Introduction
Peripheral vascular injury is a severe although
infrequent complication of acute trauma (1). Its incidence has increased due to the
rise in workplace accidents, traffic incidents and firearm assaults
(2). Regardless of its etiology, the
vessels in the lower limbs are usually the most affected (3), particularly the femoral artery and vein
(4). Although the mortality rate for
these injuries does not exceed 10% (5), the potential functional repercussions
can be incapacitating (6), both due
to neurological sequelae and in cases of limb loss through
amputation (7). Although
historically, the latter has been the most effective treatment for
the survival of patients (8), since
the late 20th century, the therapeutic approach of ‘damage control’
has been adopted, aiming to preserve both life and limb
functionality (9). Prolonged
ischemia is the main predictor for amputation (10), this approach is indicated in up to
85% of cases where ischemia lasts longer than six hours (11). Therefore, ensuring rapid reperfusion
is an imperative goal in the treatment of vascular injury (12). This can be achieved through the
placement of stents, bypasses (13)
or venous grafts during the intraoperative period (14). However, on some occasions, the
severity of the injury requires multidisciplinary management
causing delays in revascularization (15). Providing temporary relief from
ischemia through shunts helps maintain tissue perfusion until the
patient stabilizes (16), at which
point definitive treatment can proceed (17). This approach improves the overall
prognosis of critically ill patients or those with complex vascular
trauma (18), reducing mortality
while preserving the limb (19,20). The
present study describes the case of a patient with severe vascular
injury, who despite an unstable hemodynamic state, was successfully
treated using this damage control strategy.
Case report
A 28-year-old male with no significant medical
history, was admitted to the Emergency Department of Hospital
Regional Universitario (Colima, Mexico) due to a hemorrhagic injury
in the right lower limb secondary to a firearm wound, with a
progression time of 1 h and 20 min. In the initial assessment, the
patient was found to be hemodynamically unstable, presenting with
grade IV hypovolemic shock, with an entry wound on the anteromedial
side of the right leg and an exit wound on the lateral side. A
pulsatile and expanding hematoma was observed in the area, along
with a gaping wound with musculoskeletal tissue loss secondary to
short blunt trauma. Absent pulses were noted in the dorsalis pedis,
posterior tibial and anterior tibial arteries; the affected limb
was pale and poikilothermic, with a capillary refill time of 6 sec.
Sensitivity and muscle strength were preserved and the revised
trauma score (RTS) was calculated at 7.8408. Management was
initiated with oxygen therapy, hyperhydration, the transfusion of
blood products, as well as antibiotics (cclindamycin: 600 mg, i.v.
administration, every 8 h; and cefixime: 2 g i.v. administration,
every 12 h) and analgesia (buprenorphine: 0.3 mg i.v.
administration, every 8 h, combined with the continuous intravenous
infusion of paracetamol at a dose of 1 g). Following the
aforementioned, the decision was made to take the patient urgently
to the operating room for vascular exploration.
