Introduction
Leiomyomas, also known as fibroids, are the most
common benign gynecological tumors, typically found in
premenopausal women. Leiomyomas are diagnosed more frequently in
women of African origin compared to Caucasian women (80 vs. 70%);
however, the incidence of clinical symptoms in patients of African
origin is double than that observed in Caucasian women (1). Despite the high prevalence rates, the
pathophysiological mechanisms of uterine leiomyomas remain
incompletely understood. Various pathogenic mechanisms have been
proposed, involving genes, growth factors, cytokines, chemokines
and microRNA deviations (2). In
particular, there appears to be a strong association with estrogen
and progesterone levels, as the expression of both hormonal
receptors is higher in leiomyomas than in the normal myometrium
(3). The activation of receptors is
hypothesized to lead to the inhibition of key tumor suppression
genes, such as p53 and to promote the release of growth factors,
ultimately stimulating endometrial development (3). Apart from the hormonal milieu, certain
genetic mutations have been found to be associated with the
presence of leiomyomas, such as genes located in the 10q24.33
region, which are associated with myogenic differentiation and
cytoskeletal structure; impairment of which may explain the
proliferation of mesenchymal tissues and the tendency towards the
formation of leiomyomas (4).
Epigenetic factors have also been examined as potential causes of
leiomyoma development, such as microRNAs, which have been observed
to be dysregulated in leiomyomas compared to the healthy myometrium
and in turn, likely affect gene expression and cellular
development, leading to favorable conditions for the formation of
fibroids (3,4).
Leiomyomas of the female reproductive system may be
located in the uterus or in extrauterine sites (extrauterine
leiomyomas). Extrauterine leiomyomas that develop in the broad
ligament or, more rarely, in the round ligament, in the uterosacral
ligament, or the ovaries are rare (5). From the leiomyomas that develop within
the uterus (uterine leiomyomas), those found in the uterine body
(corpus uteri) are by far the most common and may be intramural,
subserosal or submucosal; while leiomyomas that develop in the
cervix of the uterus (cervical leiomyomas) are significantly less
frequent (6), being estimated to
comprise only a mere 0.6% of all uterine leiomyomas (7).
Cervical leiomyomas, depending on their location
within the cervix, can be further classified as extracervical or
intracervical leiomyomas, with the latter located within the cervix
(as in the case described herein). Extracervical cervical
leiomyomas (subserosal), which are characterized by the tumor
developing outside the cervical canal, can be further categorized
into anterior, posterior and lateral, depending on their position
in the cervix. Giant cervical leiomyomas, which can reach a maximum
diameter >15 cm, as in the patient in the present study, are
extremely rare. Obstructive uropathy accompanied by renal
dysfunction is a rare clinical manifestation of these tumors
(6).
The present case report describes the successful
surgical management of a rare case of giant cervical leiomyoma
associated with bilateral ureterohydronephrosis and retroperitoneal
perinephric urinoma formation at the level of the left kidney.
Furthermore, particular emphasis is placed on the challenging
pre-operative diagnostic approach and the significant
intraoperative difficulties encountered in the effective surgical
management of such complex cases to achieve the best postoperative
outcome.
Case report
A 51-year-old patient, with two previous cesarean
sections in her obstetric history, presented to the Emergency
Department of the General Hospital of Trikala, Trikala, Greece,
complaining of an inability to urinate. Urinary retention was
confirmed following the placement of a Foley catheter (no. 18). The
patient also reported constipation, dysuria, frequent urination and
pain in the lower abdomen extending primarily to the lumbar
regions. The onset of symptoms dated back ~6 months, with gradual
worsening in intensity. The last normal menstrual period of the
patient was 8 months prior. Since then, she had experienced
menorrhagia and abnormal vaginal bleeding. Her body mass index was
normal (23.9). In her medical history, hypothyroidism was noted,
with thyroid hormones well-regulated under medication. There were
no reports of recurrent urinary tract infections, chronic kidney
disease, or gastrointestinal disorders. According to the patient,
this was her first episode of urinary retention.
Upon a clinical examination, the abdomen was found
to be soft, with no signs of peritoneal irritation. Blood pressure
and heart rate were normal (130/80 mmHg and 87 beats/min). The
patient's body temperature was 36.8˚C. Tenderness was noted upon
the percussion of the kidney areas bilaterally (positive Giordano's
sign). Intravenous antibiotic therapy with cefoxitin
(Mefoxil®) at a dose of 2 g every 8 h was initiated. Of
note, ~2 cm below the umbilicus, a hard mass was palpated,
suspected to be a uterine fibroid or the uterine fundus. During
vaginal examination, minor vaginal bleeding was observed. The
cervix was displaced backward and to the left and appeared effaced
(Fig. 1). The Pap smear was negative
for malignancy. Laboratory tests upon admission revealed mildly
elevated inflammation markers. Tumor markers were within normal
limits (Table I). Urine culture
showed no evidence of urinary tract infection.
 | Table ILaboratory tests of the patient from
the day of admission to the clinic until the day of discharge. |
Table I
Laboratory tests of the patient from
the day of admission to the clinic until the day of discharge.
