Introduction
The novel concept of rapid access to the sellar
region was first highlighted by Davide Giordano, an Italian
anatomist, in 1897(1), while Hermann
Schloffer, an Austrian neurosurgeon, was the first to introduce
transsphenoidal pituitary surgery in 1907 by the superolateral
nasoethmoidal approach (2). In 1909,
H. Cushing took the approach a step further, demonstrating the
superiority of the sublabial, transseptal and transsphenoidal
approaches; subsequently, in the 1960s, J. Hardy was the pioneer
who routinely combined the use of televised radiofluoroscopy,
optical magnification with the surgical microscope, and the use of
microsurgical techniques in his approach (3-6).
At the beginning of the 2000s, the post-operative outcomes of
certain hospitals created a trend towards the use of the transnasal
transsphenoidal approach as it is currently known, with credit
given to E. Laws, who demonstrated a series of >6,000 patients
who were operated on using that approach (3-7).
The microsurgical transsphenoidal (MST) technique
(either sublabial or transnasal) was the gold standard approach for
pituitary surgery. Each approach has its advantages and
disadvantages. In the 1990s, the introduction of rigid endoscopes
gave rise to the endonasal endoscopic transsphenoidal (EET)
approach (8-13).
The EET approach was not instantly adopted by the majority of
neurosurgeons. Notwithstanding, the endoscopic systems evolved and,
along with the introduction of extended endoscopic approaches and
improved methods of anterior cranial base reconstruction, such as
the Hadad-Bassagasteguy flap, led to the utilization of the EET
approach by more neurosurgeons (14-16).
The currently available literature includes a
plethora of meta-analyses and actual studies providing strong
evidence that supports the superiority of the ETT over the MST
approach (17-21).
Pioneers of the EET approach, such as Jho and Carrau (22,23) in
their early reports, emphasized the advantages of their methods,
such as the greater panoramic view during the surgery, a more rapid
post-operative recovery, and the avoidance of nasal packing.
The study by Gao et al also underlined the
better view inside the sellar region and the lesser trauma to the
tissues, while they demonstrated similar results compared to the
widely utilized sublabial approach (17).
The learning curve of the EET technique was one of
the main reasons why many neurosurgeons treated this technique as
an adjunct and did not use this as a replacement of the MST
approach in the late 1990s (24).
Furthermore, with the exception of the double-blind randomized
controlled trial by Jain et al (24), to the best of our knowledge, there is
only a small number of studies directly comparing the two
techniques (25), which does not
allow for a confident verdict. Thus, it could be argued that there
is no clear superiority of one of the methods to the other.
The aim of the present study was to compare the
outcomes of pituitary macroadenomas operated using the EET approach
by a team comprised of two young consultants with those operated by
a team of senior neurosurgeons with extensive experience in using
sublabial MST pituitary surgery.
Patients and methods
The present study examined a series of 20 patients
who underwent pituitary macroadenoma resection at the Nicosia
General Hospital (Nicosia, Cyprus) between May, 2004 to January,
2021. The patients were separated into two groups as follows: The
first group included the 10 last patients operated by the former
neurosurgical team, composed of neurosurgeons with 20 to 30 years
of experience in using the MST approach. The second group, included
the first 10 patients that were operated by the current
pituitary-surgery team, comprised of an otolaryngologist and a
neurosurgeon with 6 and 4 years of experience in endoscopic
pituitary surgery, respectively.
Data for patient demographics, the date of the
surgery, the surgeon and surgical approach (sublabial microscopic
or endonasal endoscopic), late cerebrospinal fluid (CSF) leak,
tumor recurrence, the duration of hospitalization or
re-hospitalization in the case of redo, vision status pre- and
post-operative, intra-operative complications, miscellaneous
complications, lumbar drainage insertion or not post-operatively,
and peri-operative mortality were all collected retrospectively.
