Introduction
Obstructed hemivagina and ipsilateral renal anomaly
(OHVIRA) syndrome is a rare Mullerian duct anomaly. The exact
incidence of OHVIRA syndrome is unknown. The major presentations
are dysmenorrhea, lower abdominal pain, a paravaginal mass,
abnormal vaginal discharge and intermenstrual bleeding (1).
In general, the majority of cases of OHVIRA syndrome
are diagnosed during adolescence as the obstruction of menstrual
outflow causes abdominal pain early following menarche. Smith and
Laufer (1) reported that the average
age of diagnosis was 14 years. On the other hand, in the case of
incomplete vaginal obstruction, the diagnosis is sometimes delayed
due to the lack of symptoms. However, there are some cases of
OHVIRA syndrome with pelvic inflammatory disease (2) or endometriosis (3), which may influence fertility or the
quality of life of patients. Thus, it is crucial for an accurate
diagnosis to be made and to provide appropriate treatment for
patients with OHVIRA syndrome at an early age.
The present study reports a a case of a patient with
OHVIRA syndrome who was admitted to hospital due to pelvic
inflammatory disease. This diagnosed pre-operatively using
vaginoscopy and hysteroscopy.
Case report
The present study describes the case of a
25-year-old female, gravida 0 para 0, who visited an internal
medicine clinic due to fever and lower abdominal pain. Her menarche
occurred at age 11 and her menstrual cycle was regular. She
regularly had sexual intercourse. She had no history of menorrhagia
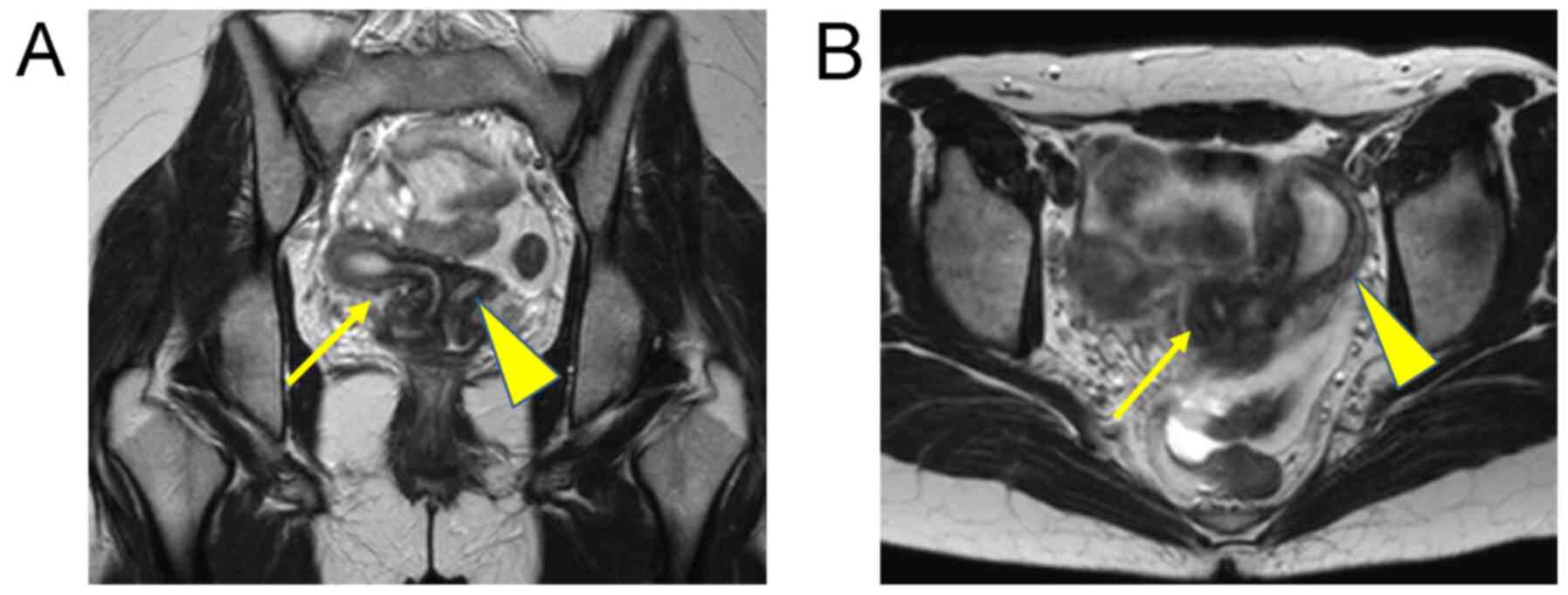
or dyspareunia. Magnetic resonance imaging (MRI) and a computed
tomography (CT) scan revealed uterus didelphys and right renal
agenesis (Fig. 1). She was referred
to the authors' hospital as gynecological disease was suspected.