| Laboratory tests | Day of admission to
the clinic | Day before
surgery | 1st post-operative
day | 2nd post-operative
day | 5th post-operative
day | Normal laboratory
values |
|---|
| Ht | 36.24% | 33.85% | 26.1% | 23.4% | 28.2% | 37.7-49.7% |
| Hb | 12.1 gr/dl | 11.6 gr/dl | 8.5 gr/dl | 7.5 gr/dl | 8.9 gr/dl | 11.8-17.8 gr/dl |
| PLT |
275x103/ml |
271x103/ml |
165x103/ml |
158x103/ml |
194x103/ml | 150-350
x103/ml |
| WBC |
11.3x103/ml |
9.2x103/ml |
21.7x103/ml |
15.3x103/ml |
9.1x103/ml | 4-10.8
x103/ml |
| NEUT | 78.9% | 71.1% | 91.5% | 81.4% | 69.3% | 40-75% |
| CRP | 0.75 mg/dl | 0.45 mg/dl | | | | <0.7 mg/dl |
| APTT | 29.8 sec | 28.6 sec | 34.1 sec | 36.1 sec | 31.1 sec | 24.0-35.0 sec |
| INR | 0.92 | 0.90 | 1.02 | 1.07 | 0.97 | 0.8-1.2 |
| FIB | 255 mg/dl | 251 mg/dl | 222 mg/dl | 215 mg/dl | 227 mg/dl | 200-400 mg/dl |
| Glu | 110 mg/dl | 85 mg/dl | 91 mg/dl | 87 mg/dl | 85 mg/dl | 75-115 mg/dl |
| Cr | 0.75 mg/dl | 0.63 mg/dl | 0.67 mg/dl | 0.61 mg/dl | 0.62 mg/dl | 0.40-1.10 mg/dl |
| Κ+ | 3.7 mmol/l | 3.9 mmol/l | 3.4 mmol/l | 4.2 mmol/l | 3.9 mmol/l | 3.5-5.1 mmol/l |
| Να+ | 141.4 mmol/l | 142.3 mmol/l | 137.3 mmol/l | 139.4 mmol/l | 141.1 mmol/l | 136-145 mmol/l |
| B | 0.48 mg/dl | - | - | - | 0.74 mg/dl | 0.3-1.2 mg/dl |
| SGOT | 29 IU/l | - | - | - | 27 IU/l | 5-33 IU/l |
| SGPT | 27 IU/l | - | - | - | 24 IU/l | 10-37 IU/l |
| CEA | 2.85 ng/ml | - | - | - | - | <5 ng/ml |
| CA 125 | 18.3 U/ml | - | - | - | - | ≤35 U/ml |
| CA 15-3 | 19.4 U/ml | - | - | - | - | 0.0-31.3 U/ml |
| CA 19-9 | 13.1 U/ml | - | - | - | - | 0.0-37 U/ml |
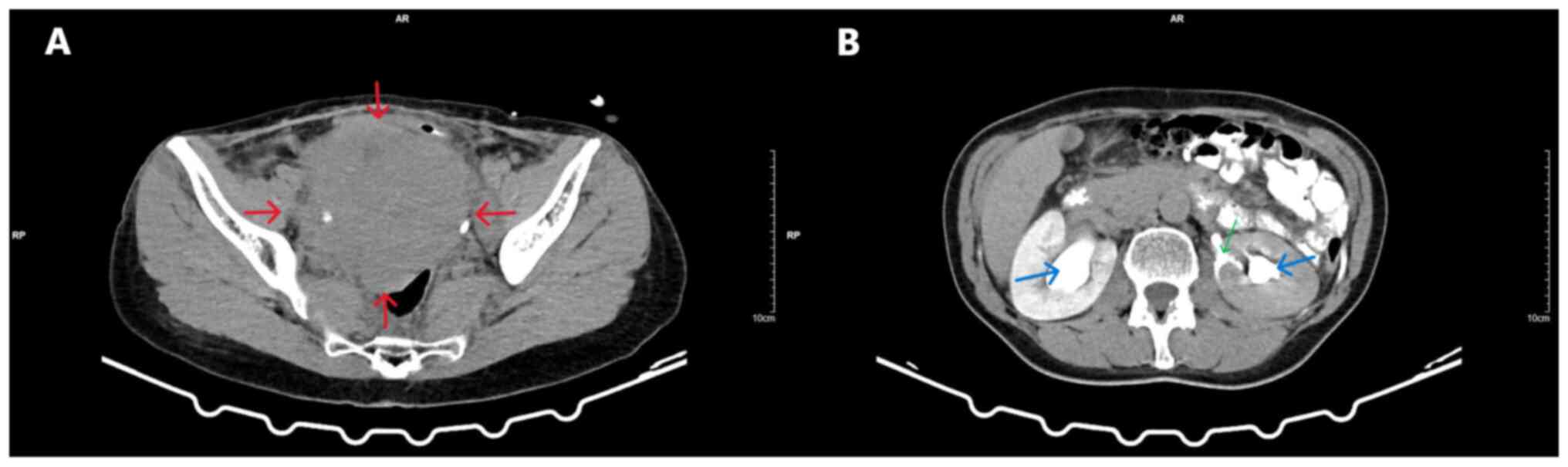
Transvaginal ultrasound was non-diagnostic due to
the large size of the mass. Similarly, the findings from the
transabdominal ultrasound were also non-diagnostic. A computed
tomography (CT) scan revealed a large (16x12x10 cm) solid echogenic
