Introduction
A liver abscess is an infectious condition that can
have varying etiologies, including bacterial or amoebic. It is a
rare entity with an incidence between 3 and 3.6 cases per 100,000
inhabitants in the United States; however, its incidence may be
higher in Latin America, presenting with mortality rates of 25 to
30% (1,2).
The clinical presentation of liver abscesses in the
emergency department requires prompt recognition in order to
prevent morbidity and mortality (3).
Point-of-care ultrasonography (PoCUS) is a useful tool in emergency
services for the rapid detection of pathologies that require urgent
intervention, including infections and abdominal complications.
Furthermore, PoCUS presents a sensitivity between 85-92% (4,5). To
date, reported literature on the use of PoCUS for the early
detection of liver abscesses is limited; the lack of training in
its management by clinical staff in emergency services has also
been described, an issue that is still challenging for the
physician due to the scarcity of symptoms and signs (6,7).
Moreover, in human immunodeficiency virus (HIV)-positive patients,
the usefulness of PoCUS is of utmost importance as a tool for the
exclusion of other differential diagnoses, or common opportunistic
infections in this population, concerns that can delay diagnosis
and subsequent treatment.
The present case report study describes the
importance of medical training in PoCUS in an emergency service, as
it is a rapid strategy for the early diagnosis of liver
abscess.
Case report
A 44-year-old male patient consulted the Hospital
San Vicente Fundación (Rionegro, Colombia) in September, 2022. He
reported a clinical condition of ~1 month of evolution consisting
of an objective fever between 38-39˚C, associated with subjective
weight loss. At 15 days prior to consultation, he presented with a
dry cough and odynophagia, symptoms that were self-limited. At 3
days prior to the consultation, he presented with diarrhea (loose
stool), not dysenteric. At 1 day prior to consulting the hospital,
he had intense pain in the right thoracoabdominal region, with
progressive onset; this reached maximum intensity and thus limited
his ability to walk; for this reason, the patient decided to
consult the hospital.
The patient reported a diagnosis of HIV infection in
2020, being adherent to treatment, without presenting opportunistic
infections until then. The patient has been receiving treatment
with tenofovir + emtricitabine (200/300 mg) every 24 h for 5 years.
In the emergency department, the patient presented with the
following vital signs: Blood pressure, 112/74 mmHg; mean blood
pressure, 87 mmHg; heart rate, 89 beats per minute; respiratory
rate, 16; oxygen saturation, 95%; temperature, 36˚C. Upon a
physical examination, no dehydration and no lymphadenopathy were
observed. He presented abdominal pain upon palpation in the right
hypochondrium and in the thoracoabdominal area, which became more
severe with inspiration.
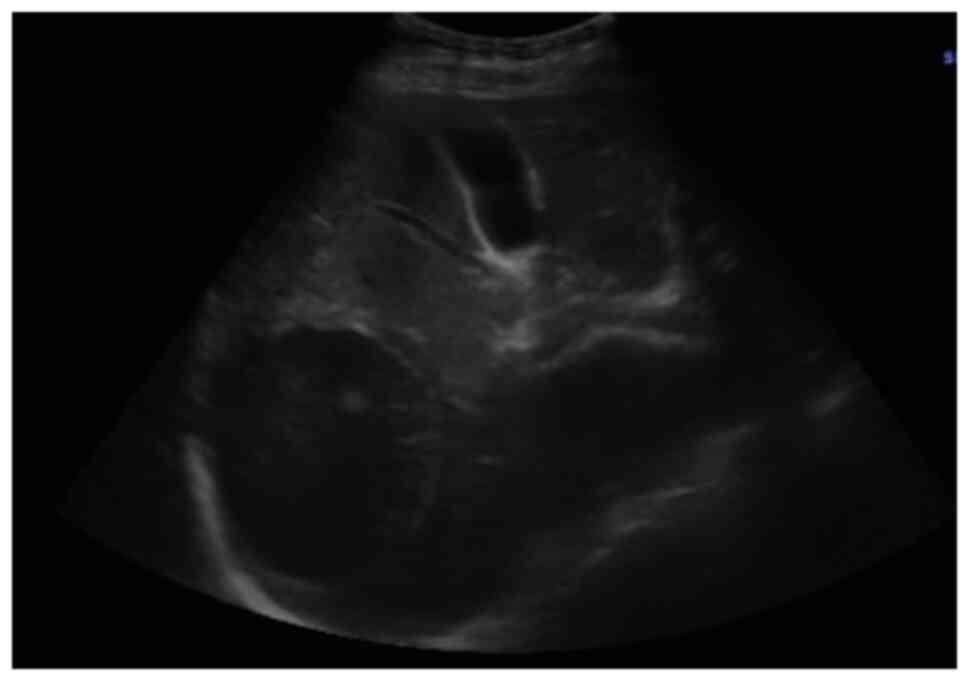
It was decided to perform PoCUS (LOGIQ e, GE
Healthcare) following previously established protocols (6). A hypodense intrahepatic image was
observed between segments VII and VI, with internal echoes
suggestive of a liver abscess (Fig.
