Introduction
The term fibroid was first introduced into everyday
clinical practice in the 1860s. Fibroids or leiomyomas are benign
neoplasms that grow on the uterine wall in women of reproductive
age and are currently the most common gynecological tumors
worldwide (1). Depending on their
development in the myometrium and their location relative to the
uterine cavity, leiomyomas can be divided into submucosal,
intramural and subserosal (2). Among
the above, three main types are leiomyomas located outside the
uterus corpus, such as the cervix (cervical leiomyomas) and the
broad ligament (intraligamental leiomyomas) (3).
Intraligamental leiomyomas are pedunculated tumors,
which originate from the lateral wall of the uterus corpus and grow
within the broad ligaments. Intraligamental leiomyomas are rare.
They are estimated to account for 6 to 10% of all uterine fibroids
(4). Huge intraligamental leiomyomas
(>10 cm) are even rarer. Extremely rare are the huge
intraligamental leiomyomas (>20 cm). It is estimated that to
date, five cases of huge intraligamental leiomyomas have been
reported in the English literature, of which the maximum diameter
was >20 cm and the weight was >3 kg (5-8).
The present study describes the case of patient who
was subjected to surgical treatment for a huge intraligamental
leiomyoma of the uterus. It is pointed out that, despite the rarity
of the nosological entity concerning tumors >3 kg and the
serious difficulties in differential diagnosis it presents from
other intra-abdominal tumors, the adequate pre-operative