Pituitary hormones were assessed pre- and post-operatively using
clinical and biochemical data. The abnormal function of the axis
was defined as biochemical data outside reference values for the
respective hormone or in the case of patients that were already on
substitution therapy. The intact function was defined in the case
of hormone levels within the normal range. The patients in the MST
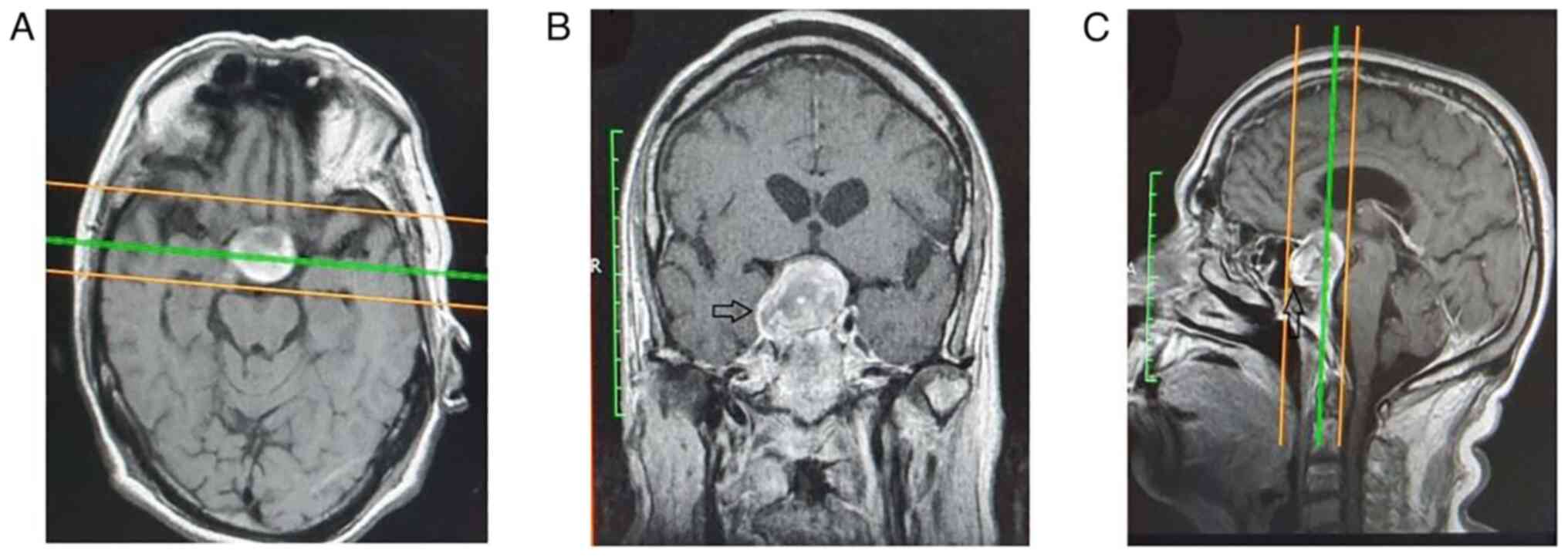
approach group underwent the standard Hardy method (Fig. 1). An incision was performed, the
vomer was removed, and the sphenoid sinus was accessed. Entering
the sphenoid sinus, the floor of the sellar region was opened,
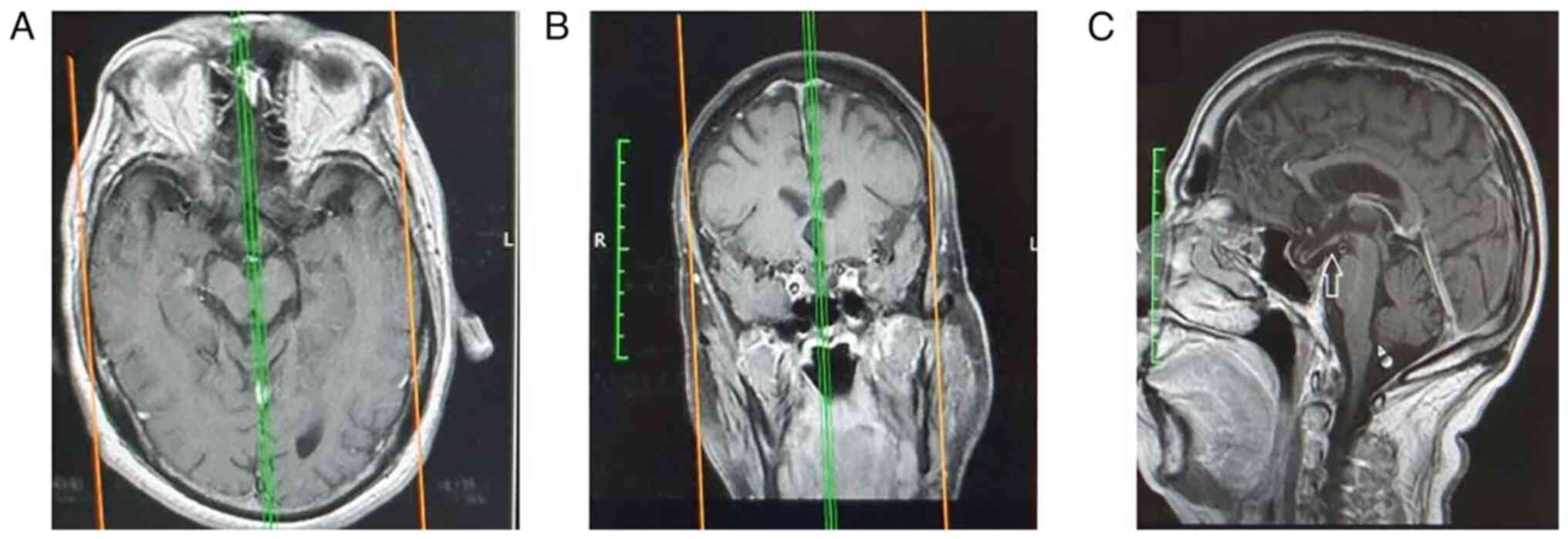
revealing the hypophysis. The post-operative radiological
evaluation is depicted in Fig.
