Introduction
Cesarean section, when medically indicated, is a
crucial procedure for safeguarding the lives of both the mother and
newborn. However, the global rise in cesarean delivery rates,
reaching levels as high as 30-40% in a number of countries
(1), has brought attention to
associated pathological conditions, such as dysmenorrhea,
dyspareunia, chronic pelvic pain and infertility (2). Post-operative pelvic adhesions, a
common complication following cesarean sections, particularly
increase in rate and severity with each subsequent surgery
(3). It has been found that the
likelihood of adhesion formation escalates from 5% after the
initial procedure to a notable 68% following three or more cesarean
sections (4). The present study
describes the case of a patient in which adhesions resulting from
two prior cesarean sections led to the entrapment and ischemic
necrosis of the left fallopian tube, with the presence of a small
hydatid of Morgagni, resulting in preterm labor. While
intra-amniotic inflammation is recognized as a predominant cause of
preterm labor, accounting for an estimated 4-16% of all births
(5) and a significant contributor to
neonatal morbidity and mortality worldwide (6), the case described herein presents a
unique scenario. The onset of preterm labor due to ischemic tubal
necrosis with a hydatid of Morgagni, subsequent to entrapment in
post-cesarean section adhesions, is an unprecedented occurrence in
the English literature.
In light of this case, the authors aim to stress the
importance of an intraoperative inspection of the fallopian tubes
and ovaries during cesarean sections in order to detect and manage
postoperative adhesions promptly. Additionally, the pre-operative
identification of pelvic adhesions following cesarean delivery is
crucial, and the present study aims to advocate for proactive
measures to prevent adhesion formation in pregnant women with a
history of cesarean sections, thereby reducing the risks of
maternal and perinatal morbidity.
Case report
A 24-year-old pregnant woman, having undergone two
previous lower-segment cesarean sections, presented to the
Emergency Department of the General Hospital of Trikala, Trikala,
Greece during the 36th week of gestation with complaints of diffuse
abdominal pain. She reported that the pain had commenced ~4 h
prior, characterized by intermittent exacerbation and escalating
intensity. The pain was diffuse across the abdomen, initially
originating from the left lumbar region, where it was most intense.
The pain was accompanied by multiple episodes of vomiting. Pain
intensity was not associated with defecation and was unaffected by
body posture. The patient denied any history of preterm labor, and
her pregnancy had been uneventful thus far. A prenatal ultrasound
and blood sugar monitoring yielded normal findings. Cervical length
measurements via ultrasound remained within normal limits
throughout each trimester. The patient exhibited a normal body mass
index (20.8 kg/m2), and the healing process of her
previous cesarean section scars was unremarkable, without any
evidence of subcutaneous tissue stiffness, keloids, or hypertrophic
scars. Additionally, there were no abdominal stretch marks
indicative of pregnancy.
Upon a vaginal examination, cervical dilation (2 cm)
was observed. A cardiotocography revealed uterine contractions. An
obstetric ultrasound indicated normal fetal growth (estimated
ultrasound weight, 2,560 g) and a normal amount of amniotic fluid
(amniotic fluid index, 8 cm), with no ultrasonographic signs of
placental abruption. A urinary tract ultrasound ruled out the
presence of calculi and did not reveal any signs of obstructive
uropathy (such as hydronephrosis). Laboratory tests indicated mild
anemia (hematocrit level, 31.6%; hemoglobin level, 10.8 g/dl),
persisting since the onset of pregnancy. The analysis of
inflammation-related markers yielded negative results: White blood
cells, 5,600/µl; neutrophils, 65.6%; C-reactive protein, 0.5 mg/dl.
Coagulation, biochemical parameters and general urinalysis did not
yield any notable findings. Vaginal fluid microscopy and culture
revealed no microbial growth, and the test for detecting the
premature rupture of fetal membranes yielded negative results.
