Introduction
Gout flares are treated using anti-inflammatory
agents, such as corticosteroids, non-steroidal anti-inflammatory
drugs and colchicine, while allopurinol is the first-line drug used
in urate-lowering therapy (ULT) to dissolve urate crystals,
suppress gout flares and resolve tophi (1,2).
However, the current treatment strategies are largely suboptimal,
with up to 89% of hospitalizations being preventable owing to
inadequate care (3). Recently, the
nurse's role in managing gout has expanded (4) to include members of multidisciplinary
teams (2), whereas the number of
nurse-led clinics has increased with promising results (5,6). The
present study aimed to identify barriers to optimal gout treatment
(Q1), understand how frequently nurses are involved in the
management of gout (Q2), and examine the role of the nurse in the
management of gout (Q3).
Data and methods
Sources and study selection
A systematic review was performed, focusing on
published evidence. The computerized literature search involved
three databases (PubMed, Google Scholar and Scopus). The search
criteria used are depicted in Table
I. Two authors (VEG and PT) assessed the titles and abstracts
of studies to eliminate records based on the study design.
Additional studies were discarded after reading the full-text
document. The reference lists of the gathered records were searched
for additional citations. Two authors (MT and PT) appraised the
quality of the gathered items based on the risk of bias,
independently. Consensus and randomized controlled studies were
considered to have a ‘low risk’ of bias, observational studies had
‘intermediate risk’, and case series and qualitative studies had a
‘high risk’. The overall quality of the available evidence was
assessed using the GRADE recommendations (7).
 | Table ISearch eligibility criteria of the
systematic review according to PICO. |
Table I
Search eligibility criteria of the
systematic review according to PICO.
| Frame | P (patients,
participants, population) | I (intervention) | C (comparator/
reference test) | O (outcome) | Time |
|---|
| Mesh terms | #1. Adults #2. ‘Gout’
OR ‘Uric acid arthritis’ #3. ‘Nurse’ OR ‘Nursing’ #4. English
language | #5. ‘Any’ | #6. ‘Any’ | #7. ‘Any’ | Search period
duration: 2010 to 2020 | Last search: April,
2020 |
| Search | #1 AND #2 AND #3 AND
#4 AND #5 AND #6 AND #7 |
| Example in
Scopus: | [TITLE (nurse) OR
TITLE (nursing) AND TITLE-ABS-KEY (gout) OR TITLE-ABS-KEY (uric AND
acid AND arthritis)] AND PUBYEAR >2010 |
| Exclusion
criteria | Irrelevant title or
abstract, irrelevant full-text, editorial, reviews, case-reports,
