Introduction
Hope is a critical component of well-being and
quality of life in various health contexts (1-3). In
the realm of cancer, and in disease in general, hope is not only
strongly associated with depression, but is also posited as a
potential prognostic factor (4,5). Given
its potential influence on key health outcomes, hope can be
influenced by numerous factors related to cancer treatment and the
disease itself (6,7). The available literature thus points at
the multifaceted nature of hope, and underlines its multiple
determinants, at the same time showing its clinical importance for
various disease states, either to improve outcomes, improve quality
of life or improve patient adaptation.
In the realm of cancer care, it is essential to
evaluate both the functional capabilities and the psychological
state of patients to deliver personalized treatments and provide
comprehensive support. The Eastern Cooperative Oncology Group
(ECOG) Performance Status is a widely recognized and standardized
tool used to assess the functional ability of a patient and their
capacity to perform everyday activities during cancer therapy
(8). This assessment enables
clinicians to determine appropriate treatment plans and predict
patient outcomes based on functional limitations. Complementarily,
the adult trait hope scale (ATHS) provides a concise yet effective
measure of the inherent hopefulness of an individual by evaluating
their motivational drive and perceived ability to devise strategies
to achieve desired goals (9). The
present study, by integrating these two dimensions of well-being,
functional and psychological, aimed to construct a more
comprehensive image of patient wellness and also explore the
interplay between functional status and hope in the care of
patients with cancer.
Artificial intelligence (AI) has revolutionized the
practice of medicine, providing decision support systems and
prognostic tools (10). However, its
application to measuring hope levels in cancer care remains largely
unexplored. While established hope indexes exist, the utilization
of patient narratives and the data they generate have not been
rigorously examined in this direction (11,12).
Text data are a valuable means of expressing thoughts and emotions,
and AI technology can unearth hidden patterns within these data
that questionnaires may not potentially capture (13,14)
(https://aws.amazon.com/what-is/text-analysis).
However, in oncology in general, text data are not readily
available or usable in predictive models. Thus, in the present
study, the authors trained an AI model using patient-generated text
data to explore the current significance of hope for cancer
patients within their specific health contexts. Additionally, the
present study evaluated whether the AI could predict hope levels
alongside various patient and disease factors, including the ECOG
performance status and scores from the shortened ATHS (s-ATHS).
Patients and methods
Patients, questionnaire administration
and data collection
Over a 6-week period from August 1, 2023, to
September 15, 2023, the present study enrolled consecutive patients
from outpatient clinics in four medical oncology departments at
various treatment centers (Departments of Medical Oncology at
Medical Park Antalya Hospital, Antalya, Turkey; SBU Antalya
Training and Research Hospital, Antalya, Turkey; Necmettin Erbakan
University Hospital (KNEU), Konya, and Vakıf (ASV) Yaşam Hospital,
Antalya, Turkey). Patients attending the outpatient clinics during
this time period were approached by the medical staff, and were
requested to take part in the study and complete the
questionnaires. Data on patients accepting to participate in the
study were collected and analyzed. Ethical committee approval from
a teaching hospital was obtained in July, 2023 (Acceptance no.
2023-162, Antalya Training and Research Hospital, Antalya, Turkey);
the approval was valid for all centers taking place in the study
and the patients verbally consented to the study.
The participating medical centers included two
private and two teaching hospitals (a university hospital and a
research and training hospital), from two different cities (Medical
Park Antalya Hospital, SBU Antalya Training and Research Hospital
and Vakıf (ASV) Yaşam Hospital are in Antalya, Turkey, whereas
Necmettin Erbakan University Hospital is in Konya, Turkey. All
patients provided verbal informed consent and completed a two-page
questionnaire. This questionnaire included questions related to the
hope index, patient demographics, disease characteristics and
treatment-related factors, along with an open-ended question as
follows: ‘What does the word ‘hope’ currently mean to you in your
life? Please describe your general hopes related to treatment and
life, or the absence of such hopes, in a few sentences below’. The
written responses of the patients to this question were evaluated
by the AI model, as detailed in the ‘Artificial intelligence
analysis of text data’ section below. In addition, a 4-item
shortened version of the ATHS (s-ATHS) was also embedded into the
questionnaire, which was shown to be as reliable as the original
12-item version (15). Patients
independently completed the questionnaires, with occasional
assistance from the medical staff. At the end of each day,
questionnaire results were entered into standard databases and
results from different centers were combined at the conclusion of
the study. In order to ensure that the ethical implications of
using AI in sensitive emotional assessments are responsibly
addressed, data privacy and confidentiality were maintained through
secure data storage protocols and anonymization of personal
identifiers prior to analysis.