mass with clear boundaries and signs of cystic degeneration,
occupying the entire pelvis, likely originating from the cervix,
and causing the compression of the ureters. The non-obstructive
dilation of the pelvicalyceal system and the upper and middle third
of the right ureter, due to chronic hydronephrotic changes, was
observed in the right kidney. In the left kidney, in addition to
pelvicalyceal dilation and dilation of the upper and middle third
of the left ureter, a small filling defect was noted in the middle
calyceal group, with a cup-shaped deformation of the upper and
lower calyces and extravasation of contrast into the
retroperitoneal space, consistent with a perinephric urinoma
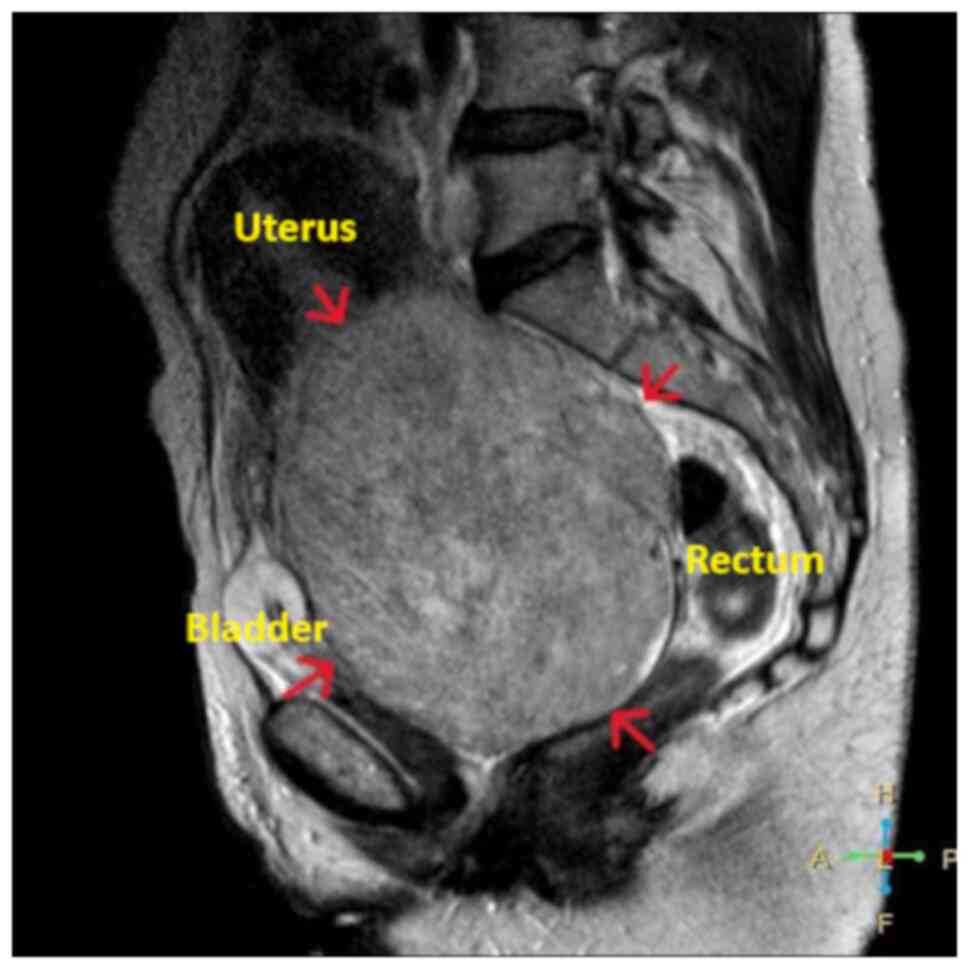
(Fig. 2). Magnetic resonance imaging
(MRI) revealed a well-defined pelvic mass measuring 16.5x12.5x11
cm, originating from the endocervix. Due to its large size, the
mass appeared to displace the endocervix backward and to the left
and the uterine body upward, making it palpable through the
abdominal wall and suggesting a diagnosis of a giant uterine
leiomyoma (Fig. 3). No
pathologically enlarged lymph nodes were visible on the current CT
or MRI imaging. Pre-operative ureteral stent placement was deemed
necessary, both for the intraoperative protection of the ureters
and for the therapeutic management of bilateral pelvicalyceal
system dilation.
Based on the imaging findings, the diagnosis of
giant cervical leiomyoma of the uterus was made. Following the
thorough consultation with the surgical team regarding the severity
of her condition, the presentation of the available treatment
options and after taking into consideration her peri-menopausal
status and the absence of further childbearing desire, the patient
consented to the recommendation of the team for an abdominal total
hysterectomy with bilateral salpingo-oophorectomy.