Based on the clinical, ultrasound and laboratory
findings outlined above, a diagnosis of preterm labor was
established, necessitating the decision to proceed with a cesarean
section. The General Hospital of Trikala lacked the logistical
infrastructure (organized operating room near the delivery room
with constant presence of an anesthesiologist) and expertise on the
part of obstetrician-gynecologists required for attempting vaginal
delivery following a previous cesarean section. Therefore, the
patient, 2 days before completing 36 weeks of pregnancy, underwent
a cesarean section, delivering a healthy, full-term female newborn
weighing 2,490 g. The procedure was performed without
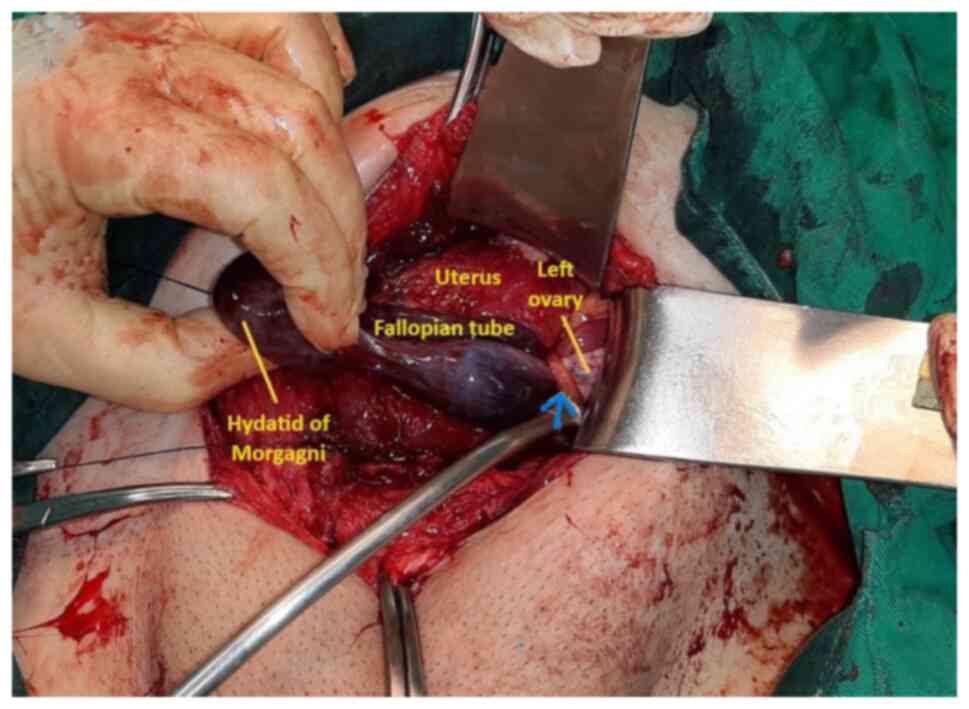
complications, with normal blood loss. Intraoperatively, numerous
post-operative adhesions were observed within the abdomen,
particularly between the uterus and the bladder at the
vesicouterine pouch, as well as between the uterus and the left
lateral abdominal wall. During intraoperative abdominal
examination, ischemic necrosis of the left fallopian tube with a
small hydatid of Morgagni was noted, secondary to entrapment in
post-cesarean section adhesions, with no involvement of the left
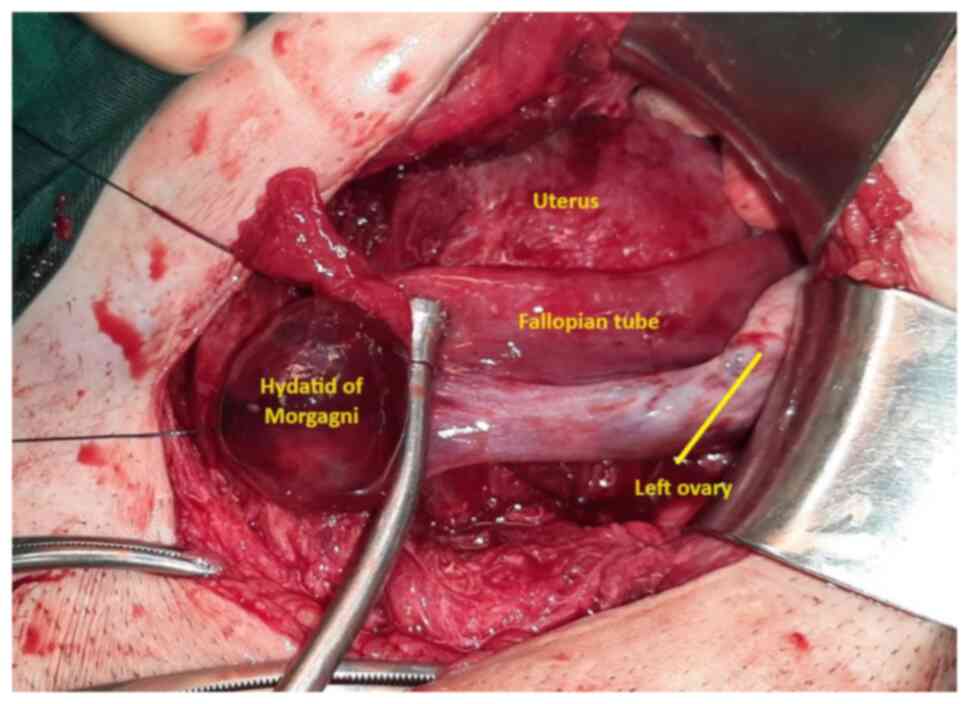
ovary (Fig. 1). Upon the dissection
of the adhesions, tubal perfusion was promptly restored within
approximately two minutes (Fig. 2).
