Introduction
Primary brain tumors comprise a heterogeneous group
of neoplasms, with different outcomes, with patients requiring
different management strategies. These tumors can range from
pilocytic astrocytomas, a very uncommon, non-invasive curable
tumor, to glioblastoma (GBM), which is associated with more
invasive and aggressive behaviors (1).
GBM is the most common primary brain tumor among
adults. It is associated with a median survival rate of 16-21
months and a 10-year survival of <1% (1-5).
GBM accounts for 45.6% of all primary brain malignancies. The
incidence rate of GBM is 3.19 among 100,000 individuals from
different age groups with a median age of 64 years; however, it can
occur at any age (6).
In general, GBM is associated with a very poor
prognosis. However, several parameters associated with improved
outcomes include an age <50 years, a non-eloquent tumor
location, a Karnofsky performance status (KPS) score ≥70 and the
maximal extent of tumor resection (7,8).
The treatment of patients with GBM includes maximal
surgical resection with adjuvant radiotherapy. The inclusion of
nitrosoureas has exhibited benefits in addition to the standard
treatment; however, this has only been demonstrated in multivariant
and randomized comparison studies (7,9). The use
of adjuvant temozolomide was previously investigated in a
randomized phase III, EORTCNCIC trials along with standard surgical
resection and radiotherapy; its use was found to be associated with
an improved overall survival rate of 14.6 compared to 12.1 months
with standard treatment with radiotherapy (10,11).
Temozolomide was approved in 2005, and since then, it has been the
standard chemotherapeutic treatment for GBM for six 6 cycles
following radiotherapy (12).
GBMs have a high recurrence rate even in cases in
which they have been discovered at an early stage and treated
completely. The median recurrence time is 9.5 months, with an
overall survival rate of 30 months (13). The treatment of recurrent or
progressive GBMs can include supportive care, as decided by the
treating physician. On the other hand, tumor-specific
multidisciplinary boards are another approach for treating patients
with GBM; the use of these has been shown to be associated with a
12-month survival rate of 32.5% compared to 11.3% in the group with
supportive treatment (14).
A previous meta-analysis investigated palliative
care intervention in adults with terminal illnesses and diseases,
including oncology. The quality of life (QOL) of patients was
assessed in 24 studies, including 4,576 patients; 12 (50%) studies
evaluated the association between QOL and palliative care
intervention and reported a statistically significant improvement
in QOL and symptoms burden (15).
When assessing the end-of-life in a patient with
GBM, a decreased level of consciousness, a change in mental status,
fever, seizures and dysphagia have been shown to have the most
marked clinical burden as the disease progresses. Moreover, this
provides the basis for care in these terminal care cases to include
anticonvulsants, steroids and gastric protection, such as
non-steroidal anti-inflammatory drugs (16,17).
Other modalities of palliative care are short-course
radiotherapy, which has been shown to be beneficial in patients
with a KPS score <50, along with the optimal supportive and
palliative care, including the use of corticosteroids (18). The use of mifepristone, a
progesterone receptor antagonist, has also been suggested for
palliative care therapy in patients with advanced-stage brain
tumors, including GBM, as it exhibits good penetration through the
blood-brain barrier (19).
The American Society of Clinical Oncology (ASCO)
Clinical Practice Guidelines recommend the addition of palliative
care in patients with advanced-stage cancer (20). Specifically, patients with GBM suffer
from progressive neurological diseases that affect their QOL along
with their decision-making capacity; of note, ~50% of patients with
primary malignant brain tumors have compromised medical
decision-making at the time of diagnosis due to cognitive
impairment, behavioral changes and poor communication abilities
(21). Therefore, advanced care
planning (ACP) has evolved to facilitate the communication of goals
and preferences regarding future medical care, and it is considered
crucial in patients with GBM. It not only includes the treatment
design and a proxy decision maker, but also extends to involve open
communications between the patient, proxy, decision-makers and care
providers to discuss the preferences for future medical care,
including palliative care options (22).
ACP can be utilized to improve the quality of
communications between patients and healthcare providers and may
reduce unwanted interventions and admissions. In addition, it
enhances the use of palliative care, which increases the
satisfaction and QOL of both patients and relatives (22,23).
Therefore, the present study aimed to systematically
review and analyze the available literature on patients with GBM
receiving palliative care.
Data and methods
Literature search strategy
The present study aimed to systematically review and
analyze the available literature on patients with GBM receiving
palliative care. The PubMed, Scopus, Wiley and Web of Science
databases were searched by three authors (AMAG, SAB and AMAA) to
gather the available literature using the following key words:
‘Glioblastoma’, ‘GBM’, ‘Grade 4 glioma’, ‘Palliative care’,
‘Conservative’, ‘Non-surgical’, ‘Comfort care’, ‘Management’,
‘Palliative Radiotherapy’, ‘Palliative Chemotherapy’ and ‘End of
life’.
Study selection, inclusion and
exclusion criteria
Studies were selected using a systematic review
following the Preferred Reporting Items for Systematic Reviews and
Meta-Analysis (PRISMA) guidelines. All articles relevant to the
topic of the review were included, covering patients of all age
groups, and all types of palliative care used, in all settings and
there was no time limit; however, articles that were not published
in the English language were excluded from the systematic
review.
Data extraction and analysis
After applying the inclusion and exclusion criteria,
AMAG, SAB and AMAA screened the titles and abstracts of possible
eligible studies. Moreover, the three authors examined the key
features from the eligible studies, extracting the aims, treatments
and palliative care applied, as well as the outcomes, place of
mortality (either at a health institute or at home), and the
recommendation from the authors of that study. In addition, the
three authors examined the year of publication, and the country
where the study was conducted.