Tenderness in the pouch of Douglas was noted upon a pelvic
examination and C-reactive protein levels were found to be high
upon a blood examination. The patient was diagnosed with pelvic
inflammatory disease. The vaginal sidewall bulge was not detected
by a speculum examination during the non-menstrual period. The
right obstructed hemivagina was not clear upon the MRI examination.
She was treated with antibiotics and recovered from pelvic
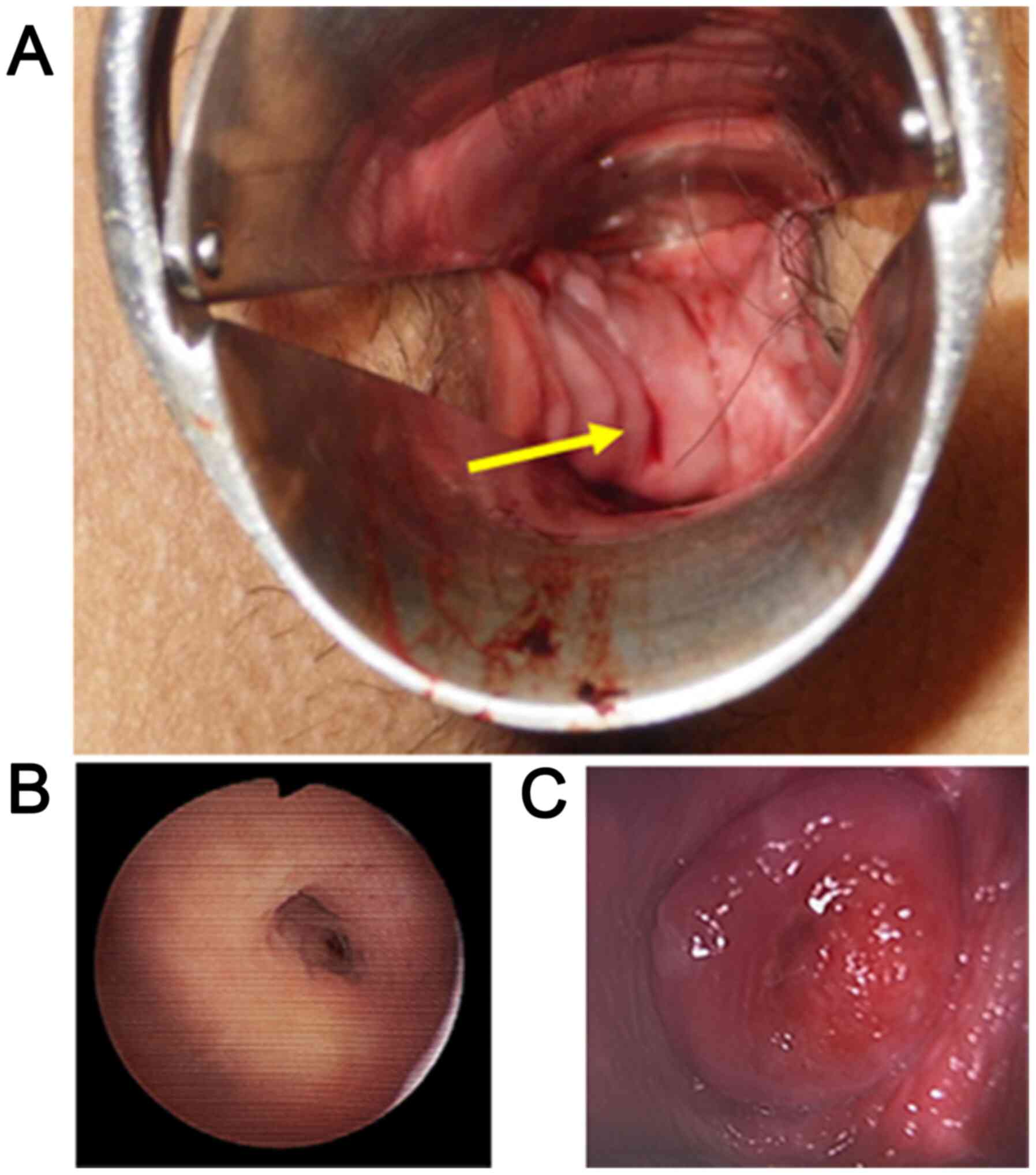
inflammatory disease within a week. A few weeks later, an opening
was found on the vaginal septum by a speculum examination during
the menstrual period (Fig. 2A).