It was decided to preserve the affected fallopian tube and perform
surgical drainage of the small hydatid of Morgagni. The neonate did
not require admission to the Neonatal Intensive Care Unit, and both
the mother and newborn were discharged in excellent condition from
the Obstetrics and Gynecology clinic of the General Hospital of
Trikala on the 4th post-operative day. A follow-up gynecological
assessment 10 weeks following delivery revealed normal findings
from her physical and ultrasonographic examination.
Discussion
The pre-operative diagnosis of intra-abdominal
surgical adhesions resulting from previous cesarean sections poses
a challenge. However, non-invasive methods, such as assessing the
characteristics of the skin scar post-cesarean section, the
presence of pregnancy stretch marks on the abdominal wall and
utilizing ultrasound guidance to examine the uterine sliding point
on the anterior abdominal wall have shown promise. The correct
application and interpretation of these methods could significantly
aid in pre-operative diagnosis before planned repeat cesarean
sections (7). In the study by
Tulandi et al (8) in 2011, it
was demonstrated that pregnant women with keloids in the cesarean
section scar were more likely to develop post-operative adhesions
between the uterus and the bladder, as well as between the uterus
and the abdominal wall. Recently, Seven et al (9) conducted a study in 2020, where they
investigated the stiffness of subcutaneous tissue in previous
cesarean section scars. Their findings revealed that elastographic
assessment of subcutaneous tissue stiffness at the cesarean section
scar site can predict the severity of intra-abdominal surgical
adhesions preoperatively in repeat cesarean sections (9).
There is a notable association between abdominal
wall stretch marks and intra-abdominal surgical adhesions in
pregnant women with prior cesarean sections. In 2016, Dogan et
al (10) conducted a study
demonstrating that a higher score for abdominal wall stretch marks
during pregnancy correlates with a reduction in intra-abdominal
surgical adhesions among pregnant women scheduled for cesarean
sections due to previous cesarean deliveries. Similarly, Cakir
Gungor et al (11) concluded
that the presence of pregnancy stretch marks on the abdominal wall
could serve as a pre-operative indicator for predicting the
formation of intra-abdominal surgical adhesions. In the case in the
present study, despite the presence of multiple postoperative
pelvic adhesions leading to entrapment and partial ischemic
necrosis of the left fallopian tube, there was no association with
the presence of keloids or subcutaneous tissue stiffness at the
scar site, or pregnancy stretch marks on the abdominal wall.
In contrast to the aforementioned clinical
indicators for the pre-operative prediction of intra-abdominal
post-cesarean section adhesions, the absence of uterine sliding
point on the anterior abdominal wall (limited uterine mobility)
detected via ultrasound examination is considered the most
significant and effective predictor of postoperative adhesions
following previous cesarean sections (2). The recent study by Yosef et al
(12) in 2023 concluded that
ultrasound assessment of the uterine sliding point is a rapid,
simple, and reliable method for prenatally predicting
intraperitoneal adhesions. The aim is to adequately prepare
pregnant women preoperatively and mitigate the risk of serious
intraoperative and postoperative complications. The authors of that
study reported a sensitivity of 100%, specificity of 86.84%,
positive predictive value of 81.5%, negative predictive value of
100%, and accuracy of 91.67% for this method (12). Similar findings were reported by
Charernjiratragul et al (13), who demonstrated that the uterine
sliding point serves as an independent prognostic indicator of
intra-abdominal surgical adhesions, with acceptable sensitivity,
high specificity and negative predictive value. In the case
described herein, the evaluation of the uterine sliding point on
the anterior abdominal wall was positive, indicating no restriction
of uterine mobility during an ultrasonographic examination.
However, it is worth noting that the examination was performed by
obstetricians-gynecologists at the Obstetrics and Gynecology Clinic
of the General Hospital of Trikala, whose specialized skills in
ultrasonography may be limited compared to specialized
sonographers.
The prevention of intra-abdominal surgical adhesions
in the pelvis may be facilitated by platelet-rich plasma infusion
(14,15); however, further research on applied
methodology is required to ascertain the value of such techniques
in the context of prevention (16,17).