Results
Study selection, including and
exclusion criteria
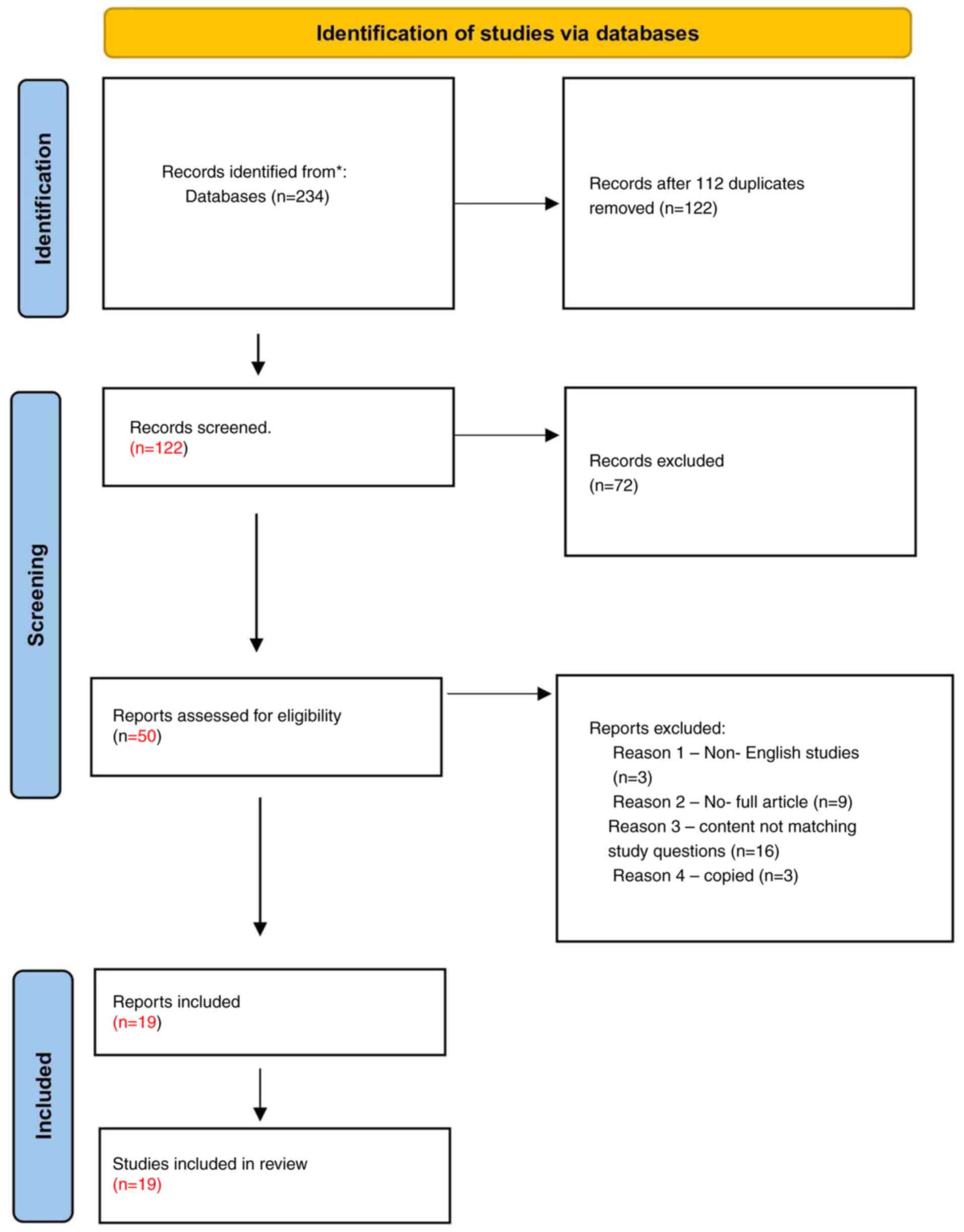
In the present systematic review, the three authors
were allocated to investigate four databases, obtaining a total of
234 studies that matched the objectives of the review. Moreover,
112 studies were excluded as they were duplicates. After reviewing
these articles, 72 studies were removed as they did not match the
aim of the review. After applying the inclusion and exclusion
criteria, a total of 50 articles were included; however, of these,
three articles were excluded as they were non-English studies, the
full article could not be accessed in nine articles and 16 articles
were not relevant to the study question. In addition, three studies
were identified as copies or duplicates, having been retrieved from
the searches conducted independently by the three different authors
and were removed. Eventually, a total of 19 articles were included
in the present systematic review (Fig.
1).
Quality assessment and geographical
distribution
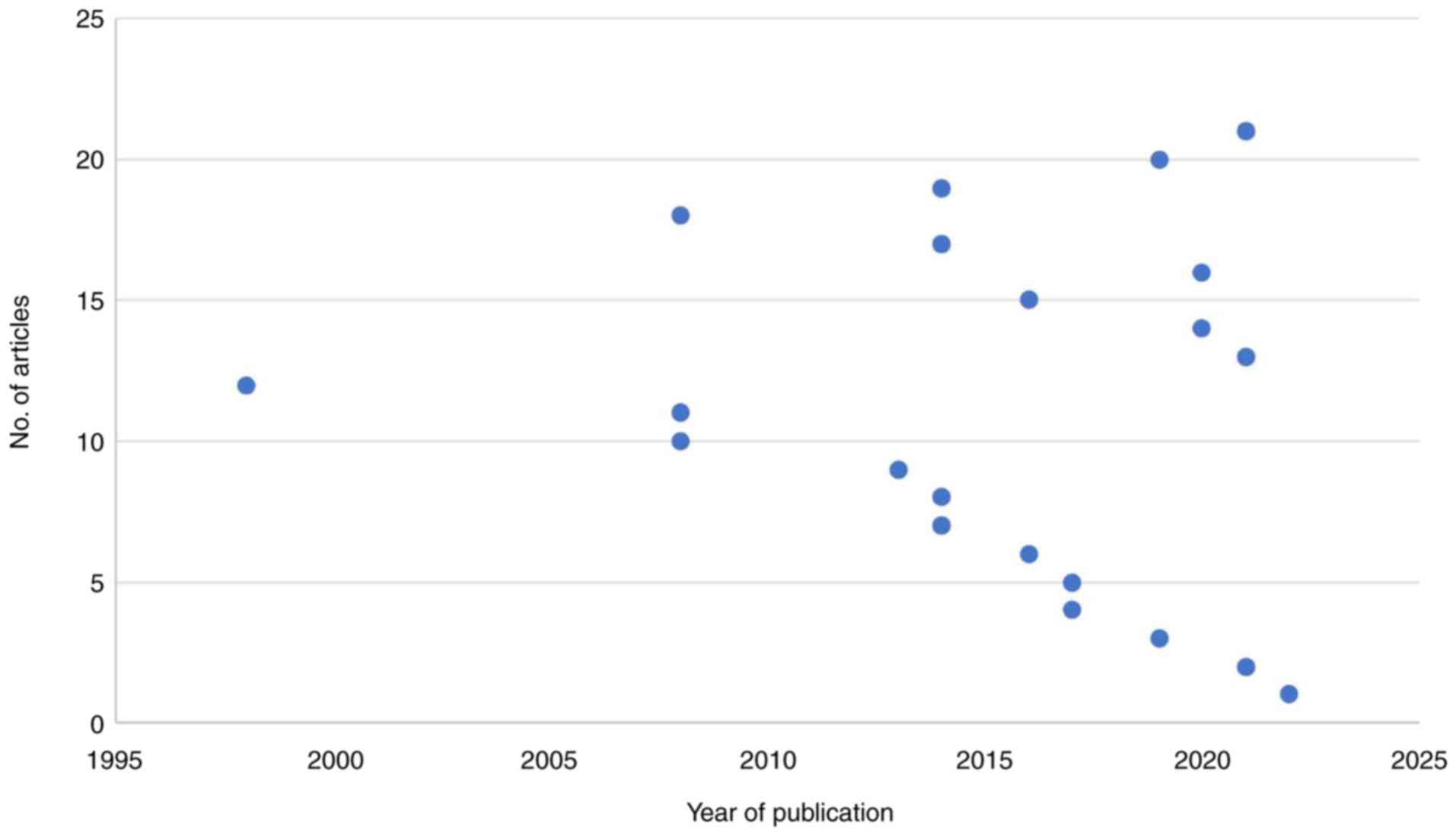
In the present systematic review, 19 articles were
included, with publication years ranging between 1998 and 2022,
with a total of 7,392 patients (Fig.