Diagnostic vaginoscopy through the opening was performed using a
flexible hysteroscope of 3.1 mm in diameter, which is usually used
for diagnostic hysteroscopy in the outpatient clinic, without
anesthetic agents. Upon diagnostic vaginoscopy and hysteroscopy,
the right vaginal cavity was enclosed, and both the uterine cervix
and uterine cavity were found to be normal (Fig. 2B and C). She was thus diagnosed with OHVIRA
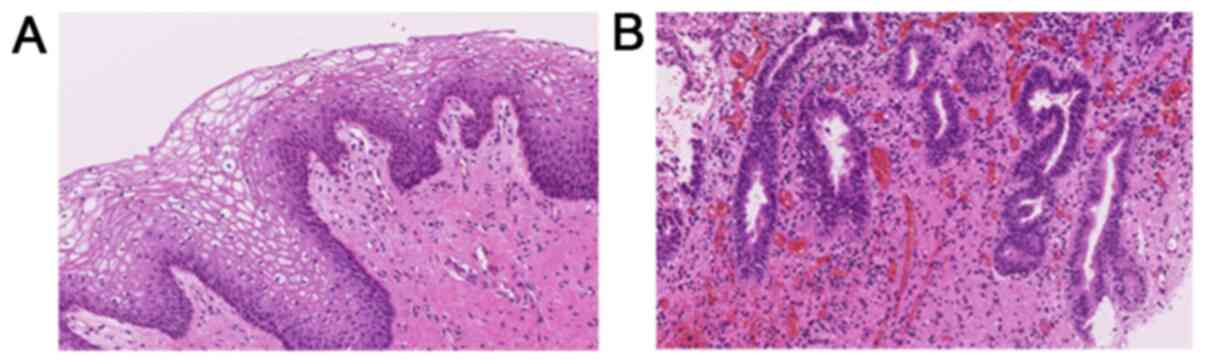
syndrome. Her vaginal septum was surgically removed under direct
visualization and the pathological findings (hematoxylin and eosin
staining, performed in the authors laboratory) of the resected
septum revealed a benign squamous epithelium (Fig. 3A). The glandular epithelium was
partially observed and vaginal adenosis was noted in the vaginal
septum (Fig. 3B). The post-operative
course was uneventful and restenosis of the vagina was not
observed.
Discussion
OHVIRA syndrome is characterized by an obstructed
hemivagina and ipsilateral renal anomaly. This syndrome was
previously classified into three groups by Rock and Jones (4) as follows: Group 1, complete vaginal
obstruction with a hematocolpos. Group 2, incomplete vaginal
obstruction without a hematocolpos. In group 2, an opening in the
partially obstructed vaginal pouch is observed. Group 3, complete
vaginal obstruction with a laterally communicating double uterus.
