Introduction
Globally, gastric cancer ranks fifth in terms of
cancer incidence and fourth in terms of mortality (1) and it is the second most common cancer
and third highest cause of deaths for patients with cancer in Japan
(2). Although the 5-year survival
rate for all patients is >60%, the prognosis for patients with
recurrent or metastatic disease remains poor, with a median overall
survival (OS) of 6-13 months (2,3).
Immune checkpoint inhibitors have become the
standard treatment option for recurrent or metastatic gastric
cancer (4,5). Nivolumab is a fully humanized
antibody drug active against programmed cell death-1 (PD-1).
Nivolumab treatment increased survival in patients participating in
the ATTRACTION-2 trial, which included placebo-controlled patients
with advanced or recurrent gastric cancer who experienced standard
second-line treatment failure (6).
Nivolumab monotherapy was approved for use in Japan in September
2017 and was subsequently recommended as a third-line therapy for
gastric cancer. (4,5). Trifluridine/tipiracil (FTD/TPI) was
introduced as a salvage-line treatment option in August 2019 in
Japan (7,8). Currently, nivolumab in combination
with platinum and fluoropyrimidine is recommended as the first-line
treatment for HER2-negative patients with gastric cancer
based on the results of the CheckMate 649 and ATTRACTION-4 trials,
following its approval in Japan in November 2021 (5,9,10).
Predicting the efficacy of immune checkpoint
inhibitors is an important clinical challenge currently being
explored. The Checkmate 649 and ATTRACTION-4 trials reported that
programmed death ligand 1 (PD-L1) expression levels in tumor cells
and tumor-associated immune cells, also known as the combined
positive score, correlated with patient prognosis (9,10).
However, the results from the ATTRACTION-2 trial, which evaluated
nivolumab monotherapy as a third-line treatment, reported that
PD-L1 expression did not correlate with patient prognosis (6). Pembrolizumab, a PD-1 antibody similar
to nivolumab, has shown clinical benefits in solid tumors,
including gastric cancer cases with microsatellite instability-high
(MSI-H) or mismatch repair-deficient (dMMR) tumors, as well as
those with high tumor mutation burden (TMB-H) (11-13).
However, MSI-H/dMMR and TMB-H are relatively uncommon in gastric
cancer, occurring in 6.7 and 5.2% of cases, respectively (14,15)
Other therapeutic strategies, such as chemotherapy, also target the
inflammatory micro-tumor environment, which suggests that the
inflammatory micro-tumor environment may be a predictor of patient
response to treatment with immune checkpoint inhibitors (16).
Several types of inflammation-based prognostic
markers, based on a combination of blood-based parameters, have
been studied for their association with clinical outcomes in
patients with various types of cancer, including gastric cancer
(17,18). In patients with cancer treated with
immune checkpoint inhibitors, serum albumin levels (19), the Glasgow prognostic score (GPS)
(20), neutrophil-lymphocyte ratio
(NLR) (21) and lung immune
prognostic index score (21,22)
have been reported to be useful in predicting prognosis. These
inflammation-based prognostic markers are readily accessible;
however, numerous markers are in disarray, and it is unclear which
markers should be prioritized in clinical decision making,
particularly when using immune checkpoint inhibitors (23-38).
In addition, while prognostic tools, such as the lung immune
prognostic index (LIPI), have been developed in the era of immune
checkpoint inhibitors (37), it
has not been thoroughly reported whether they are superior to other
existing markers.
Real-world data are the routine accumulation of
specific information on patient health status and treatment through
established mechanisms, such as the acquisition of electronic
medical records (39). Although
there are limitations in regard to the use of this type of data,
due to incomplete datasets and heterogeneity in patient
backgrounds, their utility in bridging the gap between clinical
trials and routine clinical practice has been previously reported
(40-44).
The Tokushukai Group is the largest medical corporation in Japan
and includes 75 hospitals. As all the hospitals in the Tokushukai
Group use electronic medical records and are connected by a closed
network, it is possible to simultaneously collect information from
all of these hospitals. The present real-world clinical study aimed
to utilize data from the Tokushukai Group medical database to
assess and compare correlations between inflammation-based
prognostic markers reported in patients with advanced or recurrent
gastric cancer who received nivolumab monotherapy.
Materials and methods
Ethical approval and clinical trial
registration
The Tokushukai Real-World Data project is a
nationwide retrospective cohort study conducted across the
Tokushukai Medical Group hospitals in Japan. It encompasses 46
hospitals equipped with a chemotherapy protocol system and
Diagnosis Procedure Combination, totaling ~15,000 beds. The
methodology of the present study has been outlined in our
previously published study (45).
The present protocol adhered to ethical guidelines for medical and
biological research involving human subjects in Japan (46), as well as the principles of the
Declaration of Helsinki. The present study was approved by the
Ethics Committee of the Tokushukai Group in April 2020 (approval
no. TGE01427-024) and was registered with the UMIN Clinical Trial
Registry (http://www.umin.ac.jp/ctr/index.htm) under the trial
registration number UMIN000050590 on 15th March 2023. Patients were
informed about the present study using the opt-out patient consent
method.
Patients
The present study evaluated patients with
pathologically or radiologically confirmed advanced or recurrent
gastric cancer who were treated with nivolumab monotherapy as a
late-line chemotherapy, at Tokushukai Medical Group hospitals using
the same medical record system (e-Karte; version 2.2 and Newtons2;
version 2.2; Software Service Inc.) and chemotherapy protocol
system (srvApmDrop; version 3.0.522; Software Service Inc.),
between September 1, 2017 and March 31, 2020.
Patients with histological diagnoses other than
adenocarcinoma were excluded from further analysis. Additional key
exclusion criteria were the presence of active secondary cancer,
inadequate treatment history and missing fundamental patient data,
such as body weight and height.
Data collection
The present study evaluated eligible patients
identified using electronic medical record data. Patient
information, such as age, sex, body height, body weight, body
surface area, BMI, Brinkman Index and the latest data on
confirmation of survival or death (registration of survival or
death in the electronic medical record), survival outcomes and
diagnosis on medical receipt, which is a document that outlines the
medical treatments received, costs incurred and insurance coverage
applied in Japan, were extracted from the medical record system.
Blood test data within 14 days of nivolumab treatment initiation
were extracted from the electronic medical records. Information
related to previous chemotherapy regimens, the start and end dates
of chemotherapy and Eastern Cooperative Oncology Group performance
status (PS) score (on a scale of 0-5, with higher scores indicating
greater disability) were extracted from the chemotherapy protocol
system. The linked cancer registry information, including
diagnostic information (tumor site, pathology and stage), treatment
details (surgery, endoscopic procedure, radiotherapy and systemic
therapy) and prognosis (final date of survival confirmation, date
of death and cause of death) were extracted from the National
Cancer Registry Data of Japan (2,47).
