Introduction
Clavicle fractures are a common type of fracture
observed in clinical practice, accounting for ~2.6-10% of total
body fractures; 80% of clavicle fractures occur in the midshaft
clavicle, while distal and proximal clavicle fractures have a low
incidence (1,2). Previous studies have reported that the
incidence of mid-clavicle fractures is ~29-64 cases per 100,000
individuals each year; in addition, the incidence of such fractures
in children is significantly higher than that in adults (3,4). The
traditional non-operative treatment used is usually a sling or
figure-of-eight bandage, even if the clavicle fracture is displaced
(5). If patients with a clavicle
fracture are not treated in a timely and effective manner, their
limb function and quality of life is severely affected. It has been
reported that the rate of bone non-union following the conservative
treatment of comminuted fractures can amount to 15% (6). Compared with conservative
(non-surgical) treatments, early surgical treatment can
significantly improve the prognosis of fractures and can reduce the
incidence of non-unions and malunions (7). Traditional surgical treatment with
Kirschner wire (KW) fixation is more common; however, the
associated risk of fracture end displacement and malunion is
prohibitive, and for patients with comminuted or severely unstable
clavicle fractures, it is difficult to achieve satisfactory results
with traditional treatments (8). It
has been reported that >50% of clinical clavicle fractures are
displaced, and the risk of fracture malunion and discontinuity is
relatively high; in addition, improper treatment can lead to the
development of severe complications (9).
With the continuous exploration and development of
treatment methods and the continuous improvement of patient
requirements, the treatment of clavicle fractures with an anatomic
plate (AP) has been widely used in clinical practice. At present,
AP and KW fixation are widely used in clinical practice for the
treatment of clavicle fractures. KW wire fixation requires a
smaller incision, and less soft tissue and periosteum dissection;
however, it is associated with a high possibility of fracture
displacement and re-operation. Although AP requires a long surgical
incision, it has a good stability, fewer complications and a higher
post-operative fracture healing rate, particularly for comminuted
and severely unstable fractures. Despite the fact that a variety of
fixation methods have been described in the published literature to
date, the optimal treatment of mid-clavicle fractures remains
controversial (10,11). However, to date, the available
evidence is not sufficient to confirm the advantages and
disadvantages for the use of the AP and KW in mid-clavicle
fractures. Therefore, the present study aimed to further explore
the treatment of mid-clavicle fractures by analyzing available
clinical studies on the treatment of such fractures with an AP and
KW, in order to select a more suitable clinical treatment
method.
Data and methods
Literature search and inclusion
criteria
The inclusion criteria were as follows: Randomized
controlled studies or cohort trials on mid-clavicle fractures, the
exclusion of pathological fractures, the inclusion of at least one
evaluation index and the inclusion of a full text. The exclusion
criteria were the following: No mid-clavicle fractures, multiple
injuries, no mean values. For contradictory articles and data, any
issues were resolved by the corresponding author (JZ). Two
researchers (DY and LW) searched the database and randomly searched
the literature on AP and KW fixation for mid-clavicle fractures.
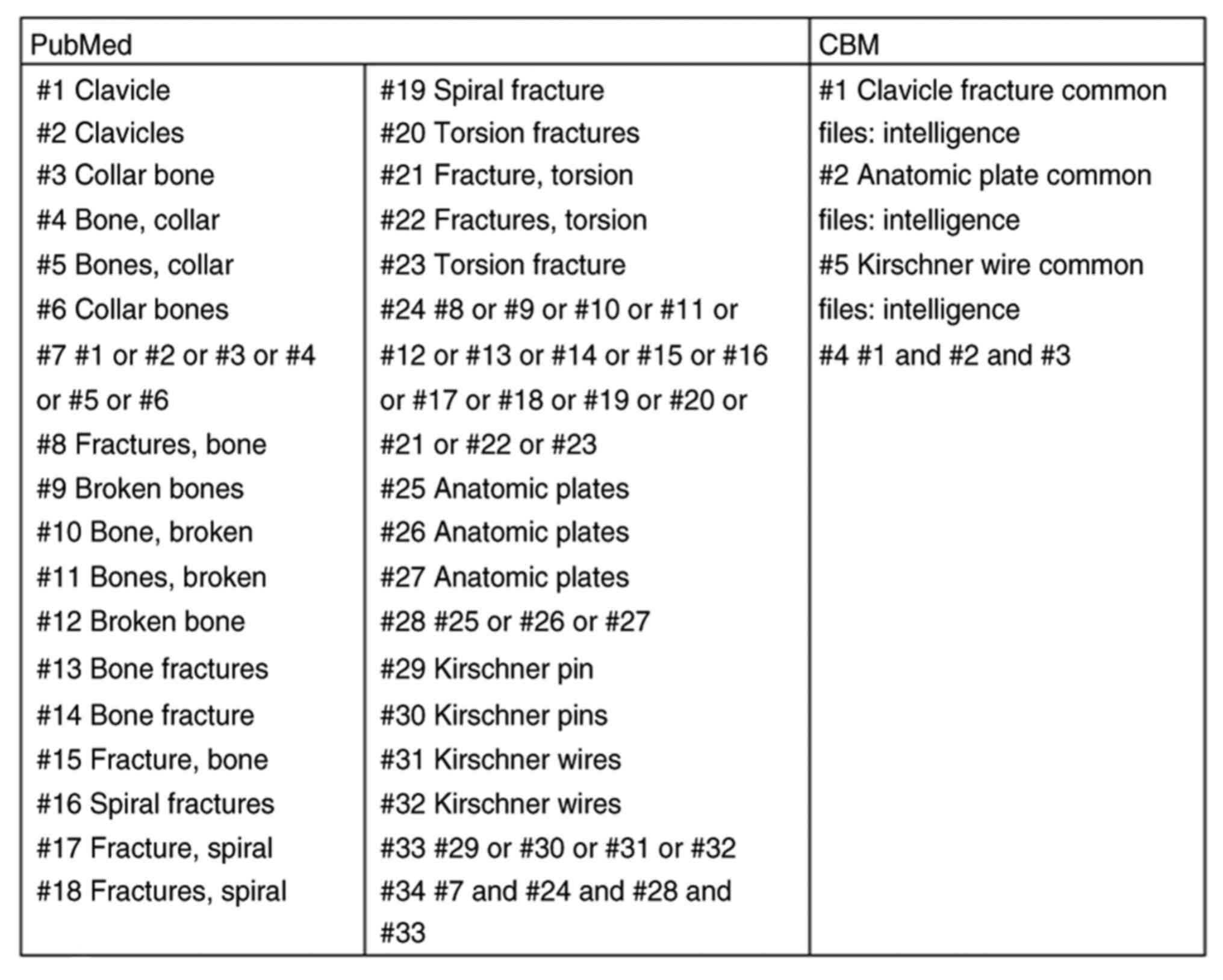
The databases used included the Cochrane Library (https://www.cochrane.org), PubMed (https://www.ncbi.nlm.nih.gov/), Embase (https://www.embase.com), CNKI (http://www.cnki.net/), Wanfang (http://www.wanfangdata.com.cn/index.html), VIP
(http://www.cqvip.com/) and CBM (sinomed.ac.cn). The retrieval time used was from the
establishment of the database to June, 2021. The key words used for
the search were the following: Clavicle fracture, anatomical plate
and Kirschner wire, and finally, the articles included at least one
evaluation index to evaluate the effectiveness of the treatment for
mid-clavicular fractures. They included mean incision length, mean
surgical duration, blood loss, constant function score (6 months),
fracture healing time, post-operative efficacy and complication
rate. The retrieval strategies for PubMed and CBM are presented in
Fig. 1 (each # symbol and number in
the figure represent a retrieval step).
