Introduction
Tracheal stenosis is a rare condition that involves
the narrowing of the tracheal lumen, causing significant
respiratory distress and potentially life-threatening complications
(1). It can occur due to a variety
of factors, such as congenital abnormalities, acquired conditions,
or traumatic injuries with a reported incidence of 1 in 6,400 live
births for congenital type, with a mortality rate as high as 79%
before the advent of current surgical techniques (2). While tracheal stenosis is more commonly
observed in adults, its occurrence in pediatric populations is less
frequent. The diagnosis and treatment of tracheal stenosis in
children pose unique challenges that require a comprehensive
understanding of the condition and its management strategies
(3). The present study describes the
clinical course of a 2-year-old female child diagnosed with
tracheal stenosis. The present study aimed to provide valuable
insight into the diagnostic and therapeutic complexities
encountered during the treatment of this condition.
Case report
Patient information
A 2-year-old female child, who had previously
undergone a tracheostomy and polypectomy at another medical center,
was referred to the Smart Health Tower, Sulaimani, Iraq due to
progressively worsening stridor and shortness of breath. The
symptoms gradually increased in intensity, eventually reaching a
severe level, where the child experienced episodes of
suffocation.
Clinical findings
Due to the urgency of the case, no physical
examination had been conducted at the previous center. An emergency
tracheostomy was thus immediately performed, which provided
temporary relief. Later, due to the persistent nature of the
condition, the case was referred to the Cardiothoracic Department
at Smart Health Tower (Sulaimani, Iraq).
Diagnostic assessment
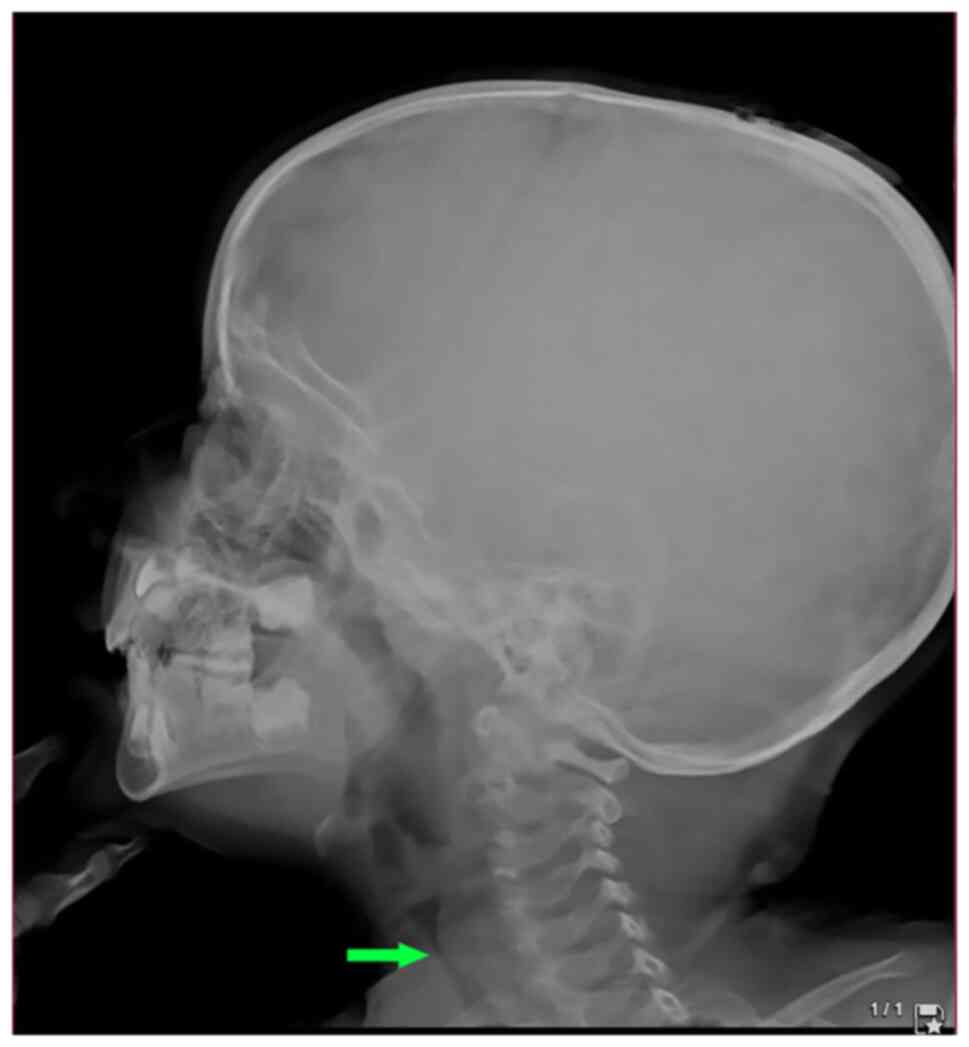
A lateral post-nasal space X-ray was performed,