The date of the last confirmed survival was extracted from both the
cancer registry and electronic medical records and the later date
was used. Patients with an inadequate treatment history, such as
previous or subsequent cancer treatment outside of Tokushukai
Medical Group hospitals or whose records reported no detailed
treatment information, were excluded from the study. Patients with
missing laboratory data were also excluded.
Statistical analysis
Basic statistics, such as absolute and relative
frequencies for categorical variables, maximum and minimum values
and medians for continuous and discrete variables, were obtained to
summarize the distribution of variables related to patient
background factors, complications and other prognostic factors.
The primary endpoint evaluated in the present study
was OS, which was defined as the time from the date of nivolumab
treatment initiation to the date of death or final survival
confirmation. Censored cases included patients who were alive at
the study end-date or dropped out of the study for any reason. The
secondary endpoint was time to treatment failure (TTF), which was
defined as the duration from the start of nivolumab treatment to
discontinuation of the treatment for any reason. For each
prognostic marker tested, Kaplan-Meier curves for the occurrence of
events associated with the study endpoint were obtained and
log-rank and chi-squared tests were performed.
Cox regression analysis was performed using all
prognostic factors at the start of nivolumab treatment (such as
age, sex, BMI, Brinkman Index, PS, location of the primary site,
stage, histology, HER2 status, previous surgery and previous
radiotherapy) to examine their degree of impact on OS. Estimated
hazard ratios (HRs) and 95% CI for each prognostic factor in
association with OS were calculated using univariate and
multivariate analyses. Subsequently, variable selection was
performed using the Akaike information criterion (AIC) to identify
useful background factors. A total of 17 inflammation-based
prognostic markers were evaluated (Table SI). For each of these markers, the
impact on the survival rate, after adjusting for background
factors, was compared using concordance and AIC analyses. The
concordance and AIC of each marker on TTF were also examined.
Survival analyses were performed using OS and TTF. A
stratified Cox proportional model was used to obtain adjusted
Kaplan-Meier survival curves for each prognostic marker, and its
significance was obtained using a likelihood ratio test. The null
hypothesis was that the item was not involved in the
goodness-of-fit of the model.
All analyses were performed using R (version 4.2.2;
R Foundation for Statistical Computing). All statistical
assessments were two-sided and P<0.05 was considered to indicate
a statistically significant difference. The present study was an
exploratory study and did not consider multiplicity.
Results
Patient characteristics
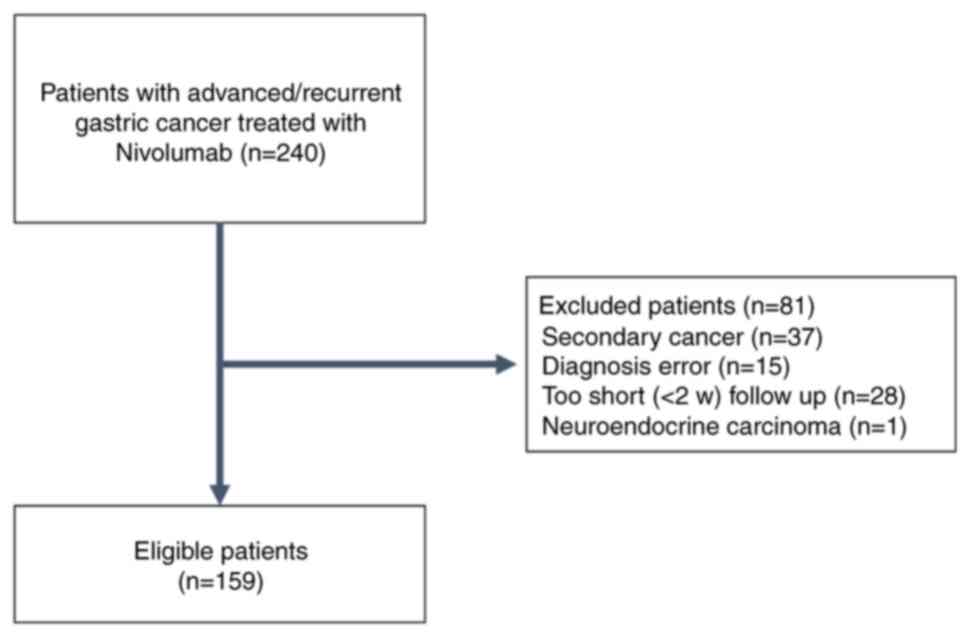
According to the aforementioned protocol, a total of
240 patients were identified, of whom 159 met the inclusion
criteria (Fig. 1; Table SII). Of the patients included in
the present study, 25% were aged >75 years and almost 60% had
primary metastatic cancer. Most patients received platinum,
fluoropyrimidine and taxane treatment, with a median of three prior
lines of systemic therapy (Table
SIII).
