Introduction
Distal radius fractures are among the most common
fractures encountered in clinical practice (1,2).
Conservative treatment is the main treatment, especially in elderly
patients (about 70-85% of patients) (3,4). On the
other hand, for the purpose of immediate return to activity and
daily activities, young patients often opt for volar locking plate
(VLP) fixation (5,6). VLP fixation improves stability in the
short term (7). VLP fixation has
recently gained widespread application in the elderly population
(5).
The functional evaluation of the wrist joint is
widely used to assess the effectiveness of distal radius fracture
treatment. This evaluation typically encompasses objective outcomes
and patient-reported outcomes, which are interconnected (8). Patient-reported outcomes are used to
evaluate patient pain and directly reflect quality of life
(8). The quick disabilities of the
arm, shoulder and hand (Q-DASH) score, a widely used
patient-reported outcome score of the upper extremity, has been
reported to be an indicator of return to activity (9).
An advantage of VLP fixation is the immediate return
to activity. However, some patients are unable to return to
activity immediately following surgery due to complications
associated with VLP fixation, such as infection, tendon injury and
screw puncture. Moreover, there have been reports of cases of poor
patient-reported outcomes due to pain, swelling and contractures
despite the absence of complications associated with VLP fixation
(10-12).
It is thus critical to identify the factors associated with poor
early post-operative patient-reported outcomes in VLP fixation in
order to achieve immediate return to activity.
The present study compared post-operative outcomes
using the Q-DASH score in the very early post-operative period (1
month following VLP fixation). The present study aimed to identify
clinical findings associated with poor outcomes.
Patients and methods
Patients
The present study was approved by the Ethics
Committee for Medical Research of Juntendo University (Tokyo,
Japan; No. E22-0447; date of approval: September 21, 2023).
Informed consent was obtained both for participation and
publication in the form of opt-out on the web-site, and those who
rejected were excluded. The present study was a retrospective
study. The patients were subjected to standard clinical practice,
including the methods of anesthesia and surgery.
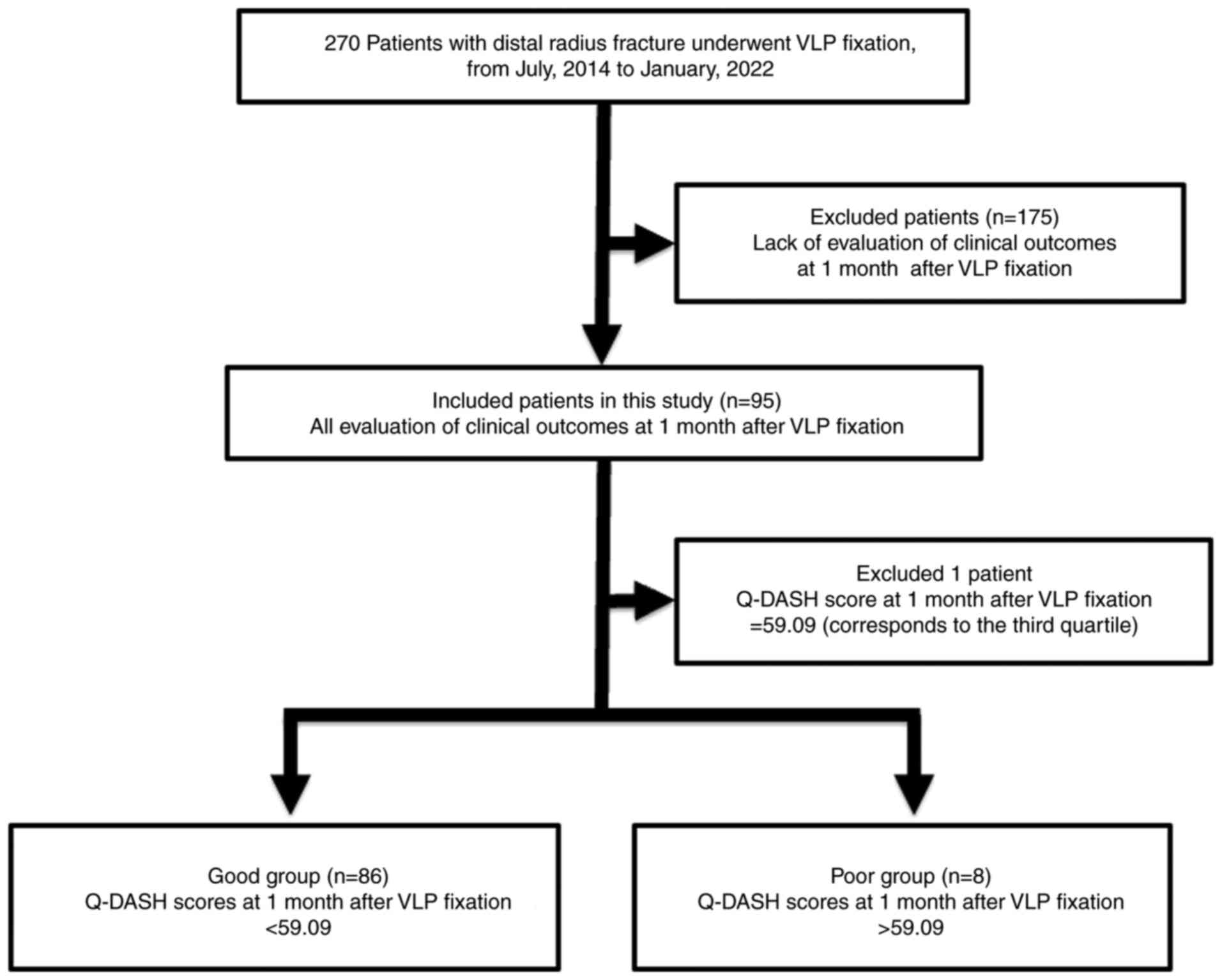
From July, 2014 to January, 2022, 270 patients with
distal radius fracture underwent VLP fixation at Juntendo