preparation of the patient is considered necessary in order to
ensure the optimal intraoperative and post-operative outcomes. At
the same time, the significant surgical challenges and potential
intraoperative complications that may arise in the treatment of
huge intraligamental leiomyomas of uterus are highlighted.
Case report
The present study describes the case of a
48-year-old patient, who visited the Gynecological Outpatient
Clinic of the General Hospital of Trikala (Trikala, Greece) for an
examination. The patient presented an abdominal ultrasound, which
was performed upon the recommendation of the general practitioner.
To the family physician, the patient complained of abdominal
distension with atypical abdominal pain, dyspepsia and anorexia.
Ultrasound imaging revealed the presence of a space-occupying
lesion of mixed echogenicity and an enormous size, which occupied
most of the peritoneal cavity and was most likely originating from
the right ovary. Furthermore, after obtaining a comprehensive
medical history, it was revealed that the aforementioned symptoms
first appeared ~20 months ago, during which time the patient had
not requested medical care until she visited her family physician.
In addition, from her personal medical history, hypothyroidism was
reported, although it was well regulated with medication. Her
menstrual cycle was normal. The patient had given birth to a child
by vaginal delivery 15 years prior.
Upon a physical examination, the abdomen was found
to be bloated and rigid, with no signs of peritoneal irritation.
