Introduction
Aneurysmal subarachnoid hemorrhage (SAH) constitutes
a devastating and life-threatening neurosurgical emergency with an
estimated global incidence of 9.1 per 100,000 individuals per year
(1,2). Due to its catastrophic short-term
complications, SAH remains a major cause of morbidity and mortality
worldwide, even though novel diagnostic and treatment techniques
have been developed over the past decades. Indeed, during the early
stages of aneurysmal SAH, there is a high risk of re-bleeding,
hydrocephalus, intracerebral hematoma, generalized cerebral edema
and vasospasm, while long-term complications include delayed
cerebral ischemia (DCI) (3-5).
The severity of the clinical presentation upon
admission, re-bleeding, the timing of the surgery and the type of
treatment are predictors of neurological outcomes and SAH-related
disability (6,7). Furthermore, patients with higher Hunt
and Hess grades (grades 4 and 5) upon admission, particularly the
elderly, are more likely to have poor clinical outcomes (8).
Upon the diagnosis of a ruptured intracranial
aneurysm, the main goal is to secure the aneurysm as soon as
possible to prevent re-bleeding. Before the 1990s, microsurgical
clipping was the only available treatment option for ruptured
intracranial aneurysms and while it still confers satisfactory
long-term results regarding re-operation rates, it is characterized
by high peri-operative complications and long periods of
hospitalization (4,5,9,10). On the other hand, the introduction of
endovascular treatment has led to lower peri-interventional
complication rates; however, this is associated with a higher rate
of incomplete occlusion and in-hospital case fatalities (11,12).
The timing of the surgery plays a crucial role
concerning the risk of re-bleeding and mortality rates,
particularly in patients with a good clinical condition upon
admission (13-16).
Over a number of years, there has been a debate as regards the most
suitable timing of surgery (17,18). The
early clipping of the cerebral aneurysm may permit for the secure
preface of hypertensive management prevented at the development
and/or treatment of DCI (14). On
the other hand, delayed surgical management may decrease the
morbidity and mortality of the microsurgical intervention due to
improvements in surgical conditions and the general condition of
individual patients, mainly in those with higher Hunt and Hess
grades (grades 4 and 5) upon admission (13).
The present retrospective study aimed to investigate
the association between the timing of treatment and the outcomes of
patients who underwent the clipping of ruptured intracranial
aneurysms. The present study and also aimed to provide contemporary
data for a more balanced approach when assessing the optimal
treatment strategy for a given aneurysm, microsurgical vs.