Data extraction and quality
evaluation
The basic features of the included studies,
including the number of cases in the AP and KW groups, mean age,
fracture type, duration of follow-up, and randomized controlled
studies or cohort trials, were obtained by two researchers (DY and
LW) by reading the title, abstract, key words and finally, the full
article. RevMan 5.0 software Cochrane bias risk assessment
(https://training.cochrane.org/handbook) was used for
randomized controlled studies and the Newcastle-Ottawa Scale (NOS)
was used for cohort trials, in order to evaluate the quality. The
scale total score is nine points, and a score of ≥6 is considered
high-quality research (12).
Statistical analysis
For continuous data obtained, the standardized mean
difference (SMD) and 95% confidence intervals (CIs) were used to
estimate validity. For dichotomous data, the odds ratios (ORs) were
calculated. A meta-analysis was carried out using RevMan 5.0
software and the I2 index for the heterogeneity
of the studies. When the I2 was >50%,
indicating a high heterogeneity (13,14), the
random effects model was used for data analysis. When the
I2 ≤50%, the fixed effects model was used for
data analysis. A value of P<0.05 was considered to indicate a
statistically significant difference.
Results
Features of the included articles
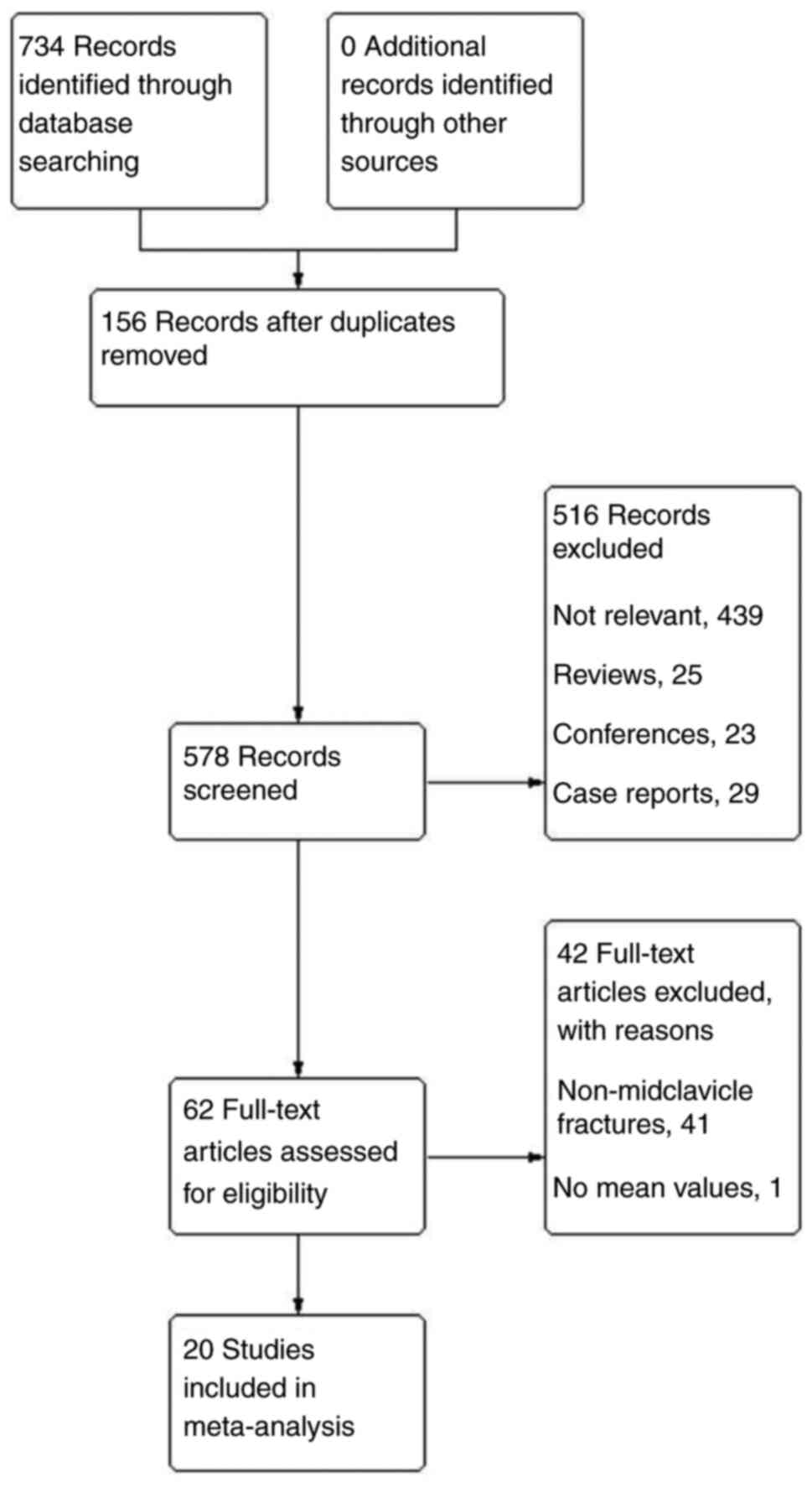
The Cochrane Library, PubMed, Embase, CNKI, Wanfang,
VIP and CBM databases were searched. A total of 734 studies were
retrieved, and 156 duplicate studies were found. After reading the
titles and abstracts, 516 articles were excluded, including: 439
unrelated articles, 25 review articles, 23 conference articles and
29 case reports; remaining 62 articles. After reading the full
articles, 41 articles were found to include no mid-clavicle
fractures, and one article had no mean values. Finally, 20 articles
containing at least one research index were obtained. Among these
20 articles, 17 included dichotomous variables and 8 included
continuous variables. A flow chart of the included studies is
presented in Fig. 2. In total, eight
randomized controlled studies (8,15-21)
and 12 cohort trials (22-33)
were included. The basic characteristics of the studies are listed
in Table I.