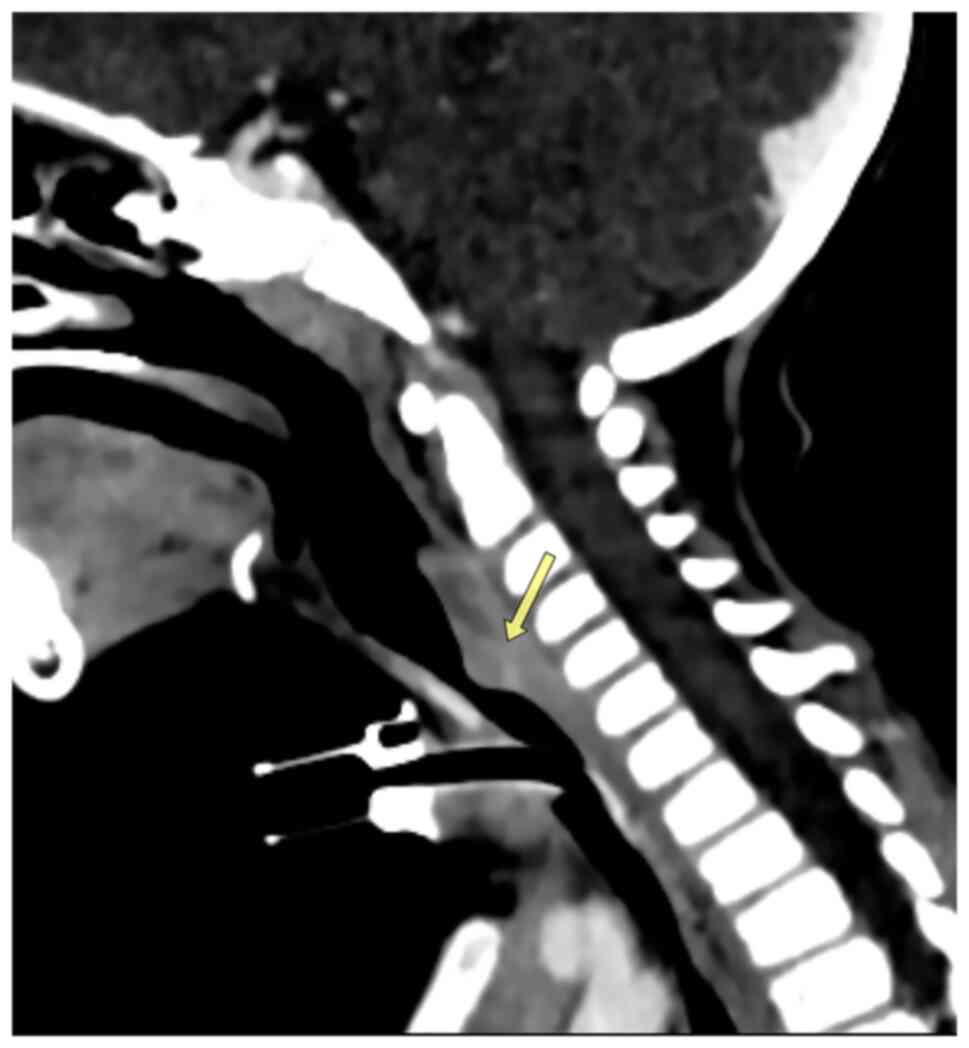
which illustrated tracheal stenosis (Fig. 1). A computed tomography (CT) scan was
conducted and confirmed severe subglottic stenosis and a narrowing
of the tracheal region just below the vocal cords (Fig. 2).
Therapeutic intervention
The patient had previously undergone a rigid
laryngoscopy to remove a vocal cord polyp at another medical
center. However, the intervention did not yield the desired
clinical benefit, and the child's symptoms persisted. Under general
anesthesia, a rigid bronchoscopy procedure was performed. The
bronchoscope was inserted through the mouth and into the trachea.
The narrowed section of the trachea, proximal to the stenosis, was
identified and forcefully dilated using a combination of scopes and
dilators of various sizes. A biopsy sample was collected from the
hypertrophied bronchial wall, and the pathological analysis
confirmed benign hypertrophic tissue. Following 1 week of
tracheostomy weaning, during which the child gradually transitioned
to breathing independently without the aid of the tracheostomy
tube, a new symptom emerged. The child developed stridor,
particularly noticeable during sleep. Concerned about the
recurrence of respiratory distress, a subsequent rigid bronchoscopy
was performed, and the trachea appeared normal. However, some
features suggestive of tracheomalacia were identified. The
condition was confirmed to be congenital due to the presence of
tracheomalacia. Following decannulation, the patient was
hospitalized for 3 days to monitor for any emerging dyspnea. An
echocardiography was performed to rule out any associated
cardiovascular abnormalities, and this revealed no significant
findings (data not shown). The child was prescribed a treatment
regimen consisting of steroids and antibiotics. Notably, the
patient responded favorably to the medical intervention, with a
significant improvement in symptoms.