Survival
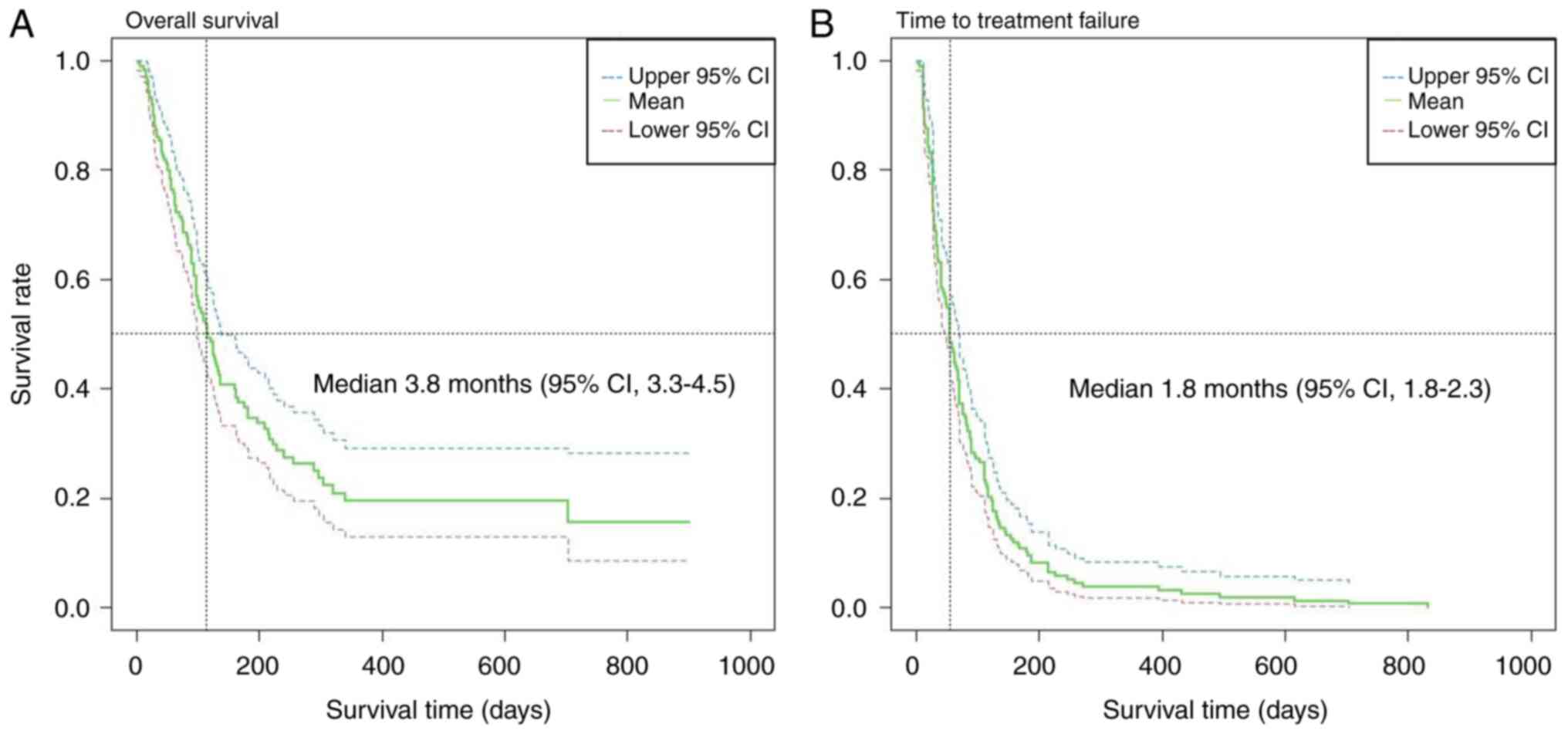
The OS and TTF were calculated using Kaplan-Meier
curves (Fig. 2). The median
follow-up period was 3.3 months (95% CI, 2.5-3.8) and the median OS
and TTF were 3.8 months (95% CI, 3.3-4.5) and 1.8 months (95% CI,
1.8-2.3), respectively. The 1- and 2-year survival rates were 19.5%
(95% CI, 13.0-29.2) and 15.6% (95% CI, 8.6-28.3), respectively.
Sequential systemic therapy was administered in 21.4% of patients,
which included taxanes (11.9%) and irinotecan (5.7%) (Table SIII). None of the patients
received FTD/TPI.
Cox regression analyses
Cox regression analyses demonstrated that no factors
that significantly affected patient prognosis were identified in
the univariate analysis (Table
SIV). As a substantial proportion of patient data were not
available (N/A), excluding these data could have affected the
accuracy of the analysis. Therefore, N/A data was treated as a
separate treatment group and included in the analyses.. The
multivariate analysis showed an improved prognosis in patients who
had received prior radiation therapy (HR, 0.22; 95% CI, 0.05-0.98).
Age, sex, tumor location, tumor stage and previous radiotherapy
treatment were selected as adjusting factors based on AIC
criterion.
Comparison of markers
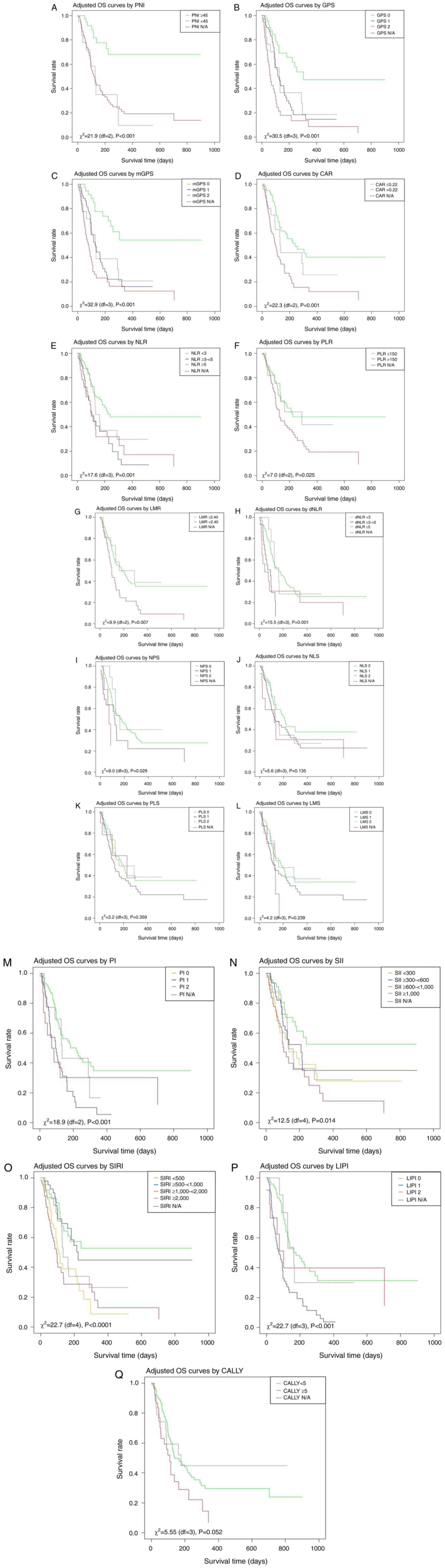
The concordance and AIC of the markers tested were
analyzed after adjusting for background factors, such as age, sex,
tumor location, tumor stage and previous radiotherapy, in relation
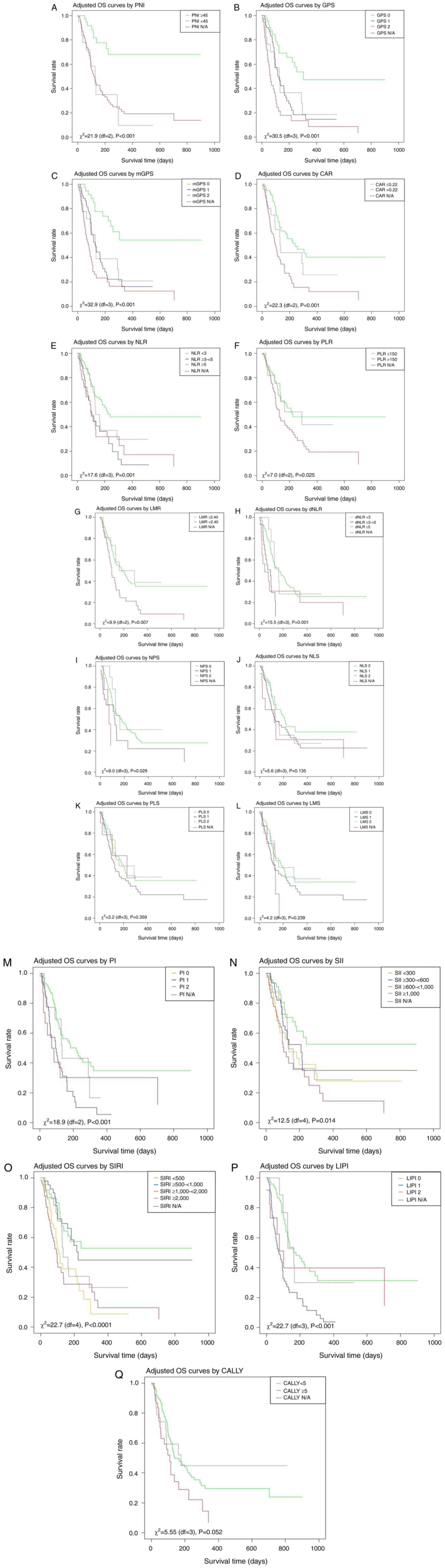
to both OS (Fig. 3; Table SV) and TTF (Fig. S1; Table SVI). Most of the markers tested
demonstrated a significant correlation with patient prognosis. The
marker modified GPS (mGPS) showed the strongest correlation with
prognosis, followed by GPS, which also exhibited a dose-response
relationship. The Cox model involving mGPS showed the highest
concordance and lowest AIC among all of the markers analyzed. The
marker that demonstrated the highest correlation with TTF was also
mGPS.