 | Table IThe characteristics of the included
studies. |
Table I
The characteristics of the included
studies.
| Author | Year of
publication | No. of cases
AP/KW | Characteristics of
cases (average age, ratio of male to female) | Fracture types
open/closed | Research type | Follow-up time
(months) | (Refs.) |
|---|
| Li | 2014 | 28/28 | AP: 38.6±5.7 years
old, 19/9 | AP: 8/20 | Cohort trial | 12 | (25) |
| | | | KW: 39.6±4.7 years
old, 17/11 | KW: 9/19 | | | |
| Tian | 2013 | 37/7 | 5-68 years old | Open 2, closed
56 | Cohort trial | 6 to 18 | (26) |
| Guo et al | 2014 | 20/20 | AP: 22.4±15.9 years
old, 13/7 | Not mentioned | Randomized controlled
study | 6 | (18) |
| | | | KW: 23.8±13.5 years
old, 14/6 | | | | |
| Yang | 2017 | 36/34 | AP: 40.58±2.43 years
old, 22/14 | All are closed | Cohort trial | 6 | (22) |
| | | | KW: 39.76.8±2.58
years old, 21/13 | | | | |
| Liu | 2017 | 35/35 | AP: 44.57±12.24
years old, 18/17 | Not mentioned | Randomized
controlled study | 6 | (15) |
| | | | KW: 44.63±12.12
years old, 20/15 | | | | |
| Li et
al | 2012 | 58/50 | AP: Average age 36,
39/19 | All are closed | Randomized
controlled study | 6 | (8) |
| | | | KW: average 34.5
years old, 32/18 | | | | |
| Lv and Du | 2010 | 24/37 | 13-65 years
old | All are closed | Cohort trial | 9-24 | (31) |
| Wang et
al | 2011 | 35/33 | AP: 37±5 years old,
19/16 | AP: 2/33 | Cohort trial | 12 to 41
(28±5) | (28) |
| | | | KW: 37±5 years old,
17/16 | KW: 3/30 | | | |
| Ma | 2014 | 44/44 | 37.45 ± 5.44 years
old, 48/40 | All are
comminuted | Randomized
controlled study | Not mentioned | (19) |
| Jue | 2017 | 38/38 | AP: 42.48±3.27
years old, 23/15 | Not mentioned | Randomized
controlled study | Not mentioned | (16) |
| | | | KW: 43.17±3.34
years old, 22/16 | | | | |
| Cheng | 2015 | 30/30 | AP: 42.3±22.69
years old, 18/12 | Not mentioned | Cohort trial | Not mentioned | (24) |
| | | | KW: 41.78±21.53
years old, 20/10 | | | | |
| Bu et
al | 2006 | 24/60 | 15-65 years
old | Not mentioned | Cohort trial | 7 to 18 | (33) |
| Qiu and Xiao | 2013 | 41/33 | 16-73 years
old | All are closed | Randomized
controlled study | 3 to 24 (average
15) | (20) |
| Wang et
al | 2015 | 100/100 | AP: 45.8 years old,
51/49 | Not mentioned | Randomized
controlled study | Not mentioned | (21) |
| | | | KW: average 45.5
years old, 50/50 | | | | |
| Zhang et
al | 2012 | 75/33 | 5-68 years old | Open 2, closed
114 | Cohort trial | 6 to 18 | (27) |
| Chen et
al | 2015 | 30/10 | 22 to 25 years
old | Not mentioned | Cohort trial | 5 to 12 | (23) |
| Zhang | 2010 | 128/33 | 15-76 years
old | Not mentioned | Cohort trial | 6 to 18 | (30) |