The upper margins of the tumor were palpable at approximately the
level of the xiphoid process. A Visual inspection of the cervix was
difficult due to its displacement by the intra-abdominal mass. The
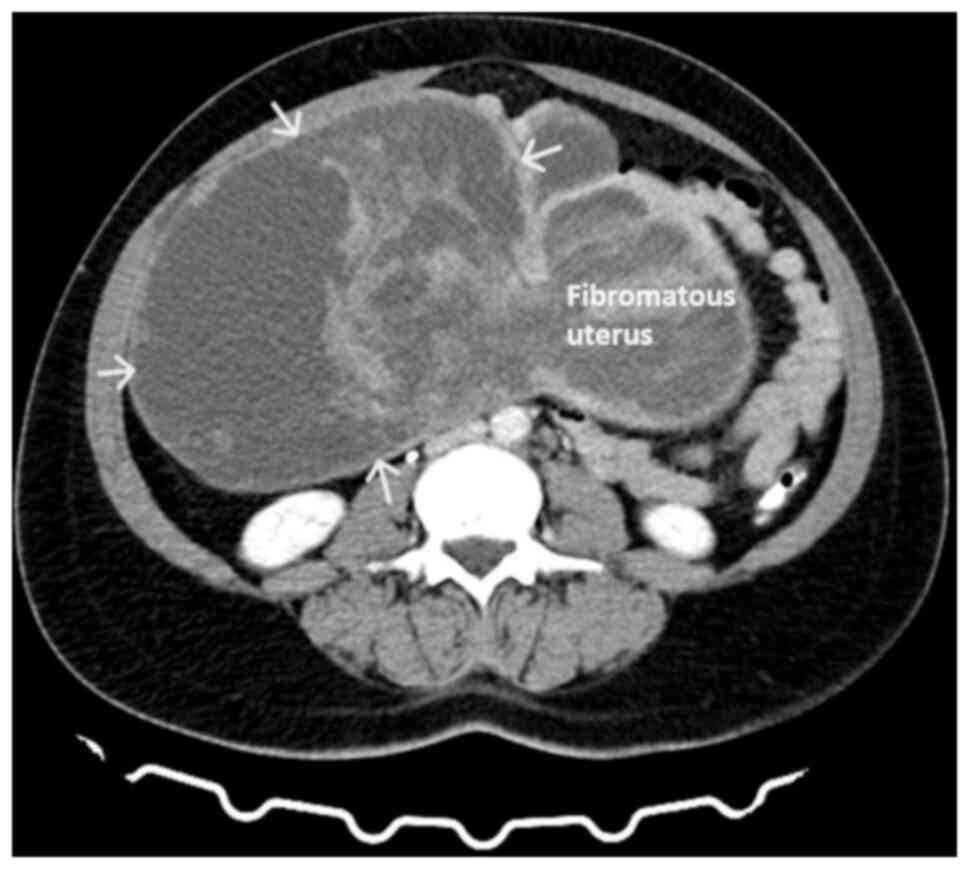
transvaginal ultrasound was not diagnostic. A computed tomography
scan revealed the presence of a large mass (28.5x23x11 cm), with
well-defined margins, which occupied most of the peritoneal cavity
and probably of adnexal origin. The intra-abdominal mass had a
multilobulated shape and was of mixed consistency, with marked
post-contrast enhancement of solid elements (Fig. 1). The findings from magnetic
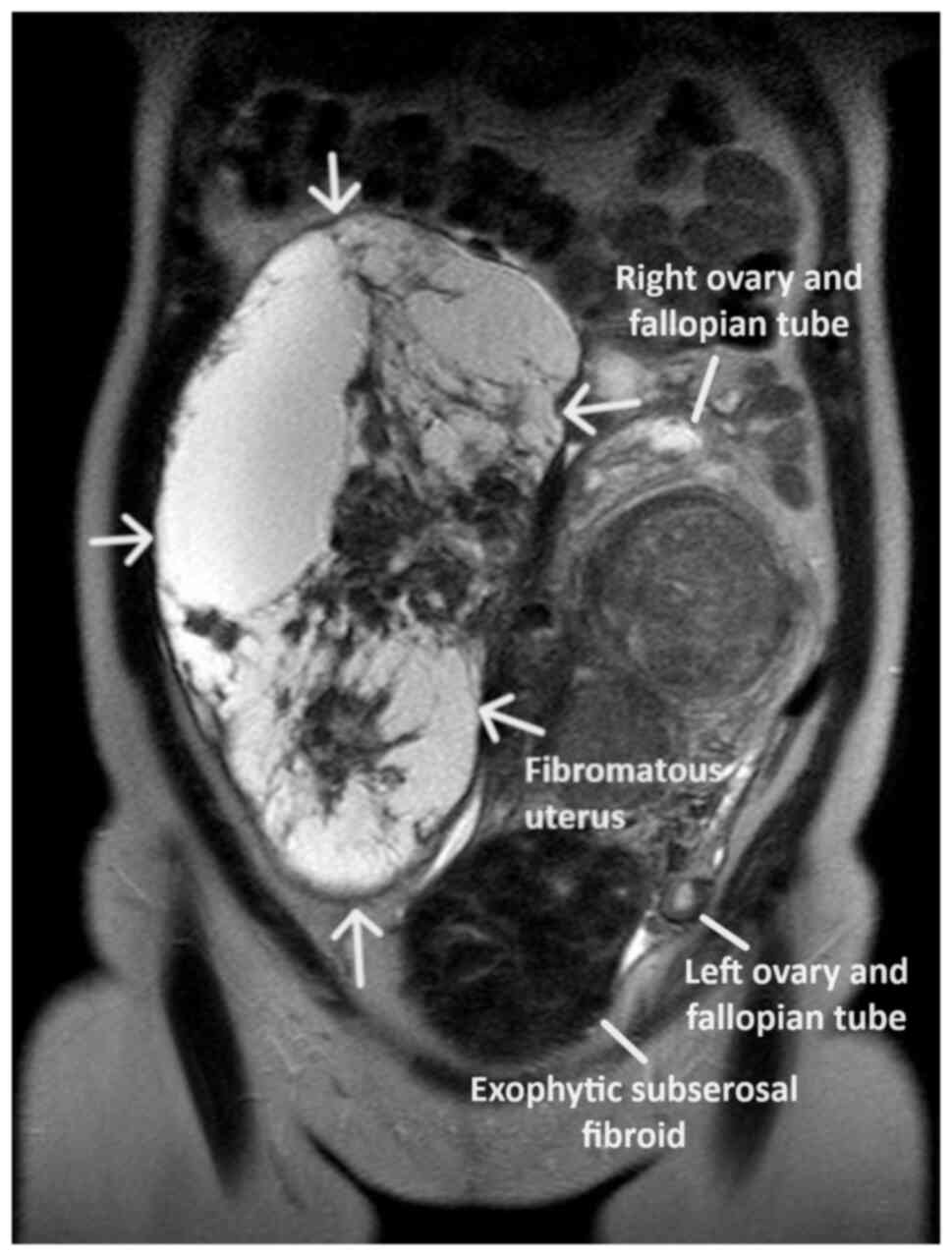
resonance imaging were similar. Magnetic resonance imaging revealed
a large heterogeneous lesion measuring ~26x13 cm, which originated
from the internal genital organs. As a consequence of the large
size, the lesion exited from the lesser pelvis and extended
superiorly, completely occupying the peritoneal cavity of the
mid-abdomen up to approximately the middle of the right kidney,
with a maximum cephalocaudal length of 27.5 cm. The lesion was
depicted with lobulated indistinct borders and had extensive
nodular solid and cystic necrotic elements, nodular wall
protrusions and multiple internal septations, presenting
inhomogeneous enhancement in the paramagnetic substance (Fig. 2). The present imaging depicted a part
of the uterus, which appeared to be encapsulated and indistinct
within the lesion, with the presence of multiple solid
