9). Extra-abdominal head and neck lesions
are more aggressive than other extra-abdominal lesions, resulting
in significant bone damage and erosion of the base of the skull.
They can occasionally expand to the trachea. Extra-abdominal tumors
affecting the limbs may cause loss of function as a result of
extensive resection, local recurrence and radiation therapy
(4). This tumor is recognized as a
highly unpredictable tumor with high rates of local recurrence
(11). The time to relapse in the
initial tumor varies from 8 to 23 months (median, 17.3 months),
whereas the time to relapse in the recurrent tumor ranges from 3 to
26 months (median, 14.8 months) (12). In the present study, the
female-to-male ratio was 3:1. Pain was the most prevalent
presenting symptom in 66.7% of the cases, followed by a palpable
mass in 33.3%. The mean interval from primary to recurrent
presentation was 28 months.
Although computed tomography reveals the size of the
tumor and its association with the neurovascular systems, magnetic
resonance imaging (MRI) is the modality of choice for diagnosing
and evaluating the extent of the tumor and the course of the
disease following therapy. The features of an MRI vary.
Heterogeneous variations are typical, depending on the collagen
distribution and cellularity of the lesions. In both T1- and
T2-weighted sequences, the lesions may be hypo- or hyper-intense
compared to surrounding muscles or adipose tissues, with sharp or
poorly demarcated margins (4,13).
All patients in the present study were diagnosed and staged using
MRI.
In recent years, urgent surgical therapy for
extraperitoneal AF has not been recommended. According to the
European Guidelines, the ‘watchful waiting’ strategy is the
preferred therapy for asymptomatic AF (9,14).
However, as the existence of the tumor is a pathological state in
itself, some patients seek surgical therapy even when there are no
obvious symptoms or disabilities caused by the tumor. AF can be
treated with surgery, radiotherapy or chemotherapy; however, there
is limited information available on the selection process for the
appropriate treatment for each particular patient (15). In all age groups, full-margin
surgical resection remains the treatment of choice for local tumor
management. However, the invasive nature of AF renders complete
removal difficult without compromising neighboring tissues,
resulting in considerable functional impairment (3). Radiotherapy can be a successful
therapeutic option, and it can be used as the only treatment for
resected tumors with local recurrences, unresectable tumors and in
individuals who refuse surgery. Radiotherapy has lately been
established as a key therapeutic option for individuals who have
relapsed following surgery (16).
In the present study, all patients underwent complete tumor
resection, followed by radiation in 5 cases.
Non-steroidal anti-inflammatory agents, such as
indomethacin or sulindac, have either been utilized as single
agents or in combination with anti-estrogens in the treatment of
AF, with varying response rates reported based on limited series
and case reports (4). Chemotherapy
has infrequently been used due to the indolent and
non-metastasizing nature of extra-abdominal AF. Agents such as
doxorubicin, methotrexate, vincristine, dactinomycin,
cyclophosphamide, vinblastine, hormonal therapies and kinase
inhibitor drugs have all been documented with varying degrees of
efficacy (17). According to a
previous systematic review, cryoablation is an appropriate
palliative therapeutic option as it is associated with a low risk
of complications and delivers a long-term tumor response and
symptom alleviation (18).
High-intensity focused ultrasound is another therapeutic option
that has exhibited immense potential as a treatment option for
desmoid tumors. While it may have some adverse effects, it stands
out for its precise removal capability and minimal invasiveness
(19). However, further
investigations are required to prove its effectiveness as a
curative method. Furthermore, radiofrequency ablation is a
minimally invasive treatment option commonly used to treat a number
of benign lesions and unresectable malignant tumors by inserting a
fine needle electrode into masses with imaging guidance. This
treatment modality has also exhibited promising outcomes in several
cases; however, it is associated with several side-effects, such as
cellulitis and soft tissue necrosis (19).