Follow-up
During a 1-year follow-up period, the child remained
asymptomatic, indicating successful management of tracheal stenosis
caused by tracheomalacia.
Discussion
Tracheal stenosis, medical condition whose incidence
among infants is rare, is characterized by the narrowing of the
trachea, leading to respiratory distress and potential
complications (4). It is crucial for
medical professionals to have a thorough understanding of this
condition and its associated complications in order to ensure
appropriate treatment and care for affected infants.
Common symptoms of tracheal stenosis include
shortness of breath and stridor, a high-pitched sound during
breathing. In severe cases, respiratory failure and asphyxiation
can occur, underscoring the need for early diagnosis and
appropriate management (4).
The incidence of tracheal stenosis is estimated to
be 1 in 6,400 live births, emphasizing its rarity and the need for
heightened awareness (2). To
diagnose tracheal stenosis, a comprehensive evaluation is required,
incorporating imaging techniques such as CT scans and
bronchoscopies, alongside a meticulous medical history and physical
examination (5). The key
differential diagnosis is foreign body aspiration (6).
The treatment of tracheal stenosis is dependent on
the severity and underlying cause of the condition. Several
treatment options are available to alleviate symptoms and improve
airway function:
Airway dilation involves the insertion of a balloon
through a bronchoscope into the narrowed area of the trachea. The
balloon is then inflated to expand the airway and enhance airflow
(7). Balloon dilation has been
proven to be a secure and efficient palliative technique for
addressing both congenital and acquired tracheal and bronchial
stenosis. Notable enhancements in symptoms and the widening of the
airway can be observed, although these improvements may only be
temporary. In order to achieve a lasting remedy, a series of
sequential dilation procedures may be required (7).
In certain cases, a stent may be positioned within
the trachea to maintain its patency. This can be achieved using a
bronchoscope or through an open surgical procedure (8). According to previous research, >90%
of patients achieve the rapid alleviation of dyspnea rather than
the complete resolution of tracheal stenosis. To assess the
efficacy of silicone stent placement, various factors are
considered, including the Borg scale, lung function, CT
measurements of stenosis, curative rates (successful stent removal)
and stability rates (8).
Laser therapy is utilized to remove excess or scar
tissue causing tracheal narrowing. It is typically performed with
the assistance of a bronchoscope (9). Neodymium:Yttrium-Aluminium-Garnet
(Nd:YAG) laser photocoagulation has demonstrated effectiveness in
managing tracheal stenosis caused by benign lesions, with the
exception of subglottic region involvement. The procedure is
associated with minimal morbidity and no mortality risks (10). Severe cases of tracheal stenosis may
necessitate surgical intervention to remove the narrowed portion of
the trachea and reconstruct the airway. Various techniques, such as
tracheal resection and anastomosis or tracheal reconstruction with
grafts, may be employed (11). The
most effective treatment for benign tracheal stenosis is surgery,
specifically tracheal resection, and end-to-end anastomosis. A
previous study demonstrated a success rate of 88% for surgery in
addressing airway stenosis, with an almost zero complication rate
(12). However, only a small
percentage of patients (<10%) with tracheal stenosis are
suitable candidates for surgery and resection due to the
significant risks associated with anesthesia and surgery, as well
as the length of the tracheal resection and the extent of the
lesion (13). In the case in the
present study, the condition was initially suspected to be caused
by a polyp on the vocal cord; thus, the patient, at another center,
underwent an emergency tracheostomy and polypectomy. The condition
was temporarily relieved but later emerged again; thus, the case
was then referred to the authors. After conducting a bronchoscopy,
the case was diagnosed as tracheomalacia. Proper workups such as
echocardiography were subsequently performed to exclude any
associated cardiovascular abnormalities.
In certain instances, medications such as
corticosteroids may be prescribed to mitigate inflammation and
alleviate symptoms. However, medical management alone is generally
not a long-term solution and is often used in conjunction with
other treatments (14). By
implementing these treatment options, medical professionals aim to
relieve symptoms, restore proper airway function and enhance the
quality of life of individuals with tracheal stenosis. The case
described herein was prescribed a treatment regimen consisting of
steroids and antibiotics, as mitomycin was not available at that
time, and the patient responded favorably to the medical
intervention. The limitation of the present study was that the
authors were not able to retrieve any data or information regarding
how the tracheostomy procedure was conducted or which protective
method was applied, as it was performed at another center. In the
present study, all the references have been filtered to avoid
citing non-peer-reviewed data (15).
