Introduction
Cystinosis is a very rare autosomal recessive
lysosomal storage disorder that leads to the buildup of cystine in
the lysosomes of affected cells (1).
There are three forms of the disease, with the infantile form
typically being the most severe, as it presents both ocular and
systemic symptoms at an early stage (2). This form is associated with severe or
truncating mutations on both alleles, and adult forms usually
involve at least one milder mutation (3). Infantile cystinosis, the most severe
and common form, presents within the first year of life with
Fanconi syndrome, growth retardation and progressive renal failure
(4).
Cystinosis often leads to systemic issues, such as
renal failure and eye conditions, particularly corneal cystine
deposits (1). The underlying cause
is the impaired transport of cystine out of lysosomes due to
mutations in the CTNS gene, which encodes cystinosin, a
transporter for lysosomal cysteine (5). This accumulation results in cellular
dysfunction and tissue damage, leading to the systemic and ocular
symptoms observed in cystinosis. The disorder follows an autosomal
recessive inheritance pattern, affecting ~1 in 100,000 to 200,000
live births (6).
There are three clinical subtypes of cystinosis:
Infantile (nephropathic), juvenile (intermediate) and adult
(non-nephropathic or ocular) (7).
Infantile cystinosis, the most severe and common form, presents
within the first year of life with Fanconi syndrome, growth
retardation and progressive renal failure (1). Without treatment, affected individuals
typically develop end-stage renal disease by adolescence. The
juvenile form manifests later in childhood with milder renal
impairment, while the adult form primarily involves ocular
symptoms, such as photophobia due to corneal cystine crystal
deposition.
Ophthalmic complications in cystinosis are
significant and include corneal cystine deposits, photophobia,
conjunctival damage, retinal degeneration, and, in rare cases,
optic nerve involvement (8).
Papilledema is an unusual finding and may indicate increased
intracranial pressure (ICP), which can be secondary to chronic
kidney disease (CKD), electrolyte disturbances, or other systemic
factors. Early diagnosis through biochemical testing (leukocyte
cystine levels) and genetic screening is crucial for initiating
timely treatment (9).
Despite therapeutic advancements, managing
cystinosis remains challenging due to medication adherence issues,
potential side-effects of cysteamine and the progressive nature of
the disease. Given its multi-systemic impact, a multidisciplinary
approach involving nephrologists, ophthalmologists, neurologists
and geneticists is essential for optimizing patient outcomes. The
present study describes the case of a patient with infantile
cystinosis that exhibited both ocular and systemic symptoms. The
aim of the present study was to underscore the diagnostic and
therapeutic challenges this condition presents and to highlight the
necessity of a multidisciplinary approach to improve the quality of
life and long-term outcomes of patients.
Case report
Patient history
A 4-year-old girl presented to the Department of
Ophthalmology, Swai Man Singh Medical College and Hospitals,
Jaipur, India with a primary concern of visual disturbances in both
eyes. Her parents had observed a gradual increase in her difficulty
with visual tasks, such as recognizing familiar objects and moving
around her environment. She had a medical history notable for
cystinosis, which was diagnosed when she was 18 months old, leading
to distal renal tubular acidosis (dRTA) and stage 4 CKD. The
patient was receiving regular dialysis and was administered
bicarbonate supplements to manage her renal acidosis. There was no
record of eye injuries, previous surgeries, or other notable
illnesses. Despite her ongoing health challenges, her developmental
milestones were appropriate for her age.
Ocular examination
The best-corrected visual acuity (BCVA) in both eyes
was finger count at six feet, indicating severe visual impairment.