2.
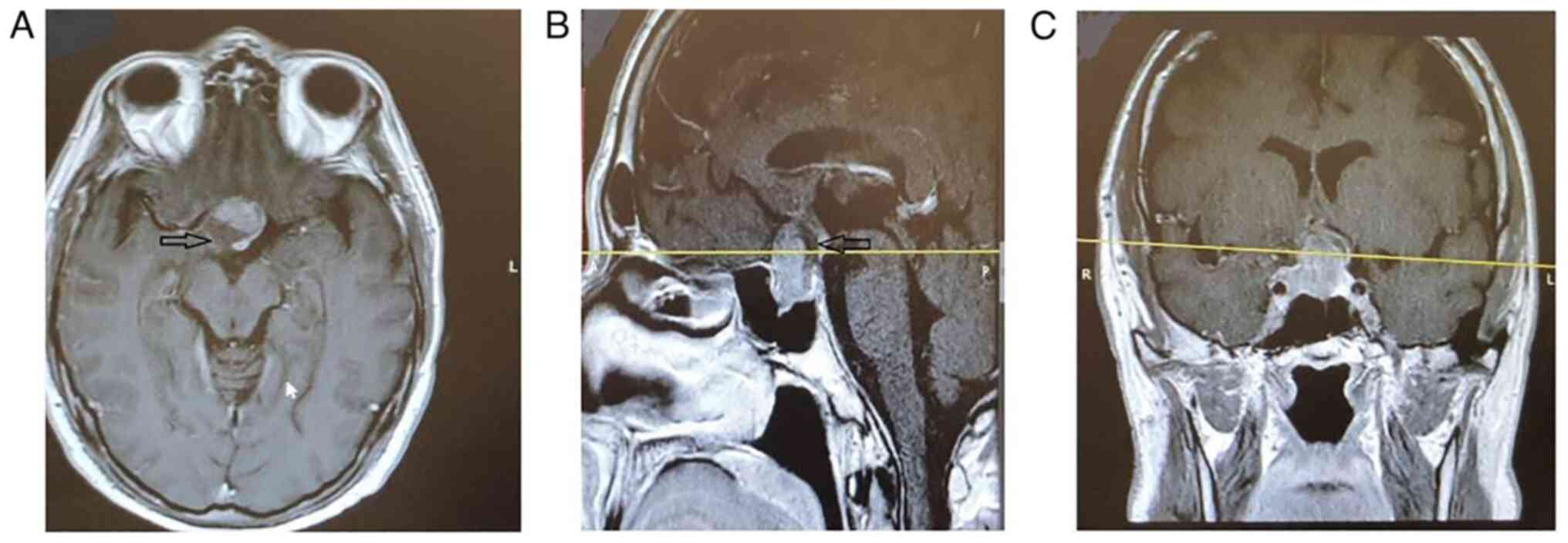
For the EET approach group (Fig. 3), a combination of 0˚, 30˚ and 45˚
rigid endoscopes were utilized to ensure adequate exposure and
visualization during tumor removal. The tumor bed was filled with
abdominal fat, the anterior wall of the sphenoid sinus was
reconstructed, and the watertight closure was ensured using a
triple layer of artificial dura, tissue glue, and rhino-septal
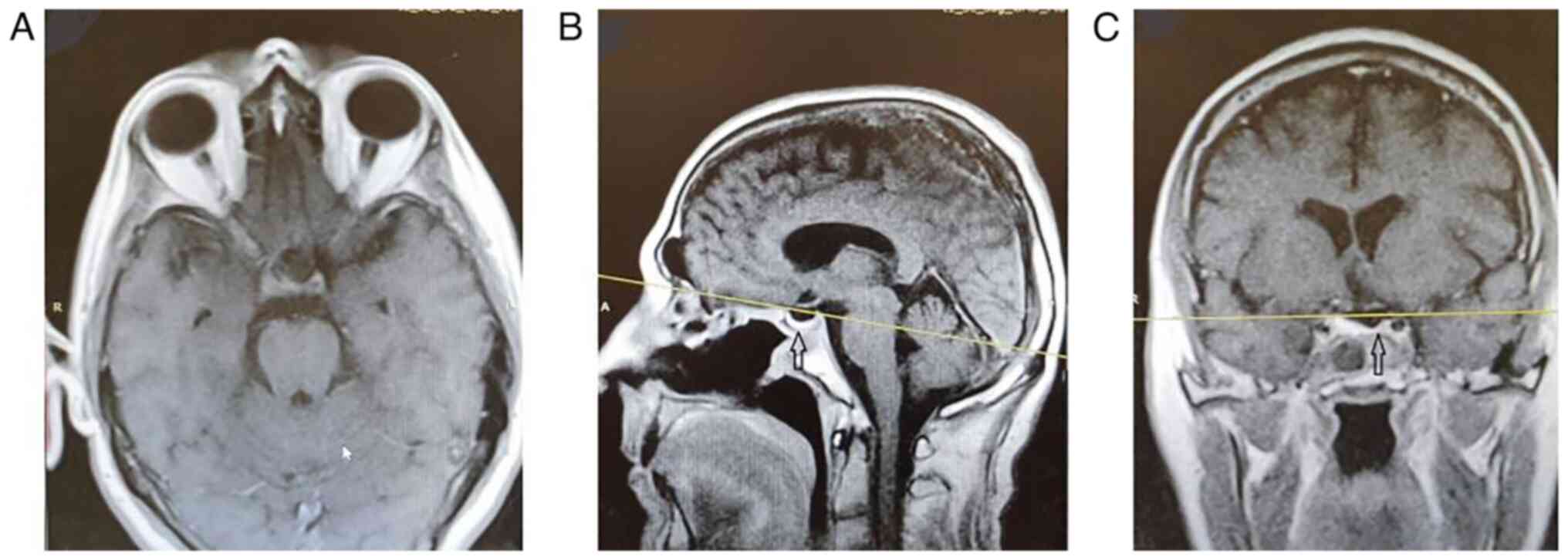
mucosal flaps. The follow-up of the patients with a magnetic
resonance imaging (MRI) and evaluation in the outpatient clinic was
similar in both groups at 1 month post-operatively, 6 months
post-operatively and once annually (Fig.
4).
All surgical records were retrieved from the
database of the hospital and accessed in an anonymous manner using
unique code identifiers. The Institutional Review Board (IRB) of
Nicosia General Hospital, Cyprus approved the study (IRB no. EEBK
EΠ 2019.02.158). The study was in line with the Declaration of
Helsinki in 1995 (as revised in Edinburgh 2000).
Results
The patient demographics and clinical data,
including surgical outcomes, are summarized in Table I. The first group of surgeries were
performed between 2004 and 2015, and the patients were followed-up
post-operatively for 1 month, 6 months, and annually for 5 years
post-operatively. The male to female ratio sex ratio in the MST
group was 7:3, while the mean age was 59.9±13.1 years.
 | Table IDemographic and clinical data of the
patients in the sublabial and endonasal groups. |
Table I
Demographic and clinical data of the
patients in the sublabial and endonasal groups.