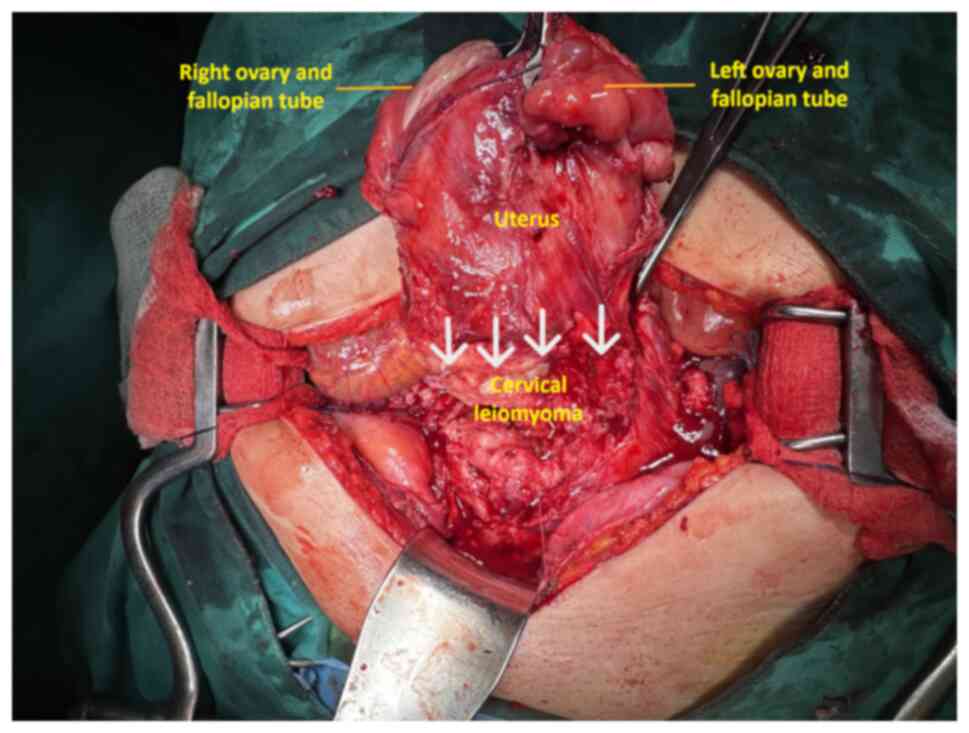
Intraoperatively, a giant cervical leiomyoma was found, wedged in
the pelvis and adherent primarily to the anterior pelvic wall due
to the previous cesarean sections, making its mobilization
difficult. The uterine body and ovaries were not involved in the
lesion (Fig. 4). The hysterectomy
was technically challenging. The electrothermal bipolar vessel
sealing device (LigaSure™) significantly aided in
reducing the risk of intraoperative bleeding. For the
intraoperative blood loss and hemodynamic stabilization of the
patient, a total of 3 units of whole blood and 1 unit of plasma
were transfused (2 units of blood and 1 plasma intraoperatively,
and 1 unit of blood on the second postoperative day) (Table I). During surgical maneuvers, a
traumatic rupture of the bladder ~5 cm in length occurred, which
was repaired in layers. Urological intervention was not required to
drain the urinoma. It was deemed appropriate to monitor the lesion
and leave the ureteral stents in place post-operatively to manage
the dilation of the pelvicalyceal system.
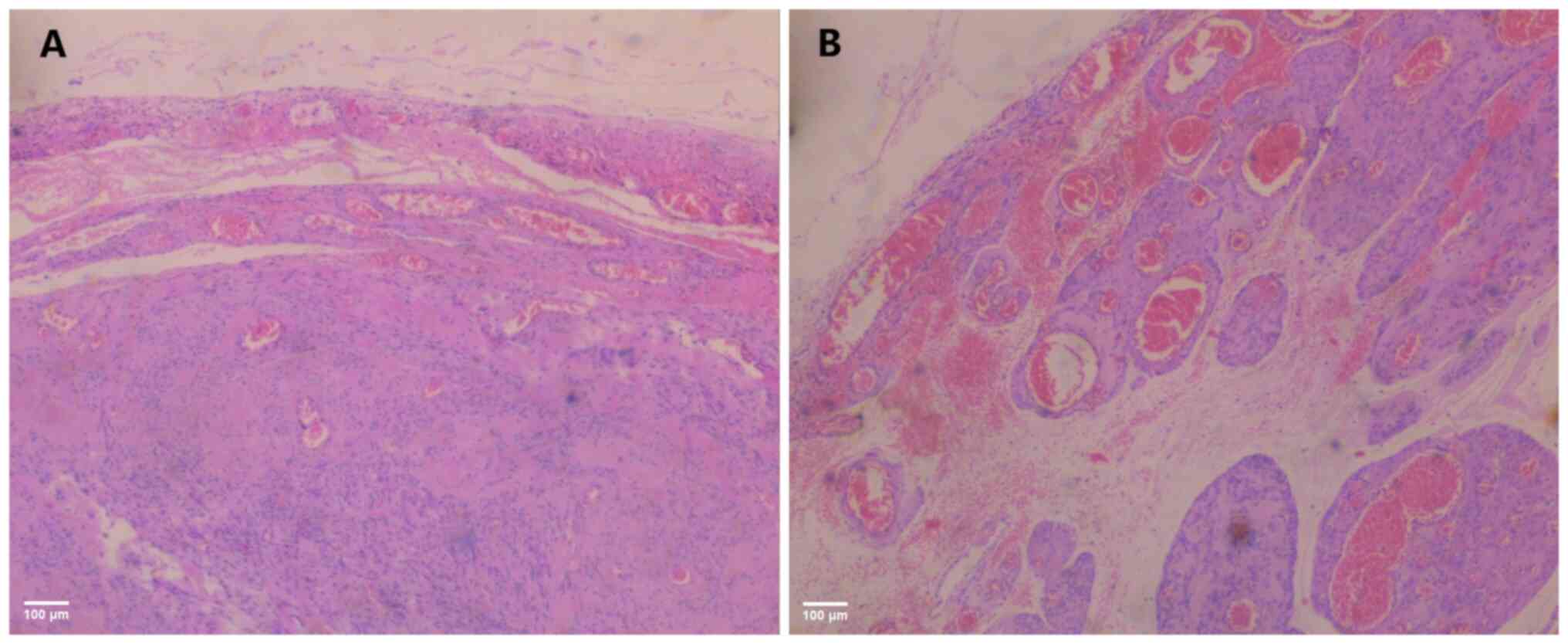
A histological examination of the surgical specimen
was performed in accordance with routine protocols of the authors'
laboratory. Specimens were embedded in paraffin cubes and sections
with a thickness of 5 µm were obtained for analysis. A buffered,
10% formalin solution was utilized as a fixative medium, for 36 h
at room temperature. Hematoxylin and eosin 0.5% alcohol solution
(Diachel A.E.) staining was used, at room temperature with a 12-min
duration. All microscopic examinations were performed using a LEICA
DM2000 optical microscope (Leica Microsystems GmbH). The
histological examination of the surgical specimen confirmed the
diagnosis of cervical leiomyoma of the uterus. A microscopic
examination revealed mild to moderate cellularity with no mitoses.