Refraction revealed hyperopic prescriptions of +2.50 diopters in
the right eye and +2.50 diopters with +0.50 diopters at 90˚ in the
left eye. An anterior segment examination revealed diffuse
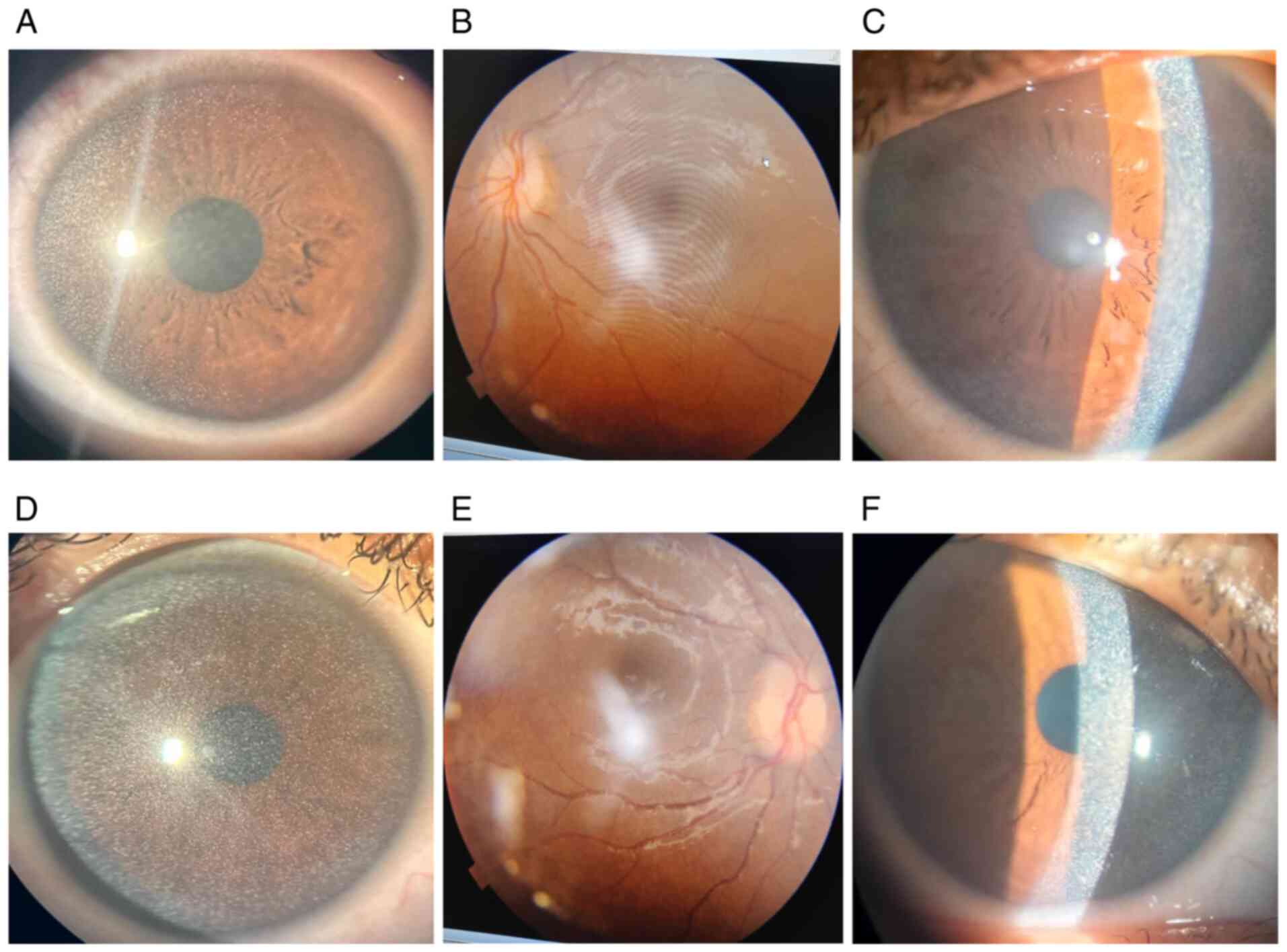
bilateral corneal cystine crystal deposits (Fig. 1A and D), which created a characteristic
shimmering effect under slit-lamp biomicroscopy. A fundoscopic
examination indicated marked papilledema in both eyes, consistent
with elevated intracranial pressure (Fig. 1B and E). Additionally, bilateral retinal cystine
deposits were observed, further supporting systemic involvement
(Fig. 1C and F). Optic nerve head swelling, confirmed by
B-scan ultrasonography, revealed optic disc diameters of 3.8 mm in
the right eye and 4.1 mm in the left eye, with notable optic disc
elevation.