2). Of note, two of these articles were case reports (19,24). The
majority of the included articles were retrospective analyses (10
articles out of 19 articles) (14,18,25-32).
A total of four articles were prospective studies (16,33-35),
two articles were systematic reviews (17,36) and
one article was a randomized clinical trial (37) (Table
I).
 | Table IQuality assessment of the included
studies. |
Table I
Quality assessment of the included
studies.
| Article no. | Authors, year of
publication | Type of study | Level of
evidence | Sample | (Refs.) |
|---|
| 1 | Senderovich et
al, 2022 | Case report | 4 | n=1,
phenobarbital | (24) |
| 2 | Witteler et
al, 2021 | Retrospective
analysis | 3b | n=31,
radiotherapy | (18) |
| 3 | Wu et al,
2021 | Systematic
review | 1a | NA | (36) |
| 4 | Harrison et
al, 2021 | Retrospective
cohort study | 3b | n=132, NA | (25) |
| 5 | Lin et al,
2020 | Retrospective
analysis | 3b | n=50, medications:
Steroids, anti-epileptic drugs, Benzodiazepines….. Allied health
involvement: Physiotherapy, occupational therapy, social work,
speech pathology, pastoral care | (26) |
| 6 | Kim et al,
2020 | Prospective
study | 2b | n=294, NA | (35) |
| 7 | Golla et al,
2020 | Randomized clinical
trial | 1b | n=214,
Interventional group [proactive early integration of palliative
care (EPIC) on a monthly basis], control group (receiving treatment
according to international standards and additional, regular
assessment of quality of life) | (37) |
| 8 | Glynn et al,
2019 | Retrospective
analysis | 3b | n=104 radiotherapy
(hypofractionated palliative radiotherapy) | (27) |
| 9 | Stavrinou e et
al, 2018 | Retrospective
analysis | 3b | n=259, glioblastoma
was treated with maximal safe resection followed by adjuvant
radiotherapy + post-operative chemotherapy (6 cycles of
temozolomide), then palliative care with supportive treatment | (14) |
| 10 | Hemminger et
al, 2017 | Retrospective
analysis | 3b | n=117,
chemotherapy | (28) |
| 11 | Kuchinad et
al, 2017 | Retrospective
analysis | 3b | n=100,
chemotherapy | (29) |
| 12 | Thier et al,
2016 | Prospective
study | 2b | n=57, non-steroidal
anti-inflammatory drugs, anticonvulsants and steroids | (16) |
| 13 | Check et al,
2014 | Case report | 4 | n=1,
mifepristone | (19) |
| 14 | Sundararajan et
al, 2014 | Retrospective
cohort study | 3b | n=678, palliative
care consult, palliative care bed, social work, physiotherapy,
occupational therapy, speech pathology, psychology, rehabilitation
bed | (30) |
| 15 | Pompili et
al, 2014 | Prospective
study | 2b | n=197, 122 of which
with GBM, sedation with midazolam, intramuscular phenobarbital for
seizure, hydration, tube feeding | (34) |
| 16 | Walbert and Khan,
2014 | Systematic
literature review | 1a | NA, interventions
include hydration, urinary catheterization, steroids, antiepileptic
drugs, oxygen insufflation, tube feeding and palliative
sedation | (17) |
| 17 | Ziobro et
al, 2008 | Retrospective
analysis | 3b | n=5,124 palliative
treatment with temozolomide | (31) |
| 18 | Oberndorfer et
al, 2008 | Retrospective
analysis | 3b | n=29, the majority
of patients were on antiepileptic drugs (AEDs), steroids, and
analgesics. | (32) |
| 19 | Reimer et
al, 1998 | Prospective
study | 2b | n=4, laser-induced
thermotherapy | (33) |
The present systematic review included articles
conducted in a variety of countries (Table II); the majority of articles were
from the USA (17,19,25,28,29,35,36), and
the remaining articles were from Germany (14,18,33,37),
Austria (16,32), Australia (26,30),
Poland (31), Italy (34), Ireland (27), and one study published by authors
from different nationalities (24).
 | Table IIGeographical distribution of
the included studies. |
Table II
Geographical distribution of
the included studies.
| Article no. | Authors: Study
title | Country | (Refs.) |
|---|
| 1 | Senderovich et
al: Evading Seizures: Phenobarbital Reintroduced as a
Multifunctional Approach to End-of-Life Care. | Published online
(Author nationalities: Canada, Ireland, Anguilla) | (24) |
| 2 | Witteler et
al: Palliative radiotherapy of primary glioblastoma. | Germany | (18) |
| 3 | Stavrinou et
al: Survival effects of a strategy favoring second-line
multimodal treatment compared to supportive care in glioblastoma
patients at first progression. | Germany | (14) |
| 4 | Hemminger et
al: Palliative and end-of-life care in glioblastoma: Defining
and measuring opportunities to improve care. | USA | (28) |
| 5 | Kuchinad et
al: End of life care for glioblastoma patients at a large
academic cancer center. | USA | (29) |
| 6 | Thier et al:
The Last 10 Days of Patients With Glioblastoma: Assessment of
Clinical Signs and Symptoms as well as Treatment. | Austria | (16) |
| 7 | Check et al:
Evidence that mifepristone, a progesterone receptor antagonist, can
cross the blood brain barrier and provide palliative benefits for
glioblastoma multiforme grade IV. | USA | (19) |
| 8 | Sundararajan et
al: Mapping the patterns of care, the receipt of palliative
care and the site of death for patients with malignant glioma. | Australia | (30) |
| 9 | Lin et al:
Inpatient palliative care consultation for patients with
glioblastoma in a tertiary hospital. | Australia | (26) |
| 10 | Ziobro et
al: Effects of palliative treatment with temozolomide in
patients with high-grade gliomas. | Poland | (31) |
| 11 | Oberndorfer et
al: The end-of-life hospital setting in patients with
glioblastoma. | Austria | (32) |
| 12 | Reimer et
al: MR-monitored LITT as a palliative concept in patients with
high grade gliomas: Preliminary clinical experience. | Germany | (33) |
| 13 | Wu et al:
Palliative Care Service Utilization and Advance Care Planning for
Adult Glioblastoma Patients: A Systematic Review. | USA | (36) |
| 14 | Kim et al:
Utilizing a Palliative Care Screening Tool in Patients With
Glioblastoma. | USA | (35) |
| 15 | Golla et al:
Effect of early palliative care for patients with glioblastoma
(EPCOG): a randomised phase III clinical trial protocol. | Germany | (37) |
| 16 | Pompili et
al: Home palliative care and end of life issues in glioblastoma
multiforme: results and comments from a homogeneous cohort of
patients. | Italy | (34) |
| 17 | Walbert and Khan:
End-of-life symptoms and care in patients with primary malignant
brain tumors: A systematic literature review. | USA | (17) |
| 18 | Glynn et al:
Glioblastoma Multiforme in the over 70's: ‘To treat or not to treat
with radiotherapy?’. | Ireland | (27) |
| 19 | Harrison et
al: Aggressiveness of care at end of life in patients with
high-grade glioma. | USA | (25) |
Palliative care
From each included study, different aspects were
evaluated, including the primary treatment administered if
applicable, the palliative care treatment introduced, whether the
study examined inpatients, outpatients, or both, and the outcomes
derived from each intervention. The median survival rate was
evaluated, and the recommendation was provided by the authors. In
the included studies, different palliative care therapies were used
as adjuvants with the primary treatment, targeting various aspects
of palliative care (Table
III).