To date, the patient's features and therapeutic
results of recurrent fibromatosis have not been adequately
addressed. In cases with recurrent pathology, surgical excision has
been associated with a relatively high risk of re-recurrence of
almost 90%, despite the fact that the chance of establishing a
clean margin does not vary from the first surgical resection. The
surgical margin quality following re-resection is unrelated to the
frequency of relapse, presumably due to microscopic residual
disease in the surgical bed after the original resection. Along
with the high risk of failure, surgery continues to play a role in
first-time recurrence; however, it does not appear to provide a
meaningful benefit when patients return with subsequent recurrences
(20).
Previous research has highlighted age, sex, tumor
size, location and the surgical margin as key risk factors for
surgical outcomes in patients with AF (21). Some researchers have demonstrated
that certain genetic variables may be more predictive of AF
recurrence as opposed to the resection margin quality (22). Timbergen et al (23) reported an association of the CTNNB1
mutation with surgical outcomes in an analysis of previously
published studies and found that the S45F mutation was associated
with an increased risk of local recurrence. Garvey et al
(22) discovered that the 45F
mutation was the only risk factor that was statistically predictive
of recurrence. Although the S45F mutation appears to be related to
a significant recurrence rate, it would be a weaker factor than the
tumor site if included in the nomogram (15).
There is much debate over whether surgical resection
margins have prognostic value for AF recurrence. Since AF is a very
infiltrative tumor, assessing the margin status is relatively
challenging (5). The previous
study by Cates and Stricker (24)
hypothesized that some ‘close but negative’ margins were definitely
positive. They also found that a positive or near-positive (1 mm)
resection margin was an independent predictor for local recurrence
(24). Two recent studies with
large patient populations yielded conflicting results. Zeng et
al (25) studied patients with
AF who had macroscopically complete resection, and found that the
R1 resection status was a factor associated with poorer
recurrence-free survival. Nevertheless, in the study by Crago et
al (15), which included the
largest cohort of patients with complete macroscopic resection, the
margin status was not a predictor associated with recurrence.
According to a previous study, the microscopic
negative margin state significantly affects the recurrence rate,
and the recurrence rate is considerably reduced following full
resection with negative margins for both original and recurrent
tumors (6). These findings suggest
that a full resection is the targeted outcome, and even recurrence
rates in patients with a primary tumor are still very low following
an R1 resection (6). By contrast,
other previous large retrospective studies found no influence of
the margin status on recurrence. However, these studies did not
distinguish between intra-abdominal and extra-abdominal AF or
account for varying adjuvant treatments (26,27).
Age is also a significant predictive factor associated with the
biological processes of AF. In their study, He et al
(5) found that younger patients
had a greater probability of local recurrence.
The location of the tumor is another factor
associated with a greater likelihood of recurrence. It has been
previously demonstrated that the extremities are an independent
risk factor related to the local recurrence of AF (15). Tsagozis et al (20) also discovered that extremity
lesions, particularly those of the lower extremities, had a greater
probability of recurrence than trunk and pelvic lesions. This may
be partially due to the proximity to neurovascular systems and the
difficulty in achieving adequate resection margins in such
locations (28). The majority of
the patients (n=6; 66.7%) in the present study experienced AF of
the extremities.
A larger tumor size is another debatable risk factor
that has previously been identified. Several researchers have
discovered that the size of the tumor increases the likelihood of
recurrence (25). However, others
have not found such an association (29). According to the study by Wang et
al (9), a larger primary tumor
size was related to a higher likelihood of recurrence and a shorter
time to recurrence. Additionally, as larger lesions tended to
infiltrate adjacent vessels and nerves, the lesion was not removed
completely during surgery in order to protect local tissue
function, and some tumor cells remained in the surrounding tissue,
resulting in a short-term recurrence (9). Another study discovered that tumor
size (5 or >5 cm) had a substantial effect on recurrence
(10).
Adjuvant radiotherapy is a controversial subject in
the treatment of AF since earlier research findings vary; some
studies have found that radiation is related to improved local
control of AF (25,30), while other scholars have found no
effect (15). According to a
previous study, adjuvant radiation appears to minimize the
incidence of local recurrence following surgical resection with
positive resection margins (6).