Artificial intelligence analysis of
text data
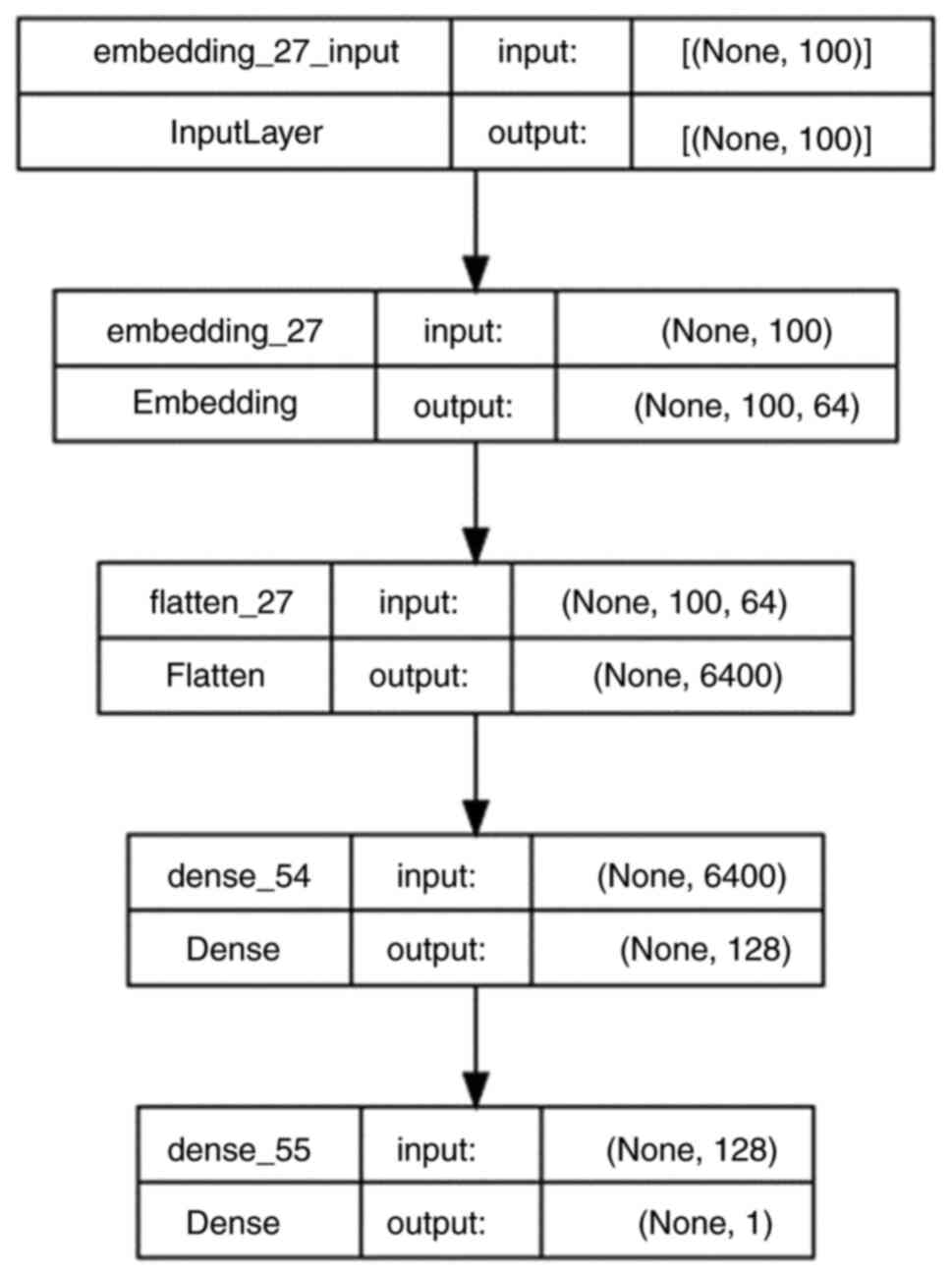
The authors developed a deep neural network and
trained it on patient-generated text data and manually labeled hope
scores on a 10-point scale. In order to establish this, one author
(HŞB) assigned hope scores, as blinded to the s-ATHS scores, to all
patient text responses, which were then cross-validated by the
other authors. The resultant neural network model was saved and
then used to forecast individual AI-predicted hope levels for each
participant. The AI code was written in Python and utilized
libraries such as TensorFlow, Pandas, NumPy and NLTK (https://www.tensorflow.org; https://pandas.pydata.org; https://numpy.org, https://www.nltk.org). Text preprocessing included
importing Turkish stop words from the NLTK library, converting the
text to lowercase, and removing special characters and digits using
regular expressions. Model accuracy was evaluated using the mean
absolute error (MAE) and root mean squared error (RMSE) (16). The deep neural network consisted of
five sequential layers from the Keras library and was trained for
80 epochs with a batch size of 256 (https://keras.io).
