Introduction
General anesthesia (GA) poses significant risks,
particularly related to inadequate ventilation (1,2), which
accounts for 40% of anesthesia-related deaths (3). According to the Fourth National Audit
Project (NAP4), intraoperative hypoxia is fatal in 12% of these
cases, while an additional 9% of patients succumb post-operatively
(4). Among the survivors, 25%
experience severe complications, such as cerebral hypoxia,
pulmonary edema, or cardiorespiratory arrest (5). Furthermore, the study by Cumberworth
et al (6) reported a global
complication rate of 0.028%, with an average of 46 intensive care
unit admissions per million procedures. Several factors further
exacerbate ventilation challenges during GA, including obesity,
maxillary hypoplasia, macroglossia and cervical instability
(7,8). Additionally, conditions such as cancer
and hypotension contribute to increased peri-operative risks
(9,10).
The American Society of Anesthesiologists (ASA)
(2) defines a difficult airway (DA)
as a situation in which an anesthesiologist is unable to provide
adequate ventilation despite the proper use of techniques and
ventilation devices (11,12). It is estimated that DA occurs in 1.2
to 3.8% of adults undergoing GA (13), with this prevalence rising to as high
as 22% in certain populations (14-16).
Additionally, NAP4 reports that mask ventilation fails in 1 out of
1,500 attempts, while endotracheal intubation is unsuccessful in 1
out of 2,000 procedures. The ‘cannot intubate, cannot ventilate’
scenario occurs in 1 out of every 5,000 patients, often with severe
consequences (17).
Although predictive indexes for DA exist, some
patients experience unexpected ventilation difficulties,
necessitating intubation (18,19).
Intubation involves inserting a tracheal tube through the mouth or
nose and is commonly performed during GA (20). The standard protocol utilizes
laryngoscopes with a Macintosh blade, achieving a success rate of
44 to 87% (21). However,
alternative techniques have been developed for patients with DA
(22), including video stylets and
video laryngoscopes, which enable the continuous monitoring of the
hypopharynx during tracheal tube insertion into the glottis
(23).
Video laryngoscopy enhances visualization in
patients with a DA and increases the success rate of first-attempt
intubation (24), while also
reducing the incidence of hypoxemia (20). Additionally, it is associated with a
lower risk of sympathetic overstimulation and traumatic injury
(23). However, the use of personal
protective equipment during the COVID-19 pandemic posed challenges
for intubation with this technique, prolonging the procedure and
leading to the increased adoption of optical stylet (OS)-based
techniques (25).
The OS is an instrument derived from lighted
stylets, originally introduced by Berci and Katz (26) in 1979 for endotracheal intubation.
This device ranges in length from 42 to 80 cm, with an average
diameter of 5.5 to 10 mm. It consists of a long, slender body
through which the endotracheal tube is inserted. Additionally, a
small video camera positioned at the tip of the stylet captures and
transmits images to an integrated monitor (27). The OS allows for intubation to be
performed either by a single operator or with assistance (28). Due to its enhanced maneuverability,
accessibility and lower cost, the OS is currently recommended for
patients with a DA (29,30).
A wide variety of OS devices are currently
available, differing in optical and morphological features, tip
angulation and flexibility (31).
Its clinical use has been validated through a well-documented case
series, each incorporating slight modifications to the technique.
Currently, several variations of the original approach of Dr
Bonfils' exist, including those proposed by Halligan and Chartres
(32), both of which have proven
effective in patients with a DA. Despite the advantages of OS for
intubation, its use remains limited in the current setting.
Therefore, the present study describes the case of a patient with a
predicted DA who was successfully intubated using an OS in
combination with the pharyngeal clearance technique and a
laryngoscope.
Case report
The present study describes the case of a
61-year-old female patient who was treated at the High Specialty
Medical Unit (UMAE), Mexican Institute of Social Security (IMSS),
97150 Mérida, Mexico with a history of type 2 diabetes mellitus and
systemic arterial hypertension, for which she was undergoing
treatment. She had been diagnosed with papillary thyroid carcinoma
in 2018 and underwent a modified right neck dissection followed by
adjuvant radiotherapy in 34 sessions. Since then, she had been on
hormone replacement therapy with 150 µg oral levothyroxine per day.