inhomogeneous formations mimicking fibroids. The left ovary was
displaced in the left iliac fossa with the presence of small
follicles. The right ovary was not visualized. From the laboratory
analysis, the following results were obtained: Hematocrit, 29.8%;
hemoglobin, 9.1 g/dl; white blood cell count, 9.820/ml;
neutrophils, 63.2%; platelets, 271x103/ml; international normalized
ratio, 0.99; fibrinogen, 278 mg/dl; urea, 34 mg/dl; creatinine,
0.71 mg/dl. The cervical smear test was negative for malignancy.
The levels of tumor markers [carcinoembryonic antigen, cancer
antigen (Ca)125, Ca15-3 and Ca19-9] were within normal range.
Following a thorough consultation of the patient, it
was decided to perform an exploratory laparotomy, with the possible
necessity of performing a total abdominal hysterectomy.
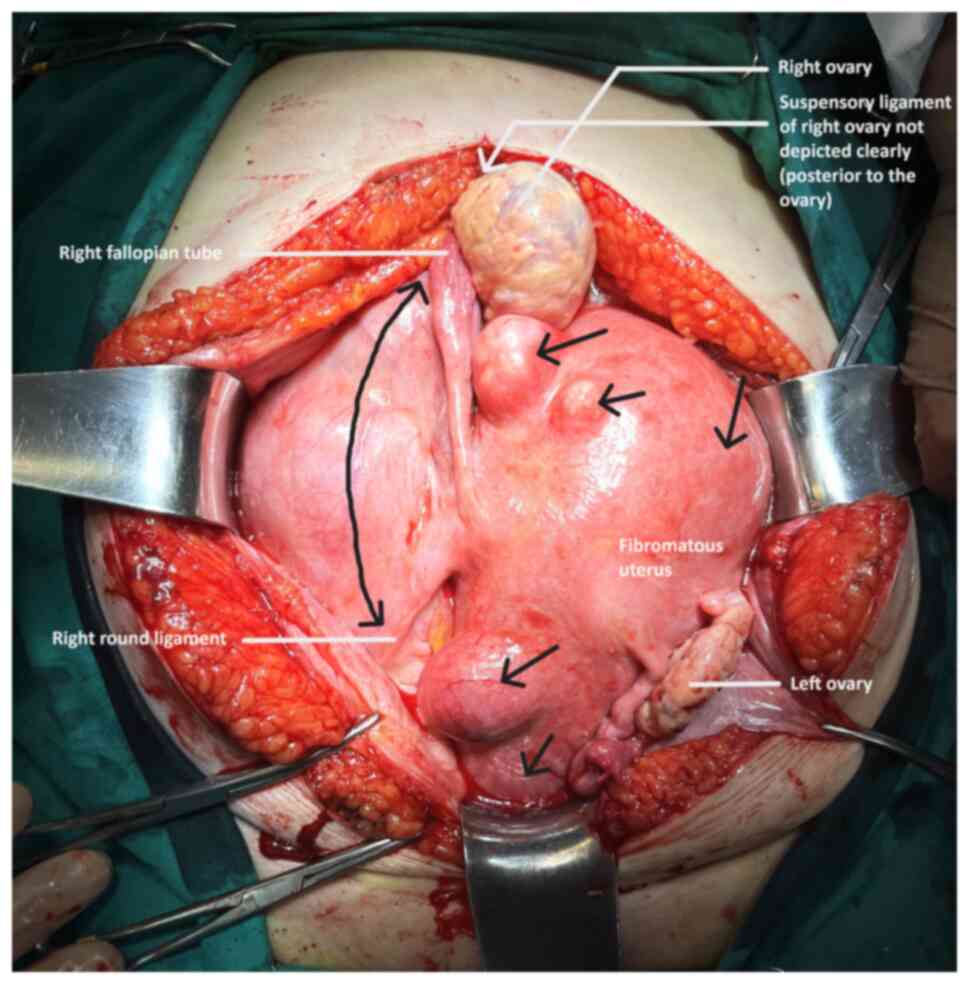
Pre-operatively, ureteral stents were placed. Intraoperatively, a
large subserosal pedunculated leiomyoma was found emerging from the
right lateral wall of the uterus with retroperitoneal extension
within the leaves of the broad ligament. The ovaries were
displaced. The presence of other smaller uterine fibroids was
evident (Fig. 3). Using an
electrothermal bipolar vessel sealing device (LigaSure™), a
dissection of the anterior leaf of the broad ligament was
performed, from the upper third of the round ligament to the
suspensory ligament (both ligaments had been previously ligated
with a suture). Subsequently, with the use of the electrothermal
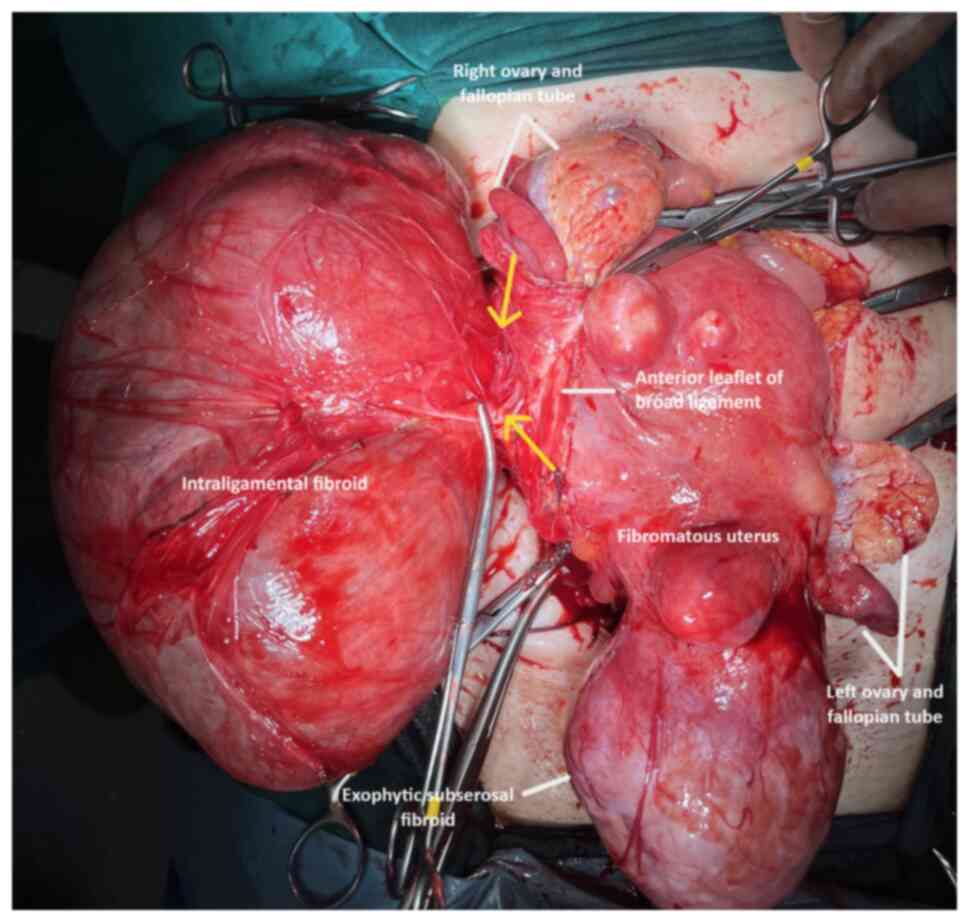