 | Figure 3OS based on different scores and
ratios. A log-rank test was used to calculate statistical
significance. (A) PNI, (B) GPS, (C) mGPS, (D) CAR, (E) NLR, (F)
PLR, (G) LMR, (H) dNLR, (I) NPS, (J) NLS, (K) PLS, (L) LMS, (M) PI,
(N) SII, (O) SIRI, (P) LIPI and (Q) CALLY. CRP, C-reactive protein,
df; degrees of freedom; OS, overall survival; PNI, prognostic
nutritional index; GPS, Glasgow prognostic score; mGPS, modified
GPS; CAR, CRP-to-albumin ratio; NLR, neutrophil-to-lymphocyte
ratio; PLR, platelet-to-lymphocyte ratio; LMR,
lymphocyte-to-monocyte ratio; dNLR, derived NLR; NPS,
neutrophil-platelet score; NLS, neutrophil-lymphocyte score; PLS,
platelet-lymphocyte score; LMS, lymphocyte-monocyte score; PI,
prognostic index; SII, systemic immune-inflammation index; SIRI,
systemic inflammation response index; LIPI, lung immune prognostic
index; CALLY, CRP albumin lymphocyte index. |
Discussion
The present study investigated the outcomes of
late-line nivolumab monotherapy in patients with advanced or
recurrent gastric cancer. The main aim of the present study was to
analyze 17 inflammation-based prognostic markers to identify
factors that correlated best with prognosis, thereby potentially
contributing to the future use of prognostic factors in clinical
practice. These findings demonstrated that mGPS exhibited the most
robust correlation with prognosis among the markers assessed, which
was consistent with our previous study in patients with
chemotherapy-naive metastatic pancreatic cancer (48). A strength of the present study was
the simultaneous evaluation of real-world data for the presence of
various inflammation-based markers in patients with advanced or
recurrent gastric cancer in the era of immune checkpoint
inhibitors. While previous studies have examined the accuracy of
similar markers (32,33), the present study included and
compared novel markers whenever possible. In addition, many of the
markers were reported prior to the use of immune checkpoint
inhibitors, and the efficacy of the markers in treatment with
immune checkpoint inhibitors was unclear.
In the ATTRACTION-2 trial, the median
progression-free survival and median OS for nivolumab as third-line
treatment were reported to be 1.6 and 5.3 months, respectively
(6). The 1- and 2-year survival
rates were 27.3 and 11.6%, respectively (49). In the present study, the median OS
was 3.8 months, with 1- and 2-year survival rates of 19.5 and
15.6%, respectively. The trends observed between these two studies
were similar; however, differences in the outcomes reported in
clinical trials may be attributed to variations in patient
characteristics and backgrounds between controlled trials and
real-world clinical practice. For example, the median age was 62
years in the ATTRACTION-2 trial, compared with 70 years in the
present study. In addition, patients were limited to PS 0 and 1 in
the ATTRACTION-2 study, whereas 12.6% of the patients in the
present study had PS 2. In the ATTRACTION-2 trial, 35.0% of the
patients received subsequent systemic therapy, compared with 21.4%
in the present study. Thus, patient conditions, including
performance status and comorbidities, were often poorer in actual
clinical practice compared with in clinical trials. Therefore,
median OS in the present study may have been shorter compared with
that reported in clinical trials. However, these findings suggest
that the results of the present study reflected actual clinical
practice (6).
In the present analysis, the only prognostic factor
that remained in the multivariate analysis was prior radiotherapy
treatment. The synergistic effects of radiotherapy and immune
checkpoint inhibitors has previously been reported in preclinical
studies (50,51). In addition, prior radiation therapy
has been reported to be an independent prognostic factor in
patients treated with nivolumab for non-small cell lung cancer
(52). Potential synergistic
mechanisms have been proposed between radiotherapy and immune
checkpoint inhibitors, with several key factors contributing to
this synergy. These include increased tumor immunogenicity,
enhanced infiltration of T cells into tumors and reversal of immune
suppression within the tumor microenvironment (53). In the present study, prior
radiotherapy had a protective effect in patients with gastric
cancer receiving nivolumab.
Among the 17 inflammation-based prognostic markers
analyzed, mGPS and GPS were most effective in predicting outcomes
in patients with gastric cancer undergoing nivolumab treatment. The
mGPS scores used in the present study were obtained from Japan,
where the cutoff value for C-reactive protein was reduced from
1.0-0.5 mg/dl. In a previous study, receiver operating
characteristic curves for serum C-reactive protein (CRP) and
albumin were generated to calculate the diagnostic cutoff point at
which survival could be most accurately assessed (25). The results showed that CRP had a
sensitivity of 79.5% and specificity of 51.1% when the cutoff value
was set at 0.5 mg/dl, and albumin had a sensitivity of 80.7% and
specificity of 36.7% when the cutoff value was set at 3.5 mg/dl. In
the present study, the mGPS had a HR of 3.28 (95% CI, 1.68-6.38)
for score 1 and a HR of 5.60 (95% CI, 2.90-10.80) for score 2,
which indicated that the HR increased with increasing mGPS score.