Additionally, she had undergone a bilateral modified radical
axillary dissection in 2022 and a parotid tail resection in 2023,
both without complications.
The patient was scheduled for a radical neck tumor
resection due to the recurrence of papillary thyroid carcinoma. A
physical examination revealed the following vital signs: Blood
pressure, 177/79 mmHg; respiratory rate, 20 breaths/min; heart
rate, 66 bpm; temperature, 37.1˚C, oxygen saturation
(SpO2), 97%; body weight, 67 kg; height, 1.38 m; and
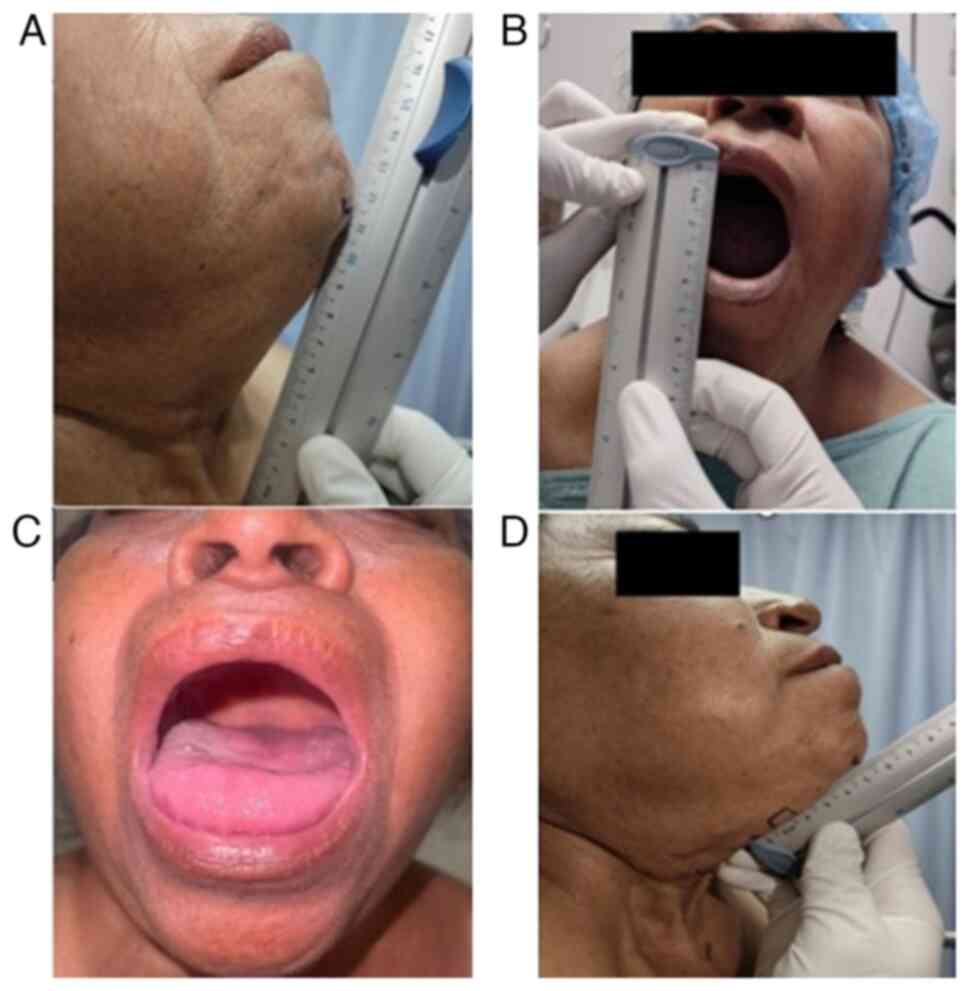
body mass index, 35.2 kg/m². Airway assessment revealed incomplete
dentition, a normal-sized tongue with restricted movement and
protrusion, Mallampati III, Patil-Aldreti III (5.5 cm),
sternomental distance III (11.5 cm), and interincisal distance I
(3.5 cm) (Fig. 1). The Bellhouse-
Doré classification was II (one-third mobility), and the Brodsky
index was negative (34 cm).