Treatment technique
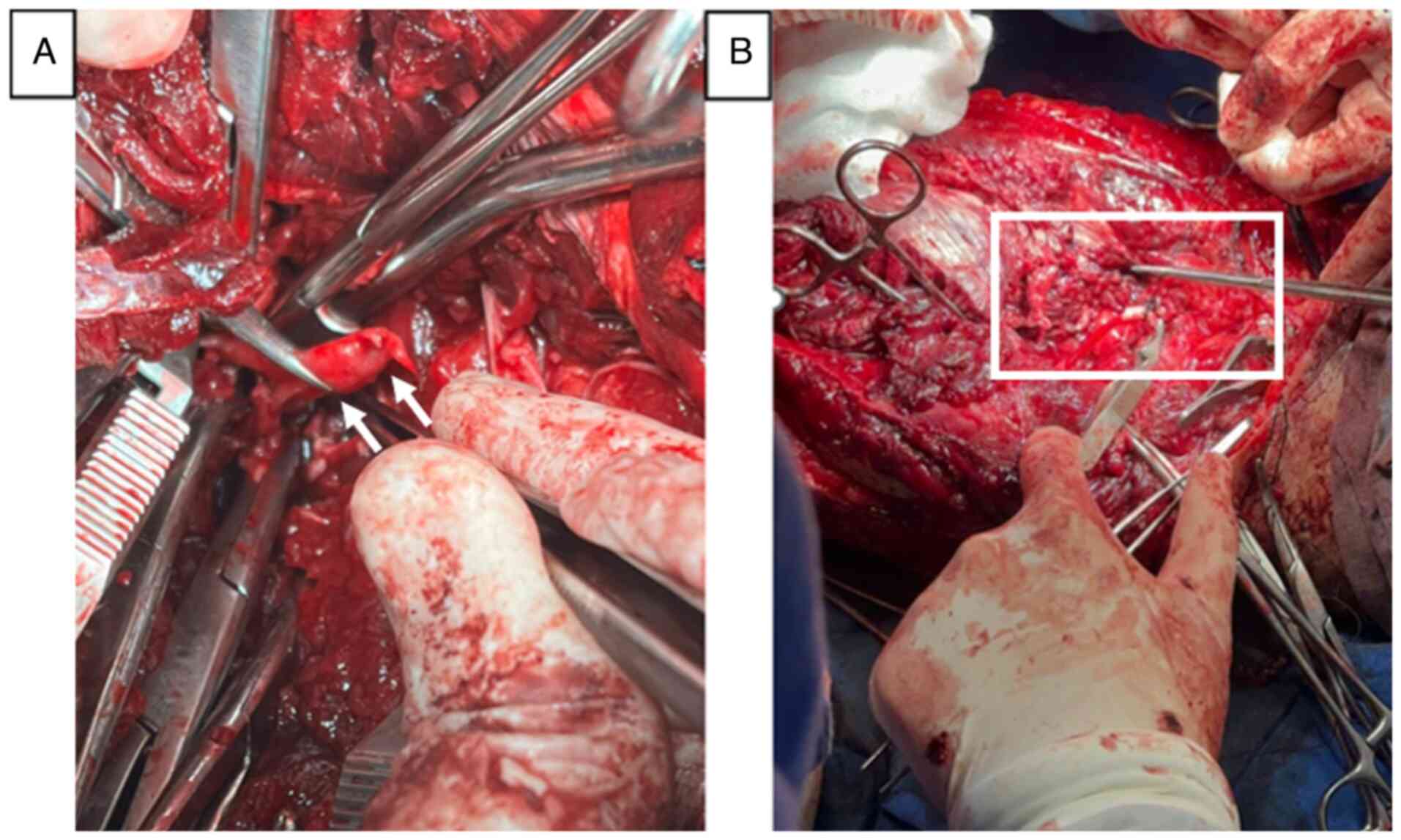
Under general anesthesia, the patient was positioned
in a prone position, and a posterior surgical approach was made to
the left popliteal artery. Distal vascular control of the popliteal
artery and vein was achieved. Subsequently, the incision was
extended proximally to explore the hematoma in the posterior region
of the right leg, thus opening the superficial and deep posterior
compartments, revealing a complete transection of the popliteal
artery with a discontinuity of ~5 cm, as well as of the popliteal
vein and the deep peroneal nerve, with no possibility of primary
anastomosis. Sodium heparin was administered at a dose of 100
IU/kg. Given the hemodynamic condition of the patient and the
development of intraoperative acidosis, a damage control strategy
was implemented, with a popliteal-popliteal shunt using an 8 French
feeding tube and the ligation of the thrombosed popliteal vein
(Fig. 1). The proximal clamp was
removed, revealing the presence of arterial flow and distal pulses,
though diminished in amplitude, with a capillary refill time of 4
sec. The surgical wound was cleaned, and partial closure was
performed. The total blood loss during the surgery and emergency
room stay was 4,000 ml. The patient received one red blood cell
concentrate during his stay in the emergency room and two in the
operating room along with one unit of fresh-frozen plasma. The
patient was admitted to the intensive care unit for comprehensive
support and to improve hemodynamic conditions for a second
definitive surgical procedure.