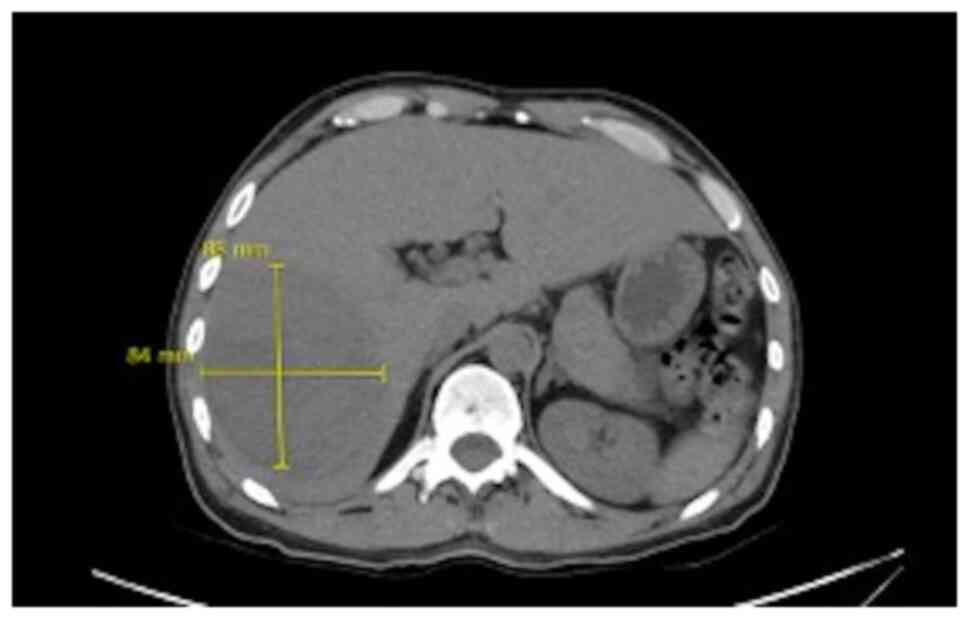
1). An ultrasound of the liver and bile ducts performed by a
radiologist was requested. A well-defined hypodense lesion between
segments VII and VI was confirmed, measuring 81x78x76 mm, with an
approximate volume of 253 cc. He presented internal echoes, faint
posterior acoustic enhancement and minimal perilesional vascular
flow, findings that were associated with the clinical suspicion of
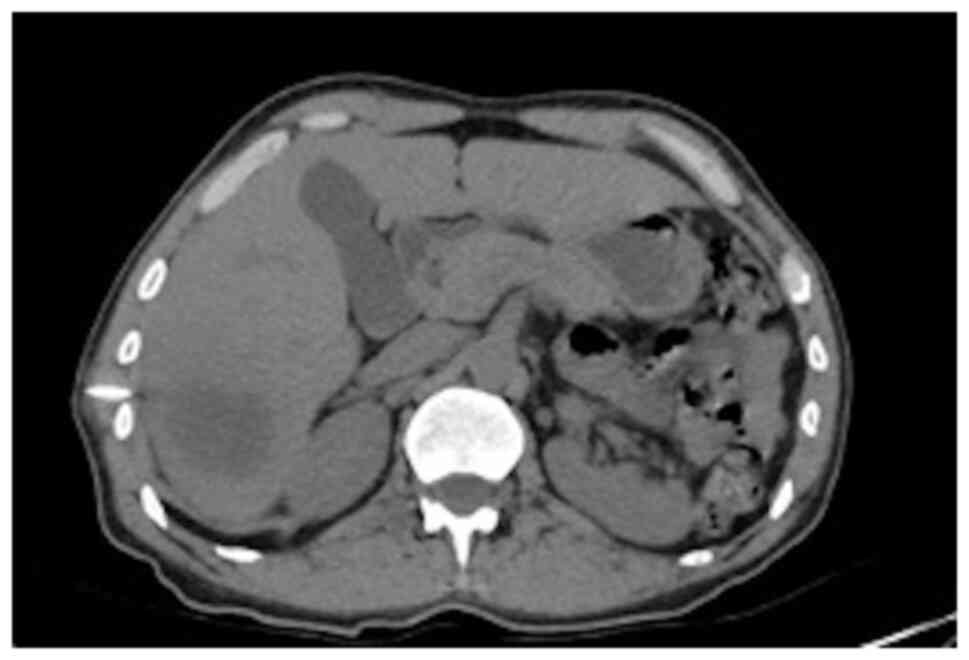
liver abscess (Fig. 2). On the same
day, radiology and general surgery were consulted. It was decided
to perform tomography-guided percutaneous drainage of the liver
abscess (IQon Spectral CT, Philips) following formerly recognized
protocols (6). A 230 cc drainage was
obtained, with no complications (Fig.
3, Fig. 4 and Fig. 5).
Complementary laboratory analyses were performed,
yielding the following results: Leukocytes, 8,700/ml (normal range,
4,500-11,500/ml); neutrophils, 69% (normal range, 40-60%);
hemoglobin, 10.6 g/dl (normal range, 13.8-17.2 g/dl); hematocrit,
32% (normal range, 40.7-50.3%); platelets, 353,000/ml (normal
range, 150,000-400,00/ml); international normalized ratio (INR),
1.4 (normal value, 1); partial prothrombin time (PTT), 30.6 sec
(normal range, 24.2-36.3 sec); prothrombin time (PT), 16.3 sec
(normal range, 12.7-16.3 sec); creatinine, 0.86 mg/dl (normal
range, 0.7-1.3 mg/dl); C-reactive protein, 20.8 mg/dl (normal,
<10 mg/dl); CD4, 345 cells per mm3 (normal range,
200-500 cells per mm3); and an undetectable HIV viral
load. A chest X-ray was performed, which revealed the elevation of
the right hemidiaphragm, without pneumoperitoneum, without the
presence of consolidations that suggested pneumonia or the presence
of pleural effusion (Fig. 6).
Considering all the aforementioned information,
antibiotic treatment with ampicillin/sulbactam and IV metronidazole
