Introduction
Primary hyperparathyroidism (PHPT) is one of the
most common causes of hypercalcemia with various etiologies among
outpatients. Parathyroid adenoma followed by parathyroid
hyperplasia is a frequent cause of PHPT, whereas carcinoma of the
parathyroid is the main cause of hypercalcemia in hospitalized
patients (1,2).
Granulomatous disorders are a type of chronic
inflammation caused by autoimmune diseases, allergies, infections,
toxins, and neoplastic conditions (3). Tuberculosis (TB) and sarcoidosis are
common granulomatous diseases that rarely affect the parathyroid
gland and their co-occurrence with a functioning parathyroid
adenoma leading to hypercalcemia is extremely uncommon (4,5). Vitamin
D [1,25(OH)2D3]-mediated granulomatous
disorder, along with osteoclast activation within the bones, is the
leading cause of high serum levels of calcium. The majority of
patients with granulomatous disease-related hypercalcemia do not
present with symptoms; however, in some cases, chronic
hypercalcemia may occur (6). To
date, at least to the best of our knowledge, only eight cases of
granulomatous inflammation of the parathyroid gland caused by TB
have been reported in the literature (4,7-13).
The present study reports a rare case of parathyroid
adenoma with caseating granulomatous inflammation leading to
hypercalcemia. The cited articles were assessed for eligibility
based on Kscien's list (14).
Case report
Patient information
A 58-year-old female patient with a positive history
of recurrent renal calculi presented to the Head and Neck clinic at
Smart Health Tower (Sulaimani, Iraq) with complaints of generalized