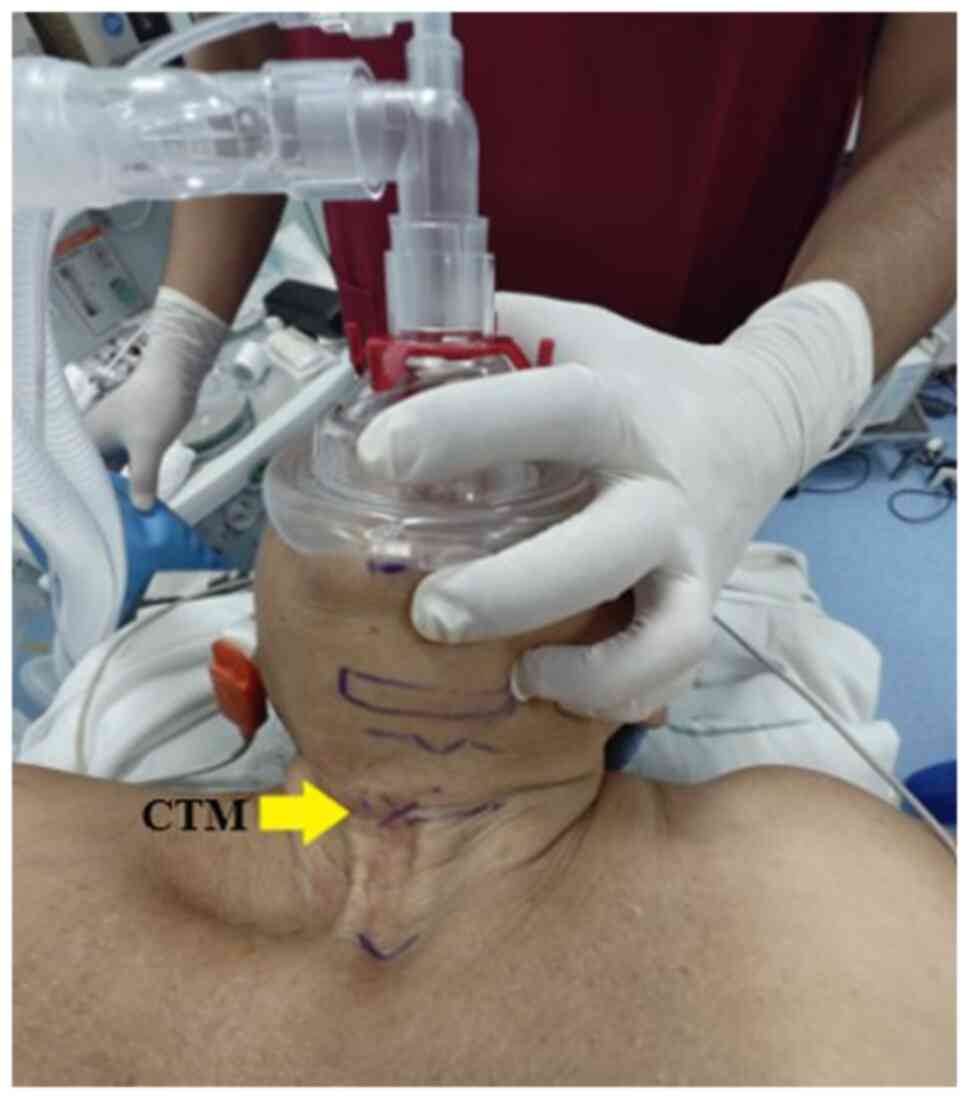
Additionally, the neck exhibited surgical scars and
signs of post-radiation fibrosis, which limited proper cervical
extension (Fig. 2). Laryngeal
structures were difficult to palpate, prompting an ultrasound
examination to identify and mark the cricothyroid membrane with a
clip using a linear probe in both longitudinal and transverse
planes (Fig. 3).