In the case presented herein, an opening was noted on the vaginal
septum and the communication between the uteruses could not be
observed. Thus, the patient was diagnosed with OHVIRA syndrome with
group 2 classification. Smith and Laufer (1) reported 27 cases of OHVIRA syndrome. The
mean age at diagnosis was 14 years. A total of 23 patients had
ipsilateral renal anomalies, including 20 with renal agenesis. In
addition, 26 patients underwent vaginal reconstruction, eight of
whom additionally underwent laparoscopy for the classification of
the diagnosis. Furthermore, 6 patients required two-stage
vaginoplasty due to incomplete previous resection (n=1), infection
or anatomic distortion (n=4), or restenosis (n=2). Vaginal septum
adenosis was noted in 7 patients. In their study, they concluded
that the majority of patients with OHVIRA syndrome can be treated
solely by single- stage vaginoplasty and that routine laparoscopy
is not essential for management. They also described two cases of
post-operative restenosis among 7 patients with vaginal adenosis in
the resected vaginal septum (1).
Candiani et al (3) reported
36 cases of double uterus, blind hemivagina and ipsilateral renal
agenesis in 1997. In their study, the vaginal septum was excised
and marsupialization was carried out in 30 out of the 36 cases. The
pregnancy rate among the 15 women wanting children was 87% and the
live birth rate was 77% (3). Kamio
et al (2) reported a case of
OHVIRA syndrome with septic shock. In that case, a 37-year-old
female was diagnosed with OHVIRA syndrome and she developed septic
shock due to pyocolpos, requiring intensive care unit
hospitalization (2). According to
another study, patients with OHVIRA syndrome can develop pyocolpos,
abscesses or pelvic inflammatory disease (5).
As aforementioned, the majority of cases of OHVIRA
syndrome are diagnosed during adolescence as the obstruction of
menstrual outflow causes abdominal pain early following menarche.
On the other hand, in the case of incomplete vaginal obstruction,
such as in the case in the present study, the diagnosis is
sometimes delayed due to the lack of symptoms. However, there are
some cases of OHVIRA syndrome with pelvic inflammatory disease
(2) or endometriosis (3), which may influence fertility or the
quality of life of patients. Thus, it is important to make an
accurate diagnosis and provide appropriate treatment for patients
with OHVIRA syndrome at an early age.
In the present case, the patient did not exhibit
menorrhalgia or dyspareunia, although she regularly had sexual
intercourse. Due to the lack of symptoms related to menstruation or
coitus, she had not visited a gynecologist until the occurrence of
pelvic inflammatory disease. She visited an internal medicine
clinic due to experiencing fever and lower abdominal pain, and the
judgment by the physician led to a correct diagnosis of OHVIRA
syndrome. It was not difficult to diagnose uterus didelphys and
right renal agenesis by MRI and a CT scan. An opening was found on
the vaginal septum by speculum examination during the menstruation
period. Diagnostic vaginoscopy through the opening was performed
without the leakage of saline solution as the opening and the
fiberscope had almost same diameter. Diagnostic vaginoscopy and
hysteroscopy through the opening were also useful to observe the
obstructed vaginal cavity and the right uterine cavity. In the case
presented herein, pelvic inflammatory disease was considered to be
associated with OHVIRA syndrome due to the stasis of menstrual
blood and regular sexual intercourse. Her vaginal septum was
surgically removed and the pathological findings of the resected
septum revealed benign squamous and glandular epithelium. Thus,
vaginal adenosis was noted in the vaginal septum and attention
should be paid to vaginal restenosis, as previously reported
(1). Following surgery, the
reduction of the risk of pelvic inflammatory disease and normal
childbearing is expected.
In the cases of uterus didelphys without
hematocolpos, such as in the case presented herein, a speculum
examination during the menstruation period is useful for searching
the menstrual outflow passage. If a passage is not found in the
vagina, an exploratory laparoscopy or laparotomy is then required
to identify the communication locus between the uteruses. These
procedures are crucial in order to avoid misdiagnoses in the cases
of incomplete vaginal obstruction without hematocolpos.
Cheng et al (6) reported the technique of vaginoscopic
incision of the vaginal septum in patients with OHVIRA syndrome.