body aches and fatigue for about a year. The patient did not have
any notable previous surgical history or infection with TB.
Clinical findings
A physical examination did not reveal any notable
findings, and there was no associated palpable cervical
lymphadenopathy.
Diagnostic assessment
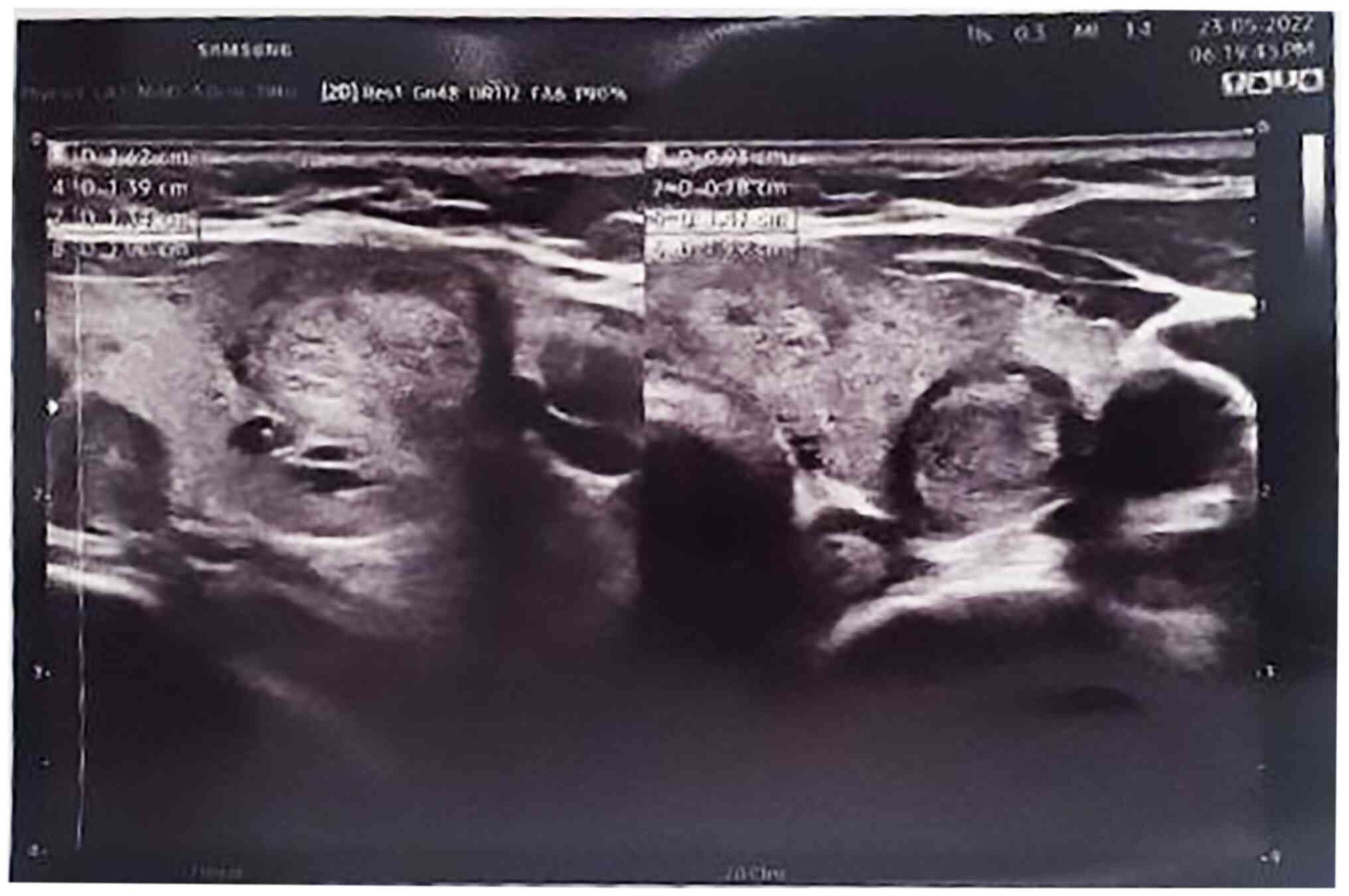
The results of blood analyses revealed a high level
of parathyroid hormone (PTH) (154.7 pg/ml) and serum calcium (11.26
mg/dl). An ultrasound examination of the neck revealed a
multinodular goiter with mildly suspicious (TR3) bilateral
homogeneous echo texture nodules measuring 4mm within the right
thyroid gland. The left thyroid gland showed a non-suspicious (TR2)
nodule measuring 13x9x8 mm and a mildly suspicious (TR3) nodule
measuring 10x9x7 mm. Below the left lower pole of the thyroid
gland, a solid hypoechoic hypovascular nodule of 20x7 mm was
observed, which suggested a parathyroid adenoma. No notable
cervical lymphadenopathy was observed (Fig. 1).
Therapeutic intervention
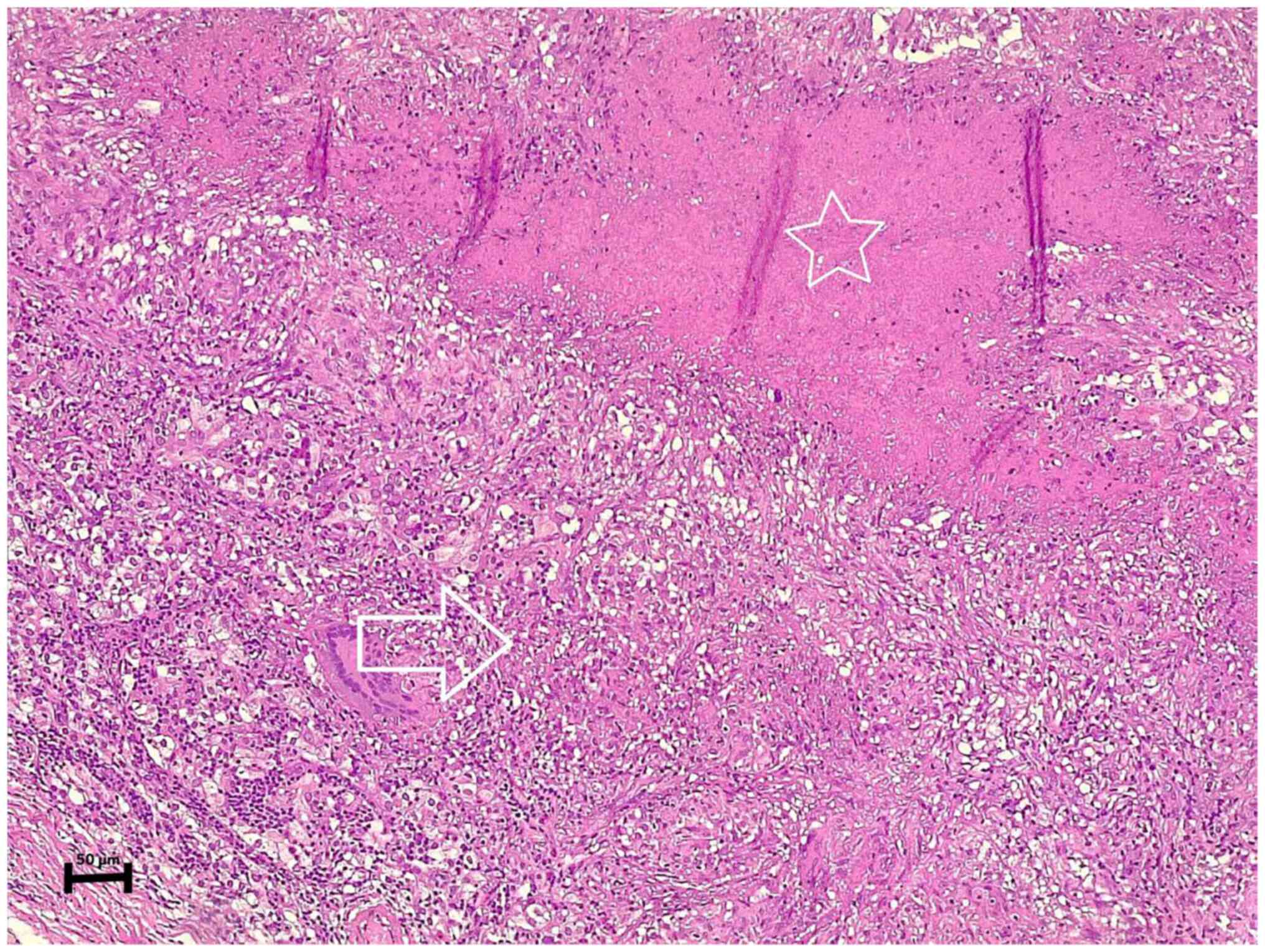
After proceeding to the left thyroid lobectomy and
excising the left parathyroid gland, the histopathological
examination revealed a parathyroid adenoma with caseating
granulomatous inflammation involving the adenoma, suggestive of TB
(Fig. 2). In addition, the left
thyroid gland exhibited a nodular goiter with focal lymphocytic
thyroiditis.
The histopathological examination was performed by
the authors' laboratory as follows: The sections (4-µm-thick) were
paraffin-embedded and fixed with 10% neutral buffered formalin at
room temperature for 24 h. They were subsequently stained with