Data were split into 80% for training and 20% for validation. The
deep neural network structure is depicted in Fig. 1.
Statistical analysis
Hope index scores (s-ATHS), calculated using
standard methodology, were predicted through both univariate and
multivariate gamma regression analysis. s-ATHS was subjected to
logarithmic transformation due to the highly skewed nature of the
response variable. Gamma regression was chosen for the regression
analysis due to the fact that response variable was continuous,
strictly positive, and skewed, even after log transformation.
Independent variables included various patient, disease, and
treatment factors, along with AI-predicted hope levels. Separate
generalized linear models were constructed for each analysis.
Variables with a P-value <0.10 in the univariate analyses were
then included in the multivariate analyses; P-values <0.05 were
considered to indicate statistically significant differences. SPSS
21.0 was employed for gamma regression analysis (https://www.ibm.com/spss).
Results
General characteristics
Out of the 475 recruited patients with cancer, 461
with complete data were used for AI model training and subsequent
statistical analyses. The majority of the patients were female
(57.7%), with a median age of 59 years. Metastatic disease was
present in 42.1% of the patients. Breast, lung and colorectal
cancer patients comprised 37.6% of cases, and the remaining
majority of cases had varied solid cancers apart from breast, lung
and colorectal cancers. The median s-ATHS score was 26 on a scale
of 32, while AI-predicted hope levels had a median of 7.3 on a
10-point scale, with a RMSE of 1.5. The detailed patient
characteristics are presented in Table
I.
 | Table IPatient demographics. |
Table I
Patient demographics.
| Characteristic | No. of patients | % | Median | Mean | Minimum | Maximum |
|---|
| Total no. of
patients | 461 | 100 | | | | |
| Center | | | | | | |
|
Antalya
Training and Research Hospital | 220 | 47.7 | | | | |
|
Antalya
Medical Park Hospital | 49 | 10.6 | | | | |
|
Konya
Necmettin Erbakan University | 124 | 26.9 | | | | |
|
Antalya
Vakıf Yaşam Hospital | 68 | 14.8 | | | | |
| Sex | | | | | | |
|
Female | 266 | 57.7 | | | | |
|
Male | 195 | 42.3 | | | | |
| Age, years | | | 59 | 57.7 | 21 | 87 |
| ECOG performance
status | | | 1 | 1.5 | 0 | 4 |
| Education | | | | | | |
|
Primary or
secondary school | 261 | 56.6 | | | | |
|
Lycee | 88 | 19.1 | | | | |
|
University | 112 | 24.3 | | | | |
| Income | | | | | | |
|
Poor | 120 | 26 | | | | |
|
Average | 325 | 70.5 | | | | |
|
High | 15 | 3.3 | | | | |
| Marital status | | | | | | |
|
Married | 360 | 78.1 | | | | |
|
Not
married | 101 | 21.9 | | | | |
| Type of cancer | | | | | | |
|
Breast
cancer | 81 | 17.6 | | | | |
|
Lung
cancer | 45 | 9.8 | | | | |
|
Colorectal
cancer | 47 | 10.2 | | | | |
|
Other types
of cancer | 288 | 62.5 | | | | |
| Disease stage | | | | | | |
|
1 to 3 | 267 | 57.9 | | | | |
|
4 | 194 | 42.1 | | | | |
| Time since
diagnosis | | | | | | |
|
<6
months | 146 | 31.7 | | | | |
|
6 to 12
months | 101 | 21.9 | | | | |
|
>1
year | 214 | 46.4 | | | | |
| Treatment
status | | | | | | |
|
Active
treatment | 363 | 78.7 | | | | |