bipolar vessel sealing device and using suture ligation where
necessary, the fibroid (weighing 3,370 g) was dissected from the
leaves of the broad ligament and resected following the ligation
and dissection of the vascular pedicle in the lateral right wall of
uterus (Fig. 4). Surgical steps were
carefully performed to avoid injury to the ureters, bladder and the
large vessels, and their branches that pass through the anatomical
area. The surgery was completed with the resection of the uterus
and adnexa. Transfusion with two units of whole blood was deemed
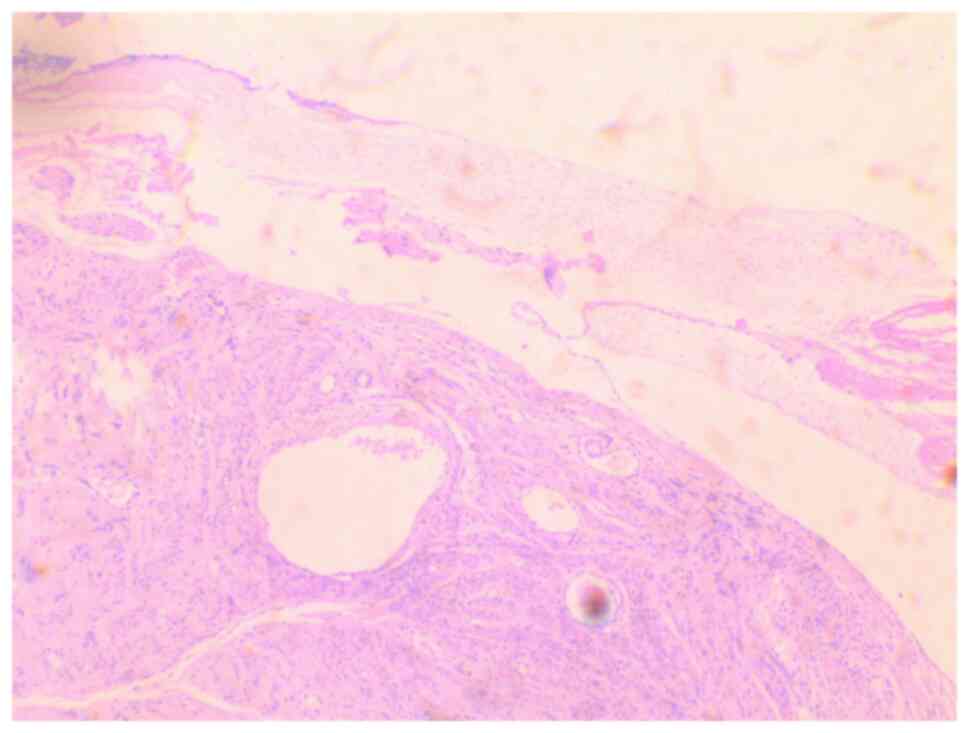
necessary. A histological examination of the surgical specimen
confirmed the diagnosis of intraligamental leiomyoma of the uterus.
A microscopic examination of the tumor revealed cystic and hydropic
degeneration with a low mitotic index (0 to 2 mitoses) and
thick-wall blood vessels within the stroma. No necrosis or severe
cellular atypia was observed (Fig.
5). The staining was performed by the Anatomic Pathology
Laboratory of the General Hospital of Trikala. The thickness of the
sections used was 5 µm, and the tissue sections were
paraffin-embedded. The fixative used was buffered formalin 10%, at
room temperature, for 36 h. The stain used was hematoxylin-eosin
0.5% alcohol (DIACEL), at room temperature and for a duration of 12
min. A LEICA DM2000 optical microscope was used. The thickness of
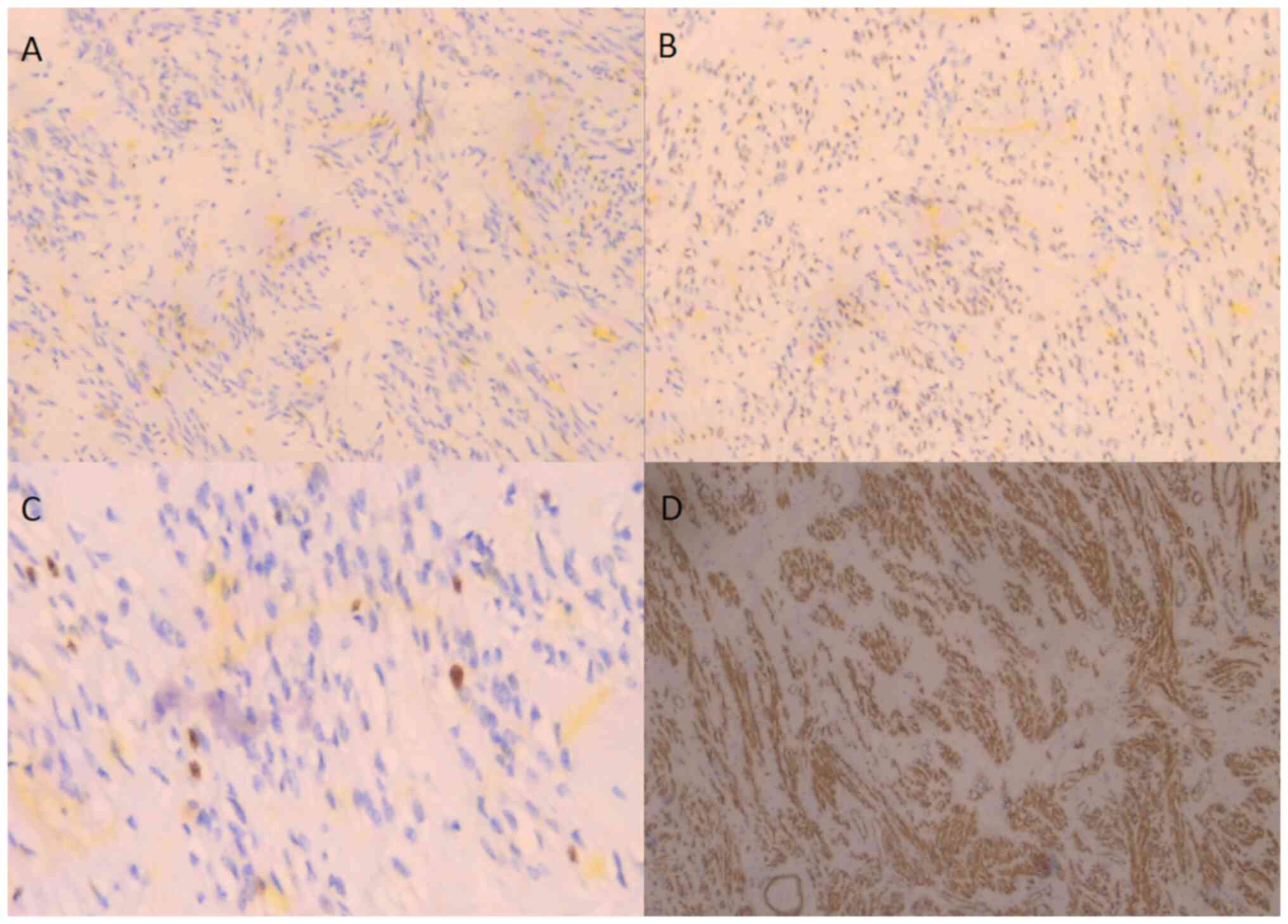
the sections used in the immunohistochemical analysis was 4 µm, the
sections were paraffin-embedded and dewaxed for 40 min at 75˚C.