endovascular, when both options are available.
Materials and methods
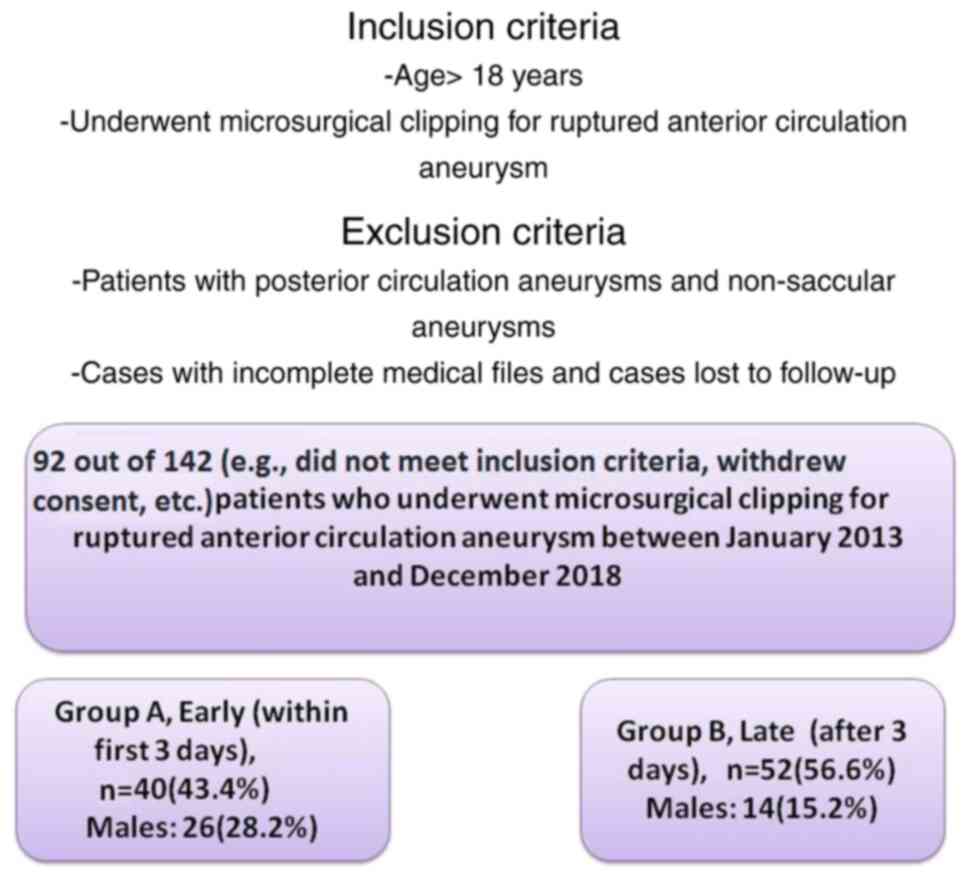
Patient population and aneurysm characteristics. A
retrospective analysis of 92 of 142 consecutive patients who were
diagnosed with anterior circulation ruptured aneurysms and treated
only by microsurgical clipping was conducted between January, 2013
and December, 2018 (AHEPA University Hospital, Aristotle University
School of Medicine, Thessaloniki, Greece).
The study protocol was approved by the Ethics
Committee of the hospital-(AHEPA University Hospital, Aristotle
School of Medicine Thessaloniki, Greece; Ref. no. 1085-2023). In
compliance with the current legislation, the National Data
Protection Authority was notified on its conduction (Ref. no.
985-2024). The study was conducted in accordance with the ethical
standards laid down in the Declaration of Helsinki 1964 and its
later amendments. Written informed consent was obtained from all
included patients or their next-of-kin prior to surgery. All
patients were >18 years of age.
Patients with posterior circulation aneurysms and
non-saccular aneurysms were excluded from the study. In the final
pool, 92 patients were included, and these patients were divided
into two groups. Data collection was performed, and the data were
reviewed and analyzed by two physicians (GF and DP) based on the
following inclusion criteria: Patients aged >18 years who
underwent microsurgical clipping for ruptured anterior circulation
aneurysm between 2013 and 2018. Cases with incomplete medical files
and cases lost to follow-up were excluded (Fig. 1).
Demographic data including age, sex, comorbidities
and post-operative outcomes were collected prospectively. Baseline
characteristics included age, sex, risk factors, aneurysm size and
location, clinical presentation upon admission, Fisher grade, and
the timing of surgery (Table I).
Risk factors for aneurysm formation and rupture, including
hypertension, diabetes mellitus, hypercholesterolemia and smoking
were documented and the data are also presented in Table I. The clinical presentation of the
patient upon admission was assessed according to Hunt and Hess
grading scale (Table I). Clinical
status upon admission was dichotomized as good (grade ≤2) and
severe (grade ≥3). At the emergency department, all patients
underwent urgent Computed Tomography (CT) angiography. Aneurysm
location, size, and extent of SAH according to Fisher grading scale
were documented and the presence of multiple aneurysms was also
investigated (Table I). The timing
of the surgery was dichotomized as early (within the first 3 days
after SAH) and late (after ≥4 days).
 | Table IBaseline demographic characteristics
of the patients. |
Table I
Baseline demographic characteristics
of the patients.