Systemic associations
The systemic condition of the patient was primarily
affected by complications arising from cystinosis. Renal function
tests (urea, 92.57 mg/dl; creatinine, 1.46 mg/dl; serum
thyroid-stimulating-hormone, 10 mIU/l) indicated stage 4 CKD, which
required ongoing dialysis and bicarbonate supplementation to manage
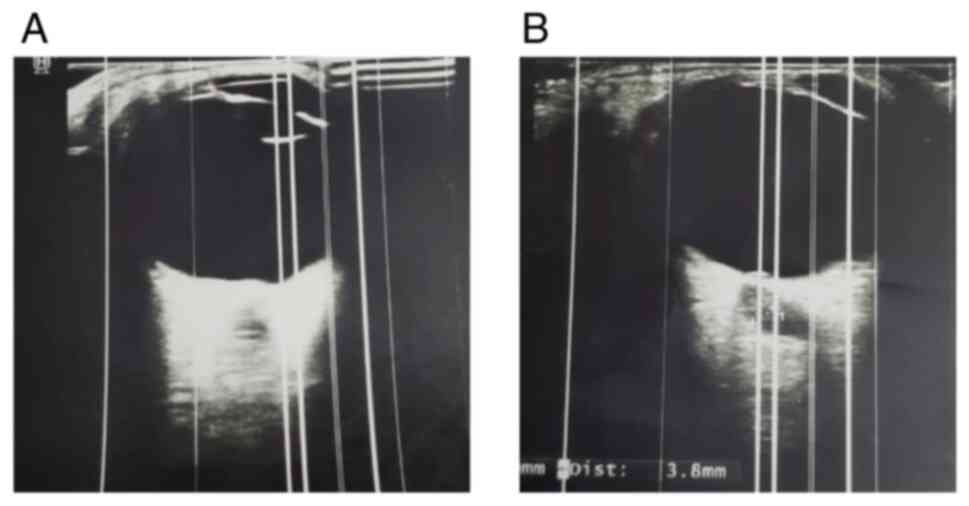
persistent metabolic acidosis. A neurological evaluation indicated
elevated intracranial pressure, likely resulting from a combination
of CKD and electrolyte imbalances (Fig.
2). A neurological examination revealed no motor or sensory
deficits, and a referral was made to a pediatric neurologist for
further evaluation and management of the intracranial
hypertension.
Diagnosis
The patient was diagnosed with corneal cystine
deposits due to systemic cystinosis and papilledema linked to
elevated intracranial pressure, likely stemming from CKD and its
associated complications. The ocular findings were directly tied to
the systemic condition, underscoring the interconnected nature of
her health issues.
Ophthalmological care
The main objective of ophthalmological management
was to protect the remaining vision of the patient and relieve
symptoms. Corrective lenses were prescribed to enhance her visual
acuity. Topical cysteamine eye drops were commenced as a standard
treatment to decrease the accumulation of corneal cystine crystals,
which would help improve corneal clarity and prevent further visual
decline. Artificial tears were suggested to alleviate dryness on
the ocular surface and improve patient comfort. Regular follow-up
appointments were arranged to track the progression of corneal
deposits and papilledema, with slit-lamp and fundoscopic
examinations conducted at each visit.
Systemic treatment
The management of the systemic condition of the
patient focused on controlling the complications associated with
cystinosis and CKD. Dialysis was continued, and bicarbonate
supplementation was provided to manage metabolic acidosis. The
patient was referred to a pediatric neurologist to investigate the
cause of elevated intracranial pressure and to commence appropriate
treatment. This included monitoring for any signs of worsening
papilledema and neurological symptoms that may necessitate
cerebrospinal fluid pressure management or other interventions.
Nutritional support and growth monitoring were also prioritized to
ensure the overall development and health of the patient.
Follow-up protocol
A thorough follow-up protocol was established, which
included corneal evaluations every 3 to 6 months and fundoscopic
examinations every 1 to 2 months. This approach aimed to ensure the
early detection of any deterioration in corneal clarity or optic
nerve health. Effective coordination among the ophthalmology,
nephrology and neurology teams was essential for providing
comprehensive care.