| Yang et
al | 2009 | 102/97 | 6-73 years old | Open 9 | Cohort trial | 6 to 12 | (32) |
| Ji et
al | 2010 | 53/79 | 25 to 67 years
old | Not mentioned | Cohort trial | 24 | (29) |
| Ren | 2016 | 53/76 | 27-76 years
old | Not mentioned | Randomized
controlled study | | (17) |
Qualitative evaluation and bias risk
assessment of the included studies
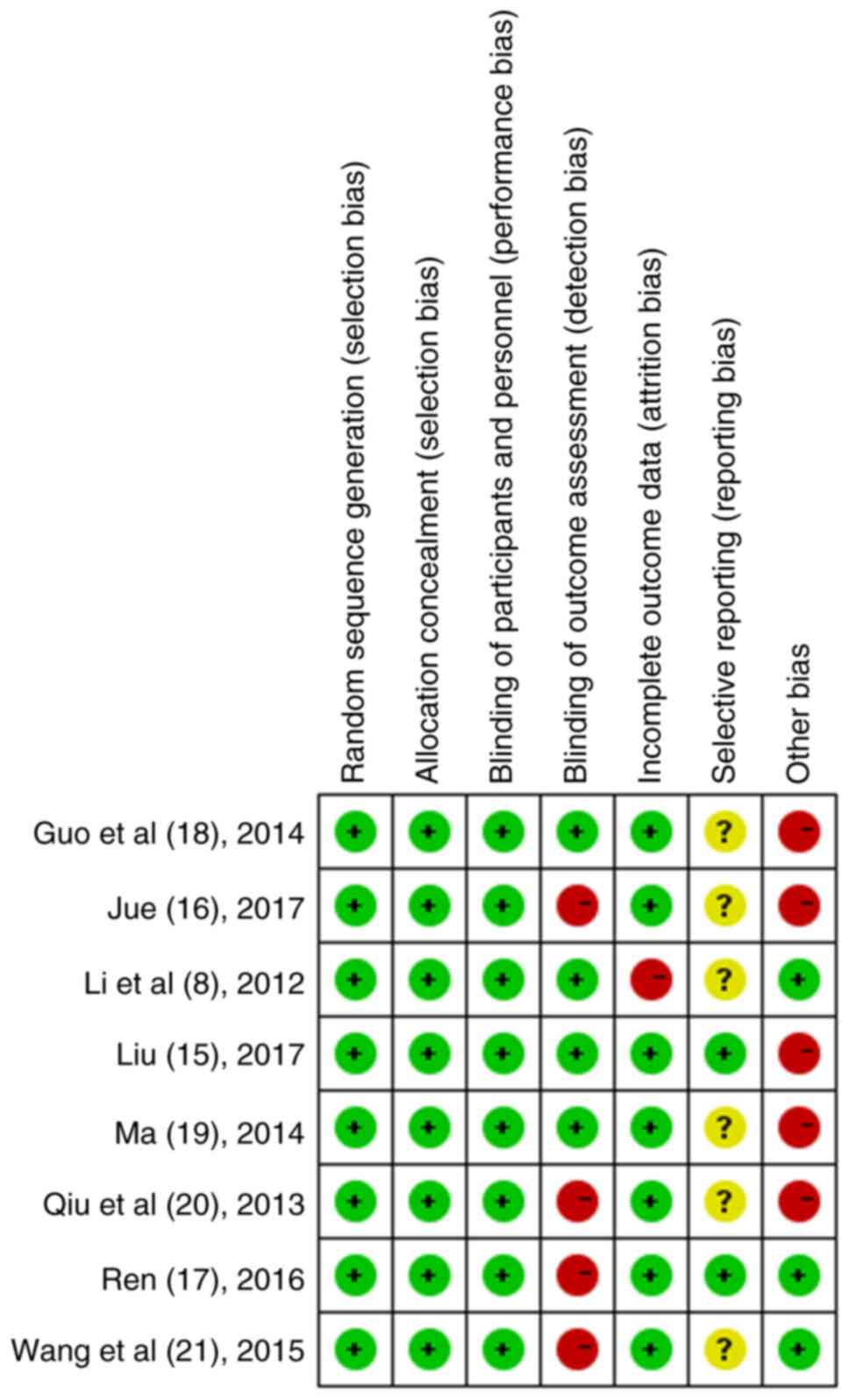
There were 20 studies, including eight randomized
controlled studies (8,15-21)
and 12 cohort trials (22-33).
Participants were treated for mid-clavicular fractures within a
certain period of time, and not all studies provided criteria for
inclusion. The evaluation criteria for a post-operative good rate
were not consistent. All the studies covered mid-clavicle fractures
and provided specific surgical procedures. For the included
studies, it was not suggested that all treatments were treated
using the blind method, and the sample size of each study was not
arranged in advance, and the end point of evaluation of the
post-operative rehabilitation status of the patients was also
randomly determined. The bias risk assessment of the included
randomized controlled studies is illustrated in Fig. 3, and the quality assessment of the
cohort studies is presented in Table
II.
 | Table IIQuality evaluation of the cohort
studies, all of which were >6 points. |
Table II
Quality evaluation of the cohort
studies, all of which were >6 points.
| | Case selection | | Outcome
measure | |
|---|
| Author/(Refs.) | Year of
publication | 1 | 2 | 3 | 4 | Comparability | A | B | C | Score |
|---|
| Li (25) | 2014 | * | * | * | * | ** | | * | * | 8 |
| Tian (26) | 2013 | | * | * | * | * | | * | * | 6 |
| Yang (22) | 2017 | * | * | * | * | ** | | * | | 7 |
| Lu and Du (31) | 2010 | | * | * | * | * | | * | * | 6 |
| Wang et al
(28) | 2011 | * | * | * | * | ** | | * | | 7 |
| Cheng (24) | 2015 | * | * | * | * | ** | * | | | 7 |
| Bu et al
(33) | 2006 | * | * | * | * | ** | | * | | 7 |
| Zhang et al
(27) | 2012 | | * | * | * | * | | * | * | 6 |
| Chen et al
(23) | 2015 | * | * | * | * | * | * | * | * | 8 |
| Zhang (30) | 2010 | * | * | * | * | * | | * | | 6 |
| Yang et al
(32) | 2009 | | * | * | * | * | * | * | * | 7 |
| Ji et al
(29) | 2010 | * | * | * | * | * | | * | | 6 |
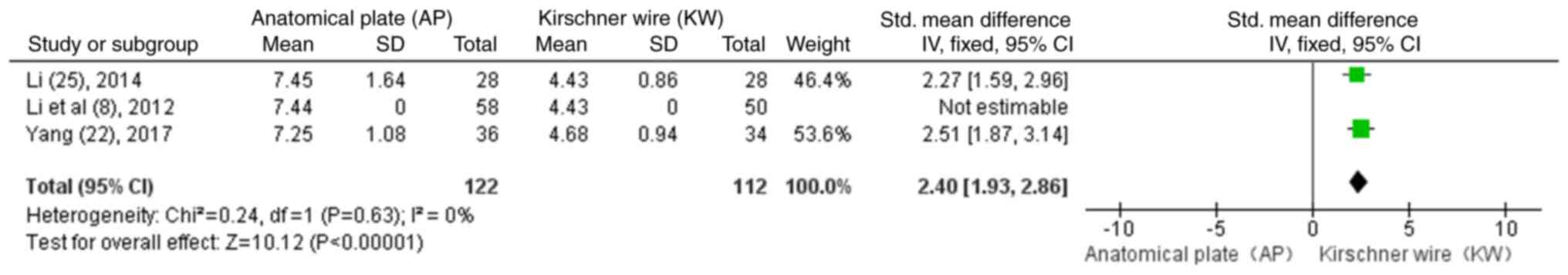
Average incision length
Of the 20 studies included, there were three studies
(8,22,25) that
included the average incision length, as shown in Fig. 4. The results revealed that the
incision length of the AP group was higher than that of the KW
group (SMD=2.40; 95% CI, 1.93-2.86; P<0.00001).