| Parameters | All patients, n=92
(100%) | Group A, early
(within first 3 days), n=40 (43.4%) | Group B, late (after
3 days), n=52 (56.6%) | P-value |
|---|
| Age, mean ± SD
(years) | 54.6±11.5 | 52.2±13.2 | 56.5±9.7 | 0.197 |
| Sex, n (%) | | | | 0.150 |
|
Male | 40 (43.4) | 26(65) | 14(35) | |
|
Female | 52 (56.6) | 14 (26.9) | 38 (73.1) | |
| Alcohol consumption,
n (%) | | | | 0.060 |
|
Yes | 20 (21.7) | 5 (5.4) | 15 (16.3) | |
|
No | 72 (78.3) | 35 (38.8) | 37 (40.5) | |
| Diabetes, n (%) | | | | 0.851 |
|
Yes | 2 (2.1) | 1 (1.0) | 1 (1.0) | |
|
No | 90 (97.9) | 39 (42.5) | 51 (55.4) | |
| Hypertension, n
(%) | | | | 0.855 |
|
Yes | 47(51) | 20 (21.7) | 27 (29.3) | |
|
No | 45(49) | 20 (21.7) | 25 (27.3) | |
| Smoking status, n
(%) | | | | 0.195 |
|
Yes | 39 (42.3) | 20 (21.7) | 19 (20.6) | |
|
No | 53 (57.7) | 20 (21.7) | 33(36) | |
| Aneurysm size, n
(%) | | | | 0.015 |
|
Small (<5
mm) | 27 (29.3) | 17 (18.4) | 10 (10.8) | |
|
Medium (5-15
mm) | 60 (65.2) | 19 (20.6) | 41 (44.5) | |
|
Large
(>15-25 mm) | 4 (4.3) | 3 (3.2) | 1 (1.0) | |
|
Giant
(>25 mm) | 1 (1.0) | 1 (1.0) | 0 (0) | |
|
Complicationsa, n (%) | | | | |
|
No
complication | 43 (46.7) | 21 (22.8) | 22 (23.9) | 0.331 |
|
Hydrocephalus | 27 (29.3) | 9 (9.7) | 18 (19.5) | 0.206 |
|
Post-operative
hemiplegia | 7 (7.6) | 3 (3.2) | 4 (4.3) | 0.972 |
|
Pneumonia | 6 (6.5) | 0 (0) | 6 (6.5) | 0.026 |
|
Diffuse
edema/DC | 15 (16.3) | 10 (10.8) | 5 (5.4) | 0.048 |
|
Multiorgan
failure | 4 (4.3) | 2 (2.1) | 2 (2.1) | 0.788 |
|
Re-bleeding | 10 (10.8) | 5 (5.4) | 5 (5.4) | 0.659 |
|
Locationa, n (%) | | | | |
|
Acom | 49 (53.2) | 20 (21.7) | 29 (31.5) | 0.582 |
|
ICA/Pcom | 17 (18.4) | 5 (5.4) | 12 (13.0) | 0.195 |
|
MCA | 22 (23.9) | 13 (14.1) | 9 (9.7) | 0.090 |
|
ICA-anterior
choroidal | 4 (4.3) | 1 (1.0) | 3 (3.2) | 0.446 |
|
Multiple
aneurysm | 11 (11.9) | 6 (6.5) | 5 (5.4) | 0.446 |
| Fisher grading
scale, n (%) | | | | 0.672 |
|
1 | 0 (0) | 0 (0) | 0 (0) | |
|
2 | 29 (31.5) | 12 (13.0) | 17 (18.4) | |
|
3 | 33 (35.8) | 13 (14.1) | 20 (21.7) | |
|
4 | 30 (32.6) | 15 (16.3) | 15 (16.3) | |
| Hunt and Hess
grading scale, n (%) | | | | 0.002 |
|
0 | 0 (0) | 0 (0) | 0 (0) | |
|
1 | 31 (33.6) | 20 (21.7) | 11 (11.9) | |
|
2 | 23(25) | 4 (4.3) | 19 (20.6) | |
|
3 | 6 (6.5) | 0 (0) | 6 (6.5) | |
|
4 | 26 (28.2) | 13 (14.1) | 13 (14.1) | |
|
5 | 6 (6.5) | 3 (3.2) | 3 (3.2) | |
| Modified Rankin
rading scale, n (%) | | | | |
|
Good outcome
≥2 | 61 (66.3) | 24 (26.0) | 37 (40.7) | |
|
Poor outcome
<2 | 31 (33.6) | 16 (17.3) | 15 (16.3) | - |
| Mortality, n
(%) | | | | 0.011 |
|
Yes | 15 (16.2) | 11 (11.9) | 4 (4.3) | |
|
No | 77 (83.8) | 29 (31.5) | 48 (52.3) | |
Clinical data
The patients were divided into two groups, namely
group A, which included patients who underwent microsurgical
clipping for ruptured anterior circulation aneurysm in the early
stages (within the first 3 days of aneurysm rupture occurrence),
and group B, which included those who were operated on in the late