| Parameters | MST group | EET group |
|---|
| No. of
patients | 10 | 10 |
| Mean age,
years | 59.5±13.1 | 54.6±12.0 |
| Sex | | |
|
Male | 7 (70%) | 5 (50%) |
|
Female | 3 (30%) | 5 (50%) |
| Pituitary function
pre-operatively | | |
|
Normal | 4 (40%) | 3 (30%) |
|
Prolactinoma | 2 (20%) | 2 (20%) |
|
Apoplexy | 1 (10%) | 2 (20%) |
|
Acromegaly | 1 (10%) | 2 (20%) |
|
Panhypopituitarism | 2 (20%) | 0 |
|
Hypocortisolism
and hypothyroidism | 0 | 1 (10%) |
| Hormone Replacement
Post-operative | 3 (30%) | 2 (20%) |
| Vision Status | | |
|
Normal | 5 (50%) | 5 (50%) |
|
Deficit
pre-operative | 5 (50%) | 5 (50%) |
|
Improvement
post-operative | 4 (80%) | 5 (100%) |
| Recurrence and
redo | 1 (10%) | 0 |
| Late leak | 2 (20%) | 2 (20%) |
| Primary
hospitalization (days) | 12.6±13.1 | 12.4±7.9 |
| Secondary
hospitalization | 2 (20%) | 0 |
| Intra-operative
complications | 3 (30%) | 3 (30%) |
| Miscellaneous
complications | | |
|
None | 10 (100%) | 8 (80%) |
|
Pneumonia | 0 | 1 (10%) |
|
Sepsis | 0 | 1 (10%) |
| Gross tumor
removal | | |
|
Residual | 3 (30%) | 1 (10%) |
|
Total | 7 (70%) | 9 (90%) |
| Lumbar drain | 1 (10%) | 1 (10%) |
| Mortality | 0 | 1 (10%) |
The macroadenomas in the MST group were two
prolactinomas, one growth hormone (GH)-secreting adenoma causing
acromegaly, and two tumors that caused panhypopituitarism, while
four patients had normal hormone levels. Finally, 1 patient had
pituitary apoplexy. The patients with prolactinomas required
surgery due to an acute loss of vision. In total, 3 patients
required post-operative hormone replacement; specifically, the
patient with apoplexy at presentation and the ones with
panhypopituitarism.