Necrosis or cytological atypia was not observed (Fig. 5).
Following an uneventful post-operative course, the
patient was discharged on the 5th post-operative day. The urinary
catheter was removed at 5 days after discharge. Urinary function
was restored without issues. Following the recommendation of the
urologists, the ureteral stents were removed 3 months after
surgery, at which time the renal ultrasound was normal, without
pelvicalyceal system dilation or perinephric urinoma (Fig. 6).
Discussion
The clinical diagnosis of giant cervical leiomyomas
of the uterus presents a challenge in everyday medical practice.
The clinical symptoms are non-specific and usually relate to the
pressure of the enlarged cervical leiomyoma on adjacent pelvic
organs, occupying the entire pelvic cavity. Therefore, pain
localized in the lower abdomen, primarily radiating to the lumbar
regions or, less frequently, to the kidney areas, abdominal
distension, intense dysuric discomfort, urinary retention and
constipation are the most common clinical manifestations of giant
cervical leiomyomas of the uterus (8). In contrast to uterine body fibroids,
abnormal uterine bleeding is not a frequent symptom in patients
with cervical leiomyomas (9). Thus,
it is not surprising that the patient described herein did not
report symptoms related to menstruation. In addition, it is not
unexpected that constipation, urinary retention and hydronephrosis
were the main symptoms in the patient described herein. A potential
surprise could be the non-traumatic and non-obstructive rupture of
the renal parenchyma and the formation of a retroperitoneal
perinephric urinoma, a clinical entity that is uncommon in
practice.
An urinoma is an encapsulated collection of
extravasated urine leaking from the urinary system and accumulating
in a cavity surrounded by a fibrous capsule in the perinephric or
periureteral space. This rare clinical entity, the severity of
which varies from asymptomatic cases (small retroperitoneal
urinomas after extraperitoneal urine leakage) to causing acute
abdomen with signs of peritonitis in cases where the urine leakage
is intraperitoneal, may be caused by trauma, surgery, or urinary
tract obstruction (10).
Urolithiasis, retroperitoneal fibrosis and the presence of a large
intra-abdominal mass primarily located in the pelvis are key causes
of urinoma formation, which is not due to iatrogenic surgical
trauma (11,12). In the patient in the present study,
the pressure from the giant cervical leiomyoma on the ureters
resulted in impaired urine flow, causing non-traumatic rupture of
the renal parenchyma and the formation of a retroperitoneal urinoma
in the left kidney. The early diagnosis of the urinoma, usually
confirmed by a CT scan or MRI, and prompt, appropriate conservative
or surgical management depending on the case is critical for
avoiding complications, such as infection leading to the formation
of perinephric or periureteral abscesses and transient or permanent
renal damage (13). In the patient
in the present study, due to the small size of the urinoma and the
absence of acute symptoms, urologists did not recommend surgical
intervention for drainage. It was deemed appropriate to monitor the
lesion and leave the ureteral stents in place postoperatively to
address the dilatation of the pelvicalyceal system.