was commenced, and hospital management was considered. The patient
presented clinical improvement (with drainage and antibiotic
coverage performed) and was discharged on the third day. It was
recommended antibiotic management at home (oral metronidazole)
until completing 15 effective days of treatment.
Discussion
A liver abscess can be defined as a collection of
purulent material encapsulated within the liver parenchyma caused
by bacteria, fungi and/or parasites. Pyogenic liver abscess may be
initiated by a diversity of microorganisms, involving
Escherichia coli, Klebsiella pneumoniae and Burkholderia
pseudomallei. The microbiology varies rendering to the assumed
course of hepatic invasion. Infections can occur from the biliary
tree, circulation, an adjacent point of infectivity and acute
damage (1,8). The incidence of liver abscess varies
according to the region, with ranges that occur from 2.3 cases per
100,000 inhabitants admitted to the hospitals in the United States,
and up to 17.6 per 100,000 inhabitants admitted to hospitals in
Taiwan (1,2). Mortality has been shown to be reduced
from 50 to 10% following the use of percutaneous intervention
guided by ultrasonography or tomography (8,9).
As observed in the patient presented herein, the
majority of cases are observed in males, between the third and
sixth decade of life. The etiology of liver abscess is
multifactorial and is related to predisposing factors (1,6). The
associated risk factors increase the presence of liver abscesses in
individuals with oncological diseases, diabetes mellitus,
immunosuppression, alcoholism and local factors, such as biliary
causes (history of hepatobiliary surgery, chronic obstruction of
the bile ducts), portal causes (chronic infectious focus drained by
the portal) and the superimposition of pre-existing lesions (cyst
and necrotic hepatic metastasis) (9,10).