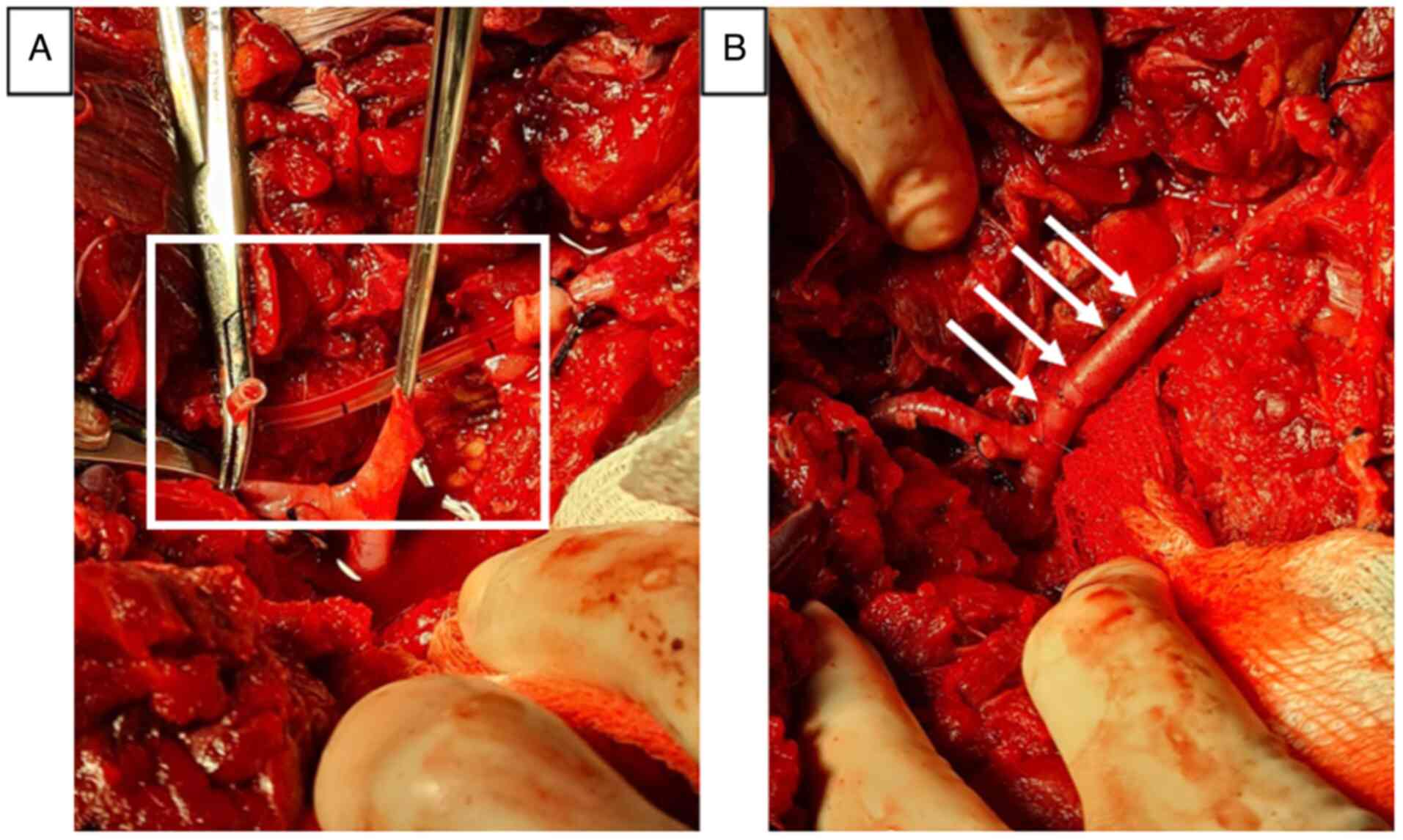
After 10 h, the patient regained hemodynamic
stability; however, signs of acute ischemia began to appear,
prompting a reintervention for limb revascularization. For this,
the contralateral greater saphenous vein was harvested for use as
an autologous graft. Upon the reopening of the previous incision,
the thrombosed shunt was found, which was dismantled. Additionally,
a previously unnoticed punctate lesion of 1 mm in diameter was
discovered in the anterior tibial artery, which was repaired with a
simple suture using 7-0 vascular Prolene. A thrombectomy was
performed proximally and distally with a 3 French Fogarty catheter,
retrieving a fresh thrombus. Subsequently an interposition graft
was made in the popliteal artery using an inverted saphenous vein,
with end-to-end anastomosis using 6-0 vascular Prolene. Upon
removing the proximal clamp, adequate arterial flow and the
presence of distal pulses were observed. Posterior and lateral
fasciotomies were performed to prevent compartment syndrome, with
partial closure of the surgical wound, and no drains were placed.
Sodium heparin was administered at a dose of 100 IU/kg (Fig. 2).
The patient was stable in the immediate
post-operative period. No signs of compartment syndrome or
reperfusion syndrome were observed. However, follow-up laboratory
tests revealed normal renal function, with a serum creatinine level
of 1.0 mg/dl, a urea level of 30 mg/dl, blood urea nitrogen (BUN)
level of 15 mg/dl, and an estimated glomerular filtration rate
(eGFR) >90 ml/min/1.73 m². Serum electrolytes were within normal
limits, including sodium at 140 mmol/l, potassium at 4.2 mmol/l,
chloride at 102 mmol/l, bicarbonate at 24 mmol/l, total calcium at
9.5 mg/dl, magnesium at 2.0 mg/dl and phosphorus at 3.5 mg/dl.