meta-analysis, pediatric/neonatal studies, experimental/nonhuman
studies, non-English studies, experimental studies. |
| Sources | Databases (PubMed and
Scopus) |
| | Reference list |
Results
Literature search results
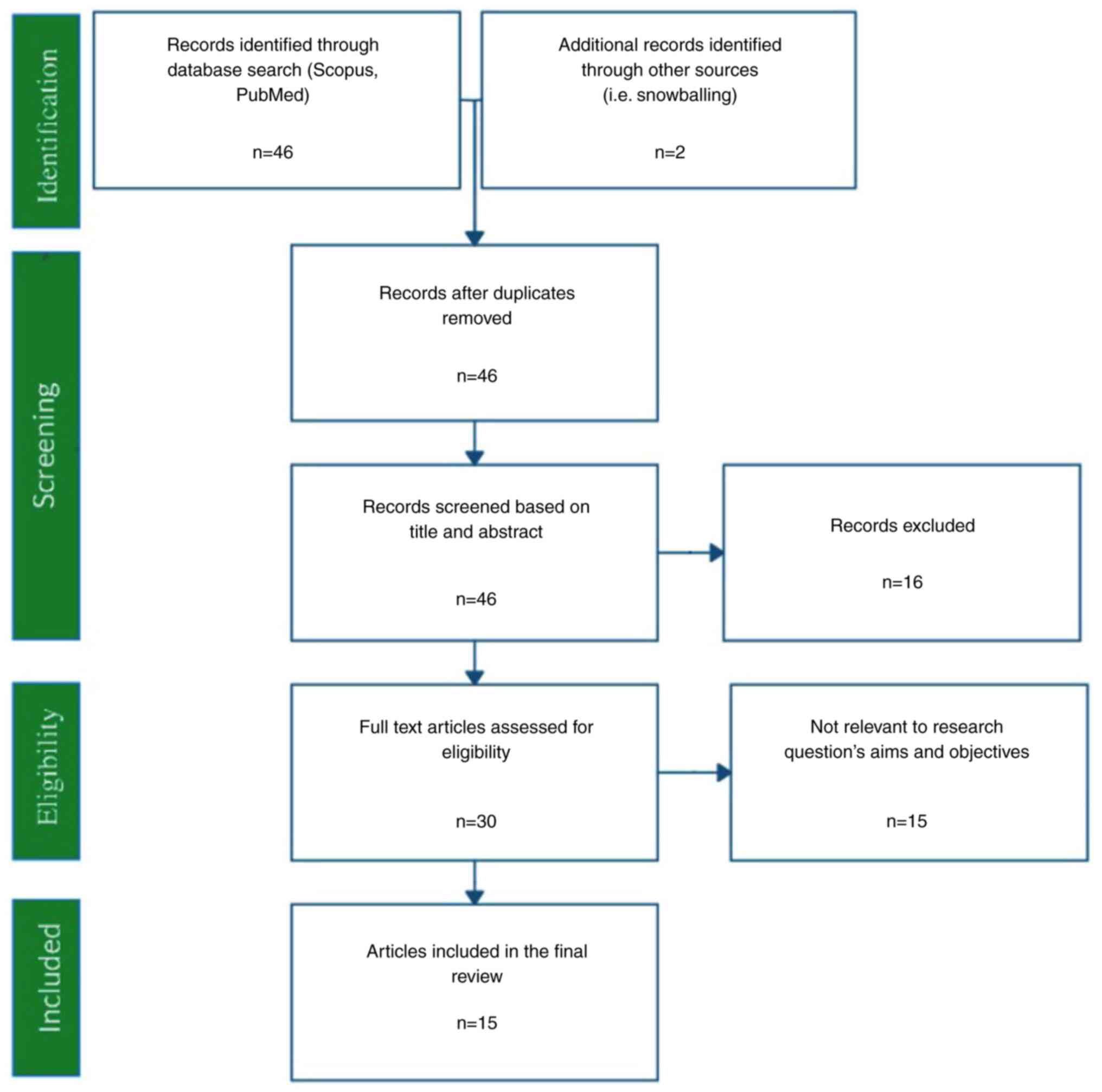
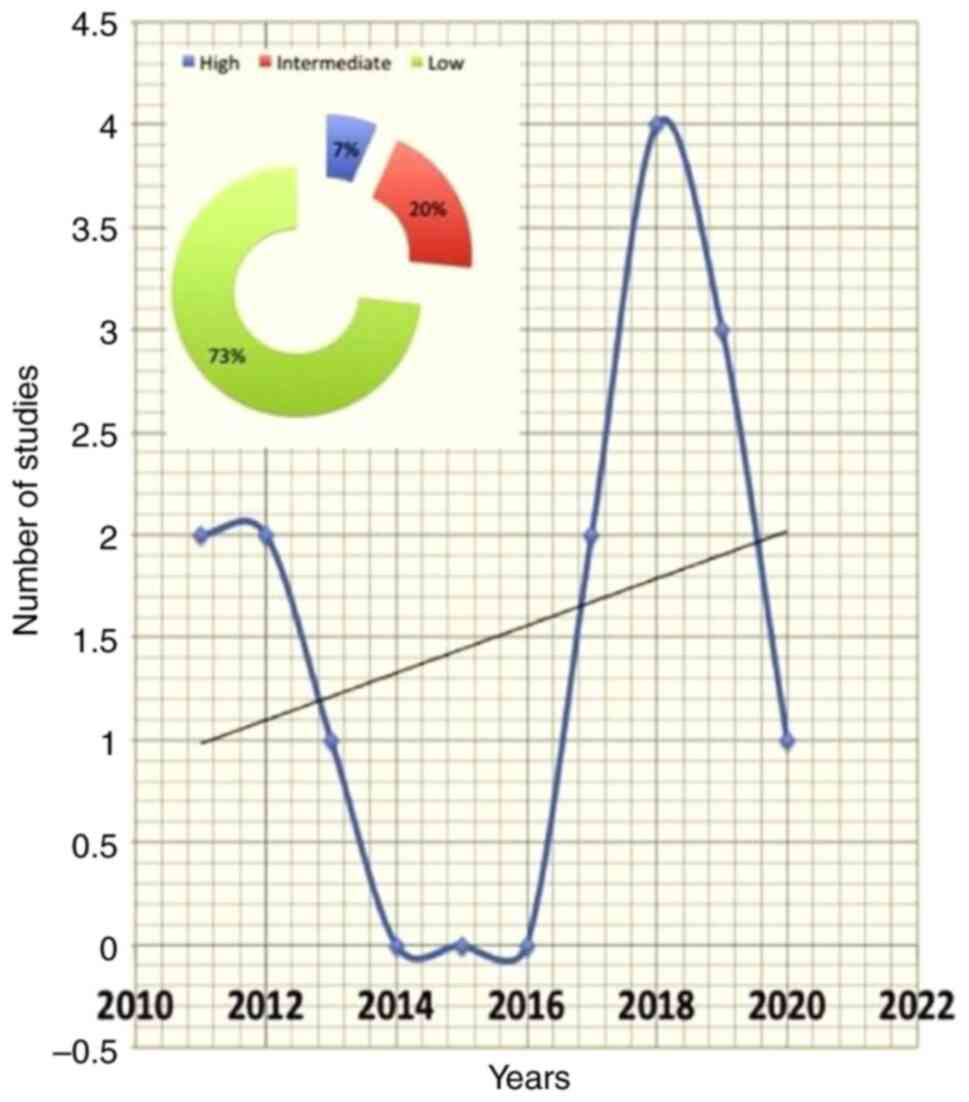
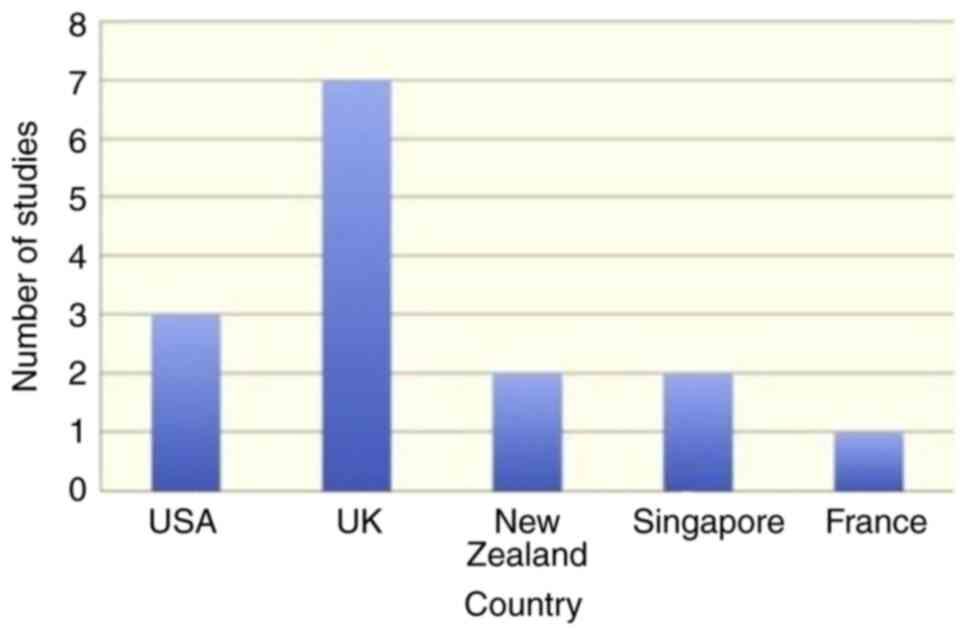
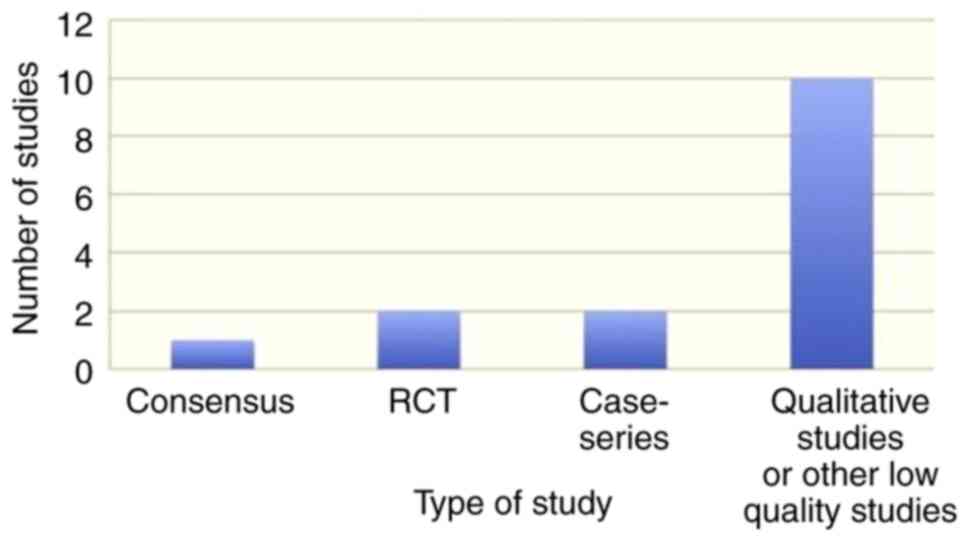
The literature search resulted in 46 records, and
two additional studies were traced through the references (Fig. 1). In total, 15 records fulfilled the
eligibility criteria and were used in the present systematic review
(Tables II and III). The gathered items included one
consensus, two randomized controlled trials, one review, one
longitudinal study, two cross-sectional studies, three case series
and five qualitative studies. The majority of the studies were
conducted in the UK and the USA. The ‘high’, ‘intermediate’ and
‘low’ quality studies accounted for 7, 20 and 73% of the available
evidence, respectively (Fig. 2,
Fig. 3 and Fig. 4). The data obtained on the role of on
nurses' role in managing gout were categorized into the
following:
 | Table IIBibliometric characteristics of the
eligible studies. |
Table II
Bibliometric characteristics of the
eligible studies.