Similar associations were shown between GPS, HR and mGPS. The
utility of the GPS for predicting patient prognosis has been
previously reported. In the early 2010s, the Glasgow Inflammation
Outcome study examined the utility of the GPS and reported its
success compared with various biochemical tests and other major
inflammation-based prognostic markers, including the NLR (54-56).
In addition, in a previous systematic review, GPS was identified as
an independent prognostic factor in various types of cancers, both
operable and inoperable (57,58).
However, the evidence showing that GPS is superior to other markers
is primarily based on operable cases from the 2010s. Therefore, to
date, there has not been sufficient investigation into its
effectiveness in inoperable cancers treated with immune checkpoint
inhibitors. The present study demonstrated that GPS was useful in
patients receiving immune checkpoint inhibitors, and that the mGPS
developed in Japan is as useful as conventional GPS.
Notably, LIPI is a novel indicator that has shown
usefulness for predicting prognosis in patients treated with immune
checkpoint inhibitors (37). In
the present study, LIPI ranked fourth among 17 markers in terms of
concordance and AIC; however, it did not surpass mGPS or GPS. LIPI
was initially developed for lung cancer and has been validated
through a previous meta-analysis (59). Additionally, it has shown
prognostic value in metastatic renal cell carcinoma (60). However, its applicability to other
types of cancer, such as gastric cancer, has not yet been reported.
Nonetheless, the comprehensive comparison of these markers in the
era of immune checkpoint inhibitors, as conducted in the present
study, provided important insights that showed GPS as most useful
prognostic marker, out of the 17 analyzed. The findings of the
present study, which indicated that mGPS and GPS were the most
accurate predictors of prognosis in patients with advanced or
recurrent gastric cancer receiving nivolumab monotherapy, were
consistent with previous reports prior to the era of immune
checkpoint inhibitors (32,33).
These markers could potentially be used as prognostic tools in
routine clinical practice in the future.
The present study had a number of limitations.
First, although the study was designed to examine prognostic
factors in late-line nivolumab treatment, the results were of
limited value in clinical practice because nivolumab is now often
used as first-line therapy in patients with HER2-negative gastric
cancer. Therefore, the usefulness of this marker in patients
receiving concomitant chemotherapy as first-line therapy would
necessitate a separate study. Second, the present study did not
provide PD-L1 expression data because its utility in a late-line
setting has not yet been reported and it is not typically measured
in clinical practice (6). MSI, MMR
and TMB status were also unavailable, as testing for these factors
is not mandatory prior to drug administration (5). Therefore, the association between
these status and inflammatory markers could not be analyzed. Third,
several patient records did not show blood test results for
C-reactive protein and albumin levels, which are not essential for
chemotherapy induction. Accordingly, the full-set analysis included
fewer patients than the total number of patients enrolled, which
resulted in a moderate sample size being included in the final
analyses. Finally, data on concomitant medications, including
steroids and immunosuppressive drugs, which could affect the
inflammatory markers tested, were not collected in the present
study. This was due to the present study's moderate sample size of
159 patients, which limited the ability to assess the impact of the
presence or absence of such relatively infrequently used
concomitant medications. Despite these limitations, the
comprehensive assessment of multiple inflammation-based prognostic
markers for immune checkpoint inhibitor monotherapy using
real-world data could be considered clinically valuable. Although
the results of the present study may not significantly impact the
choice of treatment regimen, these markers are useful for
predicting patient prognosis with immune checkpoint inhibitor
treatment, similar to their role with conventional cytotoxic
anticancer drugs. These results may also help clinicians to
navigate decisions on treatment adjustments for patients with
advanced or recurrent gastric cancer.
In conclusion, the present study analyzed real-world
data and demonstrated a strong prognostic value of various
inflammation-based markers in patients with advanced or recurrent
gastric cancer, treated with nivolumab as late-line chemotherapy.
mGPS exhibited the most robust correlation with patient prognosis.
Future studies should aim to collect and analyze data to assess the
potential utility of these inflammatory markers for first-line
treatment and preoperative treatment.
Supplementary Material
TTF based on different scores and
ratios. A log-rank test was used to calculate statistical
significance. (A) PNI, (B) GPS, (C) mGPS, (D) CAR, (E) NLR, (F)
PLR, (G) LMR, (H) dNLR, (I) NPS, (J) NLS, (K) PLS, (L) LMS, (M) PI,
(N) SII, (O) SIRI, (P) LIPI and (Q) CALLY. CRP, C-reactive protein,
df; degrees of freedom; TTF, time to treatment failure; PNI,
prognostic nutritional index; GPS, Glasgow prognostic score; mGPS,
modified GPS; CAR, CRP-to-albumin ratio; NLR,
neutrophil-to-lymphocyte ratio; PLR, platelet-to-lymphocyte ratio;
LMR, lymphocyte-to-monocyte ratio; dNLR, derived NLR; NPS,
neutrophil-platelet score; NLS, neutrophil-lymphocyte score; PLS,
platelet-lymphocyte score; LMS, lymphocyte-monocyte score; PI,
prognostic index; SII, systemic immune-inflammation index; SIRI,
systemic inflammation response index; LIPI, lung immune prognostic
index; CALLY, CRP albumin lymphocyte index.
Systemic inflammation-based prognostic
scores and ratios.
Patients medical and demographic
characteristics.
Summary of cancer treatments
administered to patients.
Estimated hazard ratios and 95% CIs of
prognostic factors for overalls survival using univariate and
multivariate Cox regression analyses.
Concordance and AIC of each model
involving each score and adjusting factors, including age, sex,
location, stage and previous radiotherapy.
Concordance and Akaike information
criterion of each score for time to treatment failure.
Acknowledgements
The authors acknowledge the dedication of Dr
Shinnichi Higashiue (Medical Corporation Tokushukai and General
Incorporated Association Tokushukai, Chiyoda, Tokyo 102-0074,
Japan) and Dr Hisaaki Afuso (Medical Corporation Tokushukai,
Chiyoda, Tokyo 102-0074, Japan) for their support in conducting
clinical research within the Tokushukai Group. The authors also
thank Mr. Katsuhiko Ozaki (Tokushukai Information System, Inc.,
Osaka 530-0001, Japan) for his assistance with the use of medical
databases.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
RS, YI and MO contributed to study design and
conception. RS, YF, MS and MH performed data acquisition. RS, YI
and MS confirm the authenticity of all the raw data.RS and YI
interpreted data and drafted the manuscript. KU, TM, KO, NS and HM
offered advice on the research design and contributed to the
interpretation of the study content. NS and HM reviewed and
approved the final version of the manuscript. All authors reviewed
and approved the final version of the manuscript.
