Introduction
Alveolar adenoma (AA) is an exceedingly rare benign
lung tumor that was first reported by Yousem et al in
1986(1). Patients with AA are
usually asymptomatic and the tumor is incidentally detected on
chest radiography as a clear solitary pulmonary nodule. When solid
pulmonary nodules are >10 mm in size, there is an increased
likelihood of surgical intervention due to a higher risk of
malignancy and patient anxiety (2,3). A
definitive diagnosis of AA depends on histopathology and
immunohistochemistry findings as it is difficult to diagnose
pre-operatively. Curative treatment consists of surgical resection,
with no case of recurrence having been described to date in the
literature, at least to the best of our knowledge.
The present study describes the case of a patient
with alveolar adenoma and reports on the imaging and pathological
differentiation of AA from other lung tumors.
Case report
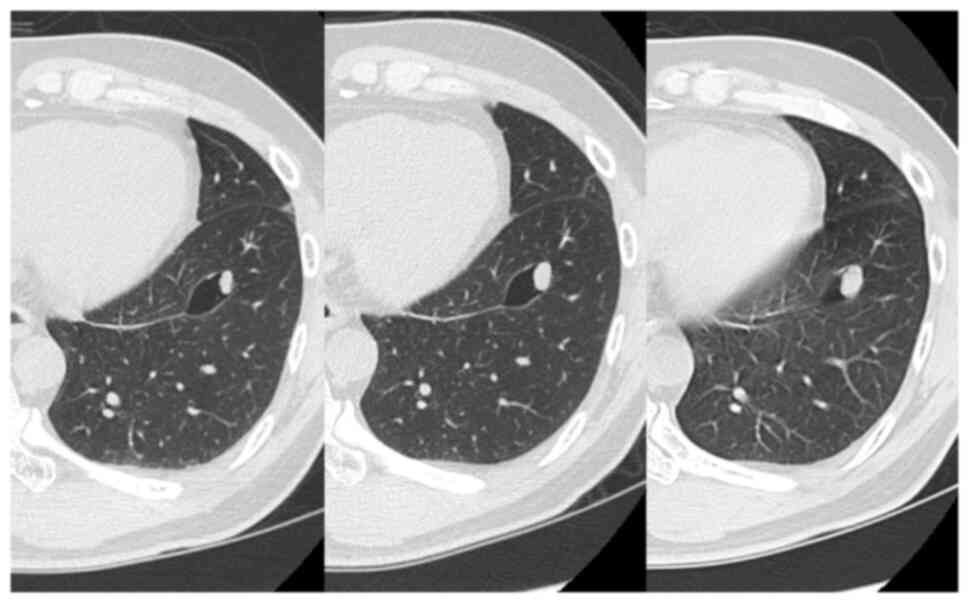
A 50-year-old male patient presented to his previous
doctor with a complaint of chest discomfort. A chest computed
tomography (CT) scan revealed a 10-mm solitary nodule with a single
cyst in the left lower lobe. The diameter of the pulmonary nodule
increased to 14 mm within a span of 2 years (CT scan results shown
in Fig. 1). He was referred to
Kansai Medical University Hospital (Hirakata, Japan) due to the
possibility of lung cancer. His medical history was notable for
benign prostatic hyperplasia. A thoracoscopic wedge resection of
the left lower lung was performed. The frozen sections were
non-diagnostic, and the surgical procedure and postoperative course
were uneventful, with no signs of recurrence 4 years
post-operatively.