|
No active
treatment | 98 | 21.3 | | | | |
| Expression of
feelings | | | 3 | 2.8 | 1 | 4 |
|
s-ATHS
score | | | 26 | 24.5 | 0 | 32 |
|
Hope
labela | | | 8 | 7.2 | 0 | 10 |
|
AI-predicted
hope level | | | 7.3 | 7.1 | 0 | 10 |
AI model
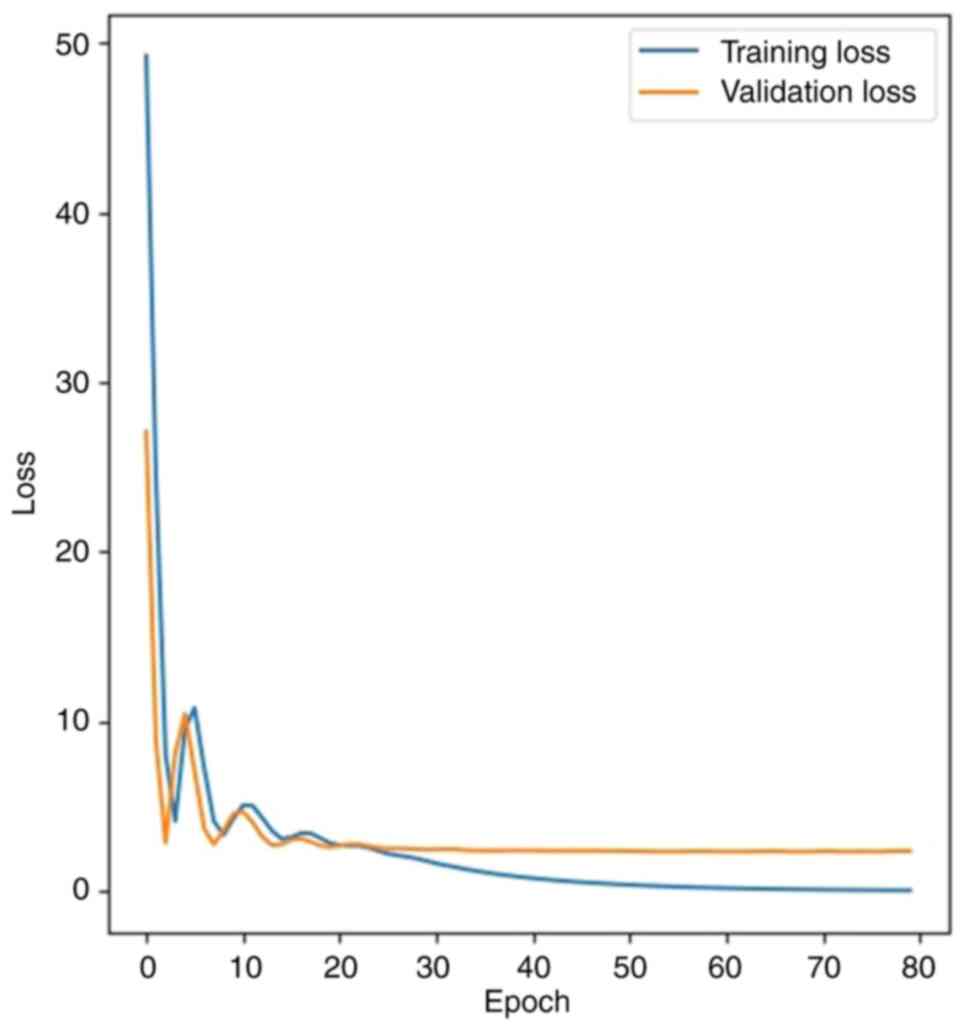
The deep neural network effectively learned from
patient text data, with the loss function [mean squared error
(MSE)] decreasing from 52.29 to 0.08 in the training set, and from
36.09 to 2.34 in the validation set. The MAE figure dropped from
7.00 to 1.12 in the training set and from 5.80 to 1.18 in the
validation set. The loss if function (MSE) changes in the training
and validation sets are presented in Fig. 2.
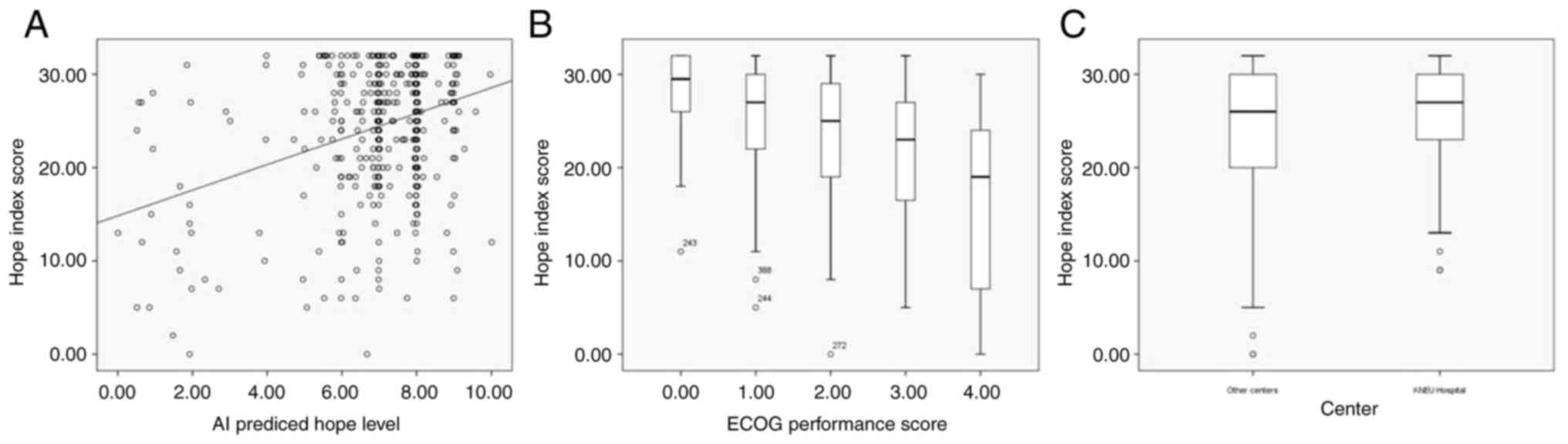
Determinants of hope
Univariate gamma regression analysis revealed
several factors associated with s-ATHS scores, including the
treatment center, age, cancer type, cancer stage, ECOG performance
status, education, income and AI-predicted hope level with varying
P-values (<0.10). In a multivariate gamma regression model,
three factors remained independently significant: The treatment
center (c3 vs. others, Wald=4.77, P=0.029), ECOG performance status
(Wald=47.41, P<0.001) and AI-predicted hope level (Wald=44.24,
P<0.001). The associations of these three factors with s-ATHS
are presented in Table II and
Fig. 3. Of note, although stage was
statistically significant in the univariate gamma regression model
(Wald=5.22, P=0.022), it lost significance in the multivariate
testing stage (Wald=0.05, P=0.818). The median s-ATHS scores in
stage 4 cases was 25, and in earlier stages (stage 1 to 3) it was
27.
 | Table IISelected features of patient from the
different centers. |
Table II
Selected features of patient from the
different centers.
| Patient
features | KNEU center
(c3) | Other centers |
|---|
| Age (median) | 55.31 | 58.61 |
| Female sex (%) | 66% | 55% |
| Diagnosis of breast
or colorectal cancer (%) | 49% | 25% |
| Utilization of
active treatment (%) | 96% | 72% |
| Graduated from
university (%) | 13% | 29% |
| Hope index scores
(mean) | 25.88 | 24.04 |
As regards to the treatment center variable, c3 was
the only center from a university hospital and was located in a
different city compared to the other three centers. The other three
centers were from private and research and training hospitals,
located in another city. The center c3 (KNEU) was different in a
number of ways compared to other centers with a younger patient
age, a greater number of female patients, a greater number of
patients diagnosed with breast and colorectal centers, a greater
utilization of active treatment, and a lower level of university
education. The selected patient features with respect to the
different centers are presented in Table II. Patients from c3 had higher
s-ATHS values. Additionally, an increasing ECOG score was
associated with lower s-ATHS values; median s-ATHS figures were
29.5 in ECOG 0, 27 in ECOG 1, 25 in ECOG 2, 23 in ECOG 3 and 19 in
ECOG 4 classes. Lastly, the AI-predicted hope level was positively
associated with s-ATHS. Further details of the univariate and
multivariate analyses are presented in Table III.