University Hospital. In the present study, 95 patients (23 males
and 72 females; mean age, 61.9±14.7 years; range, 22-87 years) with
all evaluation items recorded at 1 month post-operatively were
included (Fig. 1). The fracture type
was defined according to the Arbeitsgemeinschaft für
Osteosynthesefragen (AO) classification: Type A (n=18 patients),
type B (n=5 patients) and type C (n=72 patients). There were no
complications associated with VLP fixation at 1 month following
surgery.
Division into groups
The Q-DASH score at 1 month following VLP fixation
was used as an index of return to activity. A total of 95 patients
were divided into groups based on the Q-DASH score for the analysis
of factors associated with immediate return to activity. At 1 month
after surgery, the mean Q-DASH score was 32.7±18.7 (range,
4.55-84.09). The patients were divided according to the Q-DASH
score into good (good score and outcome) and poor (poor score and
outcome) groups according to quartiles (median, 40.91; first
quartile, 22.73; third quartile, 59.09). The good group consisted
of 86 patients with Q-DASH scores <59.09 (mean, 28.6±14.3;
range, 4.55-54.55). The poor group consisted of 8 patients with
Q-DASH scores >59.09 (mean, 73.0±6.2; range, 65.91-84.09). Of
note, 1 patient with a Q-DASH of score of 59.09 (44-year-old male,
AO classification type C) was omitted from the analysis (Fig. 1). As regards the treatment of
patients within the third quartile, cases in the third quartile may
be omitted from the analysis or included in the good or poor group.
Fritzsching et al (13) used
quartiles and omitted the third quartile in their analysis of the
prognosis of osteosarcoma when dividing the patients into good or
poor groups. According to that study, the statistical analysis was
also performed by omitting cases with a Q-DASH score of 59.09,
which corresponds to the third quartile, in the present study.
The background of the patients [the evaluation items
were as follows: Age, sex, height, weight, body mass index (BMI),
injury energy (high energy injury pertains to high energy trauma,
such as that sustained by a vehicle accident and falling from a
height; low energy injury pertains to low energy trauma, such as
that sustained by falling down), AO classification, and Q-DASH
score] were investigated and compared between the two groups
(Table I).
 | Table IComparison of the background of the
patients in the good and poor groups. |
Table I
Comparison of the background of the
patients in the good and poor groups.