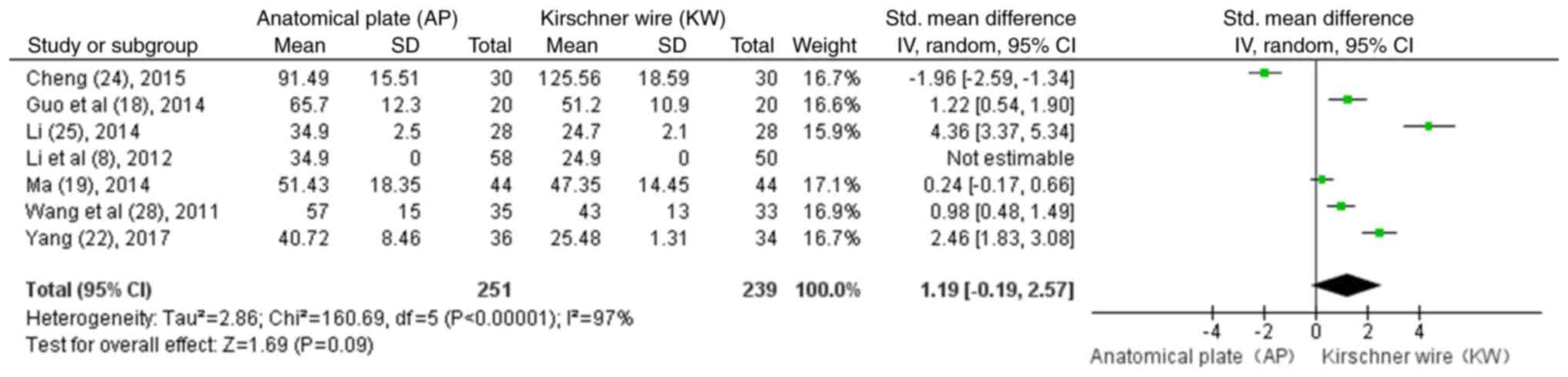
Average duration of surgery
Of all the studies that were subjected to the
meta-analysis, there were seven studies (8,18,19,22,24,25,28)
that demonstrated the results of duration of surgery, as shown in
Fig. 5. The results revealed that
there were no significant differences (P>0.05) in the duration
of surgery between the AP and KW group in the treatment of
mid-clavicle fractures (SMD=1.19; 95% CI, -0.19-2.57; P=0.09).
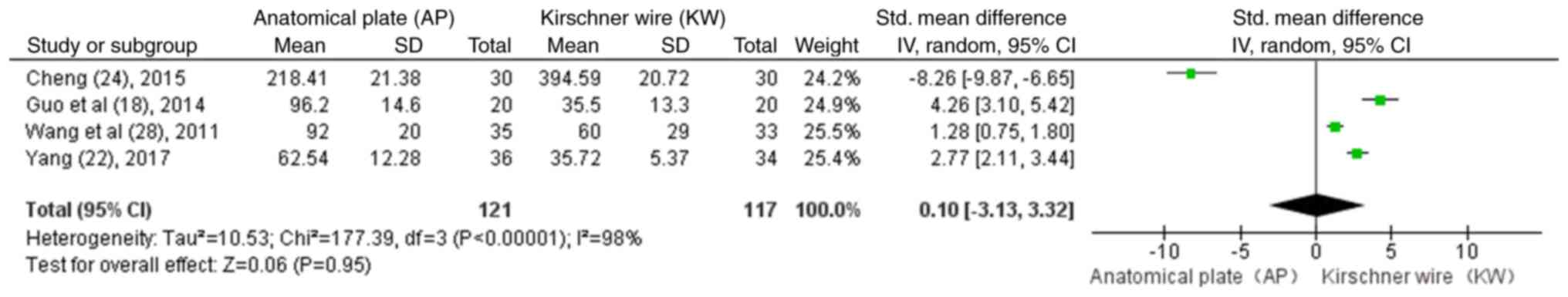
Bleeding/blood loss
At the time of the meta-analysis, there were four
studies (18,22,24,28) that
included the findings of any bleeding associated with the
treatments, as shown in Fig. 6. The
results revealed that there were no significant differences
(P>0.05) in blood loss between the AP and KW group in the
treatment of mid-clavicle fractures (SMD=0.10; 95% CI, -3.13-3.32;
P=0.95).
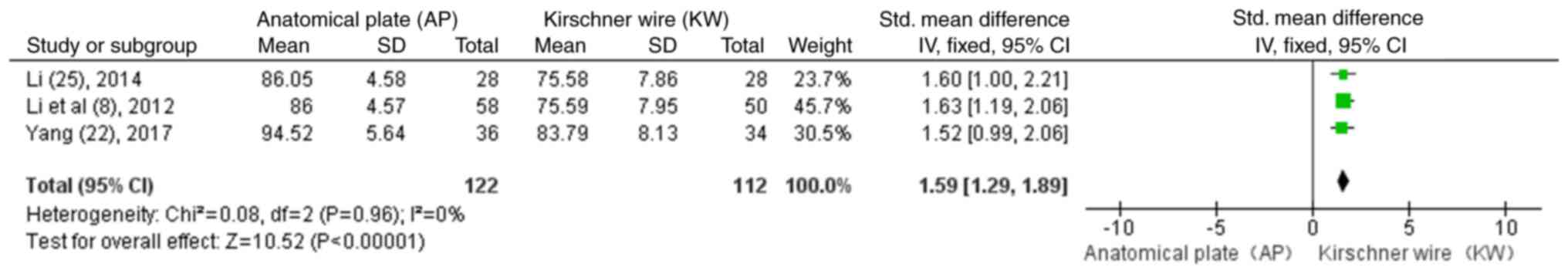
Constant function score (6
months)
There were three studies found for the comparison of
the constant function scores (8,22,25), as
shown in Fig. 7. The SMD from the
three studies was 1.59 (95% CI, 1.29-1.89; P<0.00001). These
results revealed that compared with the KW group, the AP group had
a better recovery of function following surgery (P<0.05).
