Introduction
Arteriovenous malformations (AVMs) are vascular
system anomalies considered to develop during embryogenesis, fetal
development, or shortly after birth (1). AVMs are characterized by the tangling
of arteries and veins without the presence of capillaries. This
leads to the rapid and high-pressure blood flow through these
abnormal vessels, hindering the delivery of arterial blood to the
tissues. As a result, varying degrees of ischemia occur (1). AVMs are the most challenging vascular
anomalies to manage and are frequently associated with morbidity
and mortality (2). They arise due to
developmental changes in blood vessel formation, exhibit
proportional growth alongside the child's development, and are
identified by the presence of enlarged feeding vessels, excessive
arteriovenous connections at the nidus level, and high vascularity.
While some AVMs may not present any symptoms, others can manifest
as increased size, bleeding, pain, or conditions such as
azoospermia, infertility, heart failure, and potentially
life-threatening hemorrhages (3,4). Their
most common locations are the neck, trunks, extremities, and
extracranial and intracranial areas (3). The involvement of intra-scrotal
components is extremely rare, generally manifesting as para-or
intra-testicular masses (1). The
para-testicular area contains a variety of structures, including
the tunica vaginalis, lymphatic channels, ductus deferens,
epididymis, vessels, spermatic cord, and other testicular
suppurative tissues (5). AVMs from
these structures are very rare, with only a limited number of cases
of the spermatic cord or scrotal wall reported in the literature
(1,4).
The present study reports an extremely rare case of
para-testicular AVM without the involvement of the epididymis or
spermatic cord.
Case report
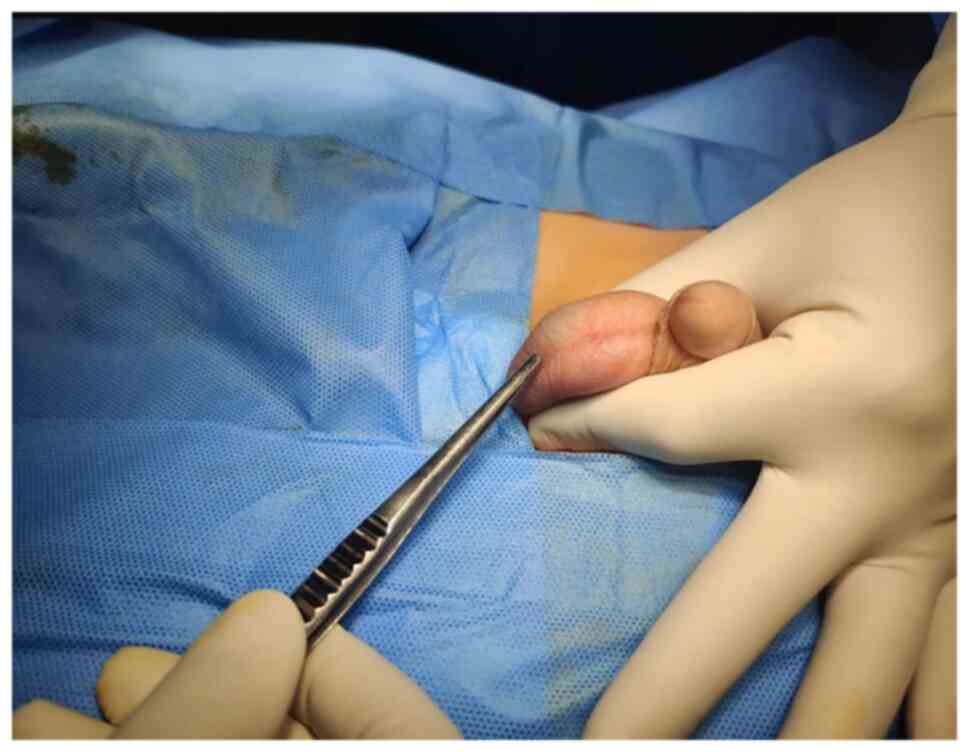
A 6-year-old boy presented with a painless swelling
on the right side of the scrotum that his parents had observed for
6 months. There was no history of surgery or trauma. Upon an
examination, a blush-colored, non-tender, immobile, and
non-pulsatile cystic swelling was observed in the right
hemi-scrotum below the testis (Fig.