Based on these findings, the surgical and anesthetic
risk was classified as E3B, ASA III. A plan for balanced general
anesthesia with invasive monitoring was established, incorporating
airway management using a flexible intubation OS. Following
thorough equipment and instrument check, the patient was
transferred to the operating room, placed in the supine position
and connected to continuous vital signs monitoring. Preoxygenation
was then performed using a sealed facial mask with a tidal volume
technique and 100% FiO2 for 3 min. For anxiolysis, 1.5
mg intravenous (IV) midazolam PiSA® were administered,
followed by 250 µg IV fentanyl PiSA®, 100 mg IV
lidocaine PiSA® and 35 mg IV rocuronium
PiSA®.
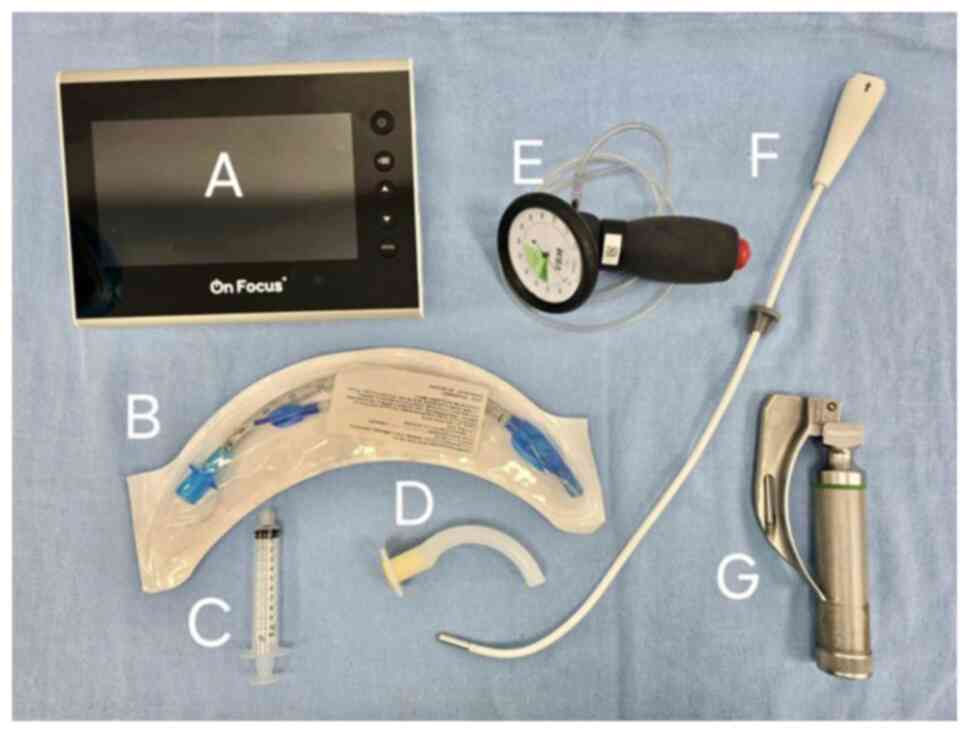
Anesthesia induction was achieved with 60 mg IV
propofol (ALVARTIS PHARMA®). Upon obtaining entropy
values of RE-49 and SE-45 with a train-of-four (TOF) ratio of 24%,
the operator inserted a Mac 3 laryngoscope blade into the oral
cavity using the non-dominant (left) hand to displace the tongue.
With the dominant (right) hand, a flexible OS with a diameter of 5
mm, preloaded with a 6.5-mm internal diameter flexible metallic
tube with a cuff, was introduced via the right retromolar approach
(Fig. 4). An epiglottoscopy was
performed, and once the glottis was visualized and identified, the
tube was smoothly advanced into the trachea on the first attempt
using the pharyngeal clearance technique with laryngoscopy. The
procedure was atraumatic, and cuff inflation was achieved with a
pressure of 30 cm H2O, confirmed by manometry (Fig. 5). The tube was then connected to
mechanical ventilation, and proper positioning was verified through
capnography and lung field auscultation
The surgical procedure was initiated with desflurane
maintained at a minimum alveolar concentration of 0.8-0.9, an IV
fentanyl PiSA® infusion at 2-4 µg/kg/h (total, 300 µg)
and a 2% IV lidocaine PiSA® infusion at 1-2 mg/kg/h
(total, 240 mg). Adjunct medications included 1 g IV paracetamol
KENER® and 2 g IV cefotaxime AMSA®.