| Author(s) | Year | Country | Citations | Level of
Evidence | Journal | Impact factor of
Journal | Study design | Question | (Refs.) |
|---|
| MacLachan et
al | 2011 | New Zealand | 6 | 4 | Eur J Cardiovasc
Nurs | 2.65 | Longitudinal
study | Q3 | (18) |
| Singh et
al | 2011 | USA | 34 | 5 | Semin Arthritis
Rheum | 5.07 | Cross-sectional
study | Q2 | (13) |
| Spencer et
al | 2012 | UK
(Nottingham) | 116 | 5 | Annals of the
Rheumatic Diseases | 14.30 | Qualitative | Q1 | (8) |
| Dalbeth | 2012 | New Zealand | 0 | 5 | Nature Reviews
Rheumatology | 18.54 | Review | Q3 | (15) |
| Rees et
al | 2013 | UK
(Nottingham) | 171 | 4 | Annals of the
Rheumatic Diseases | 14,30 | Prospective case
series | Q3 | (14) |
| Fields et
al | 2017 | USA | 17 | 5 | Semin Arthritis
Rheum | 5.07 | Case series | Q3 | (17) |
| Abhishek et
al | 2017 | UK
(Nottingham) | 22 | 5 | Rheumatology | 5.25 | Cross-sectional
study | Q3 | (16) |
| Seow et
al | 2018 | Singapore | 2 | 5 | Clinical Nursing
Research | 1.50 | Qualitative | Q1 | (11) |
| Chua et
al | 2018 | Singapore | 4 | 5 | Journal of Clinical
Nursing | 1.76 | Case series | Q1 | (12) |
| Doherty et
al | 2018 | UK
(Nottingham) | 27 | 1b | The Lancet | 59.10 | Randomized
controlled trial | Q3 | (5) |
| Erwin et
al | 2018 | UK (Cardiff) | 4 | 5 | Musculoskeletal
Care | (-) | Qualitative | Q3 | (19) |
| Mirmarin et
al | 2019 | USA | 1 | 1a | The Journal of Foot
and Ankle Surgery | 1.04 | Consensus | Q3 | (4) |
| Latif et
al | 2019 | UK
(Nottingham) | 4 | 5 | Joint Bone
Spine | 3.28 | Qualitative | Q3 | (10) |
| Deprouw et
al | 2019 | France | 0 | 5 | Joint Bone
Spine | 3.28 | Qualitative | Q1 | (9) |
| Fuller et
al | 2020 | UK
(Nottingham) | 5 | 1b | Rheumatology
(Oxford) | 7.04 | Randomized
controlled trial | Q3 | (6) |
 | Table IIISummary table with the basic
characteristics of the eligible studies. |
Table III
Summary table with the basic
characteristics of the eligible studies.
| Author(s) | Year | Participants | Intervention | Comparator | Outcome | Timing | (Refs.) |
|---|
| MacLachan et
al | 2011 | Patients with gout
and initial 5-year risk N10% for cardiovascular disease | Nurse-led
multidisciplinary | | The prescription of
aspirin, statins, nicotine replacement therapy, uptake of
self-reported activity levels, mean systolic and diastolic blood
pressure, with a trend towards reduced cigarette smoking | | (18) |
| Singh et
al | 2011 | Patients with
gout | (-) | (-) | Gout-related health
care utilization over | 1 year | (13) |
| Spencer et
al | 2012 | Mixed patients with
gout and care-givers | (-) | (-) | Patient and health
care providers beliefs and experiences about causes and
consequences of gout | (-) | (8) |
| Dalbeth | 2012 | Patients with
gout | Package of
care | (-) | (-) | (-) | (15) |
| Rees et
al | 2013 | Patients with
gout | Nurse-delivered
intervention that included education, individualized lifestyle
advice and appropriate ULT. | (-) | Percentage of
patients who had their SUA reduced below 360 µmol/l at | 1 year | (14) |
| Fields et
al | 2017 | Patients with
gout | Multi-disciplinary
team gout education and management program | (-) | Subject and
provider program evaluation questionnaires at 6 and 12 months,
program retention rate and success in reaching patients via monthly
calls. | 6 and 12
months | (17) |
| Abhishek et
al | 2017 | Patients with
gout | Nurse-delivered
intervention that included education, individualized lifestyle
advice and appropriate ULT. | (-) | Persistence and
adherence on ULT | 5 years | (16) |
| Seow et
al | 2018 | Patients with
gout | (-) | (-) | Living with
gout | (-) | (11) |
| Chua et
al | 2018 | Patients with