The incidence of fungal abscesses is on the rise due
to the increase in the number of immunocompromised patients.
Candida species is the most common fungal infection, and
bacterial co-infection is common (10). Cryptococcal liver abscess is
frequently observed in the context of HIV, solid organ transplant,
primary immune deficiency, or lymphoid hemopathies. The mode of
presentation may consist of hepatitis, possibly fulminant, or
diffuse micro abscesses (10-12).
Although episodes of liver abscess have been
reported in HIV-positive patients, the specific symptoms remain
unclear. In these patients, it is generated by the colonization of
the colon by trophozoites that produce ulcerative lesions in the
mucosa, due to an immune deficiency of CD4+
T-lymphocytes and macrophages. This leaves the capillaries exposed,
generating their migration to the enteric-hepatic venous system;
once it is in the parenchyma, it can remain and produce lysis,
causing liver abscess, or it can be distributed in other organs
with portal circulation (13-15).
As regards culture results, it has been indicated
that these may be variable. The study conducted by Zhang et
al (16) presented positive
results in 16% of cases and the presence of positive blood cultures
in 5.4% of patients. The microorganisms identified were
Staphylococcus aureus and Staphylococcus haemolyticus
(16).
The presence of a liver abscess in patients with HIV
may be associated with co-infections, such as pneumonia,
Candida infection and bacterial peritonitis; infections that
did not occur in the present case (17). Hence, the importance of recognizing
the probable microbiological etiology to guide therapy (18). On the other hand, HIV-positive
patients may also present with other complications, such as the
appearance of tumors including sarcomas located in various parts of
the body (19) and hepatocellular
carcinomas (20). Some of these
tumors are associated with opportunistic infections that appear
with a low CD4 count (19,20).
Imaging systems, including ultrasonography and
computed tomography scanning are valuable implements to validate an
area occupying lesion and corroborate the occurrence or
non-existence of a liver abscess. Computed tomography has a
superior sensitivity compared to ultrasound for the detection of
liver abscess; however, this possibility can not permanently be
available in low-middle income countries (21). Ultrasound is conventionally the
initial image used in clinical practice for the evaluation of the
liver, with a good performance to evaluate its lesions. Moreover,
it is not expensive, it can be repeated multiple times, it is
accessible and it does not generate radiation. It is widely used
not only in the diagnosis of a liver abscess, but also in patient
management in all phases of the diagnostic-therapeutic process
(22); it is also appropriate to use
ultrasound in various diseases of the liver, such as cirrhosis and
tumors (23). Therefore, when the
signs and symptoms indicate a liver abscess, ultrasound can be a
guiding instrument to reach this diagnosis. This can identify
lesions >2 cm in diameter, which shows a sensitivity of 85 to
95%, which can even increase when the study is improved with the
addition of contrast. For its part, computed tomography has a
sensitivity of 95% and can detect abscesses up to 0.5 cm (24,25).
Amebiasis is a common parasitic disease worldwide
and is prevalent in all tropical countries (26,27).
There are ultrasound protocols for parasitic infections. Upon an
ultrasound, an amoebic liver abscess presents as a focal liver
lesion that is unique in 60% of cases. It is located more
frequently in the posterior part of the right lobe. The main
clinical and ultrasound differential diagnosis of amoebic liver
abscess is a pyogenic liver abscess (28,29).
However, it is sometimes difficult to identify in the early stages
due to the similar echogenicity of the surrounding liver tissue;
pyogenic lesions become hypoechoic compared to the liver and may be
more variable in shape and often have irregular walls (30).
As handled in the case described in the present
study, antimicrobial guidelines usually advise empiric treatment,
indicating both amoebic and pyogenic causes of liver abscess. As
therapy is frequently managed prior to the compilation of suitable
samples, the causal microorganism and occurrence of either sickness
remain imprecise (21).
The mortality rate from liver abscesses in the 20th
century was close to 75-80%. With the commencement of antibiotic
coverage, the mortality rate was reduced, targeting microorganisms
such as Gram-negative bacilli, Gram-positive cocci and anaerobic
bacteria. Therefore, treatment with third-generation cephalosporins
plus metronidazole or piperacillin/tazobactam has been shown to be
effective. As regards the treatment of patients with HIV, if this
is ineffective, the possibility of opportunistic infections should
be suspected. Percutaneous drainage in these patients can reduce
the mortality rate to 10-30% (31).