Intraoperative blood loss was 30 ml, with a urine
output of 1 ml/kg/h. Fluid management consisted of 1,000 ml
Hartmann's solution and 500 ml 0.9% sodium chloride (NaCl)
PiSA®, resulting in a total intake of 1,500 ml and a net
positive balance of +140 ml. Following the procedure, the patient
remained hemodynamically stable, with a mean arterial pressure of
75-80 mmHg, a heart rate of 65 bpm, a respiratory rate of 12
breaths/min, a temperature of 35.8˚C and an SpO2 of
100%. Secretions were gently aspirated.
Emergence was achieved through metabolic lysis, with
effective spontaneous ventilation, the recovery of protective
airway reflexes, entropy values of RE-93 and SE-92, a TOF ratio
>90%, an appropriate response to verbal command, and spontaneous
eye opening. The patient was extubated awake without
complications.
The emergence was resolved through metabolic lysis,
with effective spontaneous ventilation, recovery of protective
airway reflexes, entropy values of RE-93 and SE-92, a TOF ratio
>90%, an appropriate response to verbal commands, and
spontaneous eye opening. The patient was extubated awake without
complications.
Discussion
The present study describes the case of a
61-year-old patient with predictors of a DA using a flexible OS and
the pharyngeal clearance technique with laryngoscopy. The clinical
characteristics of the patient reflect common sequelae of neck
surgery and skin changes due to fibrosis secondary to radiotherapy,
which restricts cervical extension. For these reasons, anesthetic
protocols should always incorporate alternative strategies for
cases in which traditional intubation techniques fail, with the OS
being one of the recommended tools for patients with an anticipated
DA (33).
The OS is one of several nonconventional intubation
devices, along with blade laryngoscopes, optical bougies and
stylets. These devices have been widely developed in recent years
due to their ease of use and enhanced durability. They are
available in rigid, semi-malleable and hybrid varieties, the latter
being partially rigid and partially flexible (34). Initially, the most commonly used OS
intubation technique was proposed by Dr Bonfils. In this method,
the device was pre-treated with an anti-fog solution on the distal
lens and preloaded with the endotracheal tube. It was then inserted
through the retromolar region of the right cheek until reaching the
posterior molars. At this point, the OS was redirected toward the
midline to visualize the uvula, followed by the epiglottis and then
the glottic opening, where the tube was smoothly advanced into the
trachea (26).
Subsequently, Halligan and Charters (32) proposed several maneuvers to
facilitate the use of the Bonfils OS. These maneuvers involved
inserting the non-dominant hand into the mouth of the patient to
apply forward traction on the mandible and, if necessary, on the
tongue as well. This was followed by an external mandibular
subluxation maneuver with maximal head extension. If these
techniques failed to clear the airway, direct laryngoscopy was
performed as a pharyngeal clearance strategy (32).
However, the integration of the OS into High
Specialty Medical Unit (UMAE) s relatively recent, as direct and
video laryngoscopy remain the standard alternatives for managing
predicted DA. It is important to emphasize that, given the high
prevalence of DA among in the patients treated at the UMAE (most of
whom have oncological conditions) airway management plays a
critical role in their prognosis and is a key aspect of our daily
practice. To ensure proficiency with this technique, induction
workshops using the OS were conducted with mannequins prior to its
application in actual patients, allowing operators to improve their
learning curve, as stated in previous research (35).
The OS is considered a non-conventional intubation
method that, compared to direct laryngoscopy, induces less
autonomic stimulation. Additionally, it provides several
advantages, including greater portability, ease of disinfection, a
short learning curve, lower cost and the ability to displace tumors
in the oral cavity. These features contribute to its high
first-attempt success rate (36),
rendering it a safe and effective alternative comparable to
ultrasound-guided techniques (37).