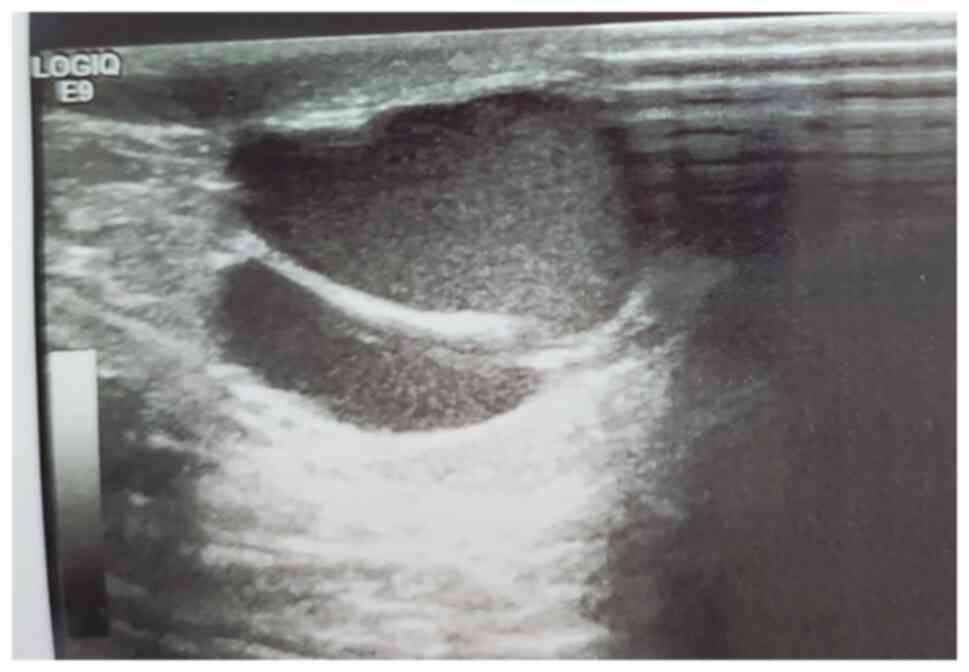
1). A scrotal Doppler ultrasound (U/S) revealed a separate
20x12 mm bilocular cystic lesion below the right testis with a
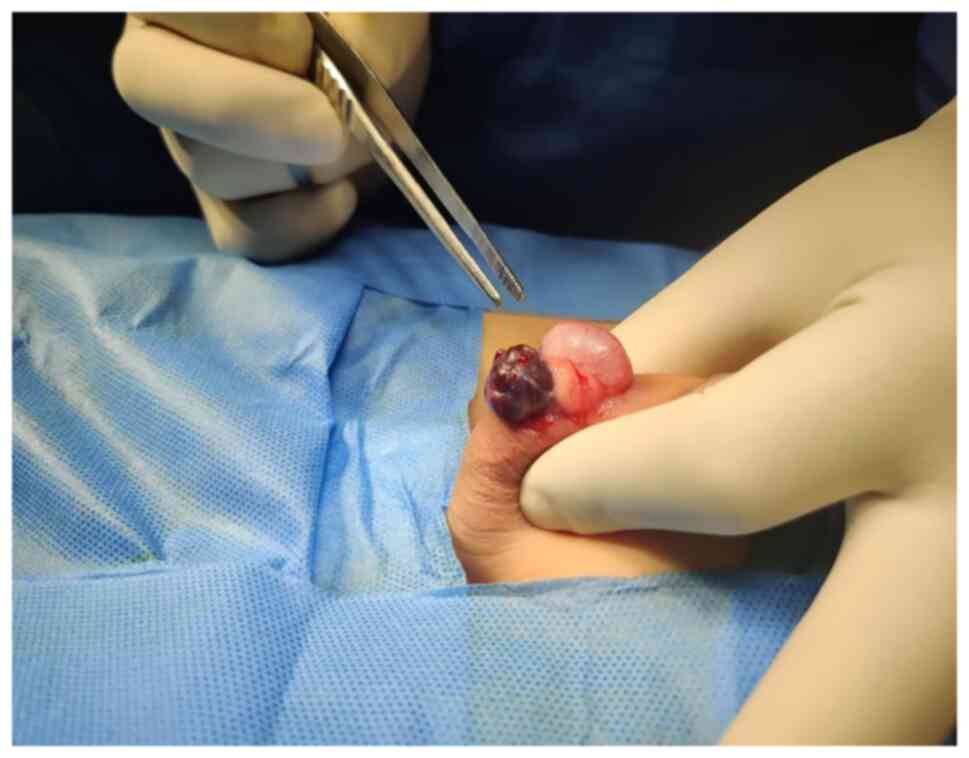
normal texture, and the vascularity of both testes (Fig. 2). Under general anesthesia, via a
small scrotal incision, the surgery was performed. A cystic,
blood-filled mass was found and excised (Fig. 3). Intraoperatively, there were no
complications. The patient was discharged the same day, and his
post-operative period was uneventful. A histopathological
examination was performed under the following conditions: The
sections (5 µm-thick) were paraffin-embedded and fixed with 10%
neutral-buffered formalin at room temperature for 24 h. The
sections were then stained with hematoxylin and eosin (Bio Optica
Co.) for 1-2 min at room temperature and examined under a light
microscope (Leica Microsystems GmbH). Histopathological
examinations also revealed fibrofatty tissue fragments with
irregular different-sized branching vascular spaces lined by
endothelial cells (Fig. 4). The
result was consistent with a vascular malformation.