Cardiac biomarkers were also within the expected range, with a
total creatine phosphokinase level of 100 U/l, a CPK-MB fraction of
20 U/l, a troponin I level of 0.02 ng/ml, a troponin T level of
0.005 ng/ml, a myoglobin concentration of 50 ng/ml, and a lactate
dehydrogenase level of 180 U/l. Complete blood count analysis
revealed severe anemia with a hemoglobin concentration of 5 g/ds,
without additional abnormalities in the leukocyte or platelet
counts. Arterial blood gas analysis demonstrated metabolic acidosis
without other significant alterations. Therefore, medical
management with fluid therapy, diuretics and the close monitoring
of renal function was initiated. Subsequently, the patient had an
adequate clinical evolution, with resolution of the rhabdomyolysis
symptoms. He was discharged 10 days following the second surgical
procedure, exhibiting adequate distal pulses and with no signs of
infection or other early complications. As regards follow-up, the
patient was evaluated at 1 and 3 months after the intervention. At
that time, adequate vascularization was confirmed through the
palpation of distal pulses and the full functionality of the
salvaged limb, along with proper wound healing. No ultrasound
images were available for this timeframe; however, based on
clinical observations, the functionality of the limb was
maintained.
Discussion
The present study described the case of a young male
patient with a firearm-induced vascular injury in the lower limb.
The complication resulted in grade IV hypovolemic shock and
metabolic acidosis, necessitating urgent intervention for
hemostatic control. However, due to the complexity of the injuries
and the presence of ischemia, a damage control strategy was
implemented, leading to limb preservation and a favorable
postoperative recovery following the definitive intervention.