gout | (-) | (-) | Medication
adherence, gout perception, relations with doctors, ULT, social
support | (-) | (12) |
| Doherty et
al | 2018 | Patients with
gout | Nurse-led care | General
practitioner- led care | Percentage of
participants who achieved serum urate concentrations less than 360
µmol/l (6 mg/d), flare frequency, presence of tophi, quality of
life, and cost per quality-adjusted life-year (QALY) gained. | 2 years | (5) |
| Erwin et
al | 2018 | Expert panel | (-) | (-) | Competencies needed
by community- based nurses and AHPs | (-) | (19) |
| Mirmarin et
al | 2019 | American College of
Foot and Ankle Surgeon and the American Association of Nurse
Practitioners | (-) | (-) | (-) | (-) | (4) |
| Latif et
al | 2019 | Patients with
gout | Nurse- led complex
package | (-) | Perception of the
role of the nurse in engagement with the ULT | 18-26 months
after | (10) |
| Deprouw et
al | 2019 | Partners and
nurses | (-) | (-) | Knowledge and
representations | | (9) |
| Fuller et
al | 2020 | Patients with
gout | Nurse-led care | General
practitioner- led care | Satisfaction,
knowledge, flairs | Over 1 year | (6) |
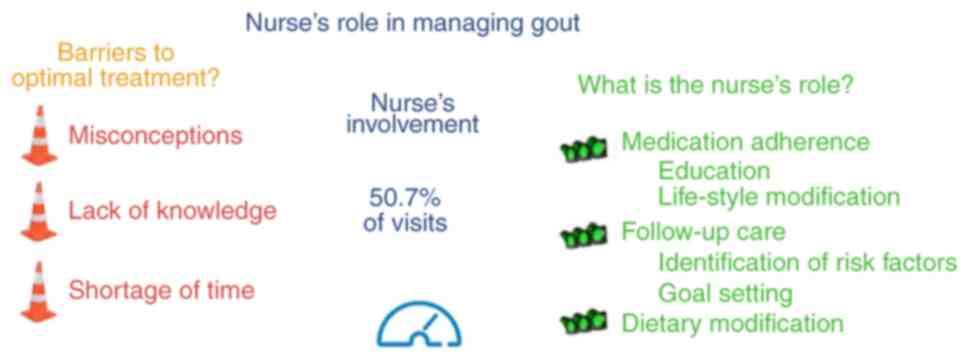
Barriers to optimal gout treatment
(Q1)
There is a small body of very low-quality evidence
regarding Q1 (Tables IV and
V). The main barriers were
attributed to the patients' experiences with gout and lay beliefs,
which affected seeking advice and adherence to treatment (8,9).
Misconceptions were preserved by the lack of understanding of the
causes and consequences of the disease and its response to
lifestyle change and the use of ULT (8,9). Gout
was considered self-inflicted or part of aging (8). The majority focused on managing acute
attacks rather than treating the underlying cause (8). The lack of knowledge by the health
professionals was reflected in the suboptimal information given to
patients and the reluctance to offer ULT as a ‘curative’ long-term
management strategy (8). The gaps in
knowledge were attributed to the absence of formal education on the
topic. Spouses highlighted that general practitioners did not have
time to educate patients (9). During
the flare of gout, feelings of powerlessness led to a delay in
seeking medical attention and patient withdrawal (9). Nurses regretted that they did not have
a sufficient amount of time to discuss issues with patients
(9). Several patients raised
concerns regarding the long-term use of ULT related to prescription
costs, polypharmacy, relative contraindications, overuse,
dependency, side-effects and long-term effects on health (10). Hearsay about these side effects
prevented them from following their doctor's prescriptions
(11). The female sex, marriage, the
absence of distracting factors (job) and the presence of multiple
co-morbidities were associated with higher rates of treatment
adherence (12).
 | Table IVGrading of the retrieved articles in
regard to the Quality of Evidence. |
Table IV
Grading of the retrieved articles in
regard to the Quality of Evidence.
| | Down-grade | Up-grade | |
|---|
| Question | Starting grade | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication
bias | Magnitude of
effect | Dose response | Confounding
factors | Final grade |
|---|
| What are the
barriers for the optimal gout treatment? (Q1) | 2 | -1 | 0 | 0 | 0 | -1 | +1 | 0 | 0 | 1 |
| How frequently are
nurses involved in the management of gout (Q2) | 1 | 0 | 0 | 0 | 0 | -1 | 0 | 0 | 0 | 0 |
| What is the role of
the nurse and is it effective? (Q3) | 4 | 0 | 0 | 0 | 0 | 0 | +1 | 0 | 0 | 5 |
 | Table VSummary-of-evidence table. |
Table V
Summary-of-evidence table.