Moreover, recent studies have highlighted its
superior utility over conventional methods. According to the study
by Zhang et al (38), this
technique enabled successful intubation in a patient who
unexpectedly presented with a DA secondary to cervical
hyperostosis. Similarly, Yang et al (39) described the case of a middle-aged
male patient with multiple comorbidities who developed hypoxemia
during an acute episode of COVID-19 and was successfully intubated
and stabilized using this technique. Additionally, a series of
cases involving patients with neck trauma who required cervical
immobilization and encountered difficulties being intubated with a
video laryngoscope were reported. As a result, the video stylet was
used, and success in intubation was achieved due to its lower
requirement for cervical manipulation (40).
It is important to highlight that the success of
intubation reported herein could be further optimized by
determining the average intubation time, allowing for an objective
comparison with other methods. In this regard, Jhuang et al
previously published a case series analyzing this parameter,
reporting a duration range of 6 to 11 sec (41). Therefore, future studies evaluating
the effectiveness of the OS are required to include the measurement
of average intubation time, providing objective data that support
the routine adoption of this instrument.
In conclusion, the integration of the OS into
routine airway management for patients with a DA represents a
promising strategy to improve clinical outcomes. As the prevalence
of patients with comorbidities and prior surgical histories
continues to increase, factors that significantly increase the
complexity of ventilation during surgery, the OS stands out as an
optimal alternative. Its adoption could enhance airway management
protocols, contributing to safer and more effective anesthetic
procedures.
Acknowledgements
The authors of the present study would like to
express their gratitude to the institutions of the High Specialty
Medical Unit (UMAE), Mexican Institute of Social Security (IMSS),
‘Ignacio García Tellez’ and the Autonomous University of Yucatán
Universidad (UADY) for their moral and logistical support.
Additionally, personal gratitude is extended to Dr Jimmy Gabriel
Rivas Alpuche from our institution (UMAE) for providing the
necessary instruments for this clinical case.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AIBG, JGRA, HENG, LHWS, CMAL and PAAS participated
equally in the preparation of this manuscript, both in the medical
care process of the patient and during data collection, as well as
in the literature search, information synthesis and in the writing
of this manuscript. AIBG and JGRA confirm that the authenticity of
all the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was performed in accordance with
the ethical standards of the Declaration of Helsinki, 1964.
Informed consent was obtained from the patient for inclusion in the
study. Ethics approval was waived by the local committee as no
personal data was used.
Patient consent for publication
Written informed consent was obtained from the
patient for the publication of the present case report and any
related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
le Roux JJ, Wakabayashi K and Jooma Z:
Defining the role of thoracic spinal anaesthesia in the 21st
century: A narrative review. Br J Anaesth. 130:e56–e65.
2023.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Apfelbaum JL, Hagberg CA, Caplan RA, Blitt
CD, Connis RT, Nickinovich DG, Caplan RA, Benumof JL, Berry FA,
Blitt CD, et al: Practice guidelines for management of the
difficult airway: An updated report by the American Society of
Anesthesiologists Task Force on Management of the Difficult Airway.
Anesthesiology. 118:251–270. 2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Downey AW, Duggan LV and Adam LJ: A
systematic review of meta-analyses comparing direct laryngoscopy
with video laryngoscopy. Can J Anesth. 68:706–714. 2021.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cook TM, Woodall N and Frerk C: Fourth
National Audit Project. Major complications of airway management in
the UK: Results of the Fourth National Audit Project of the Royal
College of Anaesthetists and the Difficult Airway Society. Part 1:
Anaesthesia. Br J Anaesth. 106:617–631. 2011.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Apfelbaum JL, Hagberg CA, Connis RT,
Abdelmalak BB, Agarkar M, Dutton RP, Fiadjoe JE, Greif R, Klock PA,
Mercier D, et al: 2022 American society of anesthesiologists
practice guidelines for management of the difficult airway.
Anesthesiology. 136:31–81. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Cumberworth A, Lewith H, Sud A, Jefferson
H, Athanassoglou V and Pandit JJ: Major complications of airway
management: A prospective multicentre observational study.
Anaesthesia. 77:640–648. 2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Başpınar ŞM, Günüşen İ, Sergin D, Sargın A
and Balcıoğlu ST: Evaluation of anthropometric measurements and
clinical tests in the diagnosis of difficult airway in patients
undergoing head and neck surgery. Turk J Med Sci. 52:730–740.