hematoxylin and eosin (Bio Optica Co.) for 1-2 min at room
temperature and then examined under a light microscope (Leica
Microsystems GmbH).
Follow-up
The post-operative period was uneventful, and the
calcium level of the patient decreased to 10 mg/dl. A negative
acid-fast bacillus test (AFB) of sputum, as well as negative
findings from a chest X-ray were achieved post-operatively.
Subsequently, the symptoms resolved following the initiation of
treatment for TB (Rifampin, 600 mg, twice a day, for 6 months), and
the generalized body aches subsided.
Discussion
TB is a communicable disease that spreads by
coughing and typically affects the lungs (pulmonary TB).
Extrapulmonary TB may affect other parts of the body (15). The clinical symptoms of TB vary and
rely on the host and microbe features along with the interaction
between them. Extrapulmonary TB involvement tends to rise in
immunocompromised patients (16).
Hyperparathyroidism is categorized into three types, primary,
secondary, and tertiary hyperparathyroidism. Parathyroid adenoma is
the cause of almost 85% of primary hyperparathyroidism cases.
Parathyroid adenoma is a type of parathyroid proliferative disease.
Patients with primary hyperparathyroidism typically present with
elevated blood calcium levels with high parathyroid hormone levels
(17,18). However, the impact of primary TB on
parathyroid function remains unknown. Granulomatous inflammation of
endocrine organs usually leads to a decrease in the function of the
affected gland (8). However, the
case described herein presented with hyperparathyroidism along with
granulomatous changes within the parathyroid adenoma, and the
patient was immunocompetent.