 | Table IIISummary of the included studies. |
Table III
Summary of the included studies.
| First author | Aim of study | Total no. of
patients | GBM diagnosis
duration | Patients KPS score
or ECOG score (if mentioned) | Treatment of the
GBM (surgery, radiation, chemotherapy, no treatment or others) | Palliative care
treatment type | PC inpatient vs.
outpatient | Palliative care
treatment | Study outcomes | Median survival
rate of patients |
Recommendations | (Refs.) |
|---|
| Pompili | Identify home
palliative care and end of life issues in GBM | 197: Brain tumors,
122 of them GBM | NM | KPS score
>70 | NM | Supportive
treatment | Outpatient | Sedation with
midazolam + Intramuscular phenobarbital for seizure + hydration +
tube feeding | 1-End of life
palliative sedation with midazolam was necessary in 11% of cases to
obtain good control of symptoms such as uncontrolled delirium,
agitation, death rattle, or refractory seizures. 2-Intramuscular
phenobarbital is the authors' drug of choice for the severe
seizures that occurred in 30% of cases. | 13.34 months | 1-Future clinical
research strategies should include new models of care for patients
with brain tumors, with special attention given to palliative home
care models. | (34) |
| Oberndorfer | To evaluate the
end-of-life phase in a hospital setting in patients with GBM. | 29 | NM | Mean KPS phase 1=
70%/Phase 2= 50%/Phase 3= 20% | Surgery +
radiotherapy + subsequent chemotherapy/7-Surgery only (n=4), or
biopsy (n=3) | Symptoms drug +
physiotherapy + occupational therapy + logopedia + psychologic
assessment-directed to mobilize the patient and to strengthen his
remaining function, was only marginal in all three phases |
Inpatient/outpatient | Antiepileptic drugs
(AED) + steroids + analgesics | 1-End of life in
patients with glioblastoma has several periods with different
clinical aspects with respect to symptoms and treatment/2-Drug
treatment generally showed a continuous increase from phase 1 to 3
except steroids, which declined in phase 3. | The last 10 weeks
before death were divided into three periods. Phase 1, from 10 to 6
weeks before death; phase 2, 6 to 2 weeks before death; and phase
3, the last 2 weeks before death | 1-In Phase 3-All
medication should be promptly available and possibly given by a
nonoral route because dysphagia is present in the majority of
patients. 2-Practice of sedation in terminal ill patients has a
wide divergence among palliative care specialists and no clear
guidelines are available. 3-The requirement of further clinical
research to develop evidence-based guidelines. | (32) |
| Kuchinad | Retrospectively
analyze end-of-life care for GBM patients at academic center and
compare utilization of these services to national quality of care
guide, lines, Identifying opportunities to improve end-of-life
care. | 100 | NM | NM | Chemotherapy | NM |
Inpatient/outpatient | chemotherapy | 1-Documentation of
palliative care and end-of-life measures could improve quality of
care for GBM patients, especially in the use of ADs, symptom,
spiritual, and psychosocial assessments, with earlier use of
hospice to prevent end-of-life hospitalizations. 2-Hospice referral
and enrollment at Johns Hopkins exceeded national standards while
documentation of advance directives, and psychosocial assessments
demonstrated room for improvement. | 22 days | 1-More research is
needed to further define appropriate symptom management and
end-of-life care for this population. 2-Collaboration amongst
providers including neuro-oncologists, medical oncologists,
radiation oncologists, neuro-surgeons, social workers, chaplains
and other members of the care team can help optimize utilization of
palliative care measures at the end-of-life and identify and
establish necessary palliative care measures specific to the GBM
population. | (29) |
| Walbert | Review the
literature on end-of-life symptoms and end-of-life care of adult
patients with high-grade glioma (HGG). | NA | NM | NM | NM | Palliative care
interventions | Inpatients =3
studies/outpatients =2 studies/both =2 studies | Hydration + urinary
catheterization+ steroids + antiepileptic drugs + oxygen
insufflation + tube feeding + palliative sedation | 1-Patients with HGG
have a significant symptom load that worsens markedly at the end of
their lives (Poor communication, speech impairments, and cognitive
decline are common at the end-of-life period). | NM | 1-More prospective
studies are needed to better understand the end-of-life phase of
brain tumor patients. 2-Interventions should be evaluated to reduce
symptom burden and improve quality of life for patients and carers
without compromising the hope paradigm. | (17) |
| Reimer | Evaluate the
clinical utility of laser-induced thermotherapy (LITT] as a
palliative treatment for patients with high-grade glioma | 4 | NM | NM | Surgery +
radiotherapy | Laser-induced
thermotherapy | Inpatient | Laser-induced
thermotherapy | 1-Interventional
MRI-controlled LITT offers a number of potential treatment
benefits/2-MRI provides excellent topographic accuracy because of
its capability for soft tissue contrast, high spatial resolution,
and functional aspects. | NM | 1-The results have
yet to be verified in a larger clinical trial and then to be
compared with those of various other minimally invasive techniques.