At presentation, visual deficits were reported in
half of the patients. Of these 5 patients, 4 patients recovered
completely, while 1 patient remained with a stable visual deficit
(bitemporal hemianopia, which was initiated 2 days prior to his
arrival at the hospital). Intra-operative complications included
two cases of CSF leak and one case of intra-operative bleeding.
The mean duration of hospitalization in the MST
group was 12.6±13.1 days (range, 5-48 days). In this group, 1
patient had an extensive intra-operative cavernous sinus
hemorrhage, which led to the termination of tumor removal by the
surgeons. The patient required 48 days of hospitalization; the
hematoma was subsequently resolved, while he did not undergo a
re-operation for the residual tissue. Additionally, 2 patients
required secondary hospitalization. The first patient required a
further 9 days of hospitalization and was the only one that
required lumbar drainage. The other patient remained in the
hospital for a total of 22 days. The latter patient also required a
redo operation 14 years later for a recurrence, which was performed
using a transcranial approach. Total tumor removal was achieved in
7 patients (70%), and in the remaining 30% of patients, a subtotal
resection was performed. No deaths were reported in the MST group.
In the EET group, the surgeries were performed between 2017 and
2021. The sex male to female ratio was equal (5:5), and the mean
patient age was 54.6±12.0 years. The macroadenomas in this group
were two prolactinomas and two GH-secreting adenomas. In total, 3
patients from the latter group had normal hormone levels, while 2
patients presented with pituitary apoplexy. The patients with
prolactinomas, similarly to the patients of the MST group, were
operated on due to acute vision disturbance at presentation. In
addition, 2 patients required permanent hormone replacements
post-operatively.
Half of the patients reported visual deficits at
presentation, although their vision significantly improved after
the surgery. A small residual tumor was observed in 1 patient in
the EET group and this patient has remained stable during the
follow-up period. The mean duration of hospitalization was 12.4±7.9
days (minimum, 7 days; maximum, 33 days).
The complications in the EET group included 3
patients who had CSF leak intra-operatively. The intra-operative
meningoplasty was sufficient in one of the patients, while the
other 2 patients exhibited a late CSF leak. These patients
underwent an endoscopic meningoplasty, while in one of the latter
cases, the use of a lumbar drain was necessary. Ultimately, the CSF
leak was resolved. Ultimately, the CSF leak was resolved. In the
EET group, one death was reported; however, this was not associated
with the procedure per se. This patient was admitted with an acute
visual deficit. The macroadenoma was identified; however, due to a
respiratory infection, the surgery was postponed. When the patient
recovered, the surgery was performed using an EET approach. On the
5th day post-operatively, the patient developed a recurrence of the
respiratory infection, followed by sepsis, admission to the
intensive care unit, and ultimately death.
The follow-up of the patients with an MRI and
evaluation in the outpatient clinic was similar in both groups,
namely 1 month post-operatively, 6 months post-operatively, and
once annually.
Discussion
In the past, only a small number of studies that
compared the efficacy of EET vs. MST were available. In these
studies, no clear recommendation for which approach should be used
was made (21,25,26).
The systematic review and meta-analysis by Goudakos
et al (26) 10 years ago
concluded that due to the subjectivity of the outcomes, the lack of
standardized protocols, the short follow-up period of the patients
and the retrospective nature of the studies, no clear verdict upon
whether the EET approach was superior to MST could be stated. The
latest meta-analysis promotes the superiority of EET compared to
MST in terms of fewer complications, larger tumor removal, and less
operative time (18,21,25-29).
Other studies promote the superiority of EET compared to MST in
terms of fewer complications, improved tumor removal and a
decreased operative time (18,28,29).
The present study, using a case series of 20
patients, demonstrated that EET could provide equal surgical
outcomes when applied by surgeons with a relatively brief
experience compared to extensively experienced neurosurgeons who
use the MST approach for treating a long list of microadenomas and
numerous macroadenomas. Additionally, using EET, a 90 vs. 70% gross
tumor removal was achieved compared with the MST group. The
superior results of EET over MST are in agreement with the current
literature (27,30-34).