 | Table IIIPredictors of hope in patients with
cancer. |
Table III
Predictors of hope in patients with
cancer.
| | Univariate
analysis | Multivariate
analysis |
|---|
| Parameter | | B | Wald | df | P-value | B | Wald | df | P-value |
|---|
| Centera | | | | | | | | | |
| | c1 [ATRH (center 1)
vs. others] | 0.08 | 6.04 | 1 | 0.014 | 0.04 | 1.12 | 1 | 0.29 |
| | c2 [AMPH (center 2)
vs. others] | -0.08 | 2.69 | 1 | 0.101 | | | | |
| | c3 [KNEU (center 3)
vs. others] | -0.07 | 3.87 | 1 | 0.049 | -0.09 | 4.77 | 1 | 0.029 |
| Age, years | | -0.003 | 5.22 | 1 | 0.022 | -0.002 | 1.99 | 1 | 0.158 |
| Sex | | 0.02 | 0.25 | 1 | 0.618 | | | | |
| Type of
cancerb | | | | | | | | | |
| | ct0 (breast cancer
vs. others) | -0.02 | 0.14 | 1 | 0.708 | | | | |
| | ct1 (lung cancer
vs. others) | 0.02 | 0.15 | 1 | 0.697 | | | | |
| | ct2 (colorectal
cancer vs. others) | -0.12 | 5.27 | 1 | 0.022 | -0.04 | 0.68 | 1 | 0.41 |
| Cancer stage | | 0.07 | 5.22 | 1 | 0.022 | -0.01 | 0.05 | 1 | 0.818 |
| Active
treatment | | -0.05 | 2.09 | 1 | 0.148 | | | | |
| Expression of
feelings | | -0.008 | 0.18 | 1 | 0.675 | | | | |
| Time since
diagnosis | | 0.01 | 0.51 | 1 | 0.475 | | | | |
| ECOG performance
status | | -0.1 | 56.32 | 1 | <0.001 | -0.09 | 47.41 | 1 |
<0.001 |
| Education | | 0.04 | 4.43 | 1 | 0.035 | 0.01 | 0.39 | 1 | 0.533 |
| Income | | 0.08 | 5.75 | 1 | 0.016 | 0.01 | 0.23 | 1 | 0.631 |
| Marital status | | -0.003 | 0.01 | 1 | 0.934 | | | | |
| AI-predicted hope
level | | 0.06 | 44.76 | 1 | <0.001 | 0.06 | 44.24 | 1 |
<0.001 |
Discussion
The present study introduces a novel AI method for
assessing hope in patients with cancer using patient-generated
narratives. This approach may provide a practical means of
evaluating hope and potentially other dimensions of well-being with
implications for research and clinical practice. The present study
incorporated a diverse patient population from various high-volume
cancer treatment centers, encompassing different cancer diagnoses
and disease stages. The heterogeneity of patient enrollment in the
present study suggests that the findings may be generalized to
various cancer patient populations and different treatment and
disease settings. Notably, three common cancer types, breast, lung
and colorectal cancers, comprised 37.6% of the included cases,
reflecting the regional distribution of cancer incidence.
Additionally, the substantial proportion of metastatic patients, at
42.1% of the study population, underscores the applicability of the
resulting AI model to different groups of cancer patients with
respect to type of diagnosis and extent of disease.
Various hope indexes and their versions have been
long-standing tools for measuring hope levels, particularly in the
context of chronic diseases and cancer (9,10,17,18).
In the present study cohort, the median hope index score of 26 on a
32-point scale highlight an above average hope level in the study
respondents. To train the AI model, manually labeled hope labels
were utilized rather than s-ATHS scores, as training the model on
the same entity it is intended to predict would introduce bias.
This approach proved successful, as AI-predicted hope labels