2022.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Roth D, Pace NL, Lee A, Hovhannisyan K,
Warenits AM, Arrich J and Herkner H: Airway physical examination
tests for detection of difficult airway management in apparently
normal adult patients. Cochrane Database Syst Rev.
5(CD008874)2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Mosier JM, Joshi R, Hypes C, Pacheco G,
Valenzuela T and Sakles JC: The physiologically difficult airway.
West J Emerg Med. 16:1109–1117. 2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Iseli TA, Iseli CE, Golden JB, Jones VL,
Boudreaux AM, Boyce JR, Weeks DM and Carroll WR: Outcomes of
intubation in difficult airways due to head and neck pathology. Ear
Nose Throat J. 91:E1–E5. 2012.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Leong SM, Tiwari A, Chung F and Wong DT:
Obstructive sleep apnea as a risk factor associated with difficult
airway management-A narrative review. J Clin Anesth. 45:63–68.
2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Jain K, Yadav M, Gupta N, Thulkar S and
Bhatnagar S: Ultrasonographic assessment of airway. J Anaesthesiol
Clin Pharmacol. 36:5–12. 2020.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Cattano D, Panicucci E, Paolicchi A,
Forfori F, Giunta F and Hagberg C: Risk factors assessment of the
difficult airway: An Italian survey of 1956 patients. Anesth Analg.
99:1774–1779. 2004.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Frerk C, Mitchell VS, McNarry AF, Mendonca
C, Bhagrath R, Patel A, O'Sullivan EP, Woodall NM and Ahmad I:
Difficult Airway Society Intubation Guidelines Working Group.
Difficult Airway Society 2015 guidelines for management of
unanticipated difficult intubation in adults. Br J Anaesth.
115:827–848. 2015.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Chhina AK, Jain R, Gautam PL, Garg J,
Singh N and Grewal A: Formulation of a multivariate predictive
model for difficult intubation: A double blinded prospective study.
J Anaesthesiol Clin Pharmacol. 34:62–67. 2018.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Carsetti A, Sorbello M, Adrario E, Donati
A and Falcetta S: Airway ultrasound as predictor of difficult
direct laryngoscopy: A systematic review and meta-analysis. Anesth
Analg. 134:740–750. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
NAP4: Major complications of airway
management in the United Kingdom: Reports and findings March 2011.
4th National Audit Project of The Royal College of Anaesthetists
and The Difficult Airway Society, 2011.
|
|
18
|
Jagannathan N and Asai T: Difficult airway
management: Children are different from adults, and neonates are
different from children! Br J Anaesth. 126:1086–1088.
2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Vannucci A and Cavallone LF: Bedside
predictors of difficult intubation: A systematic review. Minerva
Anestesiol. 82:69–83. 2016.PubMed/NCBI
|
|
20
|
Hansel J, Rogers AM, Lewis SR, Cook TM and
Smith AF: Videolaryngoscopy versus direct laryngoscopy for adults
undergoing tracheal intubation: A Cochrane systematic review and
meta-analysis update. Br J Anaesth. 129:612–623. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Kriege M, Alflen C, Tzanova I, Schmidtmann
I, Piepho T and Noppens RR: Evaluation of the McGrath MAC and
Macintosh laryngoscope for tracheal intubation in 2000 patients
undergoing general anaesthesia: The randomised multicentre EMMA
trial study protocol. Br Med J Open. 7(e016907)2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Abdelmalak BB and Doyle DJ: Recent trends
in airway management. F1000Res 9: F1000 Faculty Rev-355, 2020.
|
|
23
|
Lan CH, Luk HN, Qu JZ and Shikani A: An
approach to improve the effectiveness of the video-assisted
intubating stylet technique for tracheal intubation: A case series
report. Healthcare (Basel). 11(891)2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kriege M, Noppens RR, Turkstra T, Payne S,
Kunitz O, Tzanova I and Schmidtmann I: EMMA Trial Investigators
Group. A multicentre randomised controlled trial of the McGrath™
Mac videolaryngoscope versus conventional laryngoscopy.