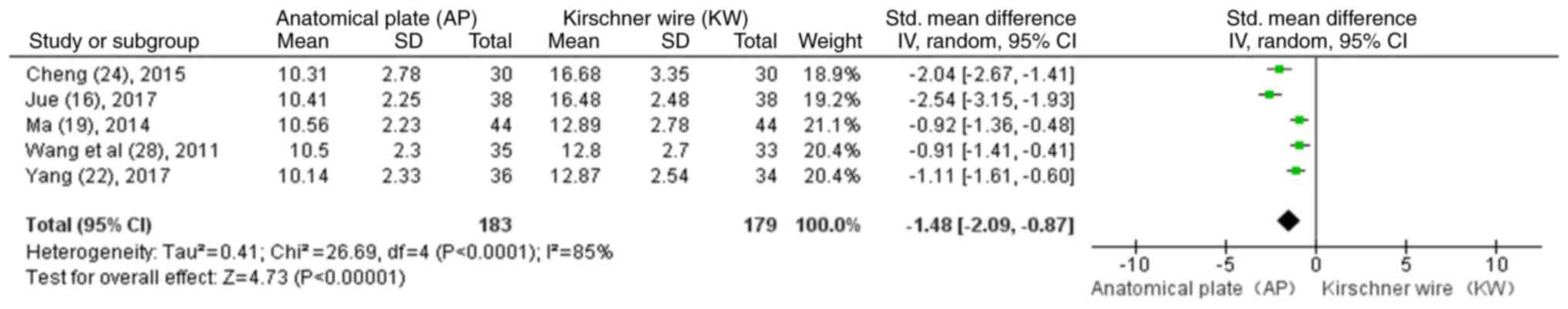
Fracture healing time (weeks)
There were five studies available for the comparison
of the fracture healing time (16,19,22,24,28), as
shown in Fig. 8. The SMD obtained
from the analysis of the data from these five studies was -1.48
(95% CI, -2.09 to -0.87; P<0.00001). These results revealed that
the AP group had a shorter fracture healing time than the KW group
(P<0.05).
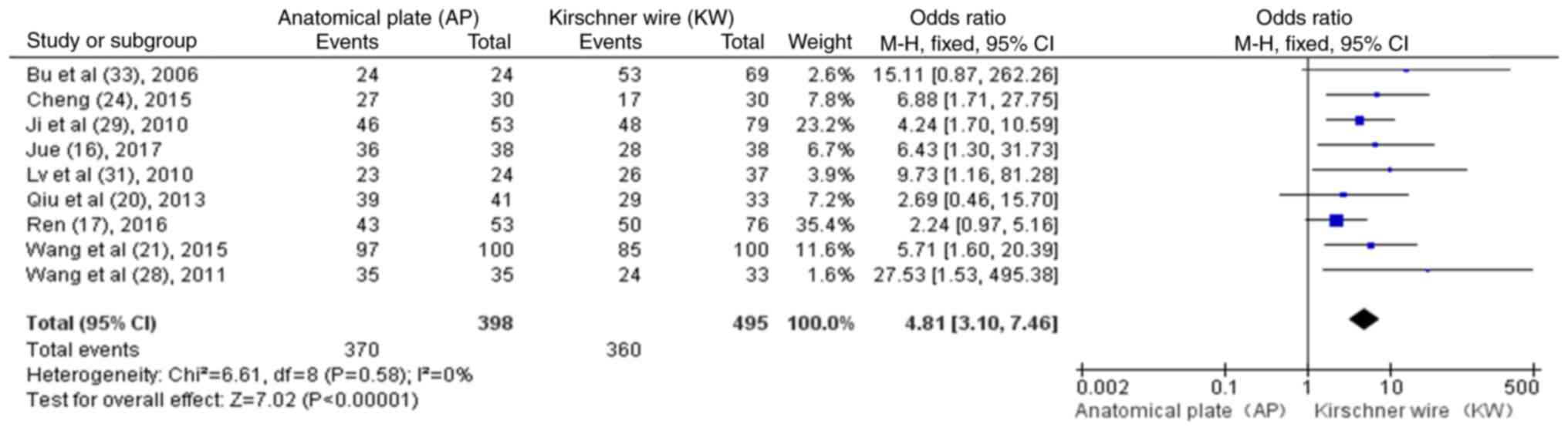
Post-operative efficacy
assessment
There were nine studies available for the assessment
of the post-operative efficacy of the two surgical methods
(16,17,20,21,24,28,29,31,33), as
shown in Fig. 9. The results
revealed that compared with the KW group, the AP group had a better
post-operative recovery rate (OR, 4.81; 95% CI, 3.10-7.46;
P<0.00001; P<0.05).
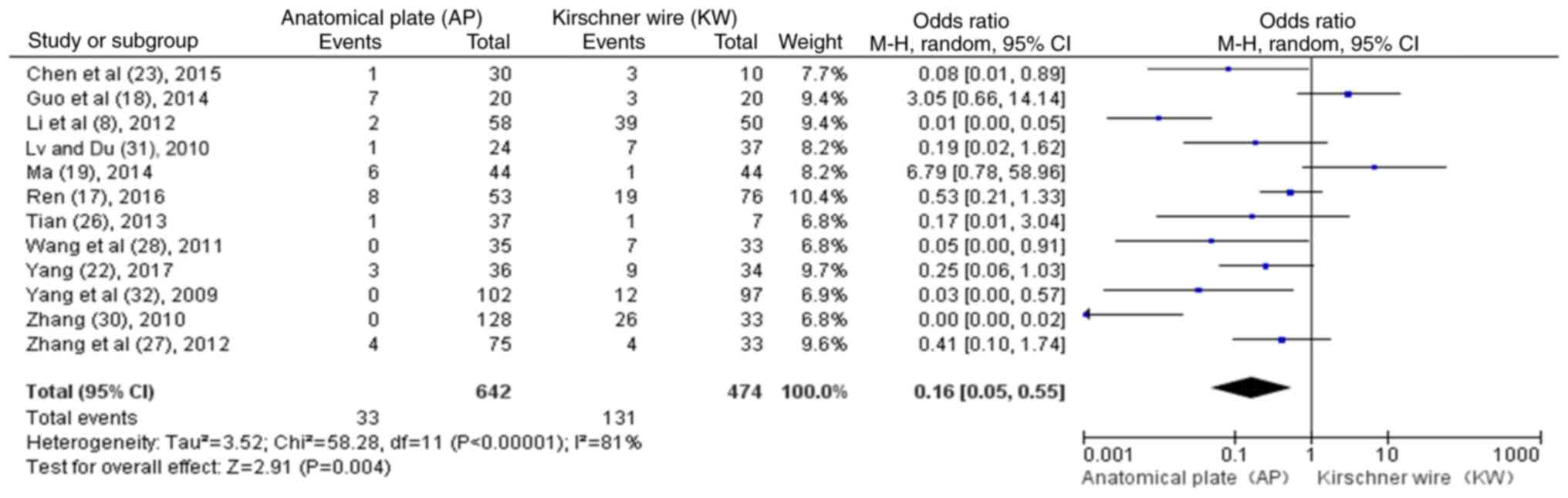
Complications
There were 12 studies available on the incidence of
post-operative complications between the two surgical methods
(8,17-19,22,23,26-28,30-32),
as shown in Fig. 10. The results
revealed that compared with the KW group, the AP group had a
relatively lower incidence of post-operative complications (OR
0.16; 95% CI, 0.05-0.55; P=0.004; P<0.05).