Immunohistochemistry was then performed with an automated
BOND-LEICA system (Leica Biosystems), using the following protocol:
i) Dewaxing with BOND™ Dewax solution,100% alcohol,
BOND™ wash solution; ii) antigen retrieval: for CD10,
BOND™ Epitope Retrieval ER2 Solution, HIER, was used for
20 min at 100˚C, while for smooth muscle actin (SMA), estrogen
receptor (ER) and Ki67 antibodies used ER1 solution (pH 7) for 20
min; iii) the block peroxide kit (BOND) was used for 5 min; iv)
only for CD10 antibody: Protein block solution was used for 20 min;
v) primary antibody: dilution for CD10 (MENARINI) ready-to-use
antibody (cat. no. 44 217 CD10 RTU), SMA (ZYTOMED) ready-to-use
(cat. no. 1A4 A00002-IFU-IVD-0002), ER (DAKO) 1:40 (cat. no.
M3643), Ki67 (Skytec) 1:150 for duration 30 min (MIB1
A00095-IFU-IVD, cat. no. CBB500), and post primary kit for duration
10 min at an incubation temperature of 100˚C; vi) secondary
detection kit polymer for duration 10 min (no secondary antibodies
were used herein); vii) DAB kit for duration 10 min, visualization;
viii) counterstain: hematoxylin kit for duration 5 min at room
temperature; ix) dehydration, mount section. The study of the
slides was carried out using an optical microscope (LEICA DM2000;
magnification, x40, x400 and x100). The following results were
obtained: Ki67, 7%; SMA (+), weakly positive for ER, and negative
for CD10 (Fig. 6). These findings
excluded the diagnosis of fibrosarcoma.
Following a smooth post-operative course, the
patient was discharged from the clinic on the fifth post-operative
day. Upon the recommendation of urologists, the ureteral stents
were removed 1 month after surgery. Upon a re-examination of the
patient at the Gynecological Outpatient Clinic of the General
Hospital of Trikala at 10 days and 3 months post-operatively, the
patient was in excellent clinical condition and reported complete
relief from the symptoms of abdominal distension with atypical
abdominal pain, dyspepsia and anorexia. The results of blood tests
were within normal ranges. A consultation for a re-examination at
the Gynecological Outpatient Clinic of the General Hospital of
Trikala at 6 months after surgery was made.
Discussion
The diagnosis of intraligamental fibroids of uterus
based on clinical manifestations is extremely difficult. In the
majority of cases, intraligamental fibroids, even those that are
large, are asymptomatic (4). Less
commonly, they may manifest with more obvious symptoms, which are
due to compression on the adjacent organs. Abdominal distension,
frequent urination, constipation, anorexia, weight loss and pain in
the ipsilateral to the tumor renal area are the main clinical
manifestations that characterize huge intraligamental fibroids
(5). In some cases, the pain may be
acute and severe (9). Not
unexpectedly, the patient described herein did not complain of any
symptoms related to rectal or bladder compression from the huge
intraligamental tumor. Abdominal distension, atypical abdominal
pain and dyspepsia were the main symptoms in the patient in the
present study. Possibly surprisingly, no hydronephrosis, due to
right ureteric compression from the huge intraligamental fibroid,
which is usually associated with large pelvic tumors, was observed
(10).
Similarly, the pre-operative imaging diagnosis of
intraligamental fibroids is difficult. Recently, there has been an
attempt to evaluate magnetic resonance imaging findings in order to
differentiate intaligamental fibroids from subserosal fibroids.