Discussion
Scrotal swelling is a relatively frequent medical
condition. Space-occupying lesions from these sites may be
neoplastic or non-neoplastic (3).
Neoplastic lesions can be benign or cancerous. Non-neoplastic
masses include inflammation, epididymal cysts, spermatic cord
cysts, spermatoceles, hydroceles, pyoceles, and hernia (5-7).
Approximately 5% of all intra-scrotal masses are para-testicular
neoplasms and the epididymis accounts for 20-30% of these (8). The spermatic cord is responsible for
70% of all lesions, with lipomas being the most common. The most
frequent epididymis tumors are adenomatoid tumors, followed by
leiomyomas. Other benign tumors include fibroma, neurofibroma,
hemangioma, and papillary cystadenoma (7).
Although vascular lesions, such as varicocele,
hemangioma, lymphangioma, and AVMs are possible, they are uncommon
and are rarely described in the medical literature (9). Adult males frequently develop benign
vascular lesions. Varicoceles are the most frequent lesion, whereas
AVMs are the rarest (3). Vascular
malformations are collections of aberrant vessels detected at birth
in 90% of cases (10). These lesions
develop alongside the infant and exhibit no signs of endothelial
growth (10). AVM is well-known due
to its presence in the central nervous system, although it can be
present everywhere (1). The
spermatic cord and scrotal wall are the most commonly reported
sites for scrotal or intra-scrotal AVMs (1,5,11-13).
AVMs of the spermatic cord are benign lesions comprised of
complicated tangles of swollen, dilated arteries and veins with no
intervening capillaries (1). In this
case, the para-testicular AVM is independent and unattached to the
surrounding structure (spermatic cord or epididymis).
Mulliken and Glowacki (14) categorized vascular abnormalities as
vascular tumors (infantile hemangioma, kaposiform
hemangioendothelioma, congenital hemangioma, and tufted angioma)
and vascular malformations (AVM, lymphatic malformation, venous
malformation, and capillary malformation). In the medical
literature, a number of vascular malformations were incorrectly
referred to as hemangiomas, and numerous patients have undergone
inappropriate therapy due to this misclassification (15). The majority of patients are
asymptomatic and present with a slow-growing, non-tender mass. A
rapidly expanding, non-tender mass is rarely reported by some
patients (7). Upon examination, they
appear as masses with dilated vessels overlying them and a thrill
(16). However, Kang et al
(17) reported a case of
para-testicular AVM with a painful gradual enlargement of the left
hemiscrotum. The case presented herein exhibited scrotal swelling
for 6 months without any pain or tenderness. Upon examination, it
appeared as a blushing mass under the skin. There was no thrill on
palpation. Pre-operatively, it was suspected to be a
hemangioma.
U/S is the preferred initial examination, since it
is readily available, inexpensive, and is associated with excellent
sensitivity and specificity. It is used to determine whether a
lesion is benign or malignant, delineates borders, and defines
echogenicity, vascularity, invasive behavior, and neighboring
tissues. If a U/S indicates a well-bordered, isolated, homogeneous,
non-invasive lesion, the use of contrast-enhanced computed
tomography or magnetic resonance imaging (MRI) may be limited. If
the results of the U/S are ambiguous or dubious, further
radiography can be conducted using computed tomography or MRI, and
tumor markers for testicular cancer can be sent for assessment
(18). A U/S can distinguish between
intratesticular and extra-testicular lesions, as well as solid and
cystic lesions, with 90-100% accuracy. This difference is critical
as the majority of para-testicular masses are benign, whereas the
majority of testicular masses are cancerous (19). A U/S usually reveals a network of
numerous vascular channels, which may resemble a varicocele
(16). As embolization may be
performed concurrently, angiography is the gold standard for
evaluating arteriovenous malformations (20). The U/S of the case in the present
study revealed a separate bilocular cystic lesion below the right
testis with normal texture and vascularity of both testes.
The preferred therapeutic options for AVMs are
sclerotherapy, embolization, and surgical excision (4). Sclerotherapy reduces the size of the
venous nidus prior to surgical excision, and embolization eases the
resection process with the least amount of bleeding (13). Finally, surgery is the only effective
and approved therapy (13). Some
consequences may occur as abnormalities are often long and poorly
defined. There is a risk of acute bleeding, and poor procedure care
may result in impotence and infertility (10,13). The
case described herein underwent surgical resection. There were no
intraoperative complications.