trained on patient-generated text data closely mirrored and
predicted s-ATHS.
In addition to hope and performance status, other
psychosocial variables, such as depression, anxiety and social
support may also play critical roles in shaping patient well-being
and treatment outcomes. Future studies of AI models in the field of
psycho-oncology could incorporate textual markers of these
psychosocial factors, enriching the understanding of the
multidimensional patient experience. Previous research has
demonstrated that emotional distress and lack of social support can
negatively affect both hope and survival in patients with cancer
(19,20). By including these variables, AI
models can potentially serve as a more comprehensive predictor of
patient well-being and even long-term survival.
Several associations identified in the present study
warrant further investigation. For instance, it would be noteworthy
to examine whether why one center (c3) exhibited higher hope scores
(s-ATHS) compared to the others. While the exact reasons for this
remain unclear, factors specific to the center, such as being a
university hospital, or local characteristics, such as city-level
influences, or unnamed factors, may play a role. Although some
differences related to this center were detected compared to the
other centers in terms of a younger patient age, a greater
predominance of the female sex, more frequent diagnoses of breast
and colorectal cancer, a heavier utilization of active treatment
and a lower level of education, the authors consider that none of
these factors alone are sufficient to explain higher hope scores at
this center, as these factors have separately been evaluated in the
regression analyses. Additionally, it was found that, while
advanced-stage disease was negatively associated with hope in the
univariate regression analysis, this association did not remain
significant in the multivariate model. This finding is in
accordance with the findings in the study by Cohen et al
(21), where it was shown that hope
can be maintained even in the latest stages of advanced-stage
cancer. This highlights the complex interplay of multiple factors
influencing hope among patients with cancer with diverse diagnoses
and disease stages.
Of note, in the present study, the use of AI to
assess hope through patient-generated narratives builds upon recent
advancements in AI-based psychosocial research. Studies, such as
that by de Hond et al (22)
demonstrated the effectiveness of deep learning models in
predicting depression from textual data and electronic records in
oncology settings, highlighting the potential of AI to capture
complex emotional states. By validating AI-predicted hope labels
against the established s-ATHS, the present study corroborates
these advancements and also extends them by specifically focusing
on hope as a critical psychosocial factor. This comparison
underscores the promising role of AI in enhancing psychosocial
assessments in clinical practice.
AI is ushering in a revolution in medicine,
facilitating the development of predictive and prognostic models,
decision support systems, and sense-making from complex and
heterogeneous data sources (23).