| Characteristic | Good group
(n=86) | Poor group (n=8) | P-value |
|---|
| Age, years | 61.9±14.7 | 63.6±15.2 | 0.95 |
| Sex | | | |
|
Male | 22 | 0 | 0.19 |
|
Female | 64 | 8 | |
| Height (cm) | 158.2±14.7 | 153.0±8.0 | 0.33 |
| Weight (kg) | 58.6±10.1 | 50.5±8.2 | 0.03 |
| BMI
(kg/m2) | 22.9±2.9 | 21.6±3.3 | 0.22 |
| Injury
energya | | | |
|
High | 19 | 2 | NS |
|
Low | 67 | 6 | |
| AO
classification | | | |
|
Type A | 18 | 0 | <0.01 |
|
Type B | 5 | 0 | |
|
Type C | 63 | 8 | |
| Q-DASH score | 28.6±14.3 | 73.0±6.2 | <0.01 |
Evaluation
The duration from injury to surgery, the direction
of fracture dislocation and radiographic parameters [radial
inclination (RI), volar tilt (VT) and ulnar variance (UV)] at the
time of injury were examined. In addition, at 1 month following VLP
fixation, the radiographic parameters (RI, VT and UV), Q-DASH
score, wrist joint range of motion (flexion, extension, pronation
and supination), grip strength ratio and visual analog scale (VAS)
were examined.
Statistical analysis
Data were analyzed for significant differences
through two-group comparisons. Fisher's exact test was utilized for
assessing sex, injury energy, the direction of fracture dislocation
and AO classification, and the Mann-Whitney U test was used for
other endpoints. Factors influencing the poor group were
identified. Multivariate analysis (logistic regression analysis)
was performed to determine whether the factors were independently
associated with poor Q-DASH scores at 1 month post-operatively.
Given that the sample size of the study was 95 patients, with only
8 patients in the poor outcome group, two explanatory variables
were included in the logistic regression analysis. Data are
presented as the mean ± standard deviation. A value of P<0.05
was considered to indicate a statistically significant
difference.
Results
The age of the patients was 61.9±14.7 years in the
good group and 63.6±15.2 years in the poor group, with no
significant difference between the two groups (Mann-Whitney U test,
P=0.95). As regards sex, there were 22 males and 64 females in the
good group, and 8 females in the poor group, with no significant
difference between the two groups (Fisher's exact test, P=0.19).
Height was 158.2±14.7 cm in the good group and 153.0±8.0 cm in the
poor group, with no significant difference between the two groups
(Mann-Whitney U test, P=0.33). Body weight was 58.6±10.1 kg in the
good group and 50.5±8.2 kg in the poor group, indicating that the
patients in the poor group had a significantly lower weight than
those in the good group (Mann-Whitney U test, P=0.03). BMI was
22.9±2.9 g/m2 in the good group and 21.6±3.3
kg/m2 in the poor group, with no significant difference
between the two groups (Mann-Whitney U test, P=0.22). Injury energy
was high (vehicle accident and falling from a height) in 19 cases
and low (falling down) in 67 cases in the good group, and high in 2
cases and low in 6 cases in the poor group, with no significant
difference between the two groups (Fisher's exact test, not
significant). As regards the AO classification, in the good group,
18 patients were classified as type A, 5 patients were classified
as type B, and 63 patients were classified as type C; in the poor
group, the 8 patients were classified as type C; there was a
significantly greater number of type C fractures in the poor group
than in the good group (Fisher's exact test, P<0.01). The Q-DASH
score was 28.6±14.3 in the good group and 73.0±6.2 in the poor
group; this was significantly higher in the poor group than in the
good group (Mann-Whitney U test, P=0.22). These results revealed
that the poor group had a significantly lower body weight and more
patients were classified as AO type C than the good group. The
Q-DASH score was significantly lower in the good group than in the
poor group (Table I).