In conclusion, tracheal stenosis is a rare condition
that poses significant challenges to affected infants. The
diagnosis involves a comprehensive evaluation, considering imaging
techniques and careful assessment of medical history. Various
treatment modalities, including airway dilation, stent placement,
laser therapy, surgery and medical management may be employed to
alleviate symptoms and improve outcomes. Continued research and
collaboration among healthcare professionals are essential to
further enhance our understanding of this condition and optimize
treatment strategies.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and material
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
FHK was a main contributor to the conception of the
study, as well as in the literature search for related studies.
SOK, BAA and MLF were involved in the literature review, in the
writing of the manuscript, and in the analysis and interpretation
of the patient's data. RJR, KMH, SSA, HOK, STSA, KHHK and BAM were
involved in the literature review, in the design of the study, as
well as in the revision of the manuscript and in the processing of
the figures. FHK and SSA confirm the authenticity of all the raw
data. All authors have read and approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
parents of the patient.
Patient consent for publication
Written informed consent was obtained from the
parents of the patient to publish any related data and any related
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Laing MR, Albert DM, Quinney RE and Bailey
CM: Tracheal stenosis in infants and young children. J Laryngol
Otol. 104:229–235. 1990.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Herrera P, Caldarone C, Forte V, Campisi
P, Holtby H, Chait P, Chiu P, Cox P, Yoo SJ, Manson D and Kim PCW:
The current state of congenital tracheal stenosis. Pediatr Surg
Int. 23:1033–1044. 2007.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Klopper GJ, Adeniyi OV and Stephenson K:
Adolescent and adult laryngotracheal stenosis: A review. Egypt J
Otolaryngol. 37(36)2021.
|
|
4
|
Catano J, Uzunhan Y, Paule R, Dion J,
Régent A, Legendre P, Gonin F, Martinod E, Cohen P, Puéchal X, et
al: Presentation, diagnosis, and management of subglottic and
tracheal stenosis during systemic inflammatory diseases. Chest.
161:257–265. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Muthialu N, Ramaswamy M, Beeman A and Yeh
YT: Management of tracheal diseases in children. Front Pediatr.
8(297)2020.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Baram A, Sherzad H, Saeed S, Kakamad FH
and Hamawandi AMH: Tracheobronchial foreign bodies in children: The
role of emergency rigid bronchoscopy. Glob Pediatr Health. 4:1–6.
2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Freitag L, Ernst A, Unger M, Kovitz K and
Marquette CH: A proposed classification system of central airway
stenosis. Eur Respir J. 30:7–12. 2007.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Walser EM: Stent placement for
tracheobronchial disease. Eur J Radiol. 55:321–330. 2005.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Deshmukh A, Jadhav S, Wadgoankar V,
Takalkar U, Deshmukh H, Apsingkar P, Sonwatikar P and Antony P:
Airway management and bronchoscopic treatment of subglottic and
tracheal stenosis using holmium laser with balloon dilatation.
Indian J Otolaryngol Head Neck Surg. 71:453–458. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Rau BK, Harikrishnan KM and Krishna S:
Neodymium: YAG laser in the management of tracheal stenosis. Ann
Acad Med Singap. 23:333–334. 1994.PubMed/NCBI
|
|
11
|
Wen W, Du X, Zhu L, Wang S, Xu Z and Lu Z:
Surgical management of long-segment congenital tracheal stenosis
with tracheobronchial malacia. Eur J Cardiothorac Surg.
61:1001–1010. 2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Lorenz RR: The evolution and outcomes of
the ‘Maddern Procedure’ for the treatment of subglottic stenosis.
Laryngoscope: May 17, 2023 (Epub ahead of print).
|
|
13
|
Nouraei SM, Middleton SE, Nouraei SA, Virk
JS, George PJ, Hayward M and Sandhu GS: Management and prognosis of
primary tracheal cancer: A national analysis. Laryngoscope.
124:145–150. 2014.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Shadmehr MB, Abbasidezfouli A, Farzanegan
R, Pejhan S, Kakhaki AD, Sheikhy K, Saghebi SR, Sadeghbeigee F,
Gharedaghi A, Jahanshahi N and Zangi M: The role of systemic
steroids in postintubation tracheal stenosis: A randomized clinical
trial. Ann Thorac Surg. 103:246–253. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Muhialdeen AS, Ahmed JO, Baba HO, Abdullah
IY, Hassan HA, Najar KA, Mikael TM, Mustafa MQ, Mohammed DA, Omer
DA, et al: Kscien's List; A new strategy to discourage predatory
journals and publishers (Second Version). Barw Medical J. 1:1–3.
2023.
|