Discussion
The case presented herein illustrates the complex
effects of cystinosis on pediatric patients, particularly as
regards its ocular and systemic manifestations. Corneal cystine
deposits, a defining feature of the disease, arise from the
accumulation of cystine in lysosomes and can severely affect vision
(1). These deposits can worsen over
time and may lead to corneal scarring, if left untreated. Topical
cysteamine has proven effective in reducing corneal crystals;
however, maintaining adherence to treatment can be difficult,
particularly for young children (10-12).
Papilledema, as observed in the patient in the
present study, is a rare, yet serious complication of cystinosis.
It can occur due to elevated intracranial pressure resulting from
chronic kidney disease, electrolyte imbalances, or other systemic
issues. If left untreated, papilledema can result in optic atrophy
and permanent vision loss (13).
Although a lumbar puncture was not performed, the patient's
clinical presentation and systemic findings were consistent with
secondary ICP elevation. The link between CKD and papilledema in
patients with cystinosis has been well-documented; however, it
remains multifactorial (3,14). In the patient in the present study,
electrolyte imbalances (hypokalemia and metabolic acidosis), fluid
retention and possible hypertension could have contributed to the
increased ICP. At the same time, the multidisciplinary approach
taken in the present case was instrumental in managing the
condition of the patient (8,15,16).
Additional neuroimaging and cerebrospinal fluid analysis could have
helped confirm the diagnosis and rule out other contributing
factors. The pathophysiology of ICP regulation in cystinosis
remains poorly understood, warranting further investigations.
Improved neuro-ophthalmologic screening guidelines may facilitate
earlier detection and intervention in such cases.
Cysteamine therapy is effective in delaying disease
progression; however, it requires strict adherence. Frequent dosing
(4-6 times daily) remains challenging, particularly in pediatric
patients (17). Research has
indicated that while cysteamine therapy significantly reduces
corneal crystal density and improves photophobia, complete
clearance is often not achieved (18). Moreover, adverse effects such as
ocular irritation, burning sensation, and the potential for
conjunctival hyperemia can further affect compliance. Beyond eye
health, systemic cysteamine therapy can lead to several
side-effects that should be considered when planning long-term
treatment (19). Common issues
include gastrointestinal symptoms, such as nausea, vomiting and
abdominal pain, as well as halitosis, which is a result of
dimethylsulfide production. Given these challenges, future research
is required to explore new drug delivery systems, such as
sustained-release formulations, that could reduce dosing frequency
and minimize some side-effects. This could help improve both the
effectiveness of the treatment and patient compliance. By better
addressing these concerns, researchers can work toward developing
more balanced, long-term strategies for managing cystinosis in
children, ensuring that the benefits of treatment outweigh the
challenges posed by side-effects (4).
The importance of genetic counseling and early
diagnosis in managing cystinosis cannot be emphasized enough.
Detecting the condition early enables the start of systemic
cysteamine therapy, which can help attenuate the progression of
renal and other systemic complications. Additionally, regular eye
examinations from infancy are vital for identifying and treating
ocular issues before they affect vision. Genetic testing was not
performed in the case in the present study, which represents a
limitation of the present study. Molecular testing of CTNS
mutations is crucial for definitive diagnosis, prognosis estimation
and family counseling. Future studies are thus required to
integrate genetic testing into standard diagnostic workflows to
enhance early detection and intervention. Newborn screening
programs using tandem mass spectrometry to detect elevated cystine
levels in leukocytes have been proposed in high-risk populations,
but are not yet widely implemented (20). Expanding awareness and accessibility
to genetic diagnostics may improve patient outcomes.
The long-term management of cystinosis requires
coordinated follow-up across multiple specialties. Regular
ophthalmologic evaluations, including corneal clarity assessments,
optic nerve examinations and visual acuity monitoring, should be
scheduled every 3-6 months. Monitoring for systemic complications,
such as gastrointestinal side-effects, halitosis, bone
abnormalities, particularly CKD progression and metabolic
imbalances, is essential for timely interventions (21). Patients should also undergo periodic
neuro-ophthalmologic evaluations to track ICP and visual function
changes. Given the burden of lifelong therapy, quality-of-life
assessments are crucial. Pediatric patients face challenges with
medication adherence, social integration and developmental
milestones (22). Psychological
support and patient education programs should be integrated into
care plans to improve adherence and mental well-being. Advances in
cysteamine formulations, gene therapy and novel neuroprotective
strategies hold promise for improving long-term outcomes in
patients with cystinosis (23).