The imaging of large cervical leiomyomas of the
uterus is crucial for an accurate pre-operative diagnostic approach
to these tumors originating from the cervix, treatment planning and
minimization of surgical complications. Ultrasound, CT scan and MRI
play a crucial role in the management of patients with cervical
leiomyomas (14). Ultrasound is the
most frequently used imaging method. With both transabdominal and
transvaginal ultrasound, a well-defined hypoechoic mass can be
observed in the endocervix or outside the cervical canal, which
typically contains solid components, as well as areas of cystic
necrosis, internal vascularization and calcification. Ultrasound
findings compatible with the presence of mixed echogenic tumors
with central necrosis and irregular vascular distribution are
observed in ~20% of large cervical leiomyomas, which require
differential diagnosis from malignant cervical lesions (15). In cases with a strong suspicion of
malignancy in the cervix, a CT scan or MRI are performed for the
further imaging evaluation of the cervical mass. In an MRI, which
provides better visualization of the lateral and posterior pelvic
regions, leiomyomas appear as sharply demarcated areas of low to
intermediate signal intensity on both T1 and T2 sequences (16). Although an MRI cannot confirm the
diagnosis of malignant cervical lesions, compared to an ultrasound,
it has higher specificity and positive predictive value (17). In the patient described herein, due
to the large size of the tumor, neither transvaginal nor
transabdominal ultrasound was diagnostic. An urgent CT scan was
performed, which established the diagnosis of cervical leiomyoma
and associated urinary tract lesions (hydronephrosis, urinoma). The
scheduled MRI was deemed necessary for better delineating the
specific imaging characteristics of the cervical mass and its
anatomical relationship with pelvic structures to optimize surgical
planning.
The presence of large pelvic masses, particularly in
the narrow pelvis minor area, such as in the present case, can
severely distort normal, expected anatomy. The use of pre-operative
imaging modalities in order to accurately explore and map out these
distortions can significantly assist intra-operatively, as the
surgeon is better prepared to work in the distorted surgical site,
is better aware of the size, location and distance of the tumor
relative to other organs, and is thus less likely to cause injury
and other complications (18). While
an ultrasound is a readily available and dynamic test, its
subjective nature and inability to adequately visualize large
tumors, such as in the present case, render it of limited value in
the context of pre-operative preparation for advanced cases
(18). Tomographic methods, such as
CT scans and particularly, MRI, constitute the gold standard for
visualizing the entire pelvis and for facilitating identification
of the tumor, its location, size and association with healthy
tissue; these methods are therefore necessary to better plan the
surgery and reduce the risk of complications (19). This was also the case for the patient
described herein, where both techniques were performed and MRI was
primarily used to plan the surgery. However, the possibility
remains that despite careful preparation and planning,
complications may occur regardless, in which case the surgeon needs
to be able to effectively address them. This was true in the
present case as well, where despite careful preparation and
planning, a rupture of the urinary bladder occurred during surgical
maneuvering due to the size of the primary tumor and the presence
of multiple adhesions in the pelvic cavity; however, it was
promptly and effectively addressed and repaired without long term
effects on the patient's health and quality of life.
The surgical management of giant cervical leiomyomas
of the uterus is challenging and is largely dependent upon the
condition and wishes of the patient. With the primary complaint
among most gynecological patients being the provision of lacking
information regarding their surgery and the lack of opportunities
to influence the selection of their treatment; thorough
consultation with the gynecological surgery team regarding the
underlying condition, its severity, the available treatment options
and the advantages and disadvantages of each one is of paramount
importance (20). It is vital that
the surgical team presents and analyzes all available treatment
options, even those that go against their recommendations and
clarifies what precise intervention they propose in addition to the
reason or indication why it is proposed over the other alternatives
(20). The matter of surgical route
should also be discussed, along with the advantages and
disadvantages of each route, in addition to issues of treatment
availability at the center of care (20). Finally, this information should
ideally be discussed well in advance of the arranged date of
surgery at the outpatient office, in order to ensure adequate time
and a stress-free environment for the patient to participate in the
decision-making process and to provide informed consent to a
mutually agreeable treatment option (20).
Hysterectomy or myomectomy, depending on the age and
desire of the patient for future pregnancy, are recommended as the
main therapeutic options for patients with large cervical
leiomyomas (7). Ideally, minimally
invasive surgery should be preferred over laparotomy, since it is
associated with reduced patient morbidity rates. However, in the
current case, the presence of large tumors combined with the
presence of severe peritoneal adhesions renders the laparoscopic
route extremely challenging and thus laparotomy may be preferred
(21). In patients who are an
increased surgical risk, where the selection of a minimally
invasive approach is more strongly recommended, robotic surgery may
be selected, as it combines the efficacy of laparotomy with the
reduced morbidity of laparoscopy (22); however, this option is highly
dependent upon availability. Abdominal cervicectomy for the
management of a giant cervical leiomyoma is extremely difficult and
may be attempted in cases where the goal is to preserve the
fertility of the patient (15).
Since the patient in the present case report did not wish to pursue
such an option, this method was rejected; however, it may be a
viable option for younger patients with an incomplete family plan
(23).
A treatment alternative, apart from surgical
excision is arterial embolization. Most commonly performed for
leiomyomas in the uterine body, uterine artery embolization
provides a minimally invasive treatment option where blood supply
to the leiomyoma is blocked, resulting in tumor shrinkage and
symptom improvement, with the preservation of the uterus. While
this methodology is not commonly applied to cervical leiomyomas,
due to the complexity and variation of cervical vessels,
specialized centers have managed to apply this technique to a
limited amount of patients with favorable outcomes, both in terms
of surgical morbidity and an improvement in quality of life
(24). Recently, an interesting
variation of this technique pertaining to a case of successful
treatment of a large symptomatic cervical leiomyoma with bilateral
ovarian artery embolization without embolization of the uterine
artery was described in the literature (25). Although it pertains to a single
patient case, under conditions where the potential risks regarding
fertility and hormonal function are managed, this method could be
considered a viable alternative in the treatment of symptomatic
cervical leiomyomas, protecting patients from a potentially
complicated and extremely hemorrhagic surgical procedure (25). Definitive conclusions regarding the
optimal treatment option for cervical leiomyomas are difficult to
make, given their rarity compared to other leiomyoma types.