Anaesthesia. 78:722–729. 2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Huang CH, Su IM, Jhuang BJ, Luk HN, Qu JZ
and Shikani A: Video-assisted stylet intubation with a plastic
sheet barrier, a safe and simple technique for tracheal intubation
of COVID-19 patients. Healthcare (Basel). 10(1105)2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Berci G and Katz R: Optical stylet: An aid
to intubation and teaching. Ann Otol Rhinol Laryngol. 88:828–831.
1979.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hartigan PM, Karamnov S, Gill RR, Ng JM,
Yacoubian S, Tsukada H, Tsukada H, Swanson J, Barlow J, McMurry TL
and Blank RS: Mediastinal masses, anesthetic interventions, and
airway compression in adults: A prospective observational study.
Anesthesiology. 136:104–114. 2022.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Luk HN, Qu JZ and Shikani AP:
Styletubation: The paradigmatic role of video-assisted intubating
stylet technique for routine tracheal intubation. Asian J
Anesthesiol. 61:102–106. 2023.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kohse EK, Siebert HK, Sasu PB, Loock K,
Dohrmann T, Breitfeld P, Barclay-Steuart A, Stark M, Sehner S,
Zöllner C and Petzoldt M: A model to predict difficult airway
alerts after videolaryngoscopy in adults with anticipated difficult
airways-The VIDIAC score. Anaesthesia. 77:1089–1096.
2022.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Chen IW, Li YY, Hung KC, Chang YJ, Chen
JY, Lin MC, Wang KF, Lin CM, Huang PW and Sun CK: Comparison of
video-stylet and conventional laryngoscope for endotracheal
intubation in adults with cervical spine immobilization: A
PRISMA-compliant meta-analysis. Medicine (Baltimore).
101(e30032)2022.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Rudolph C and Schlender M: Clinical
experiences with fiber óptico intubation with the Bonfils
intubation fiberscope. Anaesthesiol Reanim. 21:127–130.
1996.PubMed/NCBI
|
|
32
|
Halligan M and Charters P: A clinical
evaluation of the bonfils intubation fiberscope. Anaesthesia.
1087-1091:2003.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Zaytcev AY, Dubrovin KV and Svetlov VA:
The choice of tracheal intubation method in reconstructive
maxillo-facial surgery with difficult airways. Anesteziol
Reanimatol. 61:173–177. 2017.PubMed/NCBI
|
|
34
|
Mihai R, Blair E, Kay H and Cook TM: A
quantitative review and meta-analysis of performance of
non-standard laryngoscopes and rigid fibreoptic intubation aids.
Anaesthesia. 63:745–760. 2008.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Ma Y, Wang Y, Shi P, Cao X and Ge S:
Ultrasound-guided versus Shikani optical stylet-aided tracheal
intubation: A prospective randomized study. BMC Anesthesiol.
20(221)2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Pius J and Noppens RR: Learning curve and
performance in simulated difficult airway for the novel C-MAC®
video-stylet and C-MAC® Macintosh video laryngoscope: A prospective
randomized manikin trial. PLoS One. 15(e0242154)2020.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Ravindran B: Innovations in the management
of the difficult airway: A narrative review. Cureus.
15(e35117)2023.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Zhang X, Wang J, Liu Y, Li Z and Han B: A
rare case of an unexpected difficult airway management in a diffuse
idiopathic skeletal hyperostosis patient and post-operative airway
evaluation with 3D printing technique. Ann Transl Med.
9(75)2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Yang CP, Luk HN, Qu JZ and Shikani A: The
use of a video-assisted intubating stylet technique in a critically
Ill and contagious COVID-19 patient. Healthcare (Basel).
10(388)2022.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Shih TL, Koay KP, Hu CY, Luk HN, Qu JZ and
Shikani A: The use of the shikani video-assisted intubating stylet
technique in patients with restricted neck mobility. Healthcare
(Basel). 10(1688)2022.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Jhuang BJ, Luk HN, Qu JZ and Shikani A:
Video-twin technique for airway management, combining
video-intubating stylet with videolaryngoscope: A case series
report and review of the literature. Healthcare (Basel).
10(2175)2022.PubMed/NCBI View Article : Google Scholar
|