Yajima et al (11)
demonstrated that tumor shape, the attachment of the tumor to the
uterus, ovary elevation on the side of the tumor and the separation
of the round ligament from the ipsilateral uterine artery may be
criteria for the differential diagnosis of intraligamental fibroids
from subserosal fibroids. In the patient in the present study,
neither computed tomography nor magnetic resonance imaging were
able to establish the pre-operative diagnosis of intraligamental
leiomyoma of the uterus. The effort made by the radiologists of the
authors' hospital to differentiate subserosal fibroid from adnexal
mass or intraligamental leiomyoma was not successful. The presence
of a pedicle in the lateral wall of the uterus and the separation
of the round ligament from the uterine artery proximal to the tumor
were not imaged or not adequately assessed by the team of
radiologists. In addition, the non-imaging of the right ovary was
incorrectly not attributed to its elevation due to the displacement
of the suspensory ligament by the presence of the huge
intraligamental leiomyoma. Based on the experience from the
management of patients with large intraligamental leiomyomas, it is
considered that the determination and awareness of specific imaging
features of these tumors may assist in the accurate preoperative
diagnosis, which allows for the planning of the optimal surgical
treatment and the avoidance of severe intraoperative and/or
post-operative complications (12).
The diagnosis of intraligamental leiomyomas of the
uterus in almost all cases, as in the patient described herein, is
determined intraoperatively. Hysterectomy or myomectomy, depending
on the age of the patient and the patient's desire to preserve
fertility, is the main treatment option. The surgical treatment of
intraligamental uterine leiomyomas is challenging. The
understanding of the tumor characteristics (location, shape and
size) and the proper pre-operative, intraoperative and
post-operative management of these patients is critical for an
optimal surgical outcome and for the prevention of potential
intraoperative complications. Intraoperative hemorrhage is a common
complication, which may be more prevalent during laparoscopic
myomectomy, compared to myomectomy by laparotomy (4,5).
Recently, however, in 2022, Wang et al (13) demonstrated that performing
laparoscopic resection of a large intraligamental leiomyoma by
combining two novel laparoscopic ligation techniques could be a
safe and effective surgical treatment option, greatly reducing the
risk of intraoperative hemorrhage and avoiding unintentional injury
to adjacent organs, such as the bladder, rectum or ureters. In
addition, the ureters can be protected from possible intraoperative
damage by the pre-operative placement of ureteral stents (14).
Additionally, the scientific competence and skills
of the surgical team that will be called to treat patients with
large intraligamental fibroids are among the necessary requirements
for the safe and successful outcome of myomectomy or hysterectomy
with larapotomy or laparoscopy (5).
In the patient in the present study, who did not wish to preserve
fertility, abdominal total hysterectomy with bilateral adnexectomy
was selected as the treatment of choice. Intraoperatively, the
presence of a huge intraligamental leiomyoma was found, originating
from the right lateral wall of the uterus with an extension in the
broad ligament. The presence of multiple, various sized, subserosal
and intramural uterine leiomyomas was also evident (Fig. 3, black arrows). It was decided to
dissect and ligate the round ligament and the suspensory ligament,
after the patient consented pre-operatively not to preserve the
ovaries. In the case of myomectomy and in all cases of desire for
ovarian preservation, the ligation of the suspensory ligament is
not indicated. Subsequently, herein, the anterior leaf of the broad
ligament was dissected with the aid of the electrothermal bipolar
vessel sealing device, from the level of the upper third of the
round ligament to the point of the attachment of the suspensory
ligament with the ipsilateral ovary (Fig. 3, black line with double arrow),
allowing access to the retroperitoneal space. The aid of the
electrothermal bipolar vessel sealing device was critical in the
dissection of the leiomyoma from the leaves of the broad ligament,
to which it was attached with multiple, differently sized, feeding
vessels. It is considered that the use of an electrothermal bipolar
vessel sealing device greatly contributed to the control of
intraoperative bleeding. The transfusion of two units of whole
blood, which was deemed necessary for hemodynamic stabilization of
the patient post-operatively, was the outcome of the low
pre-operative hemoglobin. Careful dissection of the posterior leaf
of the broad ligament from the leiomyoma and gentle surgical
handling of the ureter was necessary in order to preserve adequate
blood supply and avoid possible injury. Subsequently, following the
ligation and dissection of the vascular pedicle of the leiomyoma
from the right lateral wall of the uterus (Fig. 4, yellow arrows) and its resection
from the surgical field, a total hysterectomy with bilateral
adnexectomy was performed.