Its efficacy in minimizing local recurrence is particularly
prominent following the R1/R2 resection of recurrent AF and appears
to have no additional benefit when surgical resection is complete
at the time of the histological analysis (6). Guadagnolo et al (31) studied patients with primary and
recurrent AF in whom adjuvant radiation obtained a 10-year local
control rate of 78%. In their systematic review, Yao et al
(32) concluded that surgery plus
adjuvant radiation decreased recurrence compared to surgery alone.
Adjuvant radiation was thus suggested for all patients, even those
with negative resection margins (32). Radiotherapy with doses ≥60 Gy has
been demonstrated to enhance local control rates by 80 to 88%
(31).
Moreover, several studies have found that radiation
efficacy is associated with margin status (6,33,34).
A previous study found that in patients with positive margins,
post-operative adjuvant radiation enhanced local control and
lowered the recurrence rate compared to surgery alone (33). A previous meta-analysis found that
although adjuvant radiation was not effective for patients with
negative margins, it may enhance local control and prevent
recurrence in individuals with inadequate resection (6). The National Comprehensive Cancer
Network (NCCN) guidelines recommend adjuvant radiation for patients
with R1 resection and definitive radiotherapy for those with R2
resection (34). The apparent
limitations of the present study were the small sample size, the
lack of a genetic profile of patients to identify the role of
genetic factors in disease emergence and the lack of any
explanation regarding the etiology of the cases.
In conclusion, fibromatosis is a rare, locally
invasive fibroblastic tumor with no metastatic potential. Despite
the fact that several therapeutic approaches have been described in
the literature, there is a significant likelihood of recurrence
following resection. Further studies are thus required to further
determine the management and risks of recurrence.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SKA provided major contributions to the study
concept and the final approval of the manuscript. FHK and MNH were
involved in the literature review, in the design of the study, and
in the writing of the manuscript. AMA was the histopathologist who
examined the specimen. SAA, SHT, CSO, RJR, FHF, BAA and SHM were
involved in critically revising the manuscript and in data
interpretation. All authors have read and approved the final
manuscript. SAA and SKA confirm the authenticity of all the raw
data. All authors agreed to be accountable for all aspects of the
work in ensuring that questions related to the accuracy or
integrity of any part of the work are appropriately investigated
and resolved.
Ethics approval and consent
The present study was approved by the Sulaimani
University Ethics Committee (2023/no. 20). All patients or the
parents of patients (for cases <18 years old) provided signed
consent for their data to be published.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Machado V, Troncoso S, Mejías L, Idoate MÁ
and San-Julián M: Risk factors for local recurrence of
fibromatosis. Rev Esp Cir Ortop Traumatol. 61:82–87.
2017.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
2
|
Hammood ZD, Salih AM, Kakamad FH, Abdullah
AM, Ali BS and Pshtiwan LR: Desmoid fibromatosis of the breast; a
rare case report. Int J Surg Case Rep. 87(106363)2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Eastley N, Aujla R, Silk R, Richards CJ,
McCulloch TA, Esler CP and Ashford RU: Extra-abdominal desmoid
fibromatosis-a sarcoma unit review of practice, long term
recurrence rates and survival. Eur J Surg Oncol. 40:1125–1130.
2014.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Papagelopoulos PJ, Mavrogenis AF,
Mitsiokapa EA, Papaparaskeva KT, Galanis EC and Soucacos PN:
Current trends in the management of extra-abdominal desmoid
tumours. World J Surg Oncol. 4(21)2006.PubMed/NCBI View Article : Google Scholar
|
|
5
|
He XD, Zhang YB, Wang L, Tian ML, Liu W,
Qu Q, Li BL, Hong T, Li NC and Na YQ: Prognostic factors for the
recurrence of sporadic desmoid-type fibromatosis after
macroscopically complete resection: Analysis of 114 patients at a
single institution. Eur J Surg Oncol. 41:1013–1019. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Janssen ML, Van Broekhoven DL, Cates JM,
Bramer WM, Nuyttens JJ, Gronchi A, Salas S, Bonvalot S, Grünhagen
DJ and Verhoef C: Meta-analysis of the influence of surgical margin
and adjuvant radiotherapy on local recurrence after resection of
sporadic desmoid-type fibromatosis. Br J Surg. 104:347–357.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Molloy AP, Hutchinson B and O'toole GC:
Extra-abdominal desmoid tumours: A review of the literature.