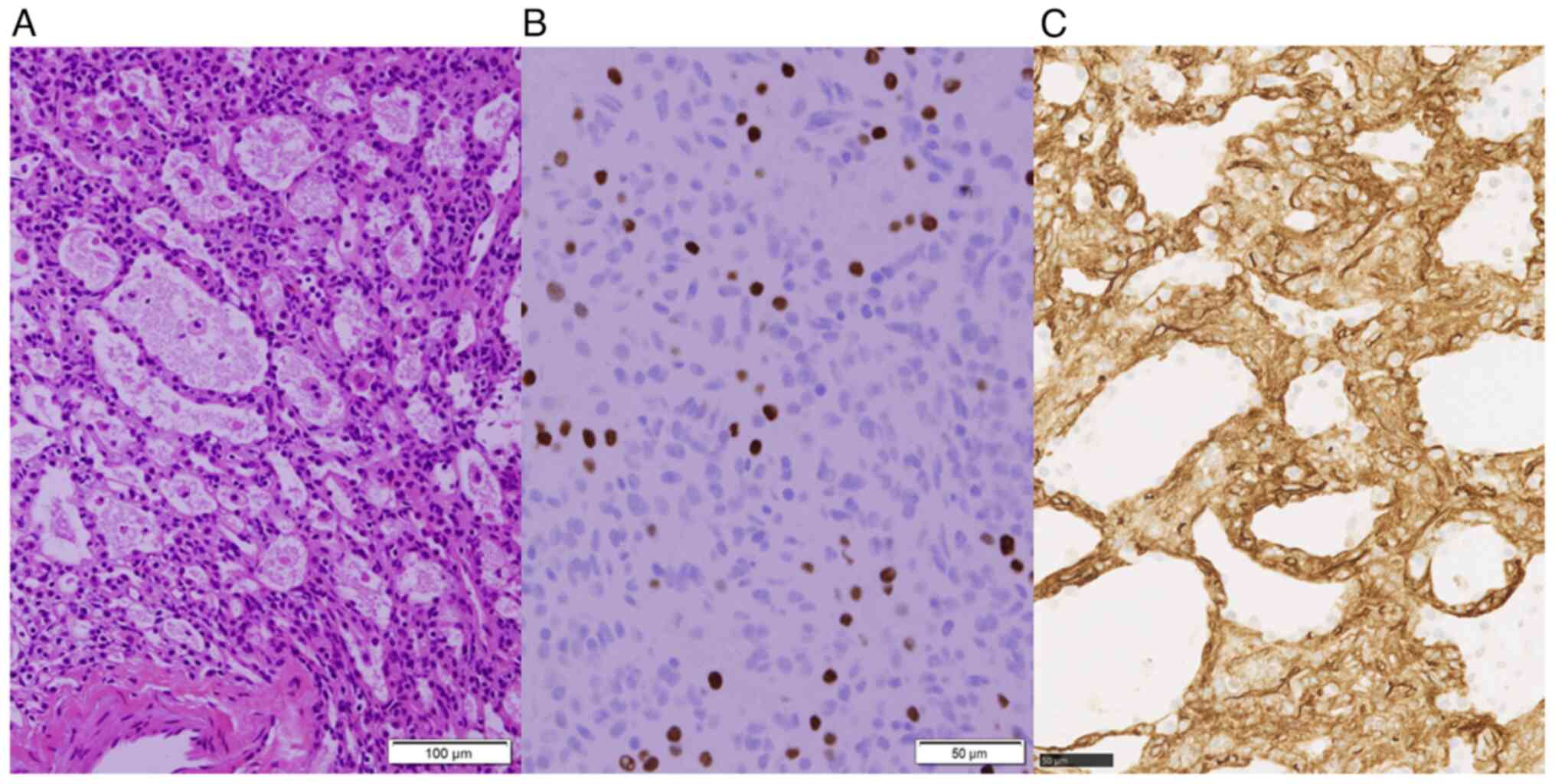
Overall, the tumor was well-defined and yellowish,
measuring 10 mm in a subpleural cyst. Microscopically, the tumor
consisted of polycystic structures resembling alveoli filled with
pulmonary surfactant. The cyst lining cells were positive for
thyroid transcription factor-1 (TTF-1) without atypia,
corresponding to type II pneumocytes (Fig. 2). Additionally, the stroma lacked
elastic fibers characteristic of alveoli and contained cluster of
differentiation 34 (CD34)-positive cells with rounded nuclei and
eosinophilic cytoplasm. These cells were negative for TTF-1, CD31,
ERG, D2-40, SALL4, BRAF and STAT6. Immunohistochemical analysis was
conducted on 4-µm-thick formalin-fixed paraffin-embedded tissue
sections (details presented in Table
I). Cultures were negative for fungi and tuberculosis, and no
malignant cells were noted. Analyses were performed under a light
microscope (Olympus Corporation) and whole slide images. Therefore,
the final pathological diagnosis was that of AA.
 | Table IAntibodies used in the present case
report. |
Table I
Antibodies used in the present case
report.
| Antibody | Clone, cat. no.,
supplier | Dilution | Incubation | Reaction time | Fully automated IHC
system, supplier | Detection system | Antigen retrieval
reagent |
|---|
| TTF-1 | 8G7G3/1, cat. no.