However, in the most recent meta-analysis on the topic by Ferrari
et al (26) the vast majority
of the patients (88%) were treated with surgery, compared to only
10% by arterial embolization, indicating a clear preference towards
the former. Furthermore, embolization treatments were successful
only in 55.5% of cases, indicating lower efficacy than traditional
surgery; however, surgery was associated with 5.6% total
complication rate, indicating relatively lower safety (26). The authors of that study ultimately
stress the challenging nature of cervical myoma treatment
regardless of the approach used and recommend that these procedures
are only undertaken by experienced teams, with embolization
treatments being promising, but with limited available data
(26).
The increased risk of intraoperative bleeding and
the potential for inadvertent trauma to adjacent organs compressed
by the giant tumor (bladder, ureters and rectum) render the
surgical management of these patients extremely difficult (7). In the patient in the present study, who
did not wish to pursue future pregnancy, abdominal total
hysterectomy with bilateral salpingectomy and oophorectomy was
selected. The surgery presented significant difficulties. Multiple
and firm adhesions between the cervical leiomyoma and the bladder
and anterior abdominal wall, due to previous cesarean sections,
combined with the displacement of these structures by the massive
size of the tumor, made mobilization of the uterus and cervical
leiomyoma in the surgical field challenging (Fig. 4). This led to significant
intraoperative bleeding, a traumatic rupture of the bladder wall,
and an increased risk of ureteral injury. To reduce the risk of
intraoperative bleeding, the use of the electrothermal bipolar
vessel sealing device (LigaSure™) was considered
crucial. The bladder wall rupture was sutured, and the integrity of
the ureters was checked. Pre-operative cystoscopy and bilateral
ureteral stent placement allowed intraoperative tracing of the
ureters and prevented inadvertent injury (7). Additionally, proper and complete
preoperative planning, well-organized operating room settings, and
the sufficient experience and skill of the surgical team with a
thorough knowledge of pelvic anatomy, which is often distorted by
the giant cervical leiomyoma, are essential for the successful
outcome of the surgical procedure (27).
In conclusion, giant cervical uterine fibroids are
extremely rare. Transient, non-traumatic or non-obstructive lesions
of the ureters and kidneys related to the pressure exerted by the
giant cervical fibroid may occur. The diagnostic and therapeutic
approach to these fibroids is challenging. An additional challenge,
which would make the management of our patient even more difficult,
would be her desire to preserve her uterus and fertility. However,
regardless of the decision to perform a hysterectomy or myomectomy,
managing these patients remains difficult even for experienced
gynecologists and depends largely on the individual circumstances
of the patient, the organization of the medical center, and the
coordination of the surgical team.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
All authors (AT, ET, EX, AZ and IT) participated in
the preparation of the manuscript. AT and ET participated in the
conception and design of the study, data acquisition, analysis and
interpretation, in the literature search and in the drafting of the
manuscript. EX and AZ participated in the study design, critical
analysis and interpretation of patient and literature data,
literature search, drafting of the manuscript and critical
reviewing and revision of the manuscript. IT was involved in the
conception and design of the study, in administrative support, in
the provision of study materials (such as blood tests, imaging) or
patient data, in patient care, in data collection and analysis, and
in manuscript writing. All authors confirm the authenticity of all
the raw data. All authors have read and approved the final
manuscript.
Ethics approval and consent to
participate
The present case report was carried out in
accordance with the Declaration of Helsinki. The patient provided
her written consent for the description of the present case
report.
Patient consent for publication
The patient provided her written consent for the
publication of the present case report.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Stewart EA, Laughlin-Tommaso SK, Catherino
WH, Lalitkumar S, Gupta D and Vollenhoven B: Uterine fibroids. Nat
Rev Dis Primers. 2(16043)2016.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ramaiyer MS, Saad E, Kurt I and Borahay
MA: Genetic mechanisms driving uterine leiomyoma pathobiology,
epidemiology, and treatment. Genes (Basel). 15(558)2024.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Ciavattini A, Di Giuseppe J, Stortoni P,
Montik N, Giannubilo SR, Litta P, Islam MS, Tranquilli AL, Reis FM
and Ciarmela P: Uterine fibroids: Pathogenesis and interactions
with endometrium and endomyometrial junction. Obstet Gynecol Int.
2013(173184)2013.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Cha PC, Takahashi A, Hosono N, Low SK,
Kamatani N, Kubo M and Nakamura Y: A genome-wide association study
identifies three loci associated with susceptibility to uterine
fibroids. Nat Genet. 43:447–450. 2011.PubMed/NCBI View
Article : Google Scholar
|
|
5
|
Thanasa A, Thanasa E, Kamaretsos E,
Grapsidi V, Xydias E, Ziogas A, Gerokostas EE, Antoniou IR,
Paraoulakis I and Thanasas I: Surgical treatment of a very rare
case of a huge intraligamental leiomyoma of the uterus: A case
report and mini-review of the literature. Med Int (Lond).