Sarcoma. 2012(578052)2012.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Muhialdeen AS, Ahmed JO, Baba HO, Abdullah
IY, Hassan HA, Najar KA, Mikael TM, Mustafa MQ, Mohammed DA, et al:
Kscien's List; A New Strategy to Discourage Predatory Journals and
Publishers (Second Version). Barw Med J. 1:1–3. 2023.
|
|
9
|
Wang J, Huang Y, Sun Y, Ge Y and Zhang M:
Value of imaging findings in predicting post-operative recurrence
of desmoid-type fibromatosis. Oncol Lett. 19:869–875.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Niu X, Jiang R and Hu C: Radiotherapy in
the treatment of primary or recurrent unresectable desmoid tumors
of the neck. Cancer Invest. 37:387–392. 2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sedaghat S, Sedaghat M, Krohn S, Jansen O,
Freund K, Streitbürger A and Reichardt B: Long-term diagnostic
value of MRI in detecting recurrent aggressive fibromatosis at two
multidisciplinary sarcoma centers. Eur J Radiol.
134(109406)2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Wang YF, Guo W, Sun KK, Yang RL, Tang XD,
Ji T and Tang S: Postoperative recurrence of desmoid tumors:
Clinical and pathological perspectives. World J Surg Oncol.
13(26)2015.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Braschi-Amirfarzan M, Keraliya AR,
Krajewski KM, Tirumani SH, Shinagare AB, Hornick JL, Baldini EH,
George S, Ramaiya NH and Jagannathan JP: Role of imaging in
management of desmoid-type fibromatosis: A primer for radiologists.
Radiographics. 36:767–782. 2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Eastley N, McCulloch T, Esler C, Hennig I,
Fairbairn J, Gronchi A and Ashford R: Extra-abdominal desmoid
fibromatosis: A review of management, current guidance and
unanswered questions. Eur J Surg Oncol. 42:1071–1083.
2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Crago AM, Denton B, Salas S, Dufresne A,
Mezhir JJ, Hameed M, Gonen M, Singer S and Brennan MF: A prognostic
nomogram for prediction of recurrence in desmoid fibromatosis. Ann
Surg. 258:347–253. 2013.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Choi SH, Yoon HI, Kim SH, Kim SK, Shin KH
and Suh CO: Optimal radiotherapy strategy for primary or recurrent
fibromatosis and long-term results. PLoS One.
13(e0198134)2018.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Wood TJ, Quinn KM, Farrokhyar F, Deheshi
B, Corbett T and Ghert MA: Local control of extra-abdominal desmoid
tumors: Systematic review and meta-analysis. Rare Tumors.
5(e2)2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Vora BMK, Munk PL, Somasundaram N,
Ouellette HA, Mallinson PI, Sheikh A, Abdul Kadir H, Tan TJ and Yan
YY: Cryotherapy in extra-abdominal desmoid tumors: A systematic
review and meta-analysis. PLoS One. 16(e0261657)2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Zhang Z, Shi J, Yang T, Liu T and Zhang K:
Management of aggressive fibromatosis. Oncol Lett.