Discussion
Mid-clavicle fractures are the most common fractures
of the clavicle. For the treatment of mid-clavicle fractures,
particularly comminuted or unstable fractures, early surgical
treatment is crucial for fracture healing and the avoidance of a
second surgery. In the present study, through the analysis of the
related studies of the treatment of mid-clavicle fractures with AP
and KW fixation, it was found that the AP treatment of mid-clavicle
fractures was associated with a better fracture healing, a shorter
healing time, an improved post-operative function recovery, and the
incidence of post-operative complications was significantly reduced
compared with the KW group.
The credibility of a meta-analysis is dependent upon
the quality of each study included. In the present meta-analysis,
20 Chinese studies were retrieved from the databases searched. Of
the included studies, only eight mentioned the randomization of
patients, and only two of these mentioned randomizations by number
(15,18). However, none of these randomized
controlled studies mentioned that participants and treatments were
assigned in a blinded manner. None of the studies was prospectively
designed for sample size, and the end points of follow-up for each
study case were randomized. Therefore, these deficiencies undermine
the credibility of the study.
The KW is a commonly used means of internal fixation
in clinical practice; however, it has no compression effect on the
fracture end, and thus the displacement of the broken end and the
occurrence of needle retreats are possible (8). The post-operative movement range of the
KW is small, which often requires cervical wrist band fixation,
severely affecting early movement. Although the present
meta-analysis found that KW fixation had a smaller incision, the
straightforward application of KW fixation was found to result in
post-operative fracture end displacement, poor healing and a high
rate of complications, which severely limit its clinical
application. The AP has excellent adhesion and can be attached only
with slight molding. It has a large post-operative mobility of the
affected limbs and can be used for initial functional exercise and
daily activities. However, excessive periosteum dissection can lead
to delaying fracture union or bone non-union in order to achieve
better adhesion.
The clavicle is the bone support structure
connecting the scapula to the trunk. By attaching ligaments and
muscles to the clavicle, the shoulder joint can be further
stabilized. The state and time of clavicle healing severely affect
the early functional movement of the shoulder joint. The present
study found that compared with KW fixation, AP fixation has a wider
force surface, stronger pressure effect, better resistance to
bending stress and rotating force, and a higher biocompatibility.
It not only reduces the slippage of internal fixation, but can also
rapidly enter the functional training stage of the shoulder joint,
which is in accordance with a previous study (29), further reducing the occurrence of
periarthritis of the shoulder and joint stiffness.
The incidence of post-operative complications in the
AP fixation group was significantly lower than that in the KW
fixation group. Common post-operative complications include
fixation loosening, Kirschner wire bending, fixation fracture,
infection, needle withdrawal, malunion, and nonunion. However, in
the included studies, the studies on postoperative complications
were often limited in some aspects, which lead to a certain
deviation in the study of postoperative complications in the two
groups, and thus reduces the credibility of the meta-analysis.
By this meta-analysis, it was concluded that AP
fixation is significantly superior to KW fixation in a number of
aspects; however, there are some limitations that should be taken
into account. First of all, the time of fracture, age, screw type,
operative years, post-operative bandage fixation time, time to
start functional exercise and other factors for each study should
be considered; in addition, the consideration of post-operative
aesthetics and economic issues should also be considered. Despite
these limitations, the present study, to the best of our knowledge,
is the first to provide a comprehensive clinical basis for
comparing AP and KW fixation for the treatment of mid-clavicle
fractures, providing a more valuable theoretical basis for clinical
practice. The present study also had some limitations; it could not
independently analyze the use of the two materials for common and
complex clavicle fractures. In future studies, the authors aim to
separately perform the comparison of the two surgical methods (AP
and KW) for closed or open clavicle fractures, so as to further
reduce the errors caused by the complexity of the surgical methods,
affecting the credibility of the study.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during this study are
included in this published article.
Authors' contributions
The title selection and design of the study were
completed by DY and JZ. The retrieval, data extraction and analysis
of the study were completed by all authors (DY, JZ and LW). The
writing of the manuscript was completed by DY. The editing and
revision of the manuscript was completed by JZ. All authors have
read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
O'neill BJ, Hirpara KM, O'briain D, Mcgarr
C and Kaar TK: Clavicle fractures: A comparison of five
classification systems and their relationship to treatment
outcomes. Int Orthop. 35:909–914. 2011.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wang N, Zhang H, Yao Q, Wang Y, Dai S and
Yang X: TGFBI promoter hypermethylation correlating with paclitaxel
chemoresistance in ovarian cancer. J Exp Clin Cancer Res.
31(6)2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
d'heurrle A, Le T, Grawe B, Casstevens EC,
Edgington J, Archdeacon MT and Wyrick J: Perioperative risks
associated with the operative treatment of clavicle fractures.
Injury. 44:1579–1581. 2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Strauss BJ, Carey TP, Seabrook JA and Lim
R: Pediatric clavicular fractures: Assessment of fracture patterns
and predictors of complicated outcome. J Emerg Med. 43:29–35.
2012.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Krishna R and Mongia AK: Outcome of
surgical and conservative management of fractures of the
middle-third of the clavicle. Indian J Orthop Surg. 1:87–92.
2015.
|
|
6
|
Canadian Orthopaedic Trauma Society.
Nonoperative treatment compared with plate fixation of displaced
midshaft clavicular fractures. A multicenter, randomized clinical
trial. J Bone Joint Surg Am. 89:1–10. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Denard PJ, Koval KJ, Cantu RV and
Weinstein JN: Management of midshaft clavicle fractures in adults.
Am J Orthop (Belle Mead NJ). 34:527–536. 2005.PubMed/NCBI
|
|
8
|
Li YE, Tong Y, Ni QW, Tian NN and Wang CX:
A comparative study of anatomical plate and Kirschner wire fixation
in the treatment of middle clavicle fractures. Chin Med Herald.