4(2)2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Thanasa E, Thanasa A, Kamaretsos E,
Paraoulakis I, Ziogas A, Kontogeorgis G, Grapsidi V, Gerokostas EE,
Kontochristos V and Thanasas I: Large cervical leiomyoma of the
uterus: A rare cause of chronic pelvic pain associated with
obstructive uropathy and renal dysfunction: A case report. Cureus.
15(e33387)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Mujalda A, Kaur T, Jindal D, Sindhu V,
Jindal P and Mujalda J: Giant cervical fibroid: A surgical
challenge. Cureus. 15(e39602)2023.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Peng K, Jiang LY, Teng SW and Wang PH:
Degenerative leiomyoma of the cervix: Atypical clinical
presentation and an unusual finding. Taiwan J Obstet Gynecol.
55:293–295. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Munro MG, Critchley HOD and Fraser IS:
FIGO Menstrual Disorders Working Group. The FIGO classification of
causes of abnormal uterine bleeding in the reproductive years.
Fertil Steril. 95:2204–2208, 2208.e1-e3. 2011.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Anjum T, Ikram M, Abdulhameed R, Khan A
and Mirza ZR: Urinoma: A rare but potential differential of acute
abdomen. Cureus. 16(e67368)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Hamard M, Amzalag G, Becker CD and Poletti
PA: Asymptomatic urolithiasis complicated by nephrocutaneous
fistula. J Clin Imaging Sci. 7(9)2017.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Sato H, Kurumisawa S, Saito T and Kawahito
K: Spontaneous ureteral rupture caused by iliac aneurysm: A case
report. Surg Case Rep. 4(146)2018.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Kajić M, Boras M, Tipurić M, Šutalo N,
Bevanda D and Mišković J: Spontaneous urinoma surgeon's
pitfall-case report. Psychiatr Danub. 33 (Suppl 13):S327–S329.
2021.PubMed/NCBI
|
|
14
|
Gupta A, Gupta P and Manaktala U: Varied
clinical presentations, the role of magnetic resonance imaging in
the diagnosis, and successful management of cervical leiomyomas: A
case-series and review of literature. Cureus.
10(e2653)2018.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Wong J, Tan GHC, Nadarajah R and Teo M:
Novel management of a giant cervical myoma in a premenopausal
patient. BMJ Case Rep. 2017(bcr2017221408)2017.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Okamoto Y, Tanaka YO, Nishida M, Tsunoda
H, Yoshikawa H and Itai Y: MR imaging of the uterine cervix:
Imaging-pathologic correlation. Radiographics. 23:425–445, 534-535.
2003.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Goto A, Takeuchi S, Sugimura K and Maruo
T: Usefulness of Gd-DTPA contrast-enhanced dynamic MRI and serum
determination of LDH and its isozymes in the differential diagnosis
of leiomyosarcoma from degenerated leiomyoma of the uterus. Int J
Gynecol Cancer. 12:354–361. 2002.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Stadtmauer L and Shah A: Gynecologic
surgery: Preoperative assessment with ultrasound. Clin Obstet
Gynecol. 60:82–92. 2017.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Acton J: Preoperative surgical planning
MRI for fibroids: What the surgeon needs to know and what to
report. J Med Imaging Radiat Oncol: Dec 27, 2024 (Epub ahead of
print).
|
|
20
|
Entwistle V, Williams B, Skea Z, MacLennan
G and Bhattacharya S: Which surgical decisions should patients
participate in and how? Reflections on women's recollections of
discussions about variants of hysterectomy. Soc Sci Med.
62:499–509. 2006.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Rajaretnam N, Okoye E and Burns B:
Laparotomy. In: StatPearls. StatPearls Publishing, Treasure Island,
FL, 2025.
|
|
22
|
Tsakos E, Xydias EM, Ziogas AC, Sorrentino
F, Nappi L, Vlachos N and Daniilidis A: Multi-port robotic-assisted
laparoscopic myomectomy: A systematic review and meta-analysis of
comparative clinical and fertility outcomes. J Clin Med.
12(4134)2023.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Gari A and Alrajhi BF: Abdominal
trachelectomy in a case of cervical myoma as a fertility sparing
surgery. J Surg Case Rep. 2022(rjac557)2022.PubMed/NCBI View Article : Google Scholar
|
|
24
|
de Bruijn AM, Adriaansens SJH, Smink M,
Venmans A, Hehenkamp WJK, Smeets AJ, Lopez A, Huirne JAF and Lohle
PNM: Uterine artery embolization in women with symptomatic cervical
leiomyomata: Efficacy and safety. Cardiovasc Intervent Radiol.
42:371–380. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Denton WD and Ozen M: Bilateral ovarian
artery embolization for a symptomatic large cervical fibroid.
Radiol Case Rep. 19:6126–6130. 2024.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Ferrari F, Forte S, Valenti G, Ardighieri
L, Barra F, Esposito V, Sartori E and Odicino F: Current treatment
options for cervical leiomyomas: A systematic review of literature.
Medicina (Kaunas). 57(92)2021.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Soleymani Majd H, Ferrari F, Gubbala K,
Campanile RG and Tozzi R: Latest developments and techniques in
gynaecological oncology surgery. Curr Opin Obstet Gynecol.
27:291–296. 2015.PubMed/NCBI View Article : Google Scholar
|