2-Radiofrequency ablation, focused ultrasound, or cryosurgery are
alternative methods for tissue coagulation/ablation and have been
described for the ablation of brain tumors. | (33) |
| Lin | Examining the
symptoms, reasons for referral and outcomes of patients with GBM
referred to inpatient palliative care service. | 50 | The median time
from diagnosis of GBM to the palliative care consultation service
referral was 111 days (range 3-1,677). | NM |
94%-Surgery/54%-Radiotherapy/48%-chemotherapy | NM | Inpatient | Medication -
Steroids + Anti-epileptic drugs + Benzodiazepines/Allied health
involvement-Physiotherapy + Occupational therapy + Social work +
Speech pathology + Pastoral care | 1-Early palliative
care review of cancer patients can result in significant
improvements in pain, somnolence, and symptom distress scores as
well as overall well-being/2-The improvements were observed within
the first few days of consultation/3-Allied health services,
rehabilitation and psychosocial support are crucial components of
patient management. | The median time
from referral to date of death was 33 days (range 0-256), The
median length of inpatient stay was 9 days (range 2-35). The median
time from diagnosis of GBM to the palliative care consultation
service referral was 111 days (range 3-1677). | 1-Allied health
services, rehabilitation and psychosocial support are crucial
components of patient management | (26) |
| Check | Determine if
mifepristone could provide palliative benefits to patient with
end-stage stage IV glioblastoma multiforme | 1 | NM | NM | radiation +
chemotherapy | progesterone
receptor antagonist | NM |
mifepristone | 1-mifepristone
cross the blood-brain barrier and could be considered for
palliative therapy of other patients with chemotherapy-resistant
brain cancer/Within two weeks of taking mifepristone, patient
became more alert and able to carry-out intelligent. | NM | 1-Mifepristone does
cross the blood-brain barrier and could be considered for
palliative therapy of other patients with chemotherapy-resistant
brain cancer. Further studies are required to determine if the
35-kDa isoform of PIBF described by Lachman et al. in the cytoplasm
of cancer cells is identical to the 34-kDa form that rises. | (19) |
| Hemminger | Evaluate adherence
to 5 palliative care quality measures and explore associations with
patient outcomes in GBM | 117 | Diagnosis between
January 1, 2010 and May 1, 2015 | NM | Chemotherapy | Hospice care | Inpatient=
31/outpatient= 12 | NM | Early PC help with:
1-Reduce symptom burden. 2-Decrease rates of depression in patients
and caregivers. 3-Reduce costs of care. 4-Minimize hospitalizations
and in-hospital deaths. 5-Decrease aggressive end-of-life care.
6-Improve a patient's survival./but the study results are
consistent with the literature in illustrating that early
involvement of palliative care services is rare in
neuro-oncology. | 12.9 months | 1-Quality measures
in glioblastoma should focus on defining early advance directive
documentation, suggesting appropriate timing for hospice
enrollment, and determining which patients may benefit from early
palliative care interventions (GUIDELINES ARE NEEDED). | (28) |
| Wu | Exploring published
literature on the prevalence of ACP, end-of-life (EOL) services
utilization (including PC services), and experiences among adults
with GBM | NA | Median time from
diagnosis to PC consult measured in one study, found to be 111
days | NM | NM | NM |
Inpatient/outpatient | NM | 1-Proactive advance
care planning and appropriate use of palliative care resources are
critical aspects of high-quality care for these patients and their
caregivers/2-our findings suggest relatively low prevalence of both
of these components among GBM patients. | NM | 1-The field would
benefit from rigorous studies, particularly involving prospective
cohorts, to inform future improvements in ACP and EOL care for
adult GBM patients as well as to explore other pertinent
topics. | (36) |
| Kim | Investigate the
feasibility, value, and effectiveness of using an adapted
palliative care screening tool to improve out-patient palliative
care screening and referral of glioblastoma patients | 294 | NM | 90-100% 70-80%
50-60% 30-40% 10-20% 133 (45%) 123 (42%), 35 (12%), 3 (1%) | NM | NM | Outpatient | NM | 1-Utilizing a
palliative care screening tool may facilitate early referral to
palliative care and lead to improved patient outcomes in symptom
management and quality of life. | NM | 1-In future
studies, a query about patient acceptance regarding palliative care
is required to identify the most effective and efficient model of
early palliative care integrated with oncology care. | (35) |
| Sundararajan | Quantify the
association between symptoms, receipt of supportive and palliative
care and site of death. | 678 | NM | NM | NM | Palliative care
consult + Palliative care bed + Social work + Occupational therapy
+ Physiotherapy | inpatient | Palliative care
consult + Palliative care bed + Social work + Physiotherapy +
Occupational therapy + Speech pathology + Psychology +
Rehabilitation bed | Malignant glioma
patients with a high burden of symptoms more likely to receive
palliative care/Patients who receive palliative care more likely to
die at home | 10.4 months, and
14.3 months for all other patients with grade three tumors. 821
(41%) did not die by the end of follow up (30-June-2009), leaving
678 (34%) patients who survived longer than 120 days from diagnosis
and died within the follow-up period. | 1-Model of care for
this population should incorporate an earlier routine palliative
care referral, heralded by the onset of symptoms. The response of
treating clinicians to a relapse may include further anti-cancer
therapies, but should also routinely offer referral to palliative
care. For patients whose survival may be measured in months, this
should ensure receipt of palliative care involvement prior to their
last days of life. | (30) |
| Senderovich | Evaluate the role
of phenobarbital as a drug of choice in end-of-life (EOL)
settings. | 1 | NM | NM | NM | Subcutaneous
drug | NM | Phenobarbital | 1-Phenobarbital
reduced complications associated with EOL care + improve quality of
remaining life. | NM | 1-Information
regarding phenobarbital use for EOL care is underwhelming and
clearly should be further explored. | (24) |
| Witteler | Identify predictors
of survival after palliative radiotherapy | 31 | NM/select patients
diagnosed with GBM between (2006-2019) | Patients with (KPS
>= 60) showed improved survival compared to those with
(KPS=<50) | Surgery (Subtotal
resection or biopsy) + radiotherapy | Radiotherapy | inpatient | radiotherapy | 1-Palliative
radiotherapy increase in survival + reasonable option for patients
with limited survival prognoses. | NM | 1-Results need to
be confirmed in a larger prospective trial. | (18) |
| Glynn | Analyze survival
data and determine predictors of survival in patients aged ≥70
years treated with radiotherapy (RT) and/or Temozolomide. | 104 | NM | NM | Radiotherapy +/-
chemotherapy | Radiotherapy | NM | Radiotherapy
(hypofractionated palliative RT) | 1-Patients aged
70-75 years had survival rates similar to younger age groups.
2-Patients undergoing palliative RT had worse results. 3-Increasing
age was associated with poorer outcomes and decreased survival.
4-Age, surgical debulking, and good performance status were
independent predictors of improved survival. | 6.0 months | 1-Maximal surgical
resection if feasible for all ages. 2-For patients aged 70-75
years, if they have Debulked and good performance status, standard
approach radical RT/TMZ, 3-If they have biopsy only and good
performance status they recommend a standard approach radical
RT/TMZ versus short course RT (±TMZ), 4-If they have Poor
performance status they reccomaned to discuss short course RT
(±TMZ) versus best supportive care (BSC). 5-for patient aged more
than 76 years and they have good performance status and Debulked
they recommended to discuss short course RT (±TMZ) versus BSC, 6-If
they have Biopsy only and poor performance status they reccomanded
to have BSC. | (27) |
| Stavrinou | Examine whether a
strategy favoring active treatment of GBM at progression offers an
advantage in OS compared to supportive care alone. | 259 (center
A=103/center B=156) | June 2010-June
2015 | Center A= 91/center
B=146 | Surgery + adjuvant
radiotherapy + postoporative chemotherapy (6 cycles of
temozolomide) | Supportive
care | NM | supportive | 1-Treatment
favoring second-line treatment GBM recurrence or progression is
associated with significantly better survival after
progression. | Center A= 4.5
months/Center B= 7 months | NM | (14) |
| Ziobro | Assess the results
of treatment with temozolomide in patients with high-grade gliomas
who no longer benefit from surgical treatment and
radiotherapy. | 51,24 | NM | NM | Surgery +
Radiotherapy + Chemotherapy (lomustine) | Speech pathology +
Psychology + Pharmacy + Rehabilitation bed | NM | Temozolomide | 1-Objective benefit
from treatment with temozolomide was noted in 49% of patients in
the study group/2-Tolerability of temozolomide in patients with
malignant gliomas is good. | 32 weeks | NM | (31) |
Supportive treatment was one approach to palliative
and end-of-life care in patients with GBM, as Pompili et al
(34) aimed to identify home
palliative care and end-of-life issues in patients with GBM. They
found that midazolam was necessary in 11% of cases to achieve good
control of symptoms, such as delirium, agitation and refractory
seizures. In addition, phenobarbital was the drug of choice for
severe seizures, which occurred in 30% of cases (34).