In conclusion, the clinical features and laboratory
findings of HIV-infected patients with a liver abscess may be
non-specific. Moreover, it is recommended to obtain a blood sample
to perform a culture to determine the variety of microorganism
involved in the infection and thus establish its origin. Likewise,
the assessment of the etiology of the infection is very relevant.
Liver abscess is not a rare condition in tropical countries; it is
an emerging condition that carries high mortality if it is
diagnosed incorrectly, or late and is not treated. The early
identification and the use of PoCUS by the emergency physician may
help to lead to timely management and interventions in the
emergency department.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
MZG, DGA, RAOC, DNH and CMA contributed to the
conception and design of the study. CMA wrote the manuscript. MZG,
DGA, RAOC and DNH searched the literature. MZG, DGA, RAOC and DNH
provided clinical assistance to the patient and were responsible
for the treatments. MZG and CMA revised the manuscript. MZG and CMA
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
The Bioethics Committee of San Vicente Fundación
Hospital (Rionegro, Colombia) approved the publication of this
case. Written informed consent for the publication of clinical
details and images was obtained from the patient.
Patient consent for publication
Written informed consent for the publication of
clinical details and images was obtained from the patient.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Johannsen EC, Sifri CD and Madoff LC:
Pyogenic liver abscesses. Infect Dis Clin North Am. 14:547–563,
vii. 2000.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Meddings L, Myers RP, Hubbard J, Shaheen
AA, Laupland KB, Dixon E, Coffin C and Kaplan GG: A
population-based study of pyogenic liver abscesses in the United
States: Incidence, mortality, and temporal trends. Am J
Gastroenterol. 105:117–124. 2010.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Chia DWJ, Kuan WS, Ho WH, Sim TB and Chua
MT: Early predictors for the diagnosis of liver abscess in the
emergency department. Intern Emerg Med. 14:783–791. 2019.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Lin AC, Yeh DY, Hsu YH, Wu CC, Chang H,
Jang TN and Huang CH: Diagnosis of pyogenic liver abscess by
abdominal ultrasonography in the emergency department. Emerg Med J.
26:273–275. 2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Pearl R, Pancu D and Legome E: Hepatic
abscess. J Emerg Med. 28:337–339. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
McClure MB, Patel K, Cabrera G and
Kalivoda EJ: Point-of-care ultrasound diagnosis of a pyogenic liver
abscess in the emergency department. J Am Coll Emerg Physicians
Open. 2(e12412)2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mavilia MG, Molina M and Wu GY: The
evolving nature of hepatic abscess: A review. J Clin Transl
Hepatol. 4:158–168. 2016.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Rivero-León A and Núñez-Calatayud M:
Modified amoebic liver abscess: Case report. Rev Colomb
Gastroenterol. 37:242–247. 2022.
|
|
9
|
Gallego A, Ramírez A and Gallego A:
Pyogenic liver abscess, polycystic bag and chronic renal failure.
Rev Elec Dr. Zoilo E: Marinello Vidaurreta 43: 2, 2018. https://revzoilomarinello.sld.cu/index.php/zmv/article/view/1233.
|
|
10
|
Rossi G, Lafont E, Rossi B, Dokmak S,
Ronot M, Zarrouk V, Fantin B and Lefort A: Liver Abscess.
EMC-Tratado de Medicina. 22:1–10. 2018.In Spanish. https://www.sciencedirect.com/science/article/abs/pii/S1636541017878685.
|
|
11
|
Mourad MM, Liossis C, Algarni A, Kumar S
and Bramhall SR: Primary hepatic tuberculosis in immunocompetent
adults: A UK case series. Oxf Med Case Reports. 2014:148–150.
2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Stanley SL Jr: Amoebiasis. Lancet.
361:1025–1034. 2003.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Rahimian J, Wilson T, Oram V and Holzman
RS: Pyogenic liver abscess: Recent trends in etiology and
mortality. Clin Infect Dis. 39:1654–1659. 2004.PubMed/NCBI View
Article : Google Scholar
|
|
14
|
Price JC and Thio CL: Liver disease in the
HIV-infected individual. Clin Gastroenterol Hepatol. 8:1002–1012.