Ethics approval and consent to
participate
The project rigorously followed ethical guidelines
for medical and biological research involving human subjects in
Japan, in accordance with the principles of The Declaration of
Helsinki. Approval for the study was obtained from the Ethics
Committee of the Tokushukai Group in April 2020 (approval no.
TGE01427-024). The study was registered in the UMIN Clinical Trial
Registry under the number UMIN000050590. Patients were informed
about the study using opt-out methods and all chose to
participate.
Patient consent for publication
Not applicable.
Competing interests
RS received speaker bureau fees/honoraria from
Daiichi-Sankyo, Ono Pharm, Taiho Pharma and Chugai outside the
scope of the submitted work. YI received speaker bureau
fees/honoraria from Bayer, Bristol-Myers Squibb, Daiichi-Sankyo,
Pfizer and Ono Pharm outside of the submitted work. HM received
speaker bureau fees/honoraria from Daiichi-Sankyo and Ono Pharm,
research funding from Astellas-Amgen Biopharma, Bayer, Bristol
Myers Squibb, Chugai, Daiichi-Sankyo, Incite, Novartis, Ono Pharm,
Pfizer and Rakuten Medical and scholarship donations from Bayer,
Chugai, Daiichi-Sankyo, Eisai, Kyowa-Kirin, Lilly, Ono
Pharmaceutical, Pfizer, Taiho Pharma and Takeda outside the scope
of the submitted work. However, these organizations were not
involved in the design, conduct or reporting of the present
study.
Authors' information
ORCID IDs: RS, 0000-0001-8601-0442; YI,
0000-0002-5202-531X; and HM, 0000-0001-8630-9145.
Use of artificial intelligence tools
During the preparation of this work, artificial
intelligence tools were used to improve the readability and
language of the manuscript or to generate images, and subsequently,
the authors revised and edited the content produced by the
artificial intelligence tools as necessary, taking full
responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Bray F, Laversanne M, Sung H, Ferlay J,
Siegel RL, Soerjomataram I and Jemal A: Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA Cancer J Clin. 74:229–263.
2024.PubMed/NCBI View Article : Google Scholar
|
|
2
|
National Cancer Registry, Ministry of
Health, Labour and Welfare Cancer Statistics: Cancer Information
Service, National Cancer Center, Japan. https://ganjoho.jp/reg_stat/statistics/data/dl/index.html.
Accessed on April 1, 2024.
|
|
3
|
SEER 5-year relative survival rate,
2012-2018. Cancer Statistics Explorer Network, National Cancer
Institute, United States. https://seer.cancer.gov/statistics-network/explorer/application.html.
Accessed on April 1, 2024.
|
|
4
|
NCCN Clinical Practice Guidelines in
Oncology; Gastric Cancer Version 1.2024. https://www.nccn.org/guidelines/category_1. Accessed
April 1, 2024.
|
|
5
|
Japanese Gastric Cancer Association.
Japanese gastric cancer treatment guidelines 2021 (6th edition).
Gastric Cancer. 26:1–25. 2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kang YK, Boku N, Satoh T, Ryu MH, Chao Y,
Kato K, Chung HC, Chen JS, Muro K, Kang WK, et al: Nivolumab in
patients with advanced gastric or gastro-oesophageal junction
cancer refractory to, or intolerant of, at least two previous
chemotherapy regimens (ONO-4538-12, ATTRACTION-2): A randomised,
double-blind, placebo-controlled, phase 3 trial. Lancet.
390:2461–2471. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Japanese Gastric Cancer Association.
Japanese gastric cancer treatment guidelines 2018 (5th edition).
Gastric Cancer. 24:1–21. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shitara K, Doi T, Dvorkin M, Mansoor W,
Arkenau HT, Prokharau A, Alsina M, Ghidini M, Faustino C, Gorbunova
V, et al: Trifluridine/tipiracil versus placebo in patients with
heavily pretreated metastatic gastric cancer (TAGS): A randomised,
double-blind, placebo-controlled, phase 3 trial. Lancet Oncol.
19:1437–1448. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Janjigian YY, Shitara K, Moehler M,
Garrido M, Salman P, Shen L, Wyrwicz L, Yamaguchi K, Skoczylas T,
Bragagnoli AC, et al: First-line nivolumab plus chemotherapy versus
chemotherapy alone for advanced gastric, gastro-oesophageal
junction, and oesophageal adenocarcinoma (CheckMate 649): A
randomised, open-label, phase 3 trial. Lancet. 398:27–40.
2021.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kang YK, Chen LT, Ryu MH, Oh DY, Oh SC,
Chung HC, Lee KW, Omori T, Shitara K, Sakuramoto S, et al:
Nivolumab plus chemotherapy versus placebo plus chemotherapy in
patients with HER2-negative, untreated, unresectable advanced or
recurrent gastric or gastro-oesophageal junction cancer
(ATTRACTION-4): A randomised, multicentre, double-blind,
placebo-controlled, phase 3 trial. Lancet Oncol. 23:234–247.
2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Ricci AD, Rizzo A and Brandi G: DNA damage
response alterations in gastric cancer: Knocking down a new wall.
Future Oncol. 7:865–868. 2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Marabelle A, Le DT, Ascierto PA, Di
Giacomo AM, De Jesus-Acosta A, Delord JP, Geva R, Gottfried M,
Penel N, Hansen AR, et al: Efficacy of pembrolizumab in patients
with noncolorectal high microsatellite Instability/Mismatch
repair-deficient cancer: Results from the phase II KEYNOTE-158
study. J Clin Oncol. 38:1–10. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Marabelle A, Fakih M, Lopez J, Shah M,
Shapira-Frommer R, Nakagawa K, Chung HC, Kindler HL, Lopez-Martin
JA, Miller WH Jr, et al: Association of tumour mutational burden
with outcomes in patients with advanced solid tumours treated with
pembrolizumab: Prospective biomarker analysis of the multicohort,
open-label, phase 2 KEYNOTE-158 study. Lancet Oncol. 21:1353–1365.
2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Akagi K, Oki E, Taniguchi H, Nakatani K,
Aoki D, Kuwata T and Yoshino T: Real-world data on microsatellite
instability status in various unresectable or metastatic solid
tumors. Cancer Sci. 112:1105–1113. 2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Parikh AR, He Y, Hong TS, Corcoran RB,
Clark JW, Ryan DP, Zou L, Ting DT, Catenacci DV, Chao J, et al:
Analysis of DNA damage response gene alterations and tumor
mutational burden across 17,486 tubular gastrointestinal
carcinomas: Implications for therapy. Oncologist. 24:1340–1347.