The case described herein highlights the complexity
of limb salvage decisions in acute vascular injuries, where the
option between amputation and preservation depends on multiple
factors, including the severity of ischemia and the patient's
overall condition (21). The patient
had no significant medical history, and no fractures were
identified. Despite this, the development of grade IV hypovolemic
shock and metabolic acidosis posed challenges in patient
management, as these conditions require immediate surgical
intervention in such injuries (22).
Although simple indices, such as the mangled
extremity score (MES) or the mangled extremity severity index
(MESI), can help determine the most appropriate treatment for acute
vascular injuries (23), functional
and individual patient factors should also be considered. While
survival rates following amputation can reach 100%, depending on
the technique used and the condition of the patient (24), the long-term consequences are
critical. Studies have reported substantial psycho-emotional
distress, increased mobility-related costs and disruptions in
interpersonal relationships, particularly when amputation results
from traumatic events (25), as in
the case described herein. Additionally, phantom limb pain,
somatosensory alterations (26) and
weight gain (27) are commonly
reported following amputation. These negative effects can be
mitigated through early rehabilitation, physiotherapy, and
prosthesis adaptation (28).
However, previous research has indicated that while cerebral cortex
reorganization occurs following upper limb amputations, it is less
effective in lower limb amputations. Consequently, symptoms such as
phantom limb pain, reduced dexterity and impaired balance tend to
be more persistent (14).
Conversely, limb salvage reduces the risk of
long-term complications, such as cardiovascular diseases and
arterial disease (29). Although not
always possible, the use of tools such as vascular shunts can
extend the time window for intervention (30). Additionally, the use of grafts as in
the case in the present study, both anatomical and
extra-anatomical, can improve the condition of the patient until
the definitive intervention (31),
preserving the affected limb and resulting in lower rates of future
reinterventions (32).
In the patient in the present study, factors such as
a young age and the absence of comorbidities supported the decision
to manage the vascular injury with a damage control approach. This
choice was based on the greater capacity of the patient for
recovery and tissue regeneration. The literature emphasizes that
damage control techniques can be particularly beneficial in such
cases, as they allow for the restoration of distal perfusion
through temporary vascular shunts prior to definitive
revascularization. This is particularly relevant when the duration
of ischemia is <6 h (2,33), as observed in the patient in the
present study. Indeed, reports of similar cases have described
favorable outcomes with the use of damage control strategies in
young patients. In a previously documented case, a young male
patient sustained severe vascular trauma following a shark attack,
resulting in multiple fractures of his right pelvic limb and
hemorrhage leading to hypovolemic shock (34). Following initial management, a damage
control approach was selected, with intervention on the popliteal
artery and vein. Following reconstruction, limb functionality was
preserved without neurological or vascular deficits (34). Similarly, another study described the
case of a young female patient who sustained a tibia and fibula
fracture in her left leg after being struck by a vehicle; in that
case, limb preservation was achieved through direct vascular repair
of the popliteal vessels (35).
Likewise, in another study, a 33-year-old male presented with a
Gustilo-Anderson type IIIA fracture of the distal tibia and fibula,
accompanied by a closed calcaneus fracture and tibial nerve
transection (36). Although
amputation was considered, the decision was made to preserve the
limb using a nerve allograft. At 29 months of post-operative
follow-up, the patient demonstrated satisfactory functional
recovery without the need for major revision, grafting, arthrodesis
or amputation (36).
Furthermore, in support of the damage control
approach, a recent meta-analysis found that patients who underwent
limb salvage demonstrated improved psychological well-being
compared to those who underwent amputations, despite the
possibility of reinterventions and a prolonged recovery period
(37). Additionally, the Lower
Extremity Assessment Project (LEAP) study revealed that although
long-term functional outcomes may be similar between both
strategies, limb reconstruction is generally preferred by patients
due to the negative psychosocial effects of amputation, which
include depressive disorders and anxiety (38).