9:162–163. 2012.(In Chinese).
|
|
9
|
Postacchjini F, Gumina S, De Santis P and
Albo F: Epidemiology of clavicle fractures. J Shoulder Elbow Surg.
11:452–456. 2002.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mckee MD, Pedersen EM, Jones C, Stephen
DJ, Kreder HJ, Schemitsch EH, Wild LM and Potter J: Deficits
following nonoperative treatment of displaced midshaft clavicular
fractures. J Bone Joint Surg Am. 88:35–40. 2006.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Zlowodzki M, Zelle BA, Cole PA, Jeray K
and McKee MD: Evidence-Based Orthopaedic Trauma Working Group.
Treatment of acute midshaft clavicle fractures: Systematic review
of 2144 fractures: On behalf of the evidence-based orthopaedic
trauma working group. J Orthop Trauma. 19:504–507. 2005.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Stang A: Critical evaluation of the
Newcastle-Ottawa scale for the assessment of the quality of
nonrandomized studies in meta-analysis. Eur J Epidemiol.
25:603–605. 2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Higgins JP, Thompson SG, Deeks JJ and
Altman DG: Measuring inconsistency in meta-analyses. BMJ.
327:557–560. 2003.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lau J, Ioannidis JP and Schmid CH:
Quantitative synthesis in systematic reviews. Ann Intern Med.
127:820–826. 1997.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Liu HF: The effect of anatomical plate
internal fixation on the treatment of 70 cases of middle clavicle
fractures and its influence on the shoulder joint function of
patients. Chin Minkang Med. 29:49–50. 2017.(In Chinese).
|
|
16
|
Jue LL: Clinical analysis of anatomical
locking plate in the treatment of middle clavicle fractures. Mod
Health: 149, 2017. kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFDLASN2017&filename=YSXD201704133&uniplatform=NZKPT&v=EFijtKCLk%25mmd2FrRT069bZ7Hbmdx4ZcQUM6nPCQ5Ren%25mmd2BMgSsVyghjsmWDhbCmMjCDpHn.
|
|
17
|
Ren XH: Comparison of treatment methods
for middle-aged, young and old patients with fracture of the middle
third of the clavicle. Prim Med Forum. 20:4216–4218. 2016.(In
Chinese).
|
|
18
|
Guo WQ, Zeng ZH and Liu WJ: Analysis of
curative effect of cluster Kirschner wire and anatomical plate in
the treatment of middle clavicle fracture. Mod Hosp. 14:53–56.
2014.(In Chinese).
|
|
19
|
Ma ZY: Application of anatomical plate in
emergency operation of comminution fracture of the middle clavicle.
J Qiqihar Med Coll. 35:1601–1602. 2014.(In Chinese).
|
|
20
|
Qiu YF and Xiao DJ: Analysis of the
curative effect of three internal fixation methods in the treatment
of middle clavicle fractures. Chin Med Innovation. 10:107–109.
2013.(In Chinese).
|
|
21
|
Wang Q, Yang F and Cui B: Analysis of
three methods of intramedullary fixation in the treatment of
mid-clavicle fracture. Med Inf. 24:244–245. 2015.(In Chinese).
|
|
22
|
Yang XK: Comparison of the effects of
internal fixation with anatomical plates and Kirschner wires on
shoulder joint function and complications in patients with middle
clavicle fractures. Chin Med Innovation. 14:59–62. 2017.(In
Chinese).
|
|
23
|
Chen JG, Liu B and Li ZD: Comparison of
the curative effect of three surgical methods for clavicle
fracture. Med Theory Pract. 28:3225–3226. 2015.(In Chinese).
|
|
24
|
Cheng J: Clinical research significance of
anatomic locking plate in the treatment of mid-clavicle fracture. J
Qiqihar Med Coll. 36:2559–2560. 2015.(In Chinese).
|
|
25
|
Li YW: The effect of S-shaped anatomical
plate in the treatment of 28 cases of fractures of the middle and
outer 1/3 of the clavicle. Contemp Med Essays. 12(50)2014.(In
Chinese).
|
|
26
|
Tian WG: Analysis of surgical treatment of
unstable middle clavicle fractures. Mod Diagn Treat. 24:2593–2594.
2013.(In Chinese).
|
|
27
|
Zhang WW, Yang JW, Hu XY, Li CJ, Wang B
and Ren XH: Surgical treatment of unstable middle clavicle
fractures. J Clin Orthop. 15:345–346. 2012.(In Chinese).
|
|
28
|
Wang T, Ye CQ and Chen GF: Comparison of
the effect of internal fixation with anatomical steel plate and
Kirschner wire in the treatment of middle clavicle fractures. Chin
Med Clin. 11:1313–1314. 2011.(In Chinese).
|
|
29
|
Ji SJ, Ning SY, Qiao WS, Zhao Y, Qi X, Li
SQ, Yang C and Yang JG: Comparison of treatment methods for
middle-aged, young and old patients with fracture of the middle
third of the clavicle. Chin J Gerontol. 30:2683–2684. 2010.(In
Chinese).
|
|
30
|
Zhang NS: Analysis of curative effect of
different internal fixation methods for middle clavicle fractures.
Chin J Bone Joint Injury. 25:449–450. 2010.(In Chinese).
|
|
31
|
Lv PC and Du XY: Comparison of internal
fixation with anatomical plate and kirschner wire in the treatment
of comminution fracture of the middle clavicle. J Clin Orthop.
13(115)2010.(In Chinese).
|
|
32
|
Yang SF, Chen J, PU ZK and Liu CC:
Different internal fixation options for middle clavicle fractures.
West Chin Med. 24:85–87. 2009.(In Chinese).
|
|
33
|
Bu BX, Zhang J, Shi FM, Cao HY and Ma HS:
Comparison of clinical efficacy of three internal fixation methods
in the treatment of clavicle fracture. Chin J Orthop Trauma.
2:66–67. 2006.kns.cnki.net/kcms/detail/detail.aspx?dbcode=CJFD&dbname=CJFD2006&filename=ZGZG200602032&uniplatform=NZKPT&v=diBeVwsph777%25mmd2BbgnEjYCKtl%25mmd2B0unz1dsE8AsylI4wbVExhJ9rqAxlj%25mmd2FyAZnqifFEM.
|