While the present study marks the initial use of AI for
comprehending textual data for hope in cancer care, this approach
holds promise for application in other disease settings and for
assessing various dimensions of patient well-being, whether
psychological or physical. Such AI models can serve exploratory,
explanatory, predictive, or prognostic purposes. The authors are
particularly interested in exploring the potential prognostic
utility of this approach and intend to follow-up with other
patients to investigate whether AI-predicted hope levels have
predictive value. Currently, the limited literature suggests that
diminished hope levels may predict poorer prognoses in various
health contexts, such as advanced-stage cancer and coronary heart
disease (5,24,25). In
the case that the AI-predicted hope level demonstrated herein is
able to provide prognostic information, it will be noteworthy to
determine whether it surpasses s-ATHS scores in its association
with prognoses.
The present study has several limitations which
should be mentioned. Although the inclusion of 461 participants
provided a solid foundation for demonstrating the feasibility of
the AI-based approach, larger datasets are required to capture more
nuanced and complex associations among variables. Expanding the
study to include data from thousands of patients could
significantly enhance the explanatory and predictive power of the
model. Additionally, future research is required to examine
specific patient subgroups to obtain deeper insight into the
associations within these categories. For instance, analyzing
non-metastatic and metastatic groups within a single cancer type
could yield valuable information.
Another limitation is the lack of the assessment of
depression, which may act as a confounding factor influencing hope
levels. Depression is known to reduce the expression of hope and
overall psychological well-being, potentially biasing the results,
particularly among patients with more advanced stages of cancer
(26). Consequently, some of the
observed associations between hope and other variables may be
partially attributable to underlying depressive symptoms. Future
studies are thus warranted to incorporate measures of depression to
more accurately isolate the effect of hope and enhance the validity
of psychosocial assessments in cancer care.
In conclusion, the present study used a novel AI
approach to assess hope in patients with cancer by leveraging
patient narratives. This approach provides a practical and
insightful method for assessing hope and other aspects of
well-being, with implications for research and clinical practice.
Looking ahead, AI-driven models could not only evaluate hope, but
could also help guide personalized psychosocial interventions for
patients. For example, personalized treatment plans could be
developed based on AI assessments of narrative-driven emotions,
helping clinicians identify patients who may benefit from
pharmacological intervention, psychological support, counseling, or
spiritual care. Additionally, as AI technology advances, it may
become feasible to integrate real-time data from patient narratives
shared via mobile health apps or social media platforms, allowing
for continuous monitoring of hope and other psychosocial variables
throughout the cancer journey.
In summary, assessing hope using textual data with
the help of AI technology has the potential to help us understand
better cancer patients and how they cope with their disease. Using
this approach, it is considered that the association of hope with
the wellbeing of patients with cancer and prognostic outcomes can
be evaluated.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
HŞB designed the study, wrote the code, collected
data and wrote the draft of the manuscript. HGG, MÖA, MY, MK, BK,
MA, GK and HŞC collected data and contributed to the writing of the
draft of the manuscript, as well as in final editing. All authors
have read and approved the final manuscript. HŞB and MK confirm the
authenticity of all the raw data.
Ethics approval and consent to
participate
Ethical committee approval from a teaching hospital
was obtained in July, 2023 (Acceptance no. 2023-162, Antalya
Training and Research Hospital, Antalya, Turkey); the approval was
valid for all centers taking place in the study and the patients
verbally consented to the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Use of artificial intelligence tools
During the preparation of this work, AI tools were
used to improve the readability and language of the manuscript or
to generate images, and subsequently, the authors revised and
edited the content produced by the AI tools as necessary, taking
full responsibility for the ultimate content of the present
manuscript.
References
|
1
|
Mardhiyah A, Philip K, Mediani HS and
Yosep I: The association between hope and quality of life among
adolescents with chronic diseases: A systematic review. Child
Health Nurs Res. 26:323–328. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Rustøen T: Hope and quality of life, two
central issues for cancer patients: A theoretical analysis. Cancer
Nurs. 18:355–361. 1995.PubMed/NCBI
|
|
3
|
Soleimani MA, Mohammad A, Zarabadi-Pour S,
Huak Chan Y, Allen KA and Shamsizadeh M: Factors associated with
hope and quality of life in patients with coronary artery disease.