Inflammatory conditions of the parathyroid gland and
its hyperfunctioning are poorly defined subjects. Theories have
suggested non-infectious and autoimmune disorders as an etiological
factor for hyperparathyroidism (19). Compared to other endocrine organs,
parathyroid gland inflammatory disorders are uncommon with an
unknown pathophysiology (20,21).
Granulomatous inflammation is a histological response of body
tissue to cell damage from neoplastic conditions, infections,
drugs, toxins, allergies, and autoimmune diseases (4). The case described in the present study
was an incidental finding of parathyroid TB; the exact cause of
hyperparathyroidism was uncertain, although the condition was
suspected to be caused by infection as per the aforementioned
theory.
Hypercalcemia is defined as a blood calcium level
>10.50 mg/dl. Primary hyperparathyroidism, sarcoidosis and TB
may induce hypercalcemia (17). In
primary hyperparathyroidism, hypercalcemia occurs from osteoclast
activation due to vitamin D-mediated granulomatous diseases
(7). Parathyroid adenoma is a type
of parathyroid proliferative disease in which patients usually have
primary hyperparathyroidism and excessive blood calcium levels,
resulting in weakness, polydipsia, polyuria and nephrolithiasis.
Necrotizing granulomatous inflammation of the parathyroid with a
functional adenoma is an unusual condition (4). The case described herein complained of
generalized body aches and weakness, as well as recurrent renal
calculi.
Acid-fast staining and mycobacteria culture remain
the diagnostic tool for TB. Sputum is the most common specimen
obtained for the diagnosis of pulmonary infection with TB (22). Good conventional chest radiography is
still the major method for early diagnosis and the follow-up of
patients with pulmonary TB. Despite normal radiographs, up to 10%
of immunocompetent individuals have been observed to have TB
(23). In the case presented herein,
both the AFB test and conventional chest radiography
postoperatively were negative. Primary pulmonary TB was thus ruled
out.
The major limitations of the present study are as
follows: First, an analysis of vitamin D levels was not performed
for the patient. Second, there was a lack of a sestamibi
parathyroid scan. Third, there was no post-operative bacterial
culture for TB, vitamin D, and PTH hormone levels.
In conclusion, caseating granulomatous inflammation
of the parathyroid gland caused by TB is an extremely rare
condition. In TB-prevalent communities, TB may be considered when
patients have symptoms of hypercalcemia. To the best of our
knowledge, this is the eighth case described in the literature to
date.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author upon reasonable
request.
Authors' contributions
AMS was a major contributor to the conception of the
study, as well as to the literature search for related studies.
SHH, SOK and FHK were involved in the literature review, in the
writing of the manuscript, and in the analysis and interpretation
of the patient's data. HMD, HAS, BAA and MHA were involved in the
literature review, in the design of the study, in the revision of
the manuscript and in the processing of the figures. SHH and MHA
confirm the authenticity of all the raw data. AMA was the
pathologist examining the specimen. AJQ was the radiologist who
performed the assessment. All authors have read and approved the
final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient whose case is presented herein.
Patient consent for publication
Written informed consent was obtained from the
patient whose case is presented herein for the publication of her
data and any related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bruder JM, Gruise TA and Mundy GR: Mineral
metabolism. In: Endocrinology and Metabolism. Felig P and Frohman
LA (eds). McGraw-Hill, New York, NY, pp1079-1179, 2001.
|
|
2
|
Kamejima S, Yamamoto I, Kobayashi A,
Nakashima A, Uchiyama T, Ohkido I and Yokoo T: Hypercalcemia caused
by comorbid parathyroid adenoma and pulmonary tuberculosis. CEN
Case Rep. 10:1–5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Shah KK, Pritt BS and Alexander MP:
Histopathologic review of granulomatous inflammation. J Clin Tuberc
Other Mycobact Dis. 7:1–12. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Jacob PM, Sukumar GC, Nair A and Thomas S:
Parathyroid adenoma with necrotizing granulomatous inflammation
presenting as primary hyperparathyroidism. Endocr Pathol.