Moreover, the use of phenobarbital was assessed by
Senderovich et al (24), in
an end-of-life setting; its use was found to reduce complications
associated with end-of-life care and improve the quality of
remaining life (24).
Kuchinad et al (29) conducted a retrospective analysis on
the management of patients with GBM, focusing on end-of-life care
practices at an academic center. Their study primarily evaluated
the use of chemotherapy as the main treatment approach for patients
with GBM, without exploring palliative interventions. By comparing
service utilization to national quality care guidelines, the
researchers identified gaps in documentation related to palliative
care and end-of-life planning. Their findings suggested that
improving these aspects could enhance the overall quality of care
provided to patients with GBM (29).
In patients receiving the full course of treatment,
including surgery, chemotherapy and radiotherapy, multiple
palliative care interventions were used to improve the quality of
life of these patients. Among such studies, Oberndorfer et
al (32) focused on symptomatic
management, including antiepileptic drugs (AEDs), steroids and
analgesia, physiotherapy, and occupational therapy in end-of-life
patients. They classified the end-of-life into phases, from phase 1
to 3. These interventions were associated with symptomatic
improvement in end-of-life patients, particularly when introduced
via the non-oral route, given that the majority of patients
developed dysphagia at this stage (32).
Lin et al (26) investigated steroids, AEDs,
benzodiazepines and allied health involvement. They found that
early palliative care resulted in a significant improvement in
pain, somnolence, symptoms and distress score; they recommended the
initiation of palliative care not only with medication treatment,
but also with rehabilitation, along with psychosocial support
(26).
Stavrinou et al (14) compared supportive care and
second-line, tumor-focused treatment at first progression in two
different groups. They found that second-line treatment, which is
tumor-focused, is more effective in terms of outcomes and in terms
of overall survival (14).
Apart from supportive care, Ziobro et al
(31) examined the effects of
palliative treatment with temozolomide in patients with high-grade
gliomas. They found this treatment to be beneficial in 49% of
patients in the study group (31).
Overall, standardizing guidelines for end-of-life
care in patients with GBM was suggested by Thier et al
(16), when they studied the
symptoms and signs in the last 10 days prior to mortality, and how
these could affect the health and care of patients (16).
In studies using radiotherapy and surgery as the
primary treatment for GBM, Witteler et al (18) used radiotherapy as a palliative care
treatment and found that it increased the survival rate, and that
it was a reasonable option for patients with a limited prognosis.
On the other hand, Reimer et al (33) used laser-induced thermotherapy (LITT)
and found that interventional MRI controlled LITT and that it
provided potential treatment benefits; MRI provides excellent
topographic accuracy due to its capability for soft tissue contrast
with high specific resolution and functional aspects (33).
Location of mortality
The location of mortality of patients with GBM
differs between hospitals and health institutes, homes and hospice
care. Out of the 19 studies included in the present systematic
review, 10 studies reported hospitals as the place of mortality
(Table IV) (16,17,24,26,28-30,32,34,36).
 | Table IVLocation of mortality reported in the
included studies. |
Table IV
Location of mortality reported in the
included studies.
| Location of
mortality | Percentage of
mortality | No. of studies |
|---|
| Home | 33.33 | 7 |
| Hospital | 57.14 | 10 |
| Hospice | 19.05 | 4 |
| NM | 42.86 | 9 |
Wu et al (36)
performed a systematic review of palliative care service
utilization and advance care planning. They demonstrated that the
location of mortality was mentioned in only six out of the 16
studies included, and they similarly found that mortality in health
care institutes was the most common compared to other locations,
reaching up to 78% (36).
Mortality at home was reported in seven studies,
with the numbers of patients varying from 12 to 53% (17,19,28-30,34,36).
On the other hand, hospice care was the least mentioned among the
included studies as the site of mortality (28,29,34,38). Wu
et al (36) found that the
mortality rate in this setting ranged from 12to 64%. However,
Sundararajan et al (30)
found that this rate was 49%.
Discussion
The present study reviewed and systematically
analyzed the available literature on patients with GBM receiving
palliative care. GBM is considered to be the most common type of
brain tumor in adults. It accounts for 45.6% of all brain tumors
(1-5).
It is generally associated with a very poor prognosis, as well as
with a high recurrence rate (7,8,13). The treatment of patients with GBM
includes maximal surgical resection with adjuvant radiotherapy
(7,9).
Other modalities of treatment include supportive
care as decided upon by the treating physician; however, other
researchers advocate for tumor-specific multidisciplinary
approaches to plan the treatment (14). Palliative care is currently
recommended by the ASCO Clinical Practice Guidelines to be
considered when treating patients with GBM (20).
A variety of studies investigating the management
and palliative care of patients with GBM have been published. The
present systematic review included publications over a wide range
of years, from 1998 to 2022. It was found that 2014 accounted for
the highest number of publications, which included four
publications, followed by 2021 (Fig.
2). However, Wu et al (36) demonstrated that 2014, 2017 and 2018
were the years with the highest number of publications. Moreover,
Ironside et al (38) found
that 2012 was the year with the highest number of publications.
Mean survival age
As GBM is a disease that is associated with a poor
prognosis, improving the QOL and prolonging the life expectancy of
patients is the main aim of palliative care, not only for patients
but also for their families (39).
The total number of patients who were diagnosed with grade 4 GBM
between 2004 and 2017 and received palliative care was
2,803(40). Compared to the results
of the present study, the total number of patients who received
palliative care was 1,630, and this was expected, as some of the
selected articles did not mention the exact number of patients who
received palliative care from GBM. In terms of the ability to carry
out daily activities, the studies have a KPS >50% with variable
modalities of palliative care. Specifically, patients who received
radiotherapy had a KPS score >60%, which is consistent in
comparison with other studies that reported patients who received
radiotherapy had a KPS score >60% (38).
Palliative care in GBM
In the present systematic review, the median
survival rate reached 14 months, which was consistent with a
recently published retrospective study by Mohammed et al
(41). Providing the optimal
treatment when dealing with patients who require palliative care is
critical; it is highly recommended to establish a specific and
well-structured palliative care guideline for patients with GBM
(16,32). Moreover, further research is
warranted to define appropriate symptom management for those
patients, which will be also helpful in the process of establishing
GBM palliative care guidelines (17,34,42).