In the good group, the duration from injury to
surgery was 9.1±4.4 days, the direction of fracture dislocation was
volar in 32.6% of patients and dorsal in 67.4% of patients, the RI
was 13.5±9.4˚, VT was -6.5±20.3˚ and UV was 1.3±2.4 mm. In the poor
group, the duration from injury to surgery was 7.6±5.4 days, the
fracture dislocation direction was volar in 12.5% of patients and
dorsal in 87.5% of patients, the RI was 6.8±11.3˚, VT was
-23.8±20.1˚ and UV was 4.2±3.5 mm. At the time of injury, the VT
was significantly lower in the poor group (P=0.02) and UV was
significantly higher (P=0.01). There were no other significant
differences between the groups (Table
II). At 1 month following VLP fixation, in the good group, the
RI was 21.6±6.5˚, VT was 10.6±4.8˚ and UV was -0.3±1.5 mm; the
wrist range of motion was 53.3±15.8˚ in flexion, 54.3±13.9˚ in
extension, 78.1±11.0˚ in pronation and 75.3±13.9˚ in supination;
the grip strength ratio was 43.8±19.9% and the VAS score was
2.4±1.7. At 1 month following VLP fixation, in the poor group, the
RI was 22.5±3.8˚, VT was 11.9±3.5˚, UV was -1.0±1.0 mm, the wrist
range of motion was 50.6±12.4˚ in flexion, 43.8±15.8˚ in extension,
74.4±11.5˚ in pronation and 69.4±17.6˚ in supination; the grip
strength ratio was 17.2±5.4% and the VAS score was 5.6±1.5. The
grip strength ratio was significantly lower in the poor group
(P<0.001) and the patients had more pain (P<0.001) than the
good group (Table III).
 | Table IIComparison of the evaluation items at
the time of injury between the good and poor groups. |
Table II
Comparison of the evaluation items at
the time of injury between the good and poor groups.
| Parameter | Good group | Poor group | P-value |
|---|
| Duration from
injury to surgery (days) | 9.1±4.4 | 7.6±5.4 | 0.23 |
| Direction of
fracture dislocation (%) | | | |
|
Volar | 32.6 | 12.5 | 0.43 |
|
Dorsal | 67.4 | 87.5 | |
| Radiographic
parameters | | | |
|
Radial
inclination (˚) | 13.5±9.4 | 6.8±11.3 | 0.06 |
|
Volar tilt
(˚) | -6.5±20.3 | -23.8±20.1 | 0.02 |
|
Ulnar
variance (mm) | 1.3±2.4 | 4.2±3.5 | 0.01 |
 | Table IIIComparison of evaluation items at 1
month post-operatively in the good and poor groups. |
Table III
Comparison of evaluation items at 1
month post-operatively in the good and poor groups.
| Parameter | Good group | Poor group | P-value |
|---|
| Radiographic
parameters | | | |
|
Radial
inclination (˚) | 21.6±6.5 | 22.5±3.8 | 0.61 |
|
Volar tilt
(˚) | 10.6±4.8 | 11.9±3.5 | 0.50 |
|
Ulnar
variance (mm) | -0.3±1.5 | -1.0±1.0 | 0.13 |
| Wrist joint range
of motion | | | |
|
Flexion
(˚) | 53.3±15.8 | 50.6±12.4 | 0.62 |
|
Extension
(˚) | 54.3±13.9 | 43.8±15.8 | 0.06 |
|
Pronation
(˚) | 78.1±11.0 | 74.4±11.5 | 0.23 |
|
Supination
(˚) | 75.3±13.9 | 69.4±17.6 | 0.36 |
| Grip strength ratio
(%) | 43.8±19.9 | 17.2±5.4 | <0.001 |
| VAS score | 2.4±1.7 | 5.6±1.5 | <0.001 |
Four factors were extracted as factors related to
the poor group: VT and UV at the time of injury, and grip strength
ratio and VAS at 1 month following VLP fixation. From these four
factors, two factors were each combined and six-way logistic
regression analysis was performed (Table IV). As a result, all four factors
were found to be independently associated with the poor Q-DASH
score group.
 | Table IVResults of logistic regression
analysis. |
Table IV
Results of logistic regression
analysis.