2019.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Rihawi K, Ricci AD, Rizzo A, Brocchi S,
Marasco G, Pastore LV, Llimpe FLR, Golfieri R and Renzulli M:
Tumor-associated macrophages and inflammatory microenvironment in
gastric cancer: Novel translational implications. Int J Mol Sci.
22(3805)2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
McMillan DC: Systemic inflammation,
nutritional status and survival in patients with cancer. Curr Opin
Clin Nutr Metab Care. 12:223–226. 2009.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dolan RD, Lim J, McSorley ST, Horgan PG,
Laird B and McMillan DC: The role of the systemic inflammatory
response in predicting outcomes in patients with advanced
inoperable cancer: Systematic review and meta-analysis. Crit Rev
Oncol Hematol. 116:134–146. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Guven DC, Sahin TK, Erul E, Rizzo A, Ricci
AD, Aksoy S and Yalcin S: The association between albumin levels
and survival in patients treated with immune checkpoint inhibitors:
A systematic review and meta-analysis. Front Mol Biosci.
9(1039121)2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Zhang Y, Chen S, Chen H and Li W: A
comprehensive analysis of Glasgow prognostic score (GPS)/the
modified Glasgow prognostic score (mGPS) on immune checkpoint
inhibitor efficacy among patients with advanced cancer. Cancer Med.
12:38–48. 2023.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chen J, Wei S, Zhao T and Zhang X, Wang Y
and Zhang X: Clinical significance of serum biomarkers in stage IV
non-small-cell lung cancer treated with PD-1 inhibitors: LIPI
Score, NLR, dNLR, LMR, and PAB. Dis Markers.
2022(7137357)2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Tanaka S, Uchino J, Yokoi T, Kijima T,
Goto Y, Suga Y, Katayama Y, Nakamura R, Morimoto K, Nakao A, et al:
Prognostic nutritional index and lung immune prognostic index as
prognostic predictors for combination therapies of immune
checkpoint inhibitors and cytotoxic anticancer chemotherapy for
patients with advanced non-small cell lung cancer. Diagnostics
(Basel). 12(423)2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Onodera T, Goseki N and Kosaki G:
Prognostic nutritional index in gastrointestinal surgery of
malnourished cancer patients. Nihon Geka Gakkai Zasshi.
85:1001–1005. 1984.PubMed/NCBI(In Japanese).
|
|
24
|
Forrest LM, McMillan DC, McArdle CS,
Angerson WJ and Dunlop DJ: Evaluation of cumulative prognostic
scores based on the systemic inflammatory response in patients with
inoperable non-small-cell lung cancer. Br J Cancer. 89:1028–1030.
2003.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Toiyama Y, Miki C, Inoue Y, Tanaka K,
Mohri Y and Kusunoki M: Evaluation of an inflammation-based
prognostic score for the identification of patients requiring
postoperative adjuvant chemotherapy for stage II colorectal cancer.
Exp Ther Med. 2:95–101. 2011.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Fairclough E, Cairns E, Hamilton J and
Kelly C: Evaluation of a modified early warning system for acute
medical admissions and comparison with C-reactive protein/albumin
ratio as a predictor of patient outcome. Clin Med (Lond). 9:30–33.
2009.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Nakahara K, Monden Y, Ohno K, Fujii Y,
Hashimoto J, Kitagawa Y and Kawashima Y: Importance of biologic
status to the postoperative prognosis of patients with stage III
nonsmall cell lung cancer. J Surg Oncol. 36:155–160.
1987.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Smith RA, Bosonnet L, Raraty M, Sutton R,
Neoptolemos JP, Campbell F and Ghaneh P: Preoperative
platelet-lymphocyte ratio is an independent significant prognostic
marker in resected pancreatic ductal adenocarcinoma. Am J Surg.
197:466–472. 2009.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Wilcox RA, Ristow K, Habermann TM, Inwards
DJ, Micallef IN, Johnston PB, Colgan JP, Nowakowski GS, Ansell SM,
Witzig TE, et al: The absolute monocyte and lymphocyte prognostic
score predicts survival and identifies high-risk patients in
diffuse large-B-cell lymphoma. Leukemia. 25:1502–1509.
2011.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Proctor MJ, McMillan DC, Morrison DS,
Fletcher CD, Horgan PG and Clarke SJ: A derived neutrophil to
lymphocyte ratio predicts survival in patients with cancer. Br J
Cancer. 107:695–699. 2012.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Watt DG, Proctor MJ, Park JH, Horgan PG
and McMillan DC: The neutrophil-platelet score (NPS) predicts
survival in primary operable colorectal cancer and a variety of
common cancers. PLoS One. 10(e0142159)2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Dolan RD, McSorley ST, Park JH, Watt DG,
Roxburgh CS, Horgan PG and McMillan DC: The prognostic value of
systemic inflammation in patients undergoing surgery for colon
cancer: Comparison of composite ratios and cumulative scores. Br J
Cancer. 119:40–51. 2018.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Dolan RD, Alwahid M, McSorley ST, Park JH,
Stevenson RP, Roxburgh CS, Horgan PG and McMillan DC: A comparison
of the prognostic value of composite ratios and cumulative scores
in patients with operable rectal cancer. Sci Rep.
10(17965)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kasymjanova G, MacDonald N, Agulnik JS,
Cohen V, Pepe C, Kreisman H, Sharma R and Small D: The predictive
value of pre-treatment inflammatory markers in advanced
non-small-cell lung cancer. Curr Oncol. 17:52–58. 2010.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W,
Zhang X, Wang WM, Qiu SJ, Zhou J and Fan J: Systemic
immune-inflammation index predicts prognosis of patients after
curative resection for hepatocellular carcinoma. Clin Cancer Res.
20:6212–6222. 2014.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Qi Q, Zhuang L, Shen Y, Geng Y, Yu S, Chen
H, Liu L, Meng Z, Wang P and Chen Z: A novel systemic inflammation
response index (SIRI) for predicting the survival of patients with
pancreatic cancer after chemotherapy. Cancer. 122:2158–2167.
2016.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Mezquita L, Auclin E, Ferrara R, Charrier
M, Remon J, Planchard D, Ponce S, Ares LP, Leroy L,
Audigier-Valette C, et al: Association of the lung immune
prognostic index with immune checkpoint inhibitor outcomes in
patients with advanced non-small cell lung cancer. JAMA Oncol.