Making these guidelines universal will ensure the right of patients
to receive all and appropriate methods of palliative care and
participation from multiple specialties recommended to target and
deliver the optimal options for the patient (34).
Location of mortality
The location of mortality for patients with GBM
varies across hospitals, homes and hospice care. Out of the 19
studies included in the present systematic review, 10 of these
reported the hospital as the place of mortality (16,17,24,26,28-30,32,34,36).
This may be explained by the late hospitalization, particularly in
intensive care, which has resulted in mortality in acute hospital
care (43). Wu et al
(36) performed a systematic review
of palliative care service utilization and advance care planning,
and demonstrated that the location of mortality was mentioned in
only six out of 16 studies included; they similarly found that
mortality in health care institutes was the most common compared to
other places, reaching up to 78% (36).
However, Sundararajan et al (30) performed a retrospective study and
found that 25% of the patients died in an acute hospital bed. Thus,
the majority of the patients prefer to die at home, as shown by
Barbaro et al (43).
Moreover, home deaths were reported to range from 12 to 53.1%
(17,19,28-30,34,36),
which is less than the number reported by Wu et al (36) in their review.
As regards hospice care, the analysis revealed this
to be the least common site of mortality (17,29,30,34). Wu
et al (36) found that the
mortality rate in this setting ranged from 12 to 64%. However,
Sundararajan et al (30)
found that this rate to be 49%.
Limitations and future
implications
The present systematic review was not without any
limitations. Moreover, with such a prolonged study period, limited
studies were found focusing on palliative care at the end-of-life
for patients of GBM. In addition, end-of-life care can be
challenging, and subjective measures will be limited to assess the
needs of patients, and the outcomes of such an intervention, which
will limit the study outcome.
In conclusion, patients with GBM have a poor
prognosis and a poor survival rate, even with the optimal treatment
available. Moreover, multiple signs and symptoms can have a
tremendous burden on the end of life of patients and their
families. Palliative care in these patients aims to relieve the
burden of end-of-life care and improve the quality of life for them
and their families. Different palliative care options were studied
that led to the effective relief of patient symptoms, including
symptomatic treatment, the involvement of other services, such as
physiotherapy and some medications targeting each symptom and
radiotherapy. Overall, the early planning and involvement of these
services are critical and have a notable impact on the end-of-life
of patients.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
AMAG and SAB were involved in data collection, data
analysis and in the writing of the manuscript. AMAA was involved in
data analysis and in the writing of the manuscript. DAH was
involved in data collection. AAH was involved in data analysis, and
in the writing and editing of the manuscript. TAS conceived and
designed the study, and was involved in writing the manuscript.
AMAG, SAB, AMAA, DAH and AAH confirm the authenticity of all the
raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Nabors LB, Portnow J, Ahluwalia M,
Baehring J, Brem H, Brem S, Butowski N, Campian JL, Clark SW,
Fabiano AJ, et al: Central nervous system cancers, version 3.2020,
NCCN clinical practice guidelines in oncology. J Natl Compr Canc
Netw. 18:1537–1570. 2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Theeler BJ and Gilbert MR: Advances in the
treatment of newly diagnosed glioblastoma. BMC Med.
13(293)2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Tykocki T and Eltayeb M: Ten-year survival
in glioblastoma. A systematic review. J Clin Neurosci. 54:7–13.
2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Stupp R, Taillibert S, Kanner A, Read W,
Steinberg D, Lhermitte B, Toms S, Idbaih A, Ahluwalia MS, Fink K,
et al: Effect of tumor-treating fields plus maintenance
temozolomide vs maintenance temozolomide alone on survival in
patients with glioblastoma: A randomized clinical trial. JAMA.
318:2306–2316. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Stupp R, Taillibert S, Kanner AA, Kesari
S, Steinberg DM, Toms SA, Taylor LP, Lieberman F, Silvani A, Fink
KL, et al: Maintenance therapy with tumor-treating fields plus
temozolomide vs temozolomide alone for glioblastoma: A randomized
clinical trial. JAMA. 314:2535–2543. 2015.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ostrom QT, Cioffi G, Waite K, Kruchko C
and Barnholtz-Sloan JS: CBTRUS statistical report: Primary brain
and other central nervous system tumors diagnosed in the United
States in 2014-2018. Neuro Oncol. 23 (12 Suppl 2):iii1–iii105.
2021.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Lacroix M, Abi-Said D, Fourney DR,
Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbusch
SJ, Holland E, et al: A multivariate analysis of 416 patients with
glioblastoma multiforme: Prognosis, extent of resection, and
survival. J Neurosurg. 95:190–198. 2001.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Curran WJ Jr, Scott CB, Horton J, Nelson
JS, Weinstein AS, Fischbach AJ, Chang CH, Rotman M, Asbell SO,
Krisch RE, et al: Recursive partitioning analysis of prognostic
factors in three Radiation Therapy Oncology Group malignant glioma
trials. J Natl Cancer Inst. 85:704–710. 1993.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Walker MD, Green SB, Byar DP, Alexander E,
Batzdorf U, Brooks WH, Hunt WE, MacCarty CS, Mahaley MS Jr, Mealey
J Jr, et al: Randomized comparisons of radiotherapy and
nitrosoureas for the treatment of malignant glioma after surgery. N
Engl J Med. 303:1323–1329. 1980.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Stupp R, Mason WP, van den Bent MJ, Weller
M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn
U, et al: Radiotherapy plus concomitant and adjuvant temozolomide
for glioblastoma. N Engl J Med. 352:987–996. 2005.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Stupp R, Hegi ME, Mason WP, van den Bent
MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B,
Belanger K, et al: Effects of radiotherapy with concomitant and
adjuvant temozolomide versus radiotherapy alone on survival in
glioblastoma in a randomised phase III study: 5-year analysis of
the EORTC-NCIC trial. Lancet Oncol. 10:459–466. 2009.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ozdemir-Kaynak E, Qutub AA and
Yesil-Celiktas O: Advances in glioblastoma multiforme treatment:
New models for nanoparticle therapy. Front Physiol.
9(170)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Roy S, Lahiri D, Maji T and Biswas J:
Recurrent glioblastoma: Where we stand. South Asian J Cancer.
4:163–173. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Stavrinou P, Kalyvas A, Grau S, Hamisch C,
Galldiks N, Katsigiannis S, Kabbasch C, Timmer M, Goldbrunner R and
Stranjalis G: Survival effects of a strategy favoring second-line
multimodal treatment compared to supportive care in glioblastoma
patients at first progression. J Neurosurg. 131:1136–1141.