21(43)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tsagozis P, Stevenson JD, Grimer R and
Carter S: Outcome of surgery for primary and recurrent desmoid-type
fibromatosis. A retrospective case series of 174 patients. Ann Med
Surg (Lond). 17:14–19. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Nishida Y, Hamada S, Kawai A, Kunisada T,
Ogose A, Matsumoto Y, Matsumoto Y, Ae K, Toguchida J, Ozaki T, et
al: Risk factors of local recurrence after surgery in
extraabdominal desmoid-type fibromatosis: A multicenter study in
Japan. Cancer Sci. 111:2935–2942. 2020.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Garvey PB, Booth JH, Baumann DP, Calhoun
KA, Liu J, Pollock RE and Butler CE: Complex reconstruction of
desmoid tumor resections does not increase desmoid tumor
recurrence. J Am Coll Surg. 217:472–480. 2013.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Timbergen MJM, Colombo C, Renckens M, Kim
HS, Rosmalen JV, Salas S, Mullen JT, Colombo P, Nishida Y, Wiemer
EAC, et al: The prognostic role of β-catenin mutations in
desmoid-type fibromatosis undergoing resection only: A
meta-analysis of individual patient data. Ann Surg. 273:1094–1101.
2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Cates JM and Stricker TP: Surgical
resection margins in desmoid-type fibromatosis: A critical
reassessment. Am J Surg Pathol. 38:1707–1714. 2014.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zeng WG, Zhou ZX, Liang JW, Hou HR, Wang
Z, Zhou HT, Zhang XM and Hu JJ: Prognostic factors for desmoid
tumor: A surgical series of 233 patients at a single institution.
Tumour Biol. 35:7513–7521. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Salas S, Dufresne A, Bui B, Blay JY,
Terrier P, Ranchere-Vince D, Bonvalot S, Stoeckle E, Guillou L, Le
Cesne A, et al: Prognostic factors influencing progression-free
survival determined from a series of sporadic desmoid tumors: A
wait-and-see policy according to tumor presentation. J Clin Oncol.
29:3553–3558. 2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Gronchi A, Colombo C, Le Péchoux C, Dei
Tos AP, Le Cesne A, Marrari A, Penel N, Grignani G, Blay JY, Casali
PG, et al: Sporadic desmoid-type fibromatosis: A stepwise approach
to a non-metastasising neoplasm-a position paper from the Italian
and the French Sarcoma Group. Ann Oncol. 25:578–583.
2014.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Horsley M, Arshad MS and Khan T:
Fibromatosis: A review of the risk factors for recurrence and
outcomes. Acta Orthop Belg 86 e-supplement. 1:55–60. 2020.
|
|
29
|
Peng PD, Hyder O, Mavros MN, Turley R,
Groeschl R, Firoozmand A, Lidsky M, Herman JM, Choti M, Ahuja N, et
al: Management and recurrence patterns of desmoids tumors: A
multi-institutional analysis of 211 patients. Ann Surg Oncol.
19:4036–4042. 2012.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Gluck I, Griffith KA, Biermann JS, Feng
FY, Lucas DR and Ben-Josef E: Role of radiotherapy in the
management of desmoid tumors. Int J Radiat Oncol Biol Phys.
80:787–792. 2011.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Guadagnolo BA, Zagars GK and Ballo MT:
Long-term outcomes for desmoid tumors treated with radiation
therapy. Int J Radiat Oncol Biol Phys. 71:441–447. 2008.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Yao X, Corbett T, Gupta AA, Kandel RA,
Verma S, Werier J and Ghert M: A systematic review of active
treatment options in patients with desmoid tumours. Curr Oncol.
21:e613–e629. 2014.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Mullen JT, DeLaney TF, Kobayashi WK,
Szymonifka J, Yeap BY, Chen YL, Rosenberg AE, Harmon DC, Choy E,
Yoon SS, et al: Desmoid tumor: Analysis of prognostic factors and
outcomes in a surgical series. Ann Surg Oncol. 19:4028–4035.
2012.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Yang T, Liu H, Liao Z, Zhang C, Xiang L
and Yang J: Postoperative adjuvant radiotherapy can delay the
recurrence of desmoid tumors After R0 resection in certain
subgroups. Front Surg. 8(697793)2021.PubMed/NCBI View Article : Google Scholar
|