4:351–357. 2018.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Müller L, Hahn F, Mähringer-Kunz A, Stoehr
F, Gairing SJ, Michel M, Foerster F, Weinmann A, Galle PR, Mittler
J, et al: Immunonutritive scoring for patients with hepatocellular
carcinoma undergoing transarterial chemoembolization: Evaluation of
the CALLY index. Cancers (Basel). 13(5018)2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Averitt AJ, Weng C, Ryan P and Perotte A:
Translating evidence into practice: Eligibility criteria fail to
eliminate clinically significant differences between real-world and
study populations. NPJ Digit Med. 3(67)2020.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Hilgers RD, König F, Molenberghs G and
Senn S: Design and analysis of clinical trials for small rare
disease populations. J Rare Dis Res Treat. 1:53–60. 2016.
|
|
41
|
Latimer NR: Survival analysis for economic
evaluations alongside clinical trials-extrapolation with
patient-level data: Inconsistencies, limitations, a practice guide.
Med Decis Making. 33:743–754. 2013.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Corrigan-Curay J, Sacks L and Woodcock J:
Real-word evidence and real-world data for evaluating drug safety
and effectiveness. JAMA. 320:867–868. 2018.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Katkade VB, Sanders KN and Zou KH: Real
world data: An opportunity to supplement existing evidence for the
use of long-established medicines in health care decision making. J
Multidiscip Healthc. 11:295–304. 2018.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Makady A, de Boer A, Hillege H, Klungel O
and Goettsch W: (on behalf of GetReal Work Package 1). What is
real-world data? A review of definitions based on literature and
stakeholder interviews. Value Health. 20:858–865. 2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Shimoyama R, Imamura Y, Uryu K, Mase T,
Fujimura Y, Hayashi M, Ohtaki M, Ohtani K, Shinozaki N and Minami
H: Real-world outcomes of systemic therapy in Japanese patients
with cancer (Tokushukai REAl-World Data Project: TREAD): Study
protocol for a nationwide cohort study. Healthcare (Basel).
10(2146)2022.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Eba J and Nakamura K: Overview of the
ethical guidelines for medical and biological research involving
human subjects in Japan. Jpn J Clin Oncol. 52:539–544.
2022.PubMed/NCBI View Article : Google Scholar
|
|
47
|
National Cancer Registry (Ministry of
Health, Labour and Welfare), tabulated by Cancer Information
Service, National Cancer Center, Japan. https://ganjoho.jp/reg_stat/statistics/data/dl/en.html.
(Accessed 1 April 2024).
|
|
48
|
Shimoyama R, Imamura Y, Uryu K, Mase T,
Shiragami M, Fujimura Y, Hayashi M, Ohtaki M, Ohtani K, Shinozaki N
and Minami H: Inflammation-based prognostic markers of metastatic
pancreatic cancer using real-world data in Japan: The Tokushukai
REAl-world Data (TREAD) project. Oncol Lett. 27(136)2024.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Chen LT, Satoh T, Ryu MH, Chao Y, Kato K,
Chung HC, Chen JS, Muro K, Kang WK, Yeh KH, et al: A phase 3 study
of nivolumab in previously treated advanced gastric or
gastroesophageal junction cancer (ATTRACTION-2): 2-year update
data. Gastric Cancer. 23:510–519. 2020.PubMed/NCBI View Article : Google Scholar
|
|
50
|
Dovedi SJ, Adlard AL, Lipowska-Bhalla G,
McKenna C, Jones S, Cheadle EJ, Stratford IJ, Poon E, Morrow M,
Stewart R, et al: Acquired resistance to fractionated radiotherapy
can be overcome by concurrent PD-L1 blockade. Cancer Res.
74:5458–5468. 2014.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Deng L, Liang H, Burnette B, Beckett M,
Darga T, Weichselbaum RR and Fu YX: Irradiation and anti-PD-L1
treatment synergistically promote antitumor immunity in mice. Clin
Invest. 124:687–695. 2014.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Yamaguchi O, Kaira K, Hashimoto K, Mouri
A, Miura Y, Shiono A, Nishihara F, Murayama Y, Noda SE, Kato S, et
al: Radiotherapy is an independent prognostic marker of favorable
prognosis in non-small cell lung cancer patients after treatment
with the immune checkpoint inhibitor, nivolumab. Thorac Cancer.
10:992–1000. 2019.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Sharabi AB, Lim M, DeWeese TL and Drake
CG: Radiation and checkpoint blockade immunotherapy:
Radiosensitisation and potential mechanisms of synergy. Lancet
Oncol. 16:e498–e509. 2015.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Proctor MJ, Talwar D, Balmar SM, O'Reilly
DS, Foulis AK, Horgan PG, Morrison DS and McMillan DC: The
relationship between the presence and site of cancer, an
inflammation-based prognostic score and biochemical parameters.
Initial results of the Glasgow inflammation outcome study. Br J
Cancer. 103:870–876. 2010.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Proctor MJ, Morrison DS, Talwar D, Balmer
SM, O'Reilly DS, Foulis AK, Horgan PG and McMillan DC: An
inflammation-based prognostic score (mGPS) predicts cancer survival
independent of tumour site: A Glasgow inflammation outcome study.
Br J Cancer. 104:726–734. 2011.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Proctor MJ, Morrison DS, Talwar D, Balmer
SM, Fletcher CD, O'Reilly DS, Foulis AK, Horgan PG and McMillan DC:
A comparison of inflammation-based prognostic scores in patients
with cancer. A Glasgow inflammation outcome study. Eur J Cancer.
47:2633–2641. 2011.PubMed/NCBI View Article : Google Scholar
|
|
57
|
McMillan DC: The systemic
inflammation-based Glasgow prognostic score: A decade of experience
in patients with cancer. Cancer Treat Rev. 39:534–540.
2013.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Wu TH, Tsai YT, Chen KY, Yap WK and Luan
CW: Utility of high-sensitivity modified Glasgow prognostic score
in cancer prognosis: A systemic review and meta-analysis. Int J Mol
Sci. 24(1318)2023.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Wang Y, Lei Y, Zheng D, Yang Y, Luo L, Li
J and Xie X: Prognostic value of lung immune prognostic index in
non-small cell lung cancer patients receiving immune checkpoint
inhibitors: A meta-analysis. Pathol Oncol Res.
30(1611773)2024.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Carril-Ajuria L, Lavaud P, Dalban C,
Negrier S, Gravis G, Motzer RJ, Chevreau C, Tannir NM, Oudard S,
McDermott DF, et al: Validation of the lung immune prognostic index
(LIPI) as a prognostic biomarker in metastatic renal cell
carcinoma. Eur J Cancer. 204(114048)2024.PubMed/NCBI View Article : Google Scholar
|