In conclusion, para-testicular AVMs are a very rare
condition. Based on this case, the authors suggest that AVM should
be included in the differential diagnosis of para-testicular
lesions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and material
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
RB and IA were the clinicians that managed the case
presented herein. MNH and FHK were involved in the literature
review, in the writing of the manuscript, as well as in the
analysis and interpretation of the patient's data. SJH, HMH and
KMS, were involved in the literature review and in the design of
the study, as well as in the revision of the manuscript and in the
processing of the figures. AAMA was the radiologist who performed
the assessment. AMA was the pathologist examining the specimen, and
was a major contributor to the conception of the study, and in
revising the manuscript. All authors have read and approved the
final manuscript. RB and FHK confirm the authenticity of all the
raw data.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient's parent for the inclusion of his data in the present
study.
Patient consent for publication
Written informed consent was obtained from the
patient's parent for the publication of his data and any related
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Sountoulides P, Bantis A, Asouhidou I and
Aggelonidou H: Arteriovenous malformation of the spermatic cord as
the cause of acute scrotal pain: A case report. J Med Case Rep.
1(110)2007.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Lekwuttikarn R, Lim YH, Admani S, Choate
KA and Teng JM: Genotype-guided medical treatment of an
arteriovenous malformation in a child. JAMA Dermatol. 155:256–257.
2019.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Mohammad A, Sahyouni W, Almeree T and
Alsaid B: Angioembolization of scrotal arteriovenous malformations:
A case report and literature review. Case Rep Vasc Med.
2020(8373816)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Guerrero Avendaño GML, Enríquez García R,
Saldívar Rodea CA, Sierra Juárez MÁ and Sotelo Cuéllar JS: Scrotal
arteriovenous malformation: Case report. Radiol Case Rep.
17:1266–1270. 2022.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Secil M, Bertolotto M, Rocher L, Pekindil
G, Stocca T, Richenberg J, Ramchandani P and Derchi LE: European
Society of Urogenital Radiology Scrotal Imaging Subcommittee.
Imaging features of paratesticular masses. J Ultrasound Med.
36:1487–1509. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Priemer DS, Trevino K, Chen S, Ulbright TM
and Idrees MT: Paratesticular soft-tissue masses in orchiectomy
specimens: A 17-year survey of primary and incidental cases from
one institution. Int J Surg Pathol. 25:480–487. 2017.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Akbar SA, Sayyed TA, Jafri SZ, Hasteh F
and Neill JS: Multimodality imaging of paratesticular neoplasms and
their rare mimics. Radiographics. 23:1461–1476. 2003.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Abdullah and Xing J: Adenomatoid
tumor of epididymis-A case report. Urol Case Rep.
28(101022)2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Jaganathan S, Gamanagatti S, Mukund A and
Dhar A: Bleeding scrotal vascular lesions: Interventional
management with transcatheter embolization. Cardiovasc Intervent
Radiol. 34 (Suppl 2):S113–S116. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Konus ÖL, Ilgit ET, Yücel C, Özbek E and
Önal B: Scrotal arteriovenous malformation and its preoperative
embolization. Eur Radiol. 9:425–427. 1999.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Joshi MA, Gadhire M, Dhake A and Patil M:
A diagnostic dilemma: Arteriovenous malformation of spermatic cord
presenting as irreducible inguinal swelling. J Postgrad Med.
57:339–340. 2011.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Guz BV, Ziegelbaum M and ontes JE:
Arteriovenous malformation of spermatic cord. Urology. 33:427–428.
1989.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zachariah JR, Gupta AK and Lamba S:
Arteriovenous malformation of the scrotum: Is preoperative
angioembolization a necessity? Indian J Urol. 28:329–334.
2012.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Mulliken JB and Glowacki J: Hemangiomas
and vascular malformations in infants and children: A
classification based on endothelial characteristics. Plast Reconstr
Surg. 69:412–422. 1982.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Fernandez-Pineda I and Parida L:
Testicular haemangiomas and vascular malformations. Lancet Oncol.
11(814)2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Yilmaz C and Arslan M and Arslan M:
Intrascrotal arteriovenous malformation simulating varicocele. AJR
Am J Roentgenol. 192(W351)2009.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kang TW, Choi YD, Jeong YY, Kwon DD, Park
K, Ryu SB and Park YI: Intrascrotal extratesticular arteriovenous
malformation. Urology. 64(590)2004.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Dighe SP, Shinde RK, Shinde SJ and
Raghuwanshi PS: The dilemma in the diagnosis of paratesticular
lesions. Cureus. 14(e22783)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
McCracken JM, MacNeily AE, Mueller D and
Magee F: Ultrasound features of a paratesticular arteriovenous
malformation: A case report of an 11-year-old boy. Pediatr Radiol.
35:532–534. 2005.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Annam A, Munden MM, Mehollin-Ray AR,
Schady D and Browne LP: Extratesticular masses in children: Taking
ultrasound beyond paratesticular rhabdomyosarcoma. Pediatr Radiol.
45:1382–1391. 2015.PubMed/NCBI View Article : Google Scholar
|