| Question | Studies | Citations | Quality of
pertinent evidence (GRADE) | Relative risk (95%
CI) | Conclusions | Future
recommendations |
|---|
| What are the
barriers for the optimal gout treatment? (Q1) | 4 | 122 | Very low
quality | (-) | There is a small
body of very low-quality evidence that the main barriers for the
optimal gout treatment are related to the lack of patient education
on gout causes, risk factors, treatment modalities, including the
‘curative’ long-term management strategy | Further evidence
from high=quality studies is needed to validate the evidence across
countries and populations |
| How frequently are
nurses involved in the manage ment of gout (Q2) | 1 | 34 | Very low
quality | (-) | There is a small
body of very low-quality evidence that the nurse practitioners are
used by about 1/4 of patients, averaging approximately 2 visits per
year | High=quality
studies are needed to quantify the frequency of nurse involvement
across different countries and populations |
| What is the role of
the nurse and is it effective? (Q3) | 10 | 253 | High quality | 3.18
(2.42-4.18) | More patients
receiving nurse-led care had serum urate concentrations less than
360 µmol/l at 2 years than those receiving usual care. Meanwhile,
the cost per QALY gained for the nurse-led intervention was £5,066
at 2 years | High=quality
studies are required to identify the role of the clinical nurse in
physician-led clinics |
Frequency with which nurses are
involved in the management of gout (Q2)
There is limited evidence of poor quality with
regard to Q2. Singh et al (13) conducted a survey of 298 patients with
gout from three metropolitan areas to study healthcare utilization
patterns. The most utilized gout-related health care resource was
the primary care physicians, used by 60.4% of patients with a mean
annual utilization of 3.1 (SD 3.4) visits (13). Visits to rheumatologists and nurse
practitioners followed with 50.7% (3.7±5.7 annual visits) and 26%
(2.7-2.5 annual visits), respectively (13). Nurse practitioners, physician
assistants, urgent care and emergency department resources were
each used by approximately 1/4 of patients, averaging ~2 visits per
year (13). Overnight
hospitalization for gout was reported by #x003C;10% of patients
(13).
Role of the nurse and its
effectiveness (Q3)
The evidence regarding Q3 is sufficient and of high
quality. A consensus for gouty arthritis agreed that
‘multidisciplinary referral provides optimal care in cases of
recalcitrant gout’ and that ‘patient education should include
dietary modification, medication adherence, and follow-up care with
their assigned health care providers’ (4).
Indeed, increased adherence to treatment was
achieved by nurse-led interventions, including education and
lifestyle counseling (14,15). The educational programs provided
detailed information about the cause of the disease and known risk
factors, the risk of irreversible joint damage and treatment
options, such as individualized risk factor modification and ULT
(14). The success rate of these
nurse-led interventions in achieving the therapeutic target (SUA
≤360 µmol) at 12 months was as high as 92% (14), which remained at the 5-year follow-up
(16). Other programs included a
nursing educational intervention via a structured curriculum and
monthly follow-up calls from pharmacists to emphasize adherence to
management programs) (17). The
majority of subjects confirmed the usefulness of the overall
program in understanding and managing their gout and appreciated
the role of the nurses and pharmacists in 81 and 50% of the
responders, respectively (17).
Furthermore, these programs corrected misconceptions about bridge
therapy, the possibility of being flare-free, and the genetic
component of gout (17).
The Nottingham Gout Treatment Trial compared
nurse-led gout care to usual care led by general practitioners for
people in the community in a randomized controlled study (5). More patients receiving nurse-led care
had serum urate concentrations #x003C;360 µmol/l at 2 years than
those receiving usual care (risk ratio, 3.18; 95% confidence
interval, 2.42-4.18) (5). Moreover,
the cost per quality-adjusted life year gained for the nurse-led
intervention was £5,066 at 2 years (5). Participants described that the
nurse-led intervention facilitated engagement with ULT, namely by
providing improved knowledge and understanding of gout and its
treatment, involvement of patients in decision-making about
treatment, increased confidence about the benefits of treatment,
and encouragement to persist with ULT (10). Among the reasons for ULT
discontinuation in the nurse-led arm were the absence of flares,
experience of side-effects, being frustrated with taking the
tablets, and the interruption of ULT prescription by the general
practitioner (6).
McLachlan et al (18) investigated a nurse-led
multidisciplinary approach to improving CVD risk management in
patients with gout. Any areas the patient with a 5-year CVD risk
>10% felt willing and confident to manage (smoking cessation,
physical activity, healthy eating, adherence to medication) were
addressed through self-management support and encouragement
(18). The prescription of aspirin,
statins, nicotine replacement therapy, uptake of self-reported
activity levels, and mean systolic and diastolic blood pressure,
markedly improved after 6 months (18).