| A, Ulnar variance
and volar tilt |
|---|
| Parameter | Good group | Poor group | OR (95% CI) | P-value |
|---|
| Ulnar variance | 1.3±2.4 | 4.2±3.5 | 1.41
(1.07-1.89) | 0.01 |
| Volar tilt | -6.5±20.3 | -23.8±20.1 | 0.96
(0.92-1.00) | 0.05 |
| B, Ulnar variance
and grip strength ratio |
| Ulnar variance | 1.3±2.4 | 4.2±3.5 | 1.41
(1.01-1.97) | 0.02 |
| Grip strength
ratio | 43.8±19.9 | 17.2±5.4 | 0.87
(0.77-0.97) | <0.01 |
| C, Ulnar variance
and VAS score |
| Ulnar variance | 1.3±2.4 | 4.2±3.5 | 1.40
(1.01-1.95) | 0.04 |
| VAS | 2.4±1.7 | 5.6±1.5 | 2.18
(1.36-3.50) | <0.01 |
| D, Volar tilt and
VAS score |
| Volar tilt | -6.5±20.3 | -23.8±20.1 | 0.93
(0.88-0.99) | <0.01 |
| VAS | 2.4±1.7 | 5.6±1.5 | 3.07
(1.60-5.87) | <0.01 |
| E, Grip strength
ratio and VAS score |
| Grip strength
ratio | 43.8±19.9 | 17.2±5.4 | 0.88
(0.77-1.00) | <0.01 |
| VAS | 2.4±1.7 | 5.6±1.5 | 2.14
(1.22-3.73) | <0.01 |
| F, Volar tilt and
grip strength ratio |
| Volar tilt | -6.5±20.3 | -23.8±20.1 | 0.95
(0.91-1.00) | 0.02 |
| Grip strength
ratio | 43.8±19.9 | 17.2±5.4 | 0.86
(0.78-0.96) | <0.01 |
Discussion
The aim of the present study was to identify
clinical findings involved in a poor Q-DASH score in the very early
post-operative period of 1 month following VLP fixation. In the
present study, VT and UV at the time of injury, and the VAS score
and grip strength ratio at 1 month following VLP fixation were the
clinical findings that contributed to a poor Q-DASH score at 1
month following VLP fixation. Interventions to improve these
clinical findings may lead to an immediate return to activity
following VLP fixation. In distal radius fractures, it has been
reported that distal radius fractures with large VT and UV
displacement at the time of injury are more likely to develop
triangular fibrocartilage complex (TFCC) injury (14). It is also known that patients with
soft tissue injury, such as TFCC injury tend to have poor
post-operative outcomes following VLP fixation (15). In other words, previous reports have
suggested that VT and UV at the time of injury are associated with
post-operative outcomes following VLP fixation. It has also been
reported that post-operative pain tends to hinder rehabilitation,
resulting in reduced patient satisfaction (16). Furthermore, Beumer and Lindau
(17) investigated the
post-operative grip strength ratio, range of motion of the wrist
joint and radiographic parameters in patients with hand and wrist
trauma, and analyzed the factors influencing the acquisition of
postoperative activities of daily life. As a result, it was
reported that the post-operative grip strength ratio had the
greatest influence on the level of activities of daily life
(17). Based on these findings and
the results of the present study, fracture displacement (VT and
UV), post-operative pain and post-operative grip strength may be
key factors for immediate return to activity.
As regards the alignment of the radius at the time
of injury, the present study found a greater amount of UV and VT
displacement in the poor group than the good group. It has been
reported that the extent of comminution and the amount of fracture
displacement are negatively associated with bone mineral density
(18). Clayton et al
(19) also reported that impact
energy and wrist position at the time of injury were associated
with the amount of fracture displacement. Among the factors that
influence the severity of fracture type, bone mineral density is a
factor that can potentially be treated by medical staff. However,
following distal radius fracture injury, the diagnosis of
osteoporosis is rare and the intervention rate for treatment is low
(~10%) (20). Addressing
osteoporosis treatment alongside the management of distal radius
fractures poses a challenge for medical staff. Moreover, the
potential of mesenchymal stem cell-derived extracellular vesicles
and exosomes derived from young plasma as a novel treatment for
osteoporosis focusing on osteogenic differentiation has also
recently been reported (21,22). The challenge for medical professional
is to be proactive in the treatment of osteoporosis, including new
therapies, to prevent an increase amount of displacement in the
patient with distal radius fractures.
The Q-DASH score was developed as a shortened
version of the DASH Outcome measure. Instead of the 30 items of the
DASH Outcome measure, the Q-DASH score uses 11 items to measure
physical function and symptoms in people with any or multiple
musculoskeletal disorders of the upper extremity. Of the 11 items,
nine are questions that involve various factors, such as range of
motion and grip strength and their impact on social activities,
work and sleep, whereas the remaining two items ask about the
severity of pain (9). Hence,
interventions for pain may alter the evaluation of two of the 11
items. In the present study, the VAS score of the good group was
2.4±1.7, whereas that of the poor group was 5.6±1.5. These findings
suggest that appropriate post-operative pain management enables an
immediate return to activity. Comparing the patient background in
the two groups, there were significantly more type C fractures in
the poor group compared with the good group (Table I). A previous study suggested that
intra-articular fractures result in more severe postoperative pain
than extra-articular fractures (23). Therefore, the type of fracture may be
a key factor in post-operative pain.