The present study has several limitations which
should be mentioned. The reliance on a single case restricts the
generalizability of the findings, emphasizing the need for larger
patient cohorts to better characterize the association between
cystinosis and papilledema. Additionally, the absence of genetic
testing represents a limitation, as molecular confirmation of
CTNS mutations would have strengthened diagnostic accuracy.
Furthermore, cerebrospinal fluid analysis and neuroimaging were not
performed, limiting the ability to fully investigate the underlying
cause of papilledema. Future research should focus on expanding
genetic screening databases, identifying biomarkers for early
disease detection, and exploring new therapeutic strategies to
improve long-term outcomes.
In conclusion, the present study described the case
of a 4-year-old girl with cystinosis, dRTA and CKD4, highlighting
the significant systemic and ocular effects of the disease. Key
findings included corneal cystine deposits and papilledema, which
were addressed through a collaborative approach. The combination of
eye care, systemic treatment and neurological assessment was
crucial in managing the symptoms of the patient and preventing
further complications. Early diagnosis, prompt intervention and
consistent follow-ups are critical for achieving the optimal
outcomes for pediatric patients with cystinosis. The present case
report highlights the importance of teamwork in managing rare and
complex conditions.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
DSC designed the study. JS and RK recruited the
participant. DSC, JS and RK conducted the clinical examinations and
collected the patient samples and data. AD obtained OCT, slit lamp
and other images. BSK and DSC analyzed the patient's data and
drafted the manuscript. BSK and DSC also critically reviewed the
manuscript and supervised the entire study process. BSK and DSC
confirm the authenticity of all the raw data. All authors provided
conceptual advice and technical support, and have read and approved
the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from the
patient's legal guardians for participation in the present study.
and publication of relevant clinical information and images.
Patient consent for publication
Written informed consent was obtained from the
patient's legal guardians for participation in the present study
and for the publication of any relevant clinical information and
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Elmonem MA, Veys KR, Soliman NA, van Dyck
M, van den Heuvel LP and Levtchenko E: Cystinosis: A review.
Orphanet J Rare Dis. 11(47)2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Nesterova G and Gahl WA: Cystinosis: The
evolution of a treatable disease. Pediatr Nephrol. 28:51–59.
2013.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Curie A, Touil N, Gaillard S, Galanaud D,
Leboucq N, Deschenes G, Morin D, Abad F, Luauté J, Bodenan E, et
al: Neuropsychological and neuroanatomical phenotype in 17 patients
with cystinosis. Orphanet J Rare Dis. 15(59)2020.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Martin-Sabroso C, Alonso-Gonzalez M,
Fernandez-Carballido A, Aparicio-Blanco J, Cordoba-Diaz D,
Navarro-Garcia F, Córdoba-Díaz M and Torres-Suárez AI: Limitations
and challenges in the stability of cysteamine eye drop compounded
formulations. Pharmaceuticals (Basel). 15(2)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Town M, Jean G, Cherqui S, Attard M,
Forestier L, Whitmore SA, Callen DF, Gribouval O, Broyer M, Bates
GP, et al: A novel gene encoding an integral membrane protein is
mutated in nephropathic cystinosis. Nat Genet. 18:319–324.
1998.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Gahl WA, Thoene JG and Schneider JA:
Cystinosis. N Engl J Med. 347:111–121. 2002.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Baumner S and Weber LT: Nephropathic
cystinosis: Symptoms, treatment, and perspectives of a systemic
disease. Front Pediatr. 6(58)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Biswas S, Gaviria M, Malheiro L, Marques
JP, Giordano V and Liang H: Latest clinical approaches in the
ocular management of cystinosis: A review of current practice and
opinion from the ophthalmology cystinosis forum. Ophthalmol Ther.