Moreover, while immediate amputation reduces the
risk of developing late complications, such as infections and
multiple reinterventions, recent research has highlighted that the
use of temporary vascular shunts and delayed revascularization can
significantly improve the success rate of limb salvage without
compromising patient safety (33).
There is evidence to suggest that careful selection of candidates
for the damage control strategy can optimize outcomes, avoiding the
adverse consequences associated with amputation, such as phantom
limb pain and difficulty adapting to prostheses (23).
However, it is important to acknowledge the inherent
risks associated with this approach, many of which arise during the
procedure itself. Among the most frequent complications are
vascular thrombosis, infections and the development of anastomotic
stenosis, all of which can jeopardize limb viability (39). Fortunately, in the case described
herein, the use of heparin and the close monitoring of the progress
of the patient reduced the risk of thrombosis during the
intraoperative period until the definitive surgical approach could
be implemented. Moreover, the risk of anastomotic stenosis can be
mitigated through surgical techniques, such as balloon angioplasty,
stent placement, or the use of temporary shunts in selected cases.
These shunts help prolong vascular patency (40), which is why these were implemented in
the patient in the present study, facilitating stabilization and
enabling a subsequent definitive intervention.
In conclusion, based on the evidence presented, the
damage control strategy emerges as a highly favorable approach in
cases of acute vascular injury, balancing the risks and benefits
associated with limb salvage. Finally, it is noteworthy that the
patient exhibited satisfactory progress 3 months following the
intervention, at which point full limb functionality was restored
with no apparent clinical deficits. Despite this positive outcome,
future studies should consider longer follow-up periods and imaging
evaluations to assess the long-term efficacy of the damage control
strategy.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contribution
SMPS, EAMR and FSS participated equally in the
preparation of this manuscript, both in the medical care process of
the patient and during data collection, as well as in the
literature search, information synthesis, and in the writing of
this manuscript. SMPS and EARM confirm the authenticity of all the
raw data described in this manuscript. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The present study was performed in accordance with
the ethical standards of the Declaration of Helsinki, 1964.
Informed consent was obtained from the patient for his inclusion in
the study. Ethics approval was waived by the local committee as no
personal data were used.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hundersmarck D, Hietbrink F, Leenen LPH,
De Borst GJ and Heng M: Blunt popliteal artery injury following
tibiofemoral trauma: Vessel-first and bone-first strategy. Eur J
Trauma Emerg Surg. 48:1045–1053. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Agarwal P, Kukrele R and Sharma D: Delayed
revascularization of extremities following vascular injuries:
Challenges and outcome. J Orthop. 35:31–36. 2022.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Herrera MA, Millán M, Del Valle AM,
Betancourt-Cajiao M, Caicedo Y, Caicedo I, Gallego LM, Rivera D,
Parra MW and Ordoñez CA: Damage control of peripheral vascular
trauma-don't be afraid of axillary or popliteal fosses. Colomb Med
(Cali). 52(e4114735)2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Himura H, Uchida K, Miyashita M and
Mizobata Y: Successful limb salvage beyond the golden time
following blunt traumatic open complete transection of the femoral
artery and vein in a patient with cardiac arrest: A case report.
Surg Case Rep. 7(177)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Potter HA, Alfson DB, Rowe VL, Wadé NB,
Weaver FA, Inaba K, O'Banion LA, Siracuse JJ and Magee GA:
Endovascular versus open repair of isolated superficial femoral and
popliteal artery injuries. J Vasc Surg. 74:814–822.e1.
2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Priyadarshini P, Kaur S, Gupta K, Kumar A,
Alam J, Bagaria D, Choudhary N, Gupta A, Sagar S, Mishra B and
Kumar S: Protocolized approach saves the limb in peripheral
arterial injury: A decade experience. Chin J Traumatol. 28:62–68.