They described that vaginoplasty can be performed under direct
visualization with a speculum for adult patients; however,
vaginoscopic management using the non-touch technique may be an
option for adolescent patients with an immature and narrow vagina
(6). Johary et al (7) reported the use of a hysteroscope for
diagnostic vaginoscopy and/or hysteroscopy in their systematic
review. Speculum inspection has limited ability to observe the
entire vagina, and may cause pain and increase the risk of hymen
injury in patients who are virgins. Johary et al (7) reported that diagnostic vaginoscopy
using flexible hysteroscope may minimize the risk of hymen injury
and may serve as an alternative option for adolescent patients.
Shih et al (8) reported the
use of a flexible hysteroscope for the diagnosis of uterus
didelphys, a vertical vaginal septum and an obstructed hemivagina
with pyocolpos in a 15-year-old patient. In the case in the present
study, the patient was 25 years of age and had regular sexual
intercourse. Diagnostic vaginoscopy through the opening on the
vaginal septum for the purpose of hemivagina cavity observation
differed from the aforementioned report about diagnostic
vaginoscopy in an adolescent. To date, to the best of our
knowledge, there are no studies available on diagnostic vaginoscopy
through the opening on the vaginal septum in incomplete vaginal
obstruction-type OHVIRA syndrome.
In conclusion, the case described in the present
study was pre-operatively diagnosed with OHVIRA syndrome by
vaginoscopy and hysteroscopy. A speculum examination during the
menstrual period revealed the outflow of menstrual blood through
the opening on the vaginal septum. This technique, diagnostic
vaginoscopy and hysteroscopy, is minimally invasive and sufficient
for the diagnosis of incomplete vaginal obstruction-type OHVIRA
syndrome. An accurate pre-operative diagnosis enabled less-invasive
surgical treatment solely by the resection of the vaginal septum,
avoiding exploratory laparoscopy or laparotomy.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The dataset used and/ or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors (YM, JH, NO and KI) participated in the
conception and design of the study. YM, JH and NO obtained the data
and treated the patient. YM examined the patient data and drafted
the manuscript. KI revised the manuscript prior to submission. In
addition, KI and YM were major contributors to the design of the
study. YM and KI confirm the authenticity of all the raw data. All
authors have read and approved the final version of the
manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
the presentation of her case.
Patient consent for publication
The patient provided written informed consent for
the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Smith NA and Laufer MR: Obstructed
hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome:
Management and follow-up. Fertil Steril. 87:918–922.
2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Kamio M, Nagata C, Sameshima H, Togami S
and Kobayashi H: Obstructed hemivagina and ipsilateral renal
anomaly (OHVIRA) syndrome with septic shock: A case report. J
Obstet Gynaecol Res. 44:1326–1329. 2018.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Candiani GB, Fedele L and Candiani M:
Double uterus, blind hemivagina, and ipsilateral renal agenesis: 36
cases and long-term follow-up. Obstet Gynecol. 90:26–32.
1997.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rock JA and Jones HW Jr: The double uterus
associated with an obstructed hemivagina and ipsilateral renal
agenesis. Am J Obstet Gynecol. 138:339–342. 1980.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Zurawin RK, Dietrich JE, Heard MJ and
Edwards CL: Didelphic uterus and obstructed hemivagina with renal
agenesis: Case report and review of the literature. J Pediatr
Adolesc Gynecol. 17:137–141. 2004.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cheng C, Subedi J, Zhang A, Johnson G,
Zhao X, Xu D and Guan X: Vaginoscopic incision of oblique vaginal
septum in adolescents with OHVIRA syndrome. Sci Rep.
9(20042)2019.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Johary J, Xue M, Xu B, Xu D and Aili A:
Use of hysteroscope for vaginoscopy or hysteroscopy in adolescents
for the diagnosis and therapeutic management of gynecologic
disorders: A systematic review. J Pediatr Adolesc Gynecol.
28:29–37. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Shih CL, Hung YC, Chen CP, Chien SC and
Lin WC: Resectoscopic excision of the vaginal septum in a virgin
with uterus didelphys and obstructed unilateral vagina. Taiwan J
Obstet Gynecol. 49:109–111. 2010.PubMed/NCBI View Article : Google Scholar
|