16:157–159. 2005.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Şirali SK, Tomar ÖK, Büberci R, Bal AZ and
Duranay M: Parathyroid adenoma mimicking tuberculosis in a
peritoneal dialysis patient. Acta Endocrinol (Buchar). 18:225–227.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Adams JS: Hypercalcemia due to
granuloma-forming disorders. In: Primer on the Metabolic Bone
Diseases and Disorders of Mineral Metabolism. Favus MJ (ed).
Lippincott Williams and Wilkins, Philadelphia, PA, p212, 1999.
|
|
7
|
Mayo-Yáñez M, Lage-Fernández FJ,
López-Solache L and Parente-Arias P: Parathyroid gland hyperplasia
associated with tuberculous granulomatous inflammation manifesting
as primary hyperparathyroidism. Med Mal Infect. 50:738–741.
2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kar DK, Agarwal G, Mehta B, Agarwal J,
Gupta RK, Dhole TN and Mishra SK: Tuberculous granulomatous
inflammation associated with adenoma of parathyroid gland
manifesting as primary hyperparathyroidism. Endocr Pathol.
12:355–359. 2001.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Sadideen HM, Blaker P, O'Donnell P, Taylor
J and Goldsmith DJ: Tuberculosis complicating tertiary
hyperparathyroidism in a patient with end-stage renal disease: A
case report. J Nephrol. 21:438–441. 2008.PubMed/NCBI
|
|
10
|
Seemann N: Studies on the frequency of
lymphocytic parathyroiditis. Dtsch Med Wochenschr. 92:106–108.
1967.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
11
|
Kabbaj DE and Oualim Z: Parathyroid gland
tuberculosis associated with secondary hyperparathyroidism in
hemodialysis patient. Saudi J Kidney Dis Transplant. 21:742–743.
2010.PubMed/NCBI
|
|
12
|
Anaforoglu I, Siviloglu C, Livaoglu A and
Algün E: Granulomatous infiltration of a parathyroid adenoma
presenting as primary hyperparathyroidism in a woman: A case
report. J Med Case Rep. 4(400)2010.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Singh HP, Narang V, Sood N and Puri H:
Parathyroid adenoma associated with granulomatous inflammation: A
curious cause of hypercalcaemia. J Clin Diagn Res. 10:ED21–ED22.
2016.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Aso SM, Jaafar Omer A, Hiwa OB, Ismael YA,
Hemn Ali H, Kayhan AN, Tomas MM, Mohammed QM, Diyar Adnan M, Rawa
B, et al: Kscien's List; A New Strategy to Discourage Predatory
Journals and Publishers (Second Version). Barw Medical Journal.
1:1–3. 2023.
|
|
15
|
World Health Organization. (n.d.). Global
tuberculosis report 2019.
|
|
16
|
Yang Z, Kong Y, Wilson F, Foxman B, Fowler
AH, Marrs CF, Cave MD and Bates JH: Identification of risk factors
for extrapulmonary tuberculosis. Clin Infect Dis. 38:199–205.
2004.PubMed/NCBI View
Article : Google Scholar
|
|
17
|
Tahbildar D, Maitra T and Goswami D:
Hypercalcaemia-A Rare Manifestation of Tuberculosis-A Case Report.
J Evol Med Dent Sci. 29:590–592. 2022.
|
|
18
|
Wieneke JA and Smith A: Parathyroid
adenoma. Head Neck Pathol. 2:305–308. 2008.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Reiner L, Klayman MJ and Cohen RB:
Lymphocytic infiltration of the parathyroid glands. Jew Mem Hosp
Bull. 6-7:103–118. 1962.PubMed/NCBI
|
|
20
|
Talat N, Diaz-Cano S and Schulte KM:
Inflammatory diseases of the parathyroid gland. Histopathology.
59:897–908. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Haglund F, Hallström BM, Nilsson IL, Höög
A, Juhlin CC and Larsson C: Inflammatory infiltrates in parathyroid
tumors. Eur J Endocrinol. 177:445–453. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Caulfield AJ and Wengenack NL: Diagnosis
of active tuberculosis disease: From microscopy to molecular
techniques. J Clin Tuberc Other Mycobact Dis. 4:33–43.
2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Al Shahed M, Abd El Bagi M and Madkour MM:
Radiology of pulmonary tuberculosis. In: Tuberculosis. Springer,
Berlin, Heidelberg, pp359-384, 2004.
|