Previous studies have reported intraoperative and
post-operative pain management methods. Egol et al (16) reported that during surgery,
subclavian blocks provide more effective post-operative analgesia
than general anesthesia alone. Luo et al (24) reported that opioids provide more
effective pain relief during rehabilitation than COX inhibitors
alone. In numerous centers, intraoperative and post-operative pain
management methods are determined by the surgeon and
anesthesiologist, and there is no unified protocol for pain
management. Pain management is insufficient in the majority of
cases (25). It is critical to
understand that pain management is a key factor in improving the
Q-DASH score and establishing appropriate pain management.
Furthermore, it has recently been reported that platinum
cluster-loaded-mesoporous polydopamine nanoparticle and
QX-314-loaded fibrin gel (Pt@MPDA/QX314@Fibrin), a
therapeutic agent for chronic diabetic ulcer wounds, has a
pain-relieving effect by inactivating glial cells in the dorsal
root ganglion. The development of such novel therapeutic agents
with the potential to relieve post-operative pain is desirable
(26). Post-operative pain control
is a key factor for immediate return to activity in patients with
distal radius fractures, and it is crucial to establish appropriate
pain management, including new therapies.
In the present study post-operative grip strength
was also found to be critical for immediate return to activity
(Table IV). A previous study
suggested that grip strength was associated with the walking
ability following distal radius fracture (27). Furthermore, grip strength has been
shown to be associated with the Q-DASH score in individuals with or
without upper limb disorders (17,28).
Based on these findings, the results of the present study suggested
that grip strength was associated with the Q-DASH score, an
indicator of return to activity, even in the early post-operative
stage of 1 month following surgery. However, in rehabilitation
following VLP fixation, although range of motion training is
actively performed from an early stage, there are concerns about
grip strength training due to excessive load on the fracture site
(29). Grip strength training
following VLP fixation surgery is currently challenging. On the
other hand, Kaji et al (30)
developed a rehabilitation program that significantly improves the
post-operative Q-DASH score without causing loss of correction.
Specifically, in their study, the patients began grip strength
training under occupational therapist supervision using a 0.7 kg
gripper on the 14th post-operative day, followed by training using
a 1.4 kg load on the 21st day and a 2.3 kg load on the 28th day.
Training was performed once a day for 20 min during
hospitalization, and two to three times a week for 20 min each time
following discharge from the hospital. The findings of the present
study support this rehabilitation approach for immediate return to
activity following VLP fixation. Aggressive grip strength
rehabilitation in the early post-operative period following VLP
fixation is critical for immediate return to activity.
The present study has several limitations. First,
all 8 patients in the poor group had an AO classification of type
C. Type C fractures are sometimes associated with poor outcomes due
to the loss of correction and limited range of motion following VLP
fixation (31,32). However, in the present study, there
were no significant differences in radiographic parameters or range
of motion at 1 month post-operatively between the good and poor
groups, indicating that the previously reported factors for poor
outcomes had been overcome. Second, although there were 270 cases
during the study period, only 95 cases with available data at 1
month post-operatively were selected for inclusion. In the
outpatient clinic for the patients with distal radius fracture
post-operatively, the evaluation of clinical outcomes were
performed normally at 3, 6 and 12 months post-operatively at the
authors' hospital. Since the present study analyzed clinical
outcomes at 1 month post-operatively, the subjects were 95 patients
(~35% of all 270 patients) who had been evaluated at 1 month
post-operatively. Thus, there may have been inclusion bias. Third,
the number of cases was limited. Further studies with a larger
number of cases and data are thus warranted.