Furthermore, the literature demonstrates that the
duration of hospitalization is shorter or at least not longer in
patients treated with EET compared to MST (26,32,34-37).
The study by Razak et al (29) is one of the exceptions, in that it
reports a more extended duration of hospitalization by EET vs. MST
when it comes to non-functioning adenomas. In the series in the
present study, there was a longer mean hospitalization duration,
than that described in the meta-analysis by Gao et al
(17). 12.4±7.9 vs. 5.1±0.7,
respectively This can be explained by the fact that in the series
in the present study, nasal packing was used in all patients
post-operatively. This may violate the post-operative algorithm
proposed by a number of authors (19,20,26);
however, none of the patients in the EET group in the present study
exhibited post-operative epistaxis, a common complication of the
procedure (17).
The comparison of the present EET and MST series
revealed similar intra- and post-operative characteristics, as
presented in Table I, even though
the EET group was operated by two young, yet well-trained surgeons.
However, the literature frequently notes that the EET approach has
a long learning curve (17,33,38). In
the late 1990s, Ciric et al (39) mentioned that the significantly lower
rate of morbidity and mortality of the EET approach compared to the
MST approach could be achieved once a surgeon has performed 200 or
up to 500 endoscopic endonasal pituitary surgeries. In the study by
O'Malley et al (33),
previously non-experienced neurosurgeons in endoscopic approaches
demonstrated improved surgical outcomes after 17 surgeries using
the EET approach. Additionally, in multidisciplinary skull base
teams, the long experience of ENT surgeons in endonasal endoscopic
surgery offers an additional advantage; it may contribute to the
more rapid mastering of the endoscopic approach (40). In the present study, the EET group
demonstrated an improved post-operative visual improvement, and an
improved post-operative hormonal status, while none of the patients
required a re-do for persistent tumor or relapse. According to the
study by Zaidi et al (41),
the results were comparable between surgeons with 1 year of EET
experience and highly experienced surgeons with 30 years of MST
pituitary surgeries (41).
Several limitations of the presented study should be
mentioned. The present study was retrospective in nature, which
renders it prone to reporting and selection bias. The study
presented all the cases that have been operated with the endonasal
endoscopic approach and the last 10 patients operated with the MST
technique by the previous team of neurosurgeons in the hospital.
The follow-up in the EET group (maximum of 2 years) was shorter
than that of the MST cases, as the MST group included older cases,
while the EET group included recent cases, which is the reason for
the difference in the follow-up period. Thus, a possible tumor
relapse or long-term post-operative complications may not have been
manifested in that time frame in the EET group. In addition,
another limitation of the present study is that the population
included in the two groups was not homogenous, as the sex ratio was
not the same between the two groups, and the mean age in MST group
was 59.5±13.1 and that in the EET group was 54.6±12.0. Finally, the
small sample size of the series does not allow for a proper
statistical analysis. A greater number of cases would allow for the
presentation of more solid data.
In conclusion, the endonasal endoscopic approach for
pituitary tumors tends to be established as the gold standard
technique, as it is steadily gaining ground over the traditional
microscopic approach. The learning curve is known to be long;
however, in the case series in the present study, the new skull
base team demonstrated equal or even better results than those of
the past neurosurgical team of the same department. Colleagues who
have yet to familiarize themselves with the endonasal endoscopic
approach may thus be encouraged to learn and utilize this
technique, provided that their center is staffed with an
experienced team of skull base surgeons to intervene in an
intraoperative complication.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
SC, AA, KF and GF conceptualized the study. KF and
AA performed the surgeries in the EET group. VEG, AAF, KT, NT, PS,
DAS, NM and PP made a substantial contribution to data analysis and
interpretation, and wrote and prepared the draft of the manuscript.
GF and KF analyzed the data and provided critical revisions. GF and
KF confirm the authenticity of all the data. All authors
contributed to manuscript revision, and have read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
The Institutional Review Board (IRB) of Nicosia
General Hospital, Cyprus approved the study (IRB no. EEBK EΠ
2019.02.158). The study was in line with the Declaration of
Helsinki in 1995 (as revised in Edinburgh 2000).
Patient consent for publication
Written informed was obtained from the patients for
publication of the data and associated images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Artico M, Pastore FS, Fraioli B and
Giuffrè R: The contribution of Davide Giordano (1864-1954) to
pituitary surgery: the transglabellar-nasal approach. Neurosurgery.
42:909–911; discussion 911-912. 1998.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Schmidt RF, Choudhry OJ, Takkellapati R,
Eloy JA, Couldwell WT and Liu JK: Hermann Schloffer and the origin
of transsphenoidal pituitary surgery. Neurosurg Focus.
33(E5)2012.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Hardy J: Transphenoidal microsurgery of
the normal and pathological pituitary. Clin Neurosurg. 16:185–217.