2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Kavalieratos D, Corbelli J, Zhang D,
Dionne-Odom JN, Ernecoff NC, Hanmer J, Hoydich ZP, Ikejiani DZ,
Klein-Fedyshin M, Zimmermann C, et al: Association between
palliative care and patient and caregiver outcomes: A systematic
review and meta-analysis. JAMA. 316:2104–2114. 2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Thier K, Calabek B, Tinchon A, Grisold W
and Oberndorfer S: The last 10 days of patients with glioblastoma:
Assessment of clinical signs and symptoms as well as treatment. Am
J Hosp Palliat Care. 33:985–988. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Walbert T and Khan M: End-of-life symptoms
and care in patients with primary malignant brain tumors: A
systematic literature review. J Neurooncol. 117:217–224.
2014.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Witteler J, Schild SE and Rades D:
Palliative radiotherapy of primary glioblastoma. In Vivo.
35:483–487. 2021.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Check JH, Wilson C, Cohen R and Sarumi M:
Evidence that Mifepristone, a progesterone receptor antagonist, can
cross the blood brain barrier and provide palliative benefits for
glioblastoma multiforme grade IV. Anticancer Res. 34:2385–2388.
2014.PubMed/NCBI
|
|
20
|
Ferrell BR, Temel JS, Temin S, Alesi ER,
Balboni TA, Basch EM, Firn JI, Paice JA, Peppercorn JM, Phillips T,
et al: Integration of palliative care into standard oncology care:
American society of clinical oncology clinical practice guideline
update. J Clin Oncol. 35:96–112. 2017.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Triebel KL, Martin RC, Nabors LB and
Marson DC: Medical decision-making capacity in patients with
malignant glioma. Neurology. 73:2086–2092. 2009.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Brinkman-Stoppelenburg A, Rietjens JA and
van der Heide A: The effects of advance care planning on
end-of-life care: A systematic review. Palliat Med. 28:1000–1025.
2014.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Houben CHM, Spruit MA, Groenen MTJ,
Wouters EFM and Janssen DJA: Efficacy of advance care planning: A
systematic review and meta-analysis. J Am Med Dir Assoc.
15:477–489. 2014.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Senderovich H, Waicus S and Mokenela K:
Evading seizures: Phenobarbital reintroduced as a multifunctional
approach to end-of-life care. Case Rep Oncol. 15:218–224.
2022.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Harrison RA, Ou A, Naqvi SMAA, Naqvi SM,
Weathers SS, O'Brien BJ, de Groot JF and Bruera E: Aggressiveness
of care at end of life in patients with high-grade glioma. Cancer
Med. 10(8387)2021.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Lin E, Rosenthal MA, Eastman P and Le BH:
Inpatient palliative care consultation for patients with
glioblastoma in a tertiary hospital. Intern Med J. 43:942–945.
2013.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Glynn AM, Rangaswamy G, O'Shea J, Dunne M,
Grogan R, MacNally S, Fitzpatrick D and Faul C: Glioblastoma
Multiforme in the over 70's: ‘To treat or not to treat with
radiotherapy?’. Cancer Med. 8:4669–4677. 2019.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Hemminger LE, Pittman CA, Korones DN,
Serventi JN, Ladwig S, Holloway RG and Mohile NA: Palliative and
end-of-life care in glioblastoma: Defining and measuring
opportunities to improve care. Neurooncol Pract. 4:182–188.
2017.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Kuchinad KE, Strowd R, Evans A, Riley WA
and Smith TJ: End of life care for glioblastoma patients at a large
academic cancer center. J Neurooncol. 134:75–81. 2017.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Sundararajan V, Bohensky MA, Moore G,
Brand CA, Lethborg C, Gold M, Murphy MA, Collins A and Philip J:
Mapping the patterns of care, the receipt of palliative care and
the site of death for patients with malignant glioma. J Neurooncol.
116:119–126. 2014.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ziobro M, Rolski J, Grela-Wojewoda A,
Zygulska A and Niemiec M: Effects of palliative treatment with
temozolomide in patients with high-grade gliomas. Neurol Neurochir
Pol. 42:210–215. 2008.PubMed/NCBI
|
|
32
|
Oberndorfer S, Lindeck-Pozza E, Lahrmann
H, Struhal W, Hitzenberger P and Grisold W: The end-of-life
hospital setting in patients with glioblastoma. J Palliat Med.
11:26–30. 2008.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Reimer P, Bremer C, Horch C, Morgenroth C,
Allkemper T and Schuierer G: MR-monitored LITT as a palliative
concept in patients with high grade gliomas: Preliminary clinical
experience. J Magn Reson Imaging. 8:240–244. 1998.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Pompili A, Telera S, Villani V and Pace A:
Home palliative care and end of life issues in glioblastoma
multiforme: Results and comments from a homogeneous cohort of
patients. Neurosurg Focus. 37(E5)2014.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Kim JY, Peters KB, Herndon JE II and
Affronti ML: Utilizing a palliative care screening tool in patients
with glioblastoma. J Adv Pract Oncol. 11:684–692. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Wu A, Ruiz Colón G, Aslakson R, Pollom E
and Patel CB: Palliative care service utilization and advance care
planning for adult glioblastoma patients: A systematic review.
Cancers (Basel). 13(2867)2021.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Golla H, Nettekoven C, Bausewein C, Tonn
JC, Thon N, Feddersen B, Schnell O, Böhlke C, Becker G, Rolke R, et
al: Effect of early palliative care for patients with glioblastoma
(EPCOG): A randomised phase III clinical trial protocol. BMJ Open.
10(e034378)2020.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Ironside SA, Sahgal A, Detsky J, Das S and
Perry JR: Update on the management of elderly patients with
glioblastoma: A narrative review. Ann Palliat Med. 10:899–908.
2021.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Teoli D, Schoo C and Kalish VB: Palliative
Care. StatPearls [Internet]. 2023 Feb 6 [cited 2024 Apr 15];
Available from: https://www.ncbi.nlm.nih.gov/books/NBK537113/.
|
|
40
|
Pando A, Patel AM, Choudhry HS, Eloy JA,
Goldstein IM and Liu JK: Palliative care effects on survival in
glioblastoma: Who receives palliative care? World Neurosurg.
170:e847–e857. 2023.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Mohammed S, Dinesan M and Ajayakumar T:
Survival and quality of life analysis in glioblastoma multiforme
with adjuvant chemoradiotherapy: A retrospective study. Rep Pract
Oncol Radiother. 27:1026–1036. 2022.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Seekatz B, Lukasczik M, Löhr M, Ehrmann K,
Schuler M, Keßler AF, Neuderth S, Ernestus RI and van Oorschot B:
Screening for symptom burden and supportive needs of patients with
glioblastoma and brain metastases and their caregivers in relation
to their use of specialized palliative care. Support Care Cancer.
25:2761–2770. 2017.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Barbaro M, Blinderman CD, Iwamoto FM,
Kreisl TN, Welch MR, Odia Y, Donovan LE, Joanta-Gomez AE, Evans KA
and Lassman AB: Causes of death and end-of-life care in patients
with intracranial high-grade gliomas: A retrospective observational
study. Neurology. 98:e260–e266. 2022.PubMed/NCBI View Article : Google Scholar
|