In conclusion, in the present study, a large amount
of fracture displacement at the time of injury was found to be a
factor that interfered with immediate return to activity following
VLP fixation. Fracture displacement at the time of injury was
reported to be associated with bone mineral density. Thus,
intervention to treat osteoporosis is critical. Furthermore,
post-operative pain management and grip strength training were
found to be key factors associated with immediate return to
activity. Thus, aggressive intervention, such as grip strength
training and pain management, may be necessary for the immediate
return to activity following VLP fixation.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
KK (first author) mainly wrote the manuscript, and
was involved in the acquisition of data, data analysis and
interpretation of the data. KN (corresponding author) and MI
conceived and designed the study. TS, YY, SK and NI performed the
acquisition of the data, data analysis, and were involved in the
interpretation of the data. KN and TS confirm the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee for Medical Research of Juntendo University (Tokyo,
Japan; no. E22-0447, date of approval: September 21st, 2023).
Informed consent was obtained both for participation and
publication in the form of opt-out on the web-site, and those who
rejected were excluded. The present study was a retrospective
study. The patients were subjected to standard clinical practice,
including the methods of anesthesia and surgery.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nellans KW, Kowalski E and Chung KC: The
epidemiology of distal radius fractures. Hand Clin. 28:113–125.
2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Bonafede M, Espindle D and Bower AG: The
direct and indirect costs of long bone fractures in a working age
US population. J Med Econ. 16:169–178. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Koo KOT, Tan DMK and Chong AKS: Distal
radius fractures: An epidemiological review. Orthop Surg.
5:209–213. 2013.PubMed/NCBI View
Article : Google Scholar
|
|
4
|
Chung KC, Shauver MJ and Birkmeyer JD:
Trends in the United States in the treatment of distal radial
fractures in the elderly. J Bone Joint Surg Am. 91:1868–1873.
2009.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Wilcke MKT, Hammarberg H and Adolphson PY:
Epidemiology and changed surgical treatment methods for fractures
of the distal radius: A registry analysis of 42,583 patients in
Stockholm County, Sweden, 2004-2010. Acta Orthop. 84:292–296.
2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Mellstrand-Navarro C, Pettersson HJ,
Tornqvist H and Ponzer S: The operative treatment of fractures of
the distal radius is increasing: Results from a nationwide Swedish
study. Bone Joint J. 96:963–969. 2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Oldrini LM, Feltri P, Albanese J, Lucchina
S, Filardo G and Candrian C: Volar locking plate vs cast
immobilization for distal radius fractures: A systematic review and
meta-analysis. EFORT Open Rev. 7:644–652. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
MacDermid JC: Patient-reported outcomes:
State-of-the-art hand surgery and future applications. Hand Clin.
30:293–304. 2014.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Imaeda T, Toh S, Wada T, Uchiyama S,
Okinaga S, Kusunose K and Sawaizumi T: Validation of the Japanese
Society for Surgery of the Hand version of the quick disability of
the Arm, Shoulder, and Hand (QuickDASH-JSSH) questionnaire. J
Orthop Sci. 11:248–253. 2006.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Soong M, Leerdam RV, Guitton TG, Got C,
Katarincic J and Ring R: Fracture of the distal radius: Risk
factors for complications after locked volar plate fixation. J Hand
Surg Am. 36:3–9. 2011.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Yu L, Zhang X, Zhang B, Hu C, Yu K, Tian D
and Bai Y: Outcomes of volar locking plate (VLP) fixation for
treatment of die-punch fracture of the distal radius: A
retrospective single-surgeon study. Medicine (Baltimore).
98(e16796)2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zhu Y, Liu S, Li Y, Yang Q, Miao R and
Zhang Y: Risk factors for complications following volar locking
plate (VLP) fixation of unstable distal radius fracture (DRF).
Biomed Res Int. 2022(9117533)2022.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fritzsching B, Fellenberg J, Moskovszky L,
Sápi Z, Krenacs T, Machado I, Poeschl J, Lehner B, Szendrõi M,
Bosch AL, et al: CD8+/FOXP3+-ratio in
osteosarcoma microenvironment separates survivors from
non-survivors: A multicenter validated retrospective study.
Oncoimmunology. 4(e990800)2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Lee HW, Kim KT, Lee S, Yoon JH and Kim JY:
Fracture severity and triangular fibrocartilage complex injury in
distal radius fractures with or without osteoporosis. J Clin Med.
13(992)2024.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Lindau T, Adlercreutz C and Aspenberg P:
Peripheral tears of the triangular fibrocartilage complex cause
distal radioulnar joint instability after distal radial fractures.