1969.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hardy J and Vezina JL: Transsphenoidal
neurosurgery of intracranial neoplasm. Adv Neurol. 15:261–273.
1976.PubMed/NCBI
|
|
5
|
Cushing H: Partial hypophysectomy for
acromegaly: With remarks on the function of the hypophysis. Ann
Surg. 50:1002–1017. 1909.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cushing H: The pituitary body and its
disorders, clinical states produced by disorders of the hypophysis
cerebri. J.B. Lippincott Company, Philadelphia, 1912.
|
|
7
|
Grosvenor AE and Laws ER: The evolution of
extracranial approaches to the pituitary and anterior skull base.
Pituitary. 11:337–345. 2008.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Laws ER Jr and Barkhoudarian G: The
transition from microscopic to endoscopic transsphenoidal surgery:
The experience at Brigham and women's hospital. World Neurosurg. 82
(6 Suppl):S152–S154. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Cavallo LM, Solari D, Esposito F and
Cappabianca P: Endoscopic endonasal approach for pituitary
adenomas. Acta Neurochir (Wien). 154:2251–2256. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Jankowski R, Auque J, Simon C, Marchai JC,
Hepner H and Wayoff M: Endoscopic pituitary tumor surgery.
Laryngoscope. 102:198–202. 1992.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Carrau RL, Jho HD and Ko Y:
Transnasal-transsphenoidal endoscopic surgery of the pituitary
gland. Laryngoscope. 106:914–918. 1996.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Gamea A, Fathi M and el-Guindy A: The use
of the rigid endoscope in trans-sphenoidal pituitary surgery. J
Laryngol Otol. 108:19–22. 1994.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Jho HD and Carrau RL: Endoscopy assisted
transsphenoidal surgery for pituitary adenoma. Technical note. Acta
Neurochir (Wien). 138:1416–1425. 1996.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Chibbaro S, Signorelli F, Milani D, Cebula
H, Scibilia A, Bozzi MT, Messina R, Zaed I, Todeschi J, Ollivier I,
et al: Primary endoscopic endonasal management of giant pituitary
adenomas: Outcome and pitfalls from a large prospective multicenter
experience. Cancers (Basel). 13(3603)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Hadad G, Bassagasteguy L, Carrau RL,
Mataza JC, Kassam A, Snyderman CH and Mintz A: A novel
reconstructive technique after endoscopic expanded endonasal
approaches: Vascular pedicle nasoseptal flap. Laryngoscope.
116:1882–1886. 2006.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Kassam AB, Thomas A, Carrau RL, Snyderman
CH, Vescan A, Prevedello D, Mintz A and Gardner P: Endoscopic
reconstruction of the cranial base using a pedicled nasoseptal
flap. Neurosurgery. 63 (1 Suppl 1):ONS44–ONS53. 2008.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Gao Y, Zhong C, Wang Y, Xu S, Guo Y, Dai
C, Zheng Y, Wang Y, Luo Q and Jiang J: Endoscopic versus
microscopic transsphenoidal pituitary adenoma surgery: A
meta-analysis. World J Surg Oncol. 12(94)2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Li A, Liu W, Cao P, Zheng Y, Bu Z and Zhou
T: Endoscopic versus microscopic transsphenoidal surgery in the
treatment of pituitary adenoma: A systematic review and
meta-analysis. World Neurosurg. 101:236–246. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Yao D, Chen S and Wang X: Efficacy of
different minimally invasive surgical methods for transsphenoidal
resection of the pituitary adenoma: A systematic review and
meta-analysis. Asian J Surg. 45:2869–2871. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Chen J, Liu H, Man S, Liu G, Li Q, Zuo Q,
Huo L, Li W and Deng W: Endoscopic vs microscopic transsphenoidal
surgery for the treatment of pituitary adenoma: A meta-analysis.
Front Surg. 8(806855)2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Rotenberg B, Tam S, Ryu WHA and Duggal N:
Microscopic versus endoscopic pituitary surgery: A systematic
review. Laryngoscope. 120:1292–1297. 2010.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Jho HD and Carrau RL: Endoscopic endonasal
transsphenoidal surgery: Experience with 50 patients. J Neurosurg.
87:44–51. 1997.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Jho HD, Carrau RL, Ko Y and Daly MA:
Endoscopic pituitary surgery: An early experience. Surg Neurol.
47:213–223. 1997.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Jain AK, Gupta AK, Pathak A, Bhansali A
and Bapuraj JR: Excision of pituitary adenomas: Randomized
comparison of surgical modalities. Br J Neurosurg. 21:328–331.