In conclusion, huge intraligamental fibroids of the
uterus (>3,000 g) are extremely rare. A pre-operative diagnosis
is difficult. Surgical treatment (myomectomy or hysterectomy) is
challenging and requires well-organized medical centers and an
experienced surgical team. The supplementary ligation of the
suspensory ligament, in combination with the established ligation
of the round ligament as a typical procedure for access to the
retroperitoneal space, is estimated to further facilitate the
resection of intraligamental fibroid and can greatly contribute to
an optimal surgical outcome. However, it requires the resection of
the ipsilateral ovary and for this reason, it should be avoided in
patients who wish to preserve fertility and achieve future
pregnancy. Finally, the present study highlights that the use of an
electrothermal bipolar vessel sealing device appears to greatly
contribute to reducing the risk of intraoperative blood loss.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
All authors (AT, ET, EK, VG, EX, AZ, EEG, IRA, IP
and IT) participated in the preparation of the manuscript and in
the final approval of the manuscript. AT, ET, EX and AZ
participated in the conception and design of the study, in the
international literature search and in the writing of the
manuscript. EK, VG, EEG and IRA were involved in the conception and
design of the study, in the provision of study materials (such as
blood tests, culture test, imaging) or patient data, in data
collection and aggregation, and data analysis and interpretation.
IP was involved in the provision of study materials (such as blood
tests, culture test, imaging) or patient data, patient care, data
collection and aggregation, and data analysis and interpretation.
IT was involved in the conception and design of the study, in
administrative support, in the provision of study materials (such
as blood tests, culture test, imaging) or patient data, in patient
care, in data collection and analysis, as well as in the writing of
the manuscript. EK, IP and IT confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki. Written informed consent
was obtained from the patient.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of her data and any related images in
the present case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yang Q, Ciebiera M, Bariani MV, Ali M,
Elkafas H, Boyer TG and Al-Hendy A: Comprehensive review of uterine
fibroids: Developmental origin, pathogenesis, and treatment. Endocr
Rev. 43:678–719. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Zepiridis LI, Grimbizis GF and Tarlatzis
BC: Infertility and uterine fibroids. Best Pract Res Clin Obstet
Gynaecol. 34:66–73. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Gomez E, Nguyen MT, Fursevich D, Macura K
and Gupta A: MRI-based pictorial review of the FIGO classification
system for uterine fibroids. Abdom Radiol (NY). 46:2146–2155.
2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Huang PS, Sheu BC, Huang SC and Chang WC:
Intraligamental myomectomy strategy using laparoscopy. J Minim
Invasive Gynecol. 23:954–961. 2016.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Lee CY and Chen CH: Huge intraligamental
leiomyoma: Two cases and review of the literature. Asian J Surg.
44:1622–1624. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Funaki K, Fukunishi H, Tsuji Y, Maeda T
and Takahashi T: Giant cystic leiomyoma of the uterus occupying the
retroperitoneal space. J Radiol Case Rep. 7:35–40. 2013.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Rajanna DK, Pandey V, Janardhan S and
Datti SN: Broad ligament fibroid mimicking as ovarian tumor on
ultrasonography and computed tomography scan. J Clin Imaging Sci.
3(8)2013.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Naz Masood S, Masood Y and Mathrani J:
Diagnostic dilemma in broad ligament leiomyoma with cystic
degeneration. Pak J Med Sci. 30:452–454. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Bechev B, Magunska N, Kovachev E and
Ivanov S: Laparoscopic treatment of intraligamental leiomyoma per
magna. Akush Ginekol (Sofiia). 55:66–68. 2016.PubMed/NCBI
|
|
10
|
Thanasa E, Thanasa A, Kamaretsos E,
Paraoulakis I, Ziogas A, Kontogeorgis G, Grapsidi V, Gerokostas EE,
Kontochristos V and Thanasas I: Large cervical leiomyoma of the
uterus: A rare cause of chronic pelvic pain associated with
obstructive uropathy and renal dysfunction: A case report. Cureus.
15(e33387)2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yajima R, Kido A, Kuwahara R, Moribata Y,
Chigusa Y, Himoto Y, Kurata Y, Matsumoto Y, Otani S, Nishio N, et
al: Diagnostic performance of preoperative MR imaging findings for
differentiation of uterine leiomyoma with intraligamentous growth
from subserosal leiomyoma. Abdom Radiol (NY). 46:4036–4045.
2021.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ambrosio M, Raimondo D, Savelli L, Salucci
P, Arena A, Borghese G, Mattioli G, Giaquinto I, Scifo MC,
Meriggiola MC, et al: Transvaginal Ultrasound And Doppler Features
Of Intraligamental Myomas. J Ultrasound Med. 39:1253–1259.
2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Wang S, Wang D and Zhao F: A combination
of two novel ligation techniques for complicated laparoscopic
Intraligamental myomectomy. Fertil Steril. 118:207–209.
2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Yanagisawa T, Mori K, Quhal F, Kawada T,
Mostafaei H, Laukhtina E, Rajwa P, Sari Motlagh R, Aydh A, König F,
et al: Iatrogenic ureteric injury during abdominal or pelvic
surgery: A meta-analysis. BJU Int. 131:540–552. 2023.PubMed/NCBI View Article : Google Scholar
|