Finally, it has been recognized that community-based
nurses require competencies to enable them to assess, care for and
manage arthritis appropriately (19). These competencies included an
understanding of the underlying pathology, the ability to
distinguish between the various types, and the ability to recognize
early warning signs, with an emphasis on osteoarthritis, rheumatoid
arthritis, gout and septic arthritis (19). In addition, nurses should be capable
of engaging in shared decision-making processes, goal setting,
providing patients with education and information, and making
appropriate referrals (19). In the
Nottingham Gout Treatment Trial, the nurses received specialized
training in the management of gout, including providing
individualized information and engaging patients in shared
decision-making (5).
Discussion
It has become apparent that the absence of proper
information prevents patients from adhering to optimal gout
treatment. Since nurses are involved in all phases of gout
treatment and are trusted in up to a fourth of the cases, the
specialized ‘rheumatology nurse’ concept has gained acceptance in a
limited number of countries, such as the UK and USA. Rheumatology
nurses have been adequately educated on all theoretical aspects of
gout, deliver a structured curriculum to the patients, and have
been trained in goal setting and engaging the patient in the
individualized shared-decision-making process. As a result,
institutions utilizing the ‘specialized rheumatology nurse’
exhibited higher adherence rates to ULT, an increased control of
gout flares and an improved quality of life of patients with gouty
(Fig. 5).
The concept of a ‘specialized nurse’ is not novel.
Pediatric nurse practitioners have been effective in promoting
breastfeeding (20). Nurse-led
clinics have also been very successful in managing hypertension and
diabetes mellitus (21,22). Emphasis should be placed on the
concept of multidisciplinary teams, where each member plays a
discrete role and works in harmony with the others. Frequently, a
rheumatologist constructs the curriculum and educates the other
members of the team (17). The
nurses then deliver the lessons to the patients, tailor the
management to the patient's needs and preferences, and monitor
adherence to treatment goals and outcomes. In Japan, it is common
for patients to receive dietary guidance from a general physician
after abnormal values are found during a physical examination
(23). Enlightenment is provided
through television health programs (24). The training of nurses with
specialized knowledge is taking place, although in small numbers
(25). Patient education that
provides detailed guidance to a wide range of patients is more
effective by nurses (25). In some
programs, pharmacists are also involved in patient motivation
(17).
The present systematic review has some critical
limitations which should be mentioned. It was based on a limited
number of studies, of which the majority are qualitative in design
with a significant risk of bias. However, it should be noted that
among the included studies, there were two well-conducted
randomized controlled studies (5,6) and the
results of a consensus meeting (4).
The majority of the studies were conducted at a single center
(5,6,10,14,16),
thus questioning the generalizability of the findings. Further
studies are thus required to validate the efficacy and efficiency
of the multidisciplinary teams in more high-quality studies,
considering the individual characteristics of various countries and
populations.
In conclusion, the present study demonstrated an
expanded role of nurses regarding the management of gout. Thus,
nurses are invited to improve their understanding of gout, its
pathogenesis and treatment, and to be capable of goal-setting and
shared decision-making. The goal is to educate patients with gout
to adhere to ULT and improve their quality of life without
increasing costs.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
PT and KP conceptualized the study. PT, EV, VEG, MT,
PP, AAF, GF and AGB analyzed the data from the studies for
inclusion in the systematic review, and wrote and prepared the
draft of the manuscript. AGB and KP provided critical revisions. GF
and AGB confirm the authenticity of all the raw data. All authors
contributed to manuscript revision and have read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dalbeth N, Choi HK, Joosten LAB, Khanna
PP, Matsuo H, Perez-Ruiz F and Stamp LK: Gout. Nat Rev Dis Primers.
5(69)2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Stamp LK and Dalbeth N: Prevention and
treatment of gout. Nat Rev Rheumatol. 15:68–70. 2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Rai SK, Choi HK, Choi SHJ, Townsend AF,
Shojania K and De Vera MA: Key barriers to gout care: A systematic
review and thematic synthesis of qualitative studies. Rheumatology
(Oxford). 57:1282–1292. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Mirmiran R, Bush T, Cerra MM, Grambart S,
Kauschinger E, Younger M and Zychowicz M: Joint clinical consensus
statement of the American college of foot and ankle surgeons® and
the American association of nurse practitioners®: Etiology,
diagnosis, and treatment consensus for gouty arthritis of the foot
and ankle. J Foot Ankle Surg. 57:1207–1217. 2018.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Doherty M, Jenkins W, Richardson H,
Sarmanova A, Abhishek A, Ashton D, Barclay C, Doherty S, Duley L,
Hatton R, et al: Efficacy and cost-effectiveness of nurse-led care
involving education and engagement of patients and a
treat-to-target urate-lowering strategy versus usual care for gout:
A randomised controlled trial. Lancet. 392:1403–1412.