J Nurs Res. 30(e200)2022.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cheavens J: Hope and Depression: Light
Through the Shadows. In: Handbook of Hope. Snyder CR (ed). Academic
Press, Cambridge, MA, pp321-340, 2000.
|
|
5
|
Corn BW, Feldman DB, Hull JG, O'Rourke MA
and Bakitas MA: Dispositional hope as a potential outcome parameter
among patients with advanced malignancy: An analysis of the ENABLE
database. Cancer. 128:401–409. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bunston T, Mings D, Mackie A and Jones D:
Facilitating Hopefulness. J Psychosoc Oncol. 13:79–103. 1995.
|
|
7
|
van Baalen CN, Grypdonck M, van Hecke A
and Verhaeghe S: Associated factors of hope in cancer patients
during treatment: A systematic literature review. J Adv Nurs.
76:1520–1537. 2020.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982.PubMed/NCBI
|
|
9
|
Snyder CR, Harris C, Anderson JR, Holleran
SA, Irving LM, Sigmon ST, Yoshinobu L, Gibb J, Langelle C and
Harney P: The will and the ways: Development and validation of an
individual-differences measure of hope. J Pers Soc Psychol.
60:570–585. 1991.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Beam AL, Drazen JM, Kohane IS, Leong TY,
Manrai AK and Rubin EJ: Artificial intelligence in medicine. N Engl
J Med. 388:1220–1221. 2023.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Obayuwana AO, Collins JL, Carter AL, Rao
MS, Mathura CC and Wilson SB: Hope index scale: An instrument for
the objective assessment of hope. J Natl Med Assoc. 74:761–765.
1982.PubMed/NCBI
|
|
12
|
Herth P: Measuring hope: Development of
the Herth Hope Index. J Nurs Scholarsh. 32:309–315. 2000.
|
|
13
|
Anastaisya Z: Text classification in
artificial intelligence. InData Labs, 2023. https://indatalabs.com/blog/text-classification-in-artificial-intelligence.
Accessed September 21, 2024.
|
|
14
|
Sandoval AM: Text Analytics: The
convergence of big data and artificial intelligence. Int J Interact
Multimed Artif Intell. 3:57–64. 2016.
|
|
15
|
Pleeging E: Measuring hope: Validity of
short versions of four popular hope scales. Qual Quant.
56:4437–4464. 2022.
|
|
16
|
Acharya S: What are RMSE and MAE? A Simple
Guide to evaluation metrics. Towards Data Science, 2021. https://towardsdatascience.com/what-are-rmse-and-mae-e405ce230383.
Accessed September 21, 2024.
|
|
17
|
Wahl AK, Rustoen T, Lerdal A, Hanestad BR,
Knudsen O Jr and Moum T: The Norwegian version of the Herth Hope
Index (HHI-N): A psychometric study. Palliat Support Care.
2:255–263. 2004.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Geiser F, Zajackowski K, Conrad R,
Imbierowicz K, Wegener I, Herth KA and Urbach AS: The German
version of the Herth Hope Index (HHI-D): Development and
psychometric properties. Oncol Res Treat. 38:356–360.
2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Mystakidou K, Parpa E, Tsilika E,
Athanasouli P, Pathiaki M, Galanos A, Pagoropoulou A and Vlahos L:
Preparatory grief, psychological distress and hopelessness in
advanced cancer patients. Eur J Cancer Care (Engl). 17:145–151.
2008.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Pinquart M and Duberstein PR: Associations
of social networks with cancer mortality: A meta-analysis. Crit Rev
Oncol Hematol. 75:122–137. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Cohen MG, Althouse AD, Arnold RM, Bulls
HW, White DB, Chu E, Rosenzweig MQ, Smith KJ and Schenker Y: Hope
and advance care planning in advanced cancer: Is there a
relationship? Cancer. 128:1339–1345. 2022.PubMed/NCBI View Article : Google Scholar
|
|
22
|
de Hond A, van Buchem M, Fanconi C, Roy M,
Blayney D, Kant I, Steyerberg E and Hernandez-Boussard T:
Predicting depression risk in patients with cancer using multimodal
data: Algorithm development study. JMIR Med Inform.
12(e51925)2024.PubMed/NCBI View
Article : Google Scholar
|
|
23
|
Haug CJ and Drazen JM: Artificial
intelligence and machine learning in clinical medicine, 2023. N
Engl J Med. 388:1201–1208. 2023.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Feldman DB and Corn BW: Hope and cancer.
Curr Opin Psychol. 49(101506)2023.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Everson SA, Goldberg DE, Kaplan GA, Cohen
RD, Pukkala E, Tuomilehto J and Salonen JT: Hopelessness and risk
of mortality and incidence of myocardial infarction and cancer.
Psychosom Med. 58:113–121. 1996.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Nikoloudi M, Tsilika E, Kostopoulou S and
Mystakidou K: Hope and distress symptoms of oncology patients in a
palliative care setting. Cureus. 15(e38041)2023.PubMed/NCBI View Article : Google Scholar
|