IR056, Dako; Agilent Technologies, Inc. | RTU | Low pH: 20 min; room
temperature | 20 min | Autostainer Link 48,
Agilent Technologies, Inc. | Envision FLEX | Envision FLEX Target
Retrieval Solution High/Low pH |
| CD31 | JC70A, cat. no.
IR610, Dako; Agilent Technologies, Inc. | RTU | High pH: 20 min; room
temperature | 20 min | | | |
| D2-40 | D2-40, cat. no.
IR072, Dako; Agilent Technologies, Inc. | RTU | High pH: 20 min; room
temperature | 3 min | | | |
| ERG | Cat. no. 418111,
Nichirei Biosciences, Inc. | RTU | CC1: 32 min 36˚C | 8 min | VENTANA BenchMark
ULTRA PLUS, Roche Diagnostics | Optiview DAB
universal kit | CC1: VENTANA ULTRA
Cell Conditioning Solution |
| SALL4 | 6E3, cat. no.
H00057167-M03, Abnova | x500 | CC1: 32 min 36˚C | 16 min | | | |
| BRAFV600E | VE1, cat. no.
790-4855, Roche Diagnostics | RTU | CC1: 64 min 36˚C | 32 min | | | |
| STAT6 | YE361, cat. no.
ab32520, Abcam | x1,000 | CC1: 32 min 36˚C | 16 min | | | |
Discussion
AA is a rare lung tumor with an incidence rate of
<1% of all lung tumors, and is classified as an adenoma in the
2015 World Health Organization Classification of lung tumors
(4). AA is often asymptomatic and is
incidentally detected during imaging examinations, typically
exhibiting no tendency to enlarge (5). The majority of patients are middle-aged
to elderly, with a slight predominance in the female sex. There is
no association between the occurrence of AA and a previous medical
history or family history. AA commonly occurs in the middle and
lower lobes of the lung and is pathologically characterized by
multifocal cystic lesions resembling alveolar cavities, with the
lumen lined by TTF-1-positive type II alveolar epithelium (6). In the present study, upon an
examination of the patient, it was found that the tumor had similar
histopathological features to the cases reported in the literature
(6-11).
AAs are characterized by the presence of vacuoles
within or around the tumor on imaging (7). It is speculated that alveoli rupture
and fuse to create cavities, similar to the cavity formation
mechanism observed in lung cancer. This occurs as tumor cells
develop toward the bronchiole, forming a unidirectional check-valve
system, which results in the accumulation of gas in the alveoli.
This phenomenon may explain the cystic lesions observed in the
pathology. Therefore, it is important to consider AA as a
differential diagnosis in cases of pulmonary nodules with air
images. In the case presented herein, the tumor increased in size
with the presence of air images, highlighting the necessity to
distinguish the tumor from lung cancer or pulmonary
aspergilloma.
The diagnosis of AA is challenging when based on
small biopsy tissue or frozen sections as it can resemble normal
lung parenchyma or mimic malignancy with small glandular spaces
lined by regular glandular epithelium (8). Additionally, there are other conditions
in the differential diagnosis of AA, including papillary adenoma,
sclerosing pneumocytoma and pulmonary hamartoma. Papillary adenoma
is characterized by distinctive papillae covered by uniform
cuboidal to columnar cells and a heterogeneous epithelial
component. The presence of TTF-1 expression in AA can help
distinguish it from sclerosing pneumocytoma. Pulmonary hamartoma
consists primarily of benign cartilage mixed with a fibrovascular
stroma and scattered bronchial glands (9).
The curative treatment for AA is surgical resection,
typically performed to rule out malignancy and confirm the
diagnosis through postoperative pathology. No recurrence has been
reported following complete resection (10). In the case described herein, surgery
was concluded with a wedge resection as the tumor was a peripheral
lesion that could be completely resected, and the frozen section
did not provide a definitive diagnosis. There is a risk of
unnecessary extended resection, such as segmentectomy or lobectomy,
if the patient is intraoperatively misdiagnosed with lung cancer
based in the frozen section; hence, wedge resection is a viable
option for small peripheral lesions (11).