7:307–322. 2018.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Emma F, Montini G, Pennesi M, Peruzzi L,
Verrina E, Goffredo BM, Canalini F, Cassiman D, Rossi S and
Levtchenko E: Biomarkers in nephropathic cystinosis: Current and
future perspectives. Cells. 11(1839)2022.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Gahl WA, Balog JZ and Kleta R:
Nephropathic cystinosis in adults: Natural history and effects of
oral cysteamine therapy. Ann Intern Med. 147:242–250.
2007.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Bradbury JA, Danjoux JP, Voller J, Spencer
M and Brocklebank T: A randomised placebo-controlled trial of
topical cysteamine therapy in patients with nephropathic
cystinosis. Eye (Lond). 5:755–760. 1991.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Makuloluwa AK and Shams F: Cysteamine
hydrochloride eye drop solution for the treatment of corneal
cystine crystal deposits in patients with cystinosis: An
evidence-based review. Clin Ophthalmol. 12:227–236. 2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Attia R, Fitoussi R, Mairot K, Demortiere
S, Stellman JP, Tilsley P, Audoin B, David T and Stolowy N: Risk
factors associated with progression from papilloedema to optic
atrophy: Results from a cohort of 113 patients. BMJ Open
Ophthalmol. 8(e001375)2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Emma F, Nesterova G, Langman C, Labbe A,
Cherqui S, Goodyer P, Janssen MC, Greco M, Topaloglu R, Elenberg E,
et al: Nephropathic cystinosis: an international consensus
document. Nephrol Dial Transplant 29 Suppl. 4 (Suppl 4):iv87–iv94.
2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ariceta G, Camacho JA, Fernandez-Obispo M,
Fernandez-Polo A, Gamez J, Garcia-Villoria J, Monteczuma EL, Leyes
P, Martín-Begué N, Oppenheimer F, et al: Cystinosis in adult and
adolescent patients: Recommendations for the comprehensive care of
cystinosis. Nefrologia. 35:304–321. 2015.PubMed/NCBI View Article : Google Scholar : (In English,
Spanish).
|
|
16
|
Choudhary DS, Verma G, Kumar K, Choudhary
P, Kalal BS and Chaudhary A: Bowman's membrane lenticule tuck-in: A
new approach for the management of neurotrophic ulcers. Saudi J
Ophthalmol. 37:120–124. 2023.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Bouazza N, Treluyer JM, Ottolenghi C,
Urien S, Deschenes G, Ricquier D, Niaudet P and Chadefaux-Vekemans
B: Population pharmacokinetics and pharmacodynamics of cysteamine
in nephropathic cystinosis patients. Orphanet J Rare Dis.
6(86)2011.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Iwata F, Kuehl EM, Reed GF, McCain LM,
Gahl WA and Kaiser-Kupfer MI: A randomized clinical trial of
topical cysteamine disulfide (cystamine) versus free thiol
(cysteamine) in the treatment of corneal cystine crystals in
cystinosis. Mol Genet Metab. 64:237–242. 1998.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Ariceta G, Giordano V and Santos F:
Effects of long-term cysteamine treatment in patients with
cystinosis. Pediatr Nephrol. 34:571–578. 2019.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Hohenfellner K, Bergmann C, Fleige T,
Janzen N, Burggraf S, Olgemoller B, Gahl WA, Czibere L, Froschauer
S, Röschinger W, et al: Molecular based newborn screening in
Germany: Follow-up for cystinosis. Mol Genet Metab Rep.
21(100514)2019.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chen TK, Knicely DH and Grams ME: Chronic
kidney disease diagnosis and management: A review. JAMA.
322:1294–1304. 2019.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Hegde SK, Ranjit O, Bhat SS and Kalal BS:
Analysis of dental caries experience and parents perception on the
oral health status of children with autism spectrum disorders from
South India. Med J Bakirkoy. 20:189–195. 2024.
|
|
23
|
Elenberg E: Optimizing long-term outcomes
in cystinosis with comprehensive patient-centered Care. Kidney Int
Rep. 10:S775–S778. 2025.PubMed/NCBI View Article : Google Scholar
|