Even surgical approach may aid in prevention, as the Misgav Ladach
technique may be associated with a higher likelihood of
post-cesarean section pelvic adhesion formation compared to more
traditional methods, such as Pfannenstiel-Dörffler and low midline
laparotomy-Dörffler techniques (18).
Performing a planned cesarean section in pregnant
women with multiple post-operative pelvic adhesions is challenging
and requires appropriate pre-operative preparation (19). In selected cases where the incision
of the anterior uterine wall is not feasible due to severe pelvic
adhesions, a low transverse incision in the posterior uterine wall
after rotation may be a safe and effective approach (20). In the case in the present study,
pelvic adhesions resulting from previous cesarean sections were not
very severe. Entry into the peritoneal cavity and delivery of the
fetus through an incision in the anterior uterine wall were
achieved without significant difficulty. The challenges primarily
stemmed from the lack of prenatal etiological diagnosis of preterm
labor, which was established intraoperatively upon discovering
ischemic necrosis of the fallopian tube and accompanying hydatid of
Morgagni due to entrapment by adhesions. In the case in the present
study, ischemic necrosis turned out to be reversible and the
fallopian tube was preserved. However, due to the inflammation
caused in the region, it was decided to only drain the hydatic of
Morgagni instead of removing it in order to avoid further injury to
the afflicted salpinx and preserve future fertility prospects. The
presence of this cyst in this case, although notable, was not the
primary etiology behind the observed pathology and was for the most
part a concurrent condition.
The main limitation of the present study was its
lack of involvement of multiple cases, which would allow for even a
limited generalization of the findings. The present study paper
describes a single case, believed to have not been previously
described in the English literature. More valid conclusions could
be drawn after conducting larger studies, aimed at investigating
the etiology and risk factors associated with the development of
postoperative pelvic adhesions, including the surgical techniques
used.
In conclusion, surgical pelvic adhesions are a
common complication following a cesarean section. The occurrence of
preterm labor as a consequence of intra-abdominal inflammation
caused by the entrapment of the fallopian tube with a hydatid of
Morgagni in a postoperative pelvic adhesion is a unique case.
However, in any instance of preterm labor onset in a pregnant woman
with a history of previous cesarean section, the potential role of
postoperative pelvic adhesions should be investigated as part of
the mechanism of labor induction. The prenatal diagnosis of
post-cesarean section adhesions is crucial for the prevention of
severe intraoperative and post-operative complications, some of
which are best treated in a tertiary medical center.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data used in the current study are available
from the corresponding author upon reasonable request.
Authors' contributions
AT, ET and AL participated in the conception and
design of the study and in the international literature search.
IRA, AC and IP were involved in the conception and design of the
study, in the provision of study materials (such as blood tests,
culture test and imaging) or patient data, in data collection and
aggregation, and in data analysis and interpretation. EX and AZ
participated in the conception and design of the study and in the
international literature search. IT was involved in the conception
and design of the study, in administrative support, in the
provision of study materials (such as blood tests, culture test,
and imaging) or patient data, in patient care, in data collection,
in manuscript writing and analysis, and had the overall supervision
of the manuscript. All authors participated in the writing of the
manuscript, contributed to the revision of the manuscript, and have
read and approved the final version of the manuscript. All authors
(AT, ET, IRA, EX, AZ, AL, AC, IP, and IT) confirm the authenticity
of all raw data.
Ethics approval and consent to
participate
The present study was conducted according to the
guidelines of the Declaration of Helsinki. Written informed consent
was obtained from the patient.
Patient consent for publication
The patient in the present study provided signed
consent for the publication of her medical case anonymously.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Antoine C and Young BK: Cesarean section
one hundred years 1920-2020: The good, the bad and the ugly. J
Perinat Med. 49:5–16. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Shafti V, Azarboo A, Ghaemi M, Gargari OK
and Madineh E: Prediction of intraperitoneal adhesions in repeated
cesarean sections: A systematic review and meta-analysis. Eur J
Obstet Gynecol Reprod Biol. 287:97–108. 2023.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Pokhrel M, Sherpa LD, Thapa M and Sharma
J: Intra-abdominal adhesions among patients undergoing repeat
caesarean section in department of obstetrics and gynaecology of a
tertiary care centre: A descriptive cross-sectional study. JNMA J
Nepal Med Assoc. 60:517–520. 2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Rossouw JN, Hall D and Harvey J: Time
between skin incision and delivery during cesarean. Int J Gynaecol
Obstet. 121:82–85. 2013.PubMed/NCBI View Article : Google Scholar
|
|
5
|
WHO. Preterm Birth. Available from:
https://www.who.int/news-room/fact-sheets/detail/preterm-birth.