J Hand Surg Am. 25:464–468. 2000.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Egol KA, Soojian MG, Walsh M, Katz J,
Rosenberg AD and Paksima N: Regional anesthesia improves outcome
after distal radius fracture fixation over general anesthesia. J
Orthop Trauma. 26:545–549. 2012.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Beumer A and Lindau TR: Grip strength
ratio: A grip strength measurement that correlates well with DASH
score in different hand/wrist conditions. BMC Musculoskelet Disord.
15(336)2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Lill CA, Goldhahn J, Albrecht A, Eckstein
F, Gatzka C and Schneider E: Impact of bone density on distal
radius fracture patterns and comparison between five different
fracture classifications. J Orthop Trauma. 17:271–278.
2003.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Clayton RAE, Gaston MS, Ralston SH,
Court-Brown CM and McQueen MM: Association between decreased bone
mineral density and severity of distal radial fractures. J Bone
Joint Surg Am. 91:613–619. 2009.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Baba T, Hagino H, Nonomiya H, Ikuta T,
Shoda E, Mogami A, Sawaguchi T and Kaneko K: Inadequate management
for secondary fracture prevention in patients with distal radius
fracture by trauma surgeons. Osteoporos Int. 26:1959–1963.
2015.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Zeng ZL and Xie H: Mesenchymal stem
cell-derived extracellular vesicles: A possible therapeutic
strategy for orthopaedic diseases: A narrative review. Biomater
Transl. 3:175–187. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Meng F, Wang G, Zhou F, Li G, Wang M, Zhou
Z, Han Y, Chen X, Hu Y, Zhang Y, et al: Exosomes from young plasma
alleviate osteoporosis through miR-217-5p-regulated osteogenesis of
bone marrow mesenchymal stem cell. Compos B Eng.
276(111358)2024.
|
|
23
|
Mulders MAM, Selles CA, Colaris JW, Peters
RW, van Heijl M, Cleffken BI and Schep NWL: Operative treatment of
intra-articular distal radius fractures with versus without
arthroscopy: Study protocol for a randomised controlled trial.
Trials. 19(84)2018.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Luo P, Lou J and Yang S: Pain management
during rehabilitation after distal radius fracture stabilized with
volar locking plate: A prospective cohort study. Biomed Res Int.
2018(5786089)2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Niedermeier SR, Crouser N, Hidden K and
Jain SA: Pain management following open reduction and internal
fixation of distal radius fractures. J Wrist Surg. 10:27–30.
2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Chen S, Wang H, Du J, Ding Z, Wang T,
Zhang L, Yang J, Guan Y, Chen C, Li M, et al: Near-infrared
light-activatable, analgesic nanocomposite delivery system for
comprehensive therapy of diabetic wounds in rats. Biomaterials.
305(122467)2024.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Yamamoto A, Fujita K, Yamada E, Ibara T,
Nihey F, Inai T, Tsukamoto K, Kobayashi Y, Nakahara K and Okawa A:
Foot characteristics of the daily-life gait in postmenopausal
females with distal radius fractures: A cross-sectional study. BMC
Musculoskelet Disord. 24(706)2023.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Izawa KP, Kasahara Y, Hiraki K, Hirano Y
and Watanabe S: Relation between the disability of the Arm,
Shoulder and Hand score and muscle strength in post-cardiac surgery
patients. Diseases. 5(31)2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Roh YH, Lee BK, Noh JH, Oh JH, Gong HS and
Baek GH: Factors delaying recovery after volar plate fixation of
distal radius fractures. J Hand Surg Am. 39:1465–1470.
2014.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Kaji Y, Yamaguchi K, Nomura Y, Oka K,
Nakamura O, Ishibashi Y and Yamamoto T: Postoperative early and
proactive grip strength training program for distal radius
fractures promotes earlier recovery of grip strength: A
retrospective study. Medicine (Baltimore).
101(e29262)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Earp BE, Foster B and Blazar PE: The use
of a single volar locking plate for AO C3-type distal radius
fractures. Hand (NY). 10:649–653. 2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Grube G, Gruber K, Giessauf C, Clar H,
Zacherl M, Fuerst F and Bernhardt GA: Volar plate fixation of AO
type C2 and C3 distal radius fractures, a single-center study of 55
patients. J Orthop Trauma. 22:467–472. 2008.PubMed/NCBI View Article : Google Scholar
|