2007.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Strychowsky J, Nayan S, Reddy K,
Farrokhyar F and Sommer D: Purely endoscopic transsphenoidal
surgery versus traditional microsurgery for resection of pituitary
adenomas: Systematic review. J Otolaryngol Head Neck Surg.
40:175–185. 2011.PubMed/NCBI
|
|
26
|
Goudakos JK, Markou KD and Georgalas C:
Endoscopic versus microscopic trans-sphenoidal pituitary surgery: A
systematic review and meta-analysis. Clin Otolaryngol. 36:212–220.
2011.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Guo S, Wang Z, Kang X, Xin W and Li X: A
meta-analysis of endoscopic vs microscopic transsphenoidal surgery
for non-functioning and functioning pituitary adenomas: Comparisons
of efficacy and safety. Front Neurol. 12(614382)2021.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Messerer M, De Battista JC, Raverot G,
Kassis S, Dubourg J, Lapras V, Trouillas J, Perrin G and Jouanneau
E: Evidence of improved surgical outcome following endoscopy for
nonfunctioning pituitary adenoma removal. Neurosurg Focus.
30(E11)2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Razak AA, Horridge M, Connolly DJ, Warren
DJ, Mirza S, Muraleedharan V and Sinha S: Comparison of endoscopic
and microscopic trans-sphenoidal pituitary surgery: Early results
in a single centre. Br J Neurosurg. 27:40–43. 2013.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Levi V, Bertani GA, Guastella C, Pignataro
L, Zavanone ML, Rampini PM, Caroli MA, Sala E, Malchiodi E,
Mantovani G, et al: Microscopic versus endoscopic transsphenoidal
surgery for pituitary adenoma: Analysis of surgical safety in 221
consecutive patients. Clin Otolaryngol. 42:466–469. 2017.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ammirati M, Wei L and Ciric I: Short-term
outcome of endoscopic versus microscopic pituitary adenoma surgery:
A systematic review and meta-analysis. J Neurol Neurosurg
Psychiatry. 84:843–849. 2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Gao Y, Zheng H, Xu S, Zheng Y, Wang Y,
Jiang J and Zhong C: Endoscopic versus microscopic approach in
pituitary surgery. J Craniofac Surg. 27:e157–e159. 2016.PubMed/NCBI View Article : Google Scholar
|
|
33
|
O'Malley BW Jr, Grady MS, Gabel BC, Cohen
MA, Heuer GG, Pisapia J, Bohman LE and Leibowitz JM: Comparison of
endoscopic and microscopic removal of pituitary adenomas:
Single-surgeon experience and the learning curve. Neurosurg Focus.
25(E10)2008.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Castaño-Leon AM, Paredes I, Munarriz PM,
Jiménez-Roldán L, Hilario A, Calatayud M, Hernandez-Lain A, Garcia
E, Garcia A, Lagares A and Alén JF: Endoscopic transnasal
trans-sphenoidal approach for pituitary adenomas: A comparison to
the microscopic approach cohort by propensity score analysis.
Neurosurgery. 86:348–356. 2020.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Cho DY and Liau WR: Comparison of
endonasal endoscopic surgery and sublabial microsurgery for
prolactinomas. Surg Neurol. 58:371–376. 2002.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Neal JG, Patel SJ, Kulbersh JS, Osguthorpe
JD and Schlosser RJ: Comparison of techniques for transsphenoidal
pituitary surgery. Am J Rhinol. 21:203–206. 2007.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Graham SM, Iseli TA, Karnell LH, Clinger
JD, Hitchon PW and Greenlee JDW: Endoscopic approach for pituitary
surgery improves rhinologic outcomes. Ann Otol Rhinol Laryngol.
118:630–635. 2009.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Duz B, Harman F, Secer HI, Bolu E and
Gonul E: Transsphenoidal approaches to the pituitary: A progression
in experience in a single centre. Acta Neurochir (Wien).
150:1133–1139. 2008.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Ciric I, Ragin A, Baumgartner C and Pierce
D: Complications of transsphenoidal surgery: Results of a national
survey, review of the literature, and personal experience.
Neurosurgery. 40:225–237. 1997.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Lofrese G, Vigo V, Rigante M, Grieco DL,
Maresca M, Anile C, Mangiola A and De Bonis P: Learning curve of
endoscopic pituitary surgery: Experience of a neurosurgery/ENT
collaboration. J Clin Neurosci. 47:299–303. 2018.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Zaidi HA, Awad AW, Bohl MA, Chapple K,
Knecht L, Jahnke H, White WL and Little AS: Comparison of outcomes
between a less experienced surgeon using a fully endoscopic
technique and a very experienced surgeon using a microscopic
transsphenoidal technique for pituitary adenoma. J Neurosurg.
124:596–604. 2016.PubMed/NCBI View Article : Google Scholar
|