2010.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Sáchez-Pobre P, Sáenz-López S, Salto E,
Sanjuán R, Ibero C, Masedo A and Solís Herruzo JA: Amebic liver
abscess with bacterial superinfection in a patient with no
epidemiologic risk factors. Rev Esp Enferm Dig. 96:796–800.
2004.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
16
|
Zhang W, Yu H, Luo N and Hu Z: Clinical
characteristics and treatment outcomes in human immunodeficiency
virus (HIV)-infected patients with liver abscess: A retrospective
study of 53 patients. Med Sci Monit. 26(e923761)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Rendón Unceta P, Macías Rodríguez MA,
Correro Aguilar F, Prieto García JL, Díaz García F and Martín
Herrera L: Hepatic abscesses: Is simple aspiration puncture with
echography control an alternative to catheter drainage?
Gastroenterol Hepatol. 23:470–473. 2000.PubMed/NCBI(In Spanish).
|
|
18
|
Boccatonda A, D'Ardes D, Cocco G,
Cipollone F and Schiavone C: Ultrasound and hepatic abscess: A
successful alliance for the internist. Eur J Intern Med.
68:e19–e21. 2019.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Colović N, Jurišić V, Terzić T, Jevtovic D
and Colović M: Alveolar granulocytic sarcoma of the mandible in a
patient with HIV. Onkologie. 34:55–58. 2011.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Yuan Z, Ma R, Zhang Q and Zhao CS:
Statistical inferences of HIVRNA and hepatocellular carcinoma based
on the PAK1 expression via neural network model. Curr HIV Res: Nov
28, 2022 (Epub ahead of print).
|
|
21
|
Khim G, Em S, Mo S and Townell N: Liver
abscess: Diagnostic and management issues found in the low resource
setting. Br Med Bull. 132:45–52. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Cardona-Castro W, Zuluaga-Gómez M,
González-Arroyave D and Ardila CM: Accuracy of point-of-care
ultrasonography in the diagnosis of necrotizing fasciitis: A case
report. Biomed Rep. 17(98)2022.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Glišić TM, Perišić MD, Dimitrijevic S and
Jurišić V: Doppler assessment of splanchnic arterial flow in
patients with liver cirrhosis: Correlation with ammonia plasma
levels and MELD score. J Clin Ultrasound. 42:264–269.
2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Elia F, Campagnaro T, Salacone P and
Casalis S: Goal-directed ultrasound in a resource-constrained
healthcare setting and a country Developing. Crit Ultrasonido J.
3:51–53. 2011.In Spanish. https://www.medigraphic.com/pdfs/revcliescmed/ucr-2015/ucr155j.pdf.
|
|
25
|
Weinke T, Grobusch MP and Güthoff W:
Amebic liver abscess-rare need for percutaneous treatment
modalities. Eur J Med Res. 7:25–29. 2002.PubMed/NCBI
|
|
26
|
Vidal JE, da Silva PR, Schiavon Nogueira
R, Bonasser Filho F and Hernandez AV: Liver abscess due to
Salmonella enteritidis in a returned traveler with HIV infection:
Case report and review of the literature. Rev Inst Med Trop Sao
Paulo. 45:115–117. 2003.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Mortelé KJ, Segatto E and Ros PR: The
infected liver: Radiologic-pathologic correlation. Radiographics.
24:937–955. 2004.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Malik AA, Bari SU, Rouf KA and Wani KA:
Pyogenic liver abscess: Changing patterns in approach. World J
Gastrointest Surg. 2:395–401. 2010.PubMed/NCBI View Article : Google Scholar
|
|
29
|
McNeil T, Daniel S and Gordon DL:
Management of pyogenic liver abscess: A South Australian
experience. ANZ J Surg. 90:2274–2278. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chen MJ, Huang MJ, Chang WH, Wang TE, Wang
HY, Chu CH, Lin SC and Shih SC: Ultrasonography of splenic
abnormalities. World J Gastroenterol. 11:4061–4066. 2005.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Kuo SH, Lee YT, Li CR, Tseng CJ, Chao WN,
Wang PH, Wong RH, Chen CC, Chen SC and Lee MC: Mortality in
emergency department sepsis score as a prognostic indicator in
patients with pyogenic liver abscess. Am J Emerg Med. 31:916–921.
2013.PubMed/NCBI View Article : Google Scholar
|