2025.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Liu G, Chen J and Xiang Z: Five-year
outcomes of trauma-specific function in patients after acute blunt
popliteal artery injury: A matched cohort analysis. J Orthop Surg
Res. 17:256–264. 2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Melton SM, Croce MA, Patton JH Jr,
Pritchard FE, Minard G, Kudsk KA and Fabian TC: Popliteal artery
trauma. Systemic anticoagulation and intraoperative thrombolysis
improves limb salvage. Ann Surg. 225:518–529. 1997.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Semaan E, Hamburg N, Nasr W, Shaw P,
Eberhardt R, Woodson J, Doros G, Rybin D and Farber A: Endovascular
management of the popliteal artery: Comparison of atherectomy and
angioplasty. Vasc Endovascular Surg. 44:25–31. 2010.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Kleinsorge GHD, Teixeira PGR, Pfannes CCB,
do Lago RDV and Abib SCV: Prognostic factors in treatment of
traumatic femoropopliteal arterial injuries at a Brazilian trauma
center. J Vasc Bras. 21(e20220020)2022.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Lian WS, Das SK, Hu XX, Zhang XJ, Xie XY
and Li MQ: Efficacy of intra-arterial catheter-directed
thrombolysis for popliteal and infrapopliteal acute limb ischemia.
J Vasc Surg. 71:141–148. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Dua A, Patel B, Desai SS, Holcomb JB, Wade
CE, Coogan S and Fox CJ: Comparison of military and civilian
popliteal artery trauma outcomes. J Vasc Surg. 59:1628–1632.
2014.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Nguyen A, Tiziano T, Beckermann J,
Wildenberg J and Carmody T: Endovascular repair of a traumatic
popliteal artery injury. Cureus. 14(e31100)2022.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Garge S, Vyas P, Rathod K, Jaggi S and
Talwar I: Leaking pseudoaneurysm of lower limb saphenous vein
graft: A rare complication and its successful treatment by
endovascular embolization. BJR Case Rep. 3(20150445)2016.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Edwards J, Treffalls RN, Abdou H, Stonko
DP, Walker PF and Morrison JJ: Lower extremity staged
revascularization (LESR) as a new innovative concept for lower
extremity salvage in acute popliteal artery injuries: A hypothesis.
Patient Saf Surg. 16(39)2022.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Feliciano DV: Long-term intra-arterial
shunt. Trauma Surg Acute Care Open. 5(e000486)2020.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Golledge J: Surgical
revascularization-best for limb ischemia? N Engl J Med.
387:2377–2378. 2022.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Ratnayake AS, Bala M, Fox CJ, Jayatilleke
AU, Thalgaspitiya SPB and Worlton TJ: A critical appraisal of
impact of compounding factors in limb salvage decision making in
combat extremity vascular trauma. BMJ Mil Health. 168:368–371.
2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Urrechaga E, Jabori S, Kang N,
Kenel-Pierre S, Lopez A, Rattan R, Rey J and Bornak A: Traumatic
lower extremity vascular injuries and limb salvage in a civilian
urban trauma center. Ann Vasc Surg. 82:30–40. 2022.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Bunn C, Kulshrestha S, Di Chiaro B,
Maduekwe U, Abdelsattar ZM, Baker MS, Luchette FA and Agnew S: A
leg to stand on: Trauma center designation and association with
rate of limb salvage in patients suffering severe lower extremity
injury. J Am Coll Surg. 233:120–129.e5. 2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Shishehbor MH, White CJ, Gray BH, Menard
MT, Lookstein R, Rosenfield K and Jaff MR: Critical limb ischemia:
An expert statement. J Am Coll Cardiol. 68:2002–2015.
2016.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fluck F, Augustin AM, Bley T and Kickuth
R: Current treatment options in acute limb ischemia. Rofo.
192:pp319–326. 2020.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Nayar SK, Alcock HMF and Edwards DS:
Primary amputation versus limb salvage in upper limb major trauma:
A systematic review. Eur J Orthop Surg Traumatol. 32:395–403.
2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Panhelleux B, Shalhoub J, Silverman AK and
McGregor AH: A review of through-knee amputation. Vascular.