In conclusion, AA is a rare, benign lung tumor. When
encountering a well-defined solitary nodule with cystic spaces in
the peripheral lung, an intraoperative diagnosis can be
challenging. Therefore, it is critical to consider the possibility
of AA, complete the surgery with a wedge resection and await the
final pathological diagnosis.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
HM was a major contributor to the conception of the
study, as well as to the literature search for related studies. TU,
NM, YT, TS and HH were involved in the literature review, and in
the examination and interpretation of the patient's data. HM, KI,
KT and TM were involved in the literature review, in the design of
the study, in the critical revision of the manuscript and in the
processing of the figures. KI and KT were the pathologists who
performed the histopathological diagnosis of the patient. HM and TM
confirm the authenticity of all the raw data. All authors have read
and approved the final manuscript.
Ethics approval and consent to
participate
The patient provided written informed consent for
participation.
Patient consent for publication
Written consent was obtained from the patient for
the publication of his data and any related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Yousem SA and Hochholzer L: Alveolar
adenoma. Hum Pathol. 17:1066–1071. 1986.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Klaveren RJ, Oudkerk M, Prokop M, Scholten
ET, Nackaerts K, Vernhout R, Iersel CA, Bergh KAM, Westeinde SV,
Aalst C, et al: Management of lung nodules detected by volume CT
scanning. N Engl J Med. 361:2221–2229. 2009.PubMed/NCBI View Article : Google Scholar
|
|
3
|
MacMahon H, Naidich DP, Goo JM, Lee KS,
Leung ANC, Mayo JR, Mehta AC, Ohno Y, Powell CA, Prokop M, et al:
Guidelines for management of incidental pulmonary nodules detected
on CT Images: From the fleischner society 2017. Radiology.
284:228–243. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Travis WD, Brambilla E, Burke AP, Marx A
and Nicholson AG: Introduction to the 2015 World Health
Organization classification of tumors of the lung, pleura, thymus,
and heart. J Thorac Oncol. 10:1240–1242. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Bhavsar T, Uppal G, Travaline JM, Gaughan
C, Huang Y and Khurana JS: An unusual case of a microscopic
alveolar adenoma coexisting with lung carcinoma: A case report and
review of the literature. J Med Case Rep. 5(187)2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Sak SD, Koseoglu RD, Demirag F, Akbulut H
and Gungor A: Alveolar adenoma of the lung. Immunohistochemical and
flow cytometric characteristics of two new cases and a review of
the literature. APMIS. 115:1443–1449. 2007.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Hsieh MS, Tseng YH, Hua SF and Chou YH:
Cystic alveolar adenoma: An unusual clinical presentation of a rare
lung neoplasm. Pathology. 47:78–80. 2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Burke LM, Rush WI, Khoor A, Mackay B,
Oliveira P, Whitsett JA, Singh G, Turnicky R, Fleming MV, Koss MN
and Travis WD: Alveolar adenoma: A histochemical,
immunohistochemical, and ultrastructural analysis of 17 cases. Hum
Pathol. 30:158–1567. 1999.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Wang L, Wang X, Rustam A and Hu J:
Alveolar adenoma resected by thoracoscopic surgery. Ann Thorac
Cardiovasc Surg. 19:489–491. 2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kondo N, Torii I, Hashimoto M, Takuwa T,
Tanaka F, Tsujimura T and Hasegawa S: Alveolar adenoma of the lung:
A case report. Ann Thorac Cardiovasc Surg. 17:71–73.
2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Saji H, Okada M, Tsuboi M, Nakajima R,
Suzuki K, Aokage K, Aoki T, Okami J, Yoshino I, Ito H, et al:
Segmentectomy versus lobectomy in small-sized peripheral
non-small-cell lung cancer (JCOG0802/WJOG4607L): A multicentre,
open-label, phase 3, randomised, controlled, non-inferiority trial.
Lancet. 399:1607–1617. 2022.PubMed/NCBI View Article : Google Scholar
|