Accessed on August 12, 2023.
|
|
6
|
Gomez-Lopez N, Galaz J, Miller D,
Farias-Jofre M, Liu Z, Arenas-Hernandez M, Garcia-Flores V, Shaffer
Z, Greenberg JM, Theis KR and Romero R: The immunobiology of
preterm labor and birth: intra-amniotic inflammation or breakdown
of maternal-fetal homeostasis. Reproduction. 164:R11–R45.
2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sönmez S, Akselim B and Karaşin SS: The
effectiveness of preoperative diagnostic methods in predicting
intra-abdominal adhesions before repeat cesarean section delivery.
Rev Assoc Med Bras (1992). 69(e20221455)2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tulandi T, Al-Sannan B, Akbar G, Ziegler C
and Miner L: Prospective study of intraabdominal adhesions among
women of different races with or without keloids. Am J Obstet
Gynecol. 204:132.e1–4. 2011.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Seven B, Yorgancı A, Alkan M, Gündüz Ö,
Keskin HL and Engin-Üstün Y: Subcutaneous tissue stiffness of
cesarean incision scar by elastography as a predictor of
intra-abdominal adhesions. J Obstet Gynaecol Res. 46:2390–2396.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Dogan A, Ertas IE, Uyar I, Karaca I,
Bozgeyik B, Töz E and Ozeren M: Preoperative Association of
abdominal striae gravidarum with intraabdominal adhesions in
pregnant women with a history of previous cesarean section: A
cross-sectional study. Geburtshilfe Frauenheilkd. 76:268–272.
2016.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Gungor AN, Oguz S, Hacivelioglu S, Isik S,
Uysal A, Gencer M and Cosar E: Predictive value of striae
gravidarum severity for intraperitoneal adhesions or uterine scar
healing in patients with previous caesarean delivery. J Matern
Fetal Neonatal Med. 27:1312–1315. 2014.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Yosef AH, Youssef AEA, Abbas AM, Mohamed
AA, Mostafa SM and Ibrahim MN: The use of ultrasound sliding sign
for prediction of adhesions in women undergoing repeated caesarean
section. J Obstet Gynaecol. 43(2114333)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Charernjiratragul K, Suntharasaj T,
Pranpanus S, Chanwadi S, Kwankaew N and Petpichetchian C:
Preoperative sonographic sliding sign for prediction of
intra-abdominal adhesions before repeat cesarean delivery. Int J
Gynaecol Obstet. 161:250–254. 2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Turan E, Ayhan B, Kargın S, Doğru O and
Uğraş NS: Evaluation of the efficacy of platelet-rich plasma in
preventing postoperative intraabdominal adhesions. Turk J Surg.
36:53–58. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Karakaş DÖ, Dandin Ö, Müftüoğlu T, Tihan
D, Bal AS and Yıldırım Ş: Effect of platelet-rich plasma on
postoperative peritoneal inflammation and adhesions. Arch Med Sci.
17:1408–1413. 2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Stratakis K, Arkoumanis T, Liakea A,
Nikiteas N, Zargaran D, Zargaran A, Kontzoglou K, Kyriakopoulou P
and Perrea D: Platelet-rich plasma gel versus hyaluronic acid on
prevention of peritoneal abdominal adhesion formation in rats.
Chirurgia (Bucur). 117:585–593. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Kurt B, Yildiz C, Koc T, Kurt-Ozkaya N and
Celikgun S: The effect of platelet-rich plasma on intra-abdominal
adhesions in rabbit uterine horn model. Cir Cir. 91:773–779.
2023.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Fatusić Z and Hudić I: Incidence of
post-operative adhesions following Misgav Ladach caesarean
section-a comparative study. J Matern Fetal Neonatal Med.
22:157–160. 2009.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Visconti F, Quaresima P, Rania E, Palumbo
AR, Micieli M, Zullo F, Venturella R and Di Carlo C: Difficult
caesarean section: A literature review. Eur J Obstet Gynecol Reprod
Biol. 246:72–78. 2020.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Tan X, Xing A and Tong A: Rotation of the
uterus to obtain a lower transverse incision in the posterior wall
in a cesarean section: A case report and literature review. J
Matern Fetal Neonatal Med. 36(2217988)2023.PubMed/NCBI View Article : Google Scholar
|