30:1149–1159. 2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Schober TL and Abrahamsen C: Patient
perspectives on major lower limb amputation-a qualitative
systematic review. Int J Orthop Trauma Nurs.
46(100958)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Littman AJ, Thompson ML, Arterburn DE,
Bouldin E, Haselkorn JK, Sangeorzan BJ and Boyko EJ: Lower-limb
amputation and body weight changes in men. J Rehabil Res Dev.
52:159–170. 2015.PubMed/NCBI View Article : Google Scholar
|
|
27
|
AlMehman DA, Faden AS, Aldahlawi BM,
Bafail MS, Alkhatieb MT and Kaki AM: Post-amputation pain among
lower limb amputees in a tertiary care hospital in Jeddah, Saudi
Arabia: A retrospective study. Saudi Med J. 43:187–96.
2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Ülger Ö, Yıldırım Şahan T and Çelik SE: A
systematic literature review of physiotherapy and rehabilitation
approaches to lower-limb amputation. Physiother Theory Pract.
34:821–834. 2018.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Zhu Y, Wu X, Zhang W and Zhang H:
Limb-salvage surgery versus extremity amputation for early-stage
bone cancer in the extremities: A population-based study. Front
Surg. 10(1147372)2023.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Barros D'Sa AAB, Harkin DW, Blair PHB,
Hood JM and McIlrath E: The belfast approach to managing complex
lower limb vascular injuries. Eur J Vasc Endovasc Surg. 32:246–256.
2006.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Di Primio M, Angelopoulos G, Lazareth I,
Priollet P, Zins M, Emmerich J and Yannoutsos A: Innovative
endovascular approach for limb salvage in critical limb ischemia. J
Med Vasc. 45:23–27. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Sousa RS, Oliveira-Pinto J and Mansilha A:
Endovascular versus open repair for popliteal aneurysm: A review on
limb salvage and reintervention rates. Int Angiol. 39:381–389.
2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Qureshi MK, Ghaffar A, Tak S and Khaled A:
Limb salvage versus amputation: A review of the current evidence.
Cureus. 12(e10092)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Khalil A: Patient survival and limb
salvage after shark attack with major vascular injury: A case
report. Chin J Traumatol. 24:401–403. 2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Giordano V, Souza FS, Belangero WD and
Pires RE: Limb salvage after lower-leg fracture and popliteal
artery transection-the role of vessel-first strategy and bone
fixation using the ilizarov external fixator device: A case report.
Medicina (Kaunas). 57(1220)2021.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Mercer DM, Nguyen HM, Curtis W, Heifner JJ
and Chafey DH: Consideration for limb salvage in place of
amputation in complex tibial fracture with neurovascular injury: A
case report. Iowa Orthop J. 43:20–24. 2023.PubMed/NCBI
|
|
37
|
Serlis A, Sgardelis P, Vampertzis T,
Rizavas K, Poulios P and Konstantopoulos G: Complex limb injuries:
Limb salvage versus amputation-a mini review and meta-analysis. Adv
Orthop. 2025(2884802)2025.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Okereke I and Abdelfatah E: Limb salvage
versus amputation for the mangled extremity: Factors affecting
decision-making and outcomes. Cureus. 14(e28153)2022.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Harnarayan P, Islam S, Harnanan D, Bheem V
and Budhooram S: Acute upper limb ischemia: Prompt surgery and
long-term anticoagulation prevent limb loss and debilitation. Vasc
Health Risk Manag. 17:489–495. 2021.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Mejia D, Warr SP, Delgado-López CA,
Salcedo A, Rodríguez-Holguín F, Serna JJ, Caicedo Y, Pino LF,
González-Hadad A, Herrera MA, et al: Reinterventions after damage
control surgery. Colomb Med (Cali). 52(e4154805)2021.PubMed/NCBI View Article : Google Scholar
|