2018.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Fuller A, Jenkins W, Doherty M and
Abhishek A: Nurse-led care is preferred over GP-led care of gout
and improves gout outcomes: Results of nottingham gout treatment
trial follow-up study. Rheumatology (Oxford). 59:575–579.
2020.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Schünemann H, Brożek J, Guyatt G and Oxman
A: GRADE handbook for grading quality of evidence and strength of
recommendations. GRADE Working Group, 2013. https://www.rama.mahidol.ac.th/ceb/sites/default/files/public/pdf/journal_club/2017/GRADE%20handbook.pdf.
|
|
8
|
Spencer K, Carr A and Doherty M: Patient
and provider barriers to effective management of gout in general
practice: A qualitative study. Ann Rheum Dis. 71:1490–1495.
2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Deprouw C, Guignot M, Bougeois-Sarran C,
Bougeois-Sarran C, Coblentz-Baumann L and Ea HK: Partners and
nurses' knowledge and representations of gout: A qualitative study.
Joint Bone Spine. 86:769–776. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Latif ZP, Nakafero G, Jenkins W, Doherty M
and Abhishek A: Implication of nurse intervention on engagement
with urate-lowering drugs: A qualitative study of participants in a
RCT of nurse led care. Joint Bone Spine. 86:357–362.
2019.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Seow LL, Jiao N, Wang W, Holroyd E, Teng
GG and He HG: A qualitative study exploring perceptions of patients
with gout. Clin Nurs Res. 29:56–65. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Chua XHJ, Lim S, Lim FP, Lim YNA, He HG
and Teng GG: Factors influencing medication adherence in patients
with gout: A descriptive correlational study. J Clin Nurs.
27:e213–e222. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Singh JA, Sarkin A, Shieh M, Khanna D,
Terkeltaub R, Lee SJ, Kavanaugh A and Hirsch JD: Health care
utilization in patients with gout. Semin Arthritis Rheum.
40:501–511. 2011.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Rees F, Jenkins W and Doherty M: Patients
with gout adhere to curative treatment if informed appropriately:
Proof-of-concept observational study. Ann Rheum Dis. 72:826–830.
2013.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Dalbeth N: Crystal arthritis: A new
‘package of care’ strategy for effective gout management. Nat Rev
Rheumatol. 8:507–508. 2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Abhishek A, Jenkins W, La-Crette J,
Fernandes G and Doherty M: Long-term persistence and adherence on
uratelowering treatment can be maintained in primary care-5-year
follow-up of a proof-of-concept study. Rheumatology (Oxford).
56:529–533. 2017.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Fields TR, Rifaat A, Yee AMF, Ashany D,
Kim K, Tobin M, Oliva N, Fields K, Richey M, Kasturi S and
Batterman A: Pilot study of a multidisciplinary gout patient
education and monitoring program. Semin Arthritis Rheum.
46:601–608. 2017.PubMed/NCBI View Article : Google Scholar
|
|
18
|
McLachlan A, Kerr A, Lee M and Dalbeth N:
Nurse-led cardiovascular disease risk management intervention for
patients with gout. Eur J Cardiovasc Nurs. 10:94–100.
2011.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Erwin J, Edwards K, Woolf A, Whitcombe S
and Kilty S: Better arthritis care: What training do
community-based health professionals need to improve their care of
people with arthritis? A Delphi study. Musculoskeletal Care.
16:48–59. 2018.PubMed/NCBI View
Article : Google Scholar
|
|
20
|
Hellings P and Howe C: Breastfeeding
knowledge and practice of pediatric nurse practitioners. J Pediatr
Health Care. 18:8–14. 2004.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Brown VM: Managing patients with
hypertension in nurse-led clinics. Nursing. 47:16–19.
2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Youngman S: The developing role of the
renal diabetes nurse. EDTNA ERCA J. 30:169–172. 2004.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Koguchi T: Modification of dietary habits
for prevention of gout in Japanese people: Gout and the Japanese
diet. Am J Health Res. 9:117–127. 2021.
|
|
24
|
Murdoch R, Mihov B, Horne AM, Petrie KJ,
Gamble GD and Dalbeth N: Impact of television depictions of gout on
perceptions of Illness: A randomized controlled trial. Arthritis
Care Res (Hoboken). 11:1–7. 2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Oliver S, Tam LS, Kwok GSK, Fusama M,
Nakahara H, Zhang CY, Yamamoto K and Furtner D: The Asia-pacific
initiative for rheumatology nurse education: current gaps,
programme development and future outlook. Musculoskeletal Care.
18:397–403. 2020.PubMed/NCBI View
Article : Google Scholar
|