stages (after 3 days of aneurysm rupture occurrence).
Perioperative treatment and surgical
technique
During hospitalization, all patients received the
same medical treatment protocol [nimodipine, 60 mg (as 2x30 mg
capsules) every 4 h for 21 consecutive days, antihypertensives to
control blood pressure, pain relievers (acetaminophen, 500 mg every
8 h for headache) and antiseizure medications (levetiracefan, 500
mg every 12 h]. Standard pterional craniotomy was used for the
clipping of anterior circulation aneurysms. In some cases,
temporary clip application was performed. A small number of
patients underwent decompressive craniectomy due to diffuse
cerebral edema and massive intracerebral hemorrhage and some of
them underwent ventriculoperitoneal shunt placement for
hydrocephalus. Following surgery, patients were moved to the
intensive care unit.
Follow-up and clinical outcomes
The presence of pre-operative re-bleeding,
hydrocephalus and diffuse cerebral edema was assessed. The modified
Rankin scale (mRS) was used to assess clinical outcomes. According
to the mRS, patients were categorized as mRS ≥2 (good outcome) and
mRS <2 (poor outcome). The mRS is a severity-of-disease
classification system that estimates the level of morbidity during
the everyday actions of participants who have suffered a stroke or
have other diseases leading to neurological disability. A numerical
score from 0 to 6 was assigned based on several factors, with
higher scores indicating a more severe situation and a greater risk
of mortality (19). Post-operative
outcomes were evaluated no less than 12 months following surgical
management.
Statistical analysis
Statistical analyses were carried out using the
Statistical Package for the Social Sciences (SPSS 11; SPSS, Inc.).
The normality of the distribution of variables was evaluated using
the Shapiro-Wilk test. Categorical variables were compared between
groups using Fisher's exact test. The continuous records also were
assessed using the Mann-Whitney U test. Receiver operating
characteristic (ROC) analysis was applied to expose the causes that
are related to patients who were diagnosed with anterior
circulation ruptured aneurysms and treated only by microsurgical
clipping and affect the outcomes of those patients. A P-value
<0.05 was considered to indicate a statistically significant
difference.
Results
Patient and aneurysm
characteristics
The baseline characteristics of patients and
aneurysms are outlined in Table I.
The present study included 92 patients, admitted to the emergency
department with a high clinical suspicion of SAH, which was
confirmed radiologically, between January, 2013 and December, 2018.
A total of 92 anterior circulation ruptured aneurysms were
identified following computed tomography angiography. All patients
underwent microsurgical clipping of the aneurysm.
The age of the patients ranged from 26 to 78 years,
with a mean age of 54.6 years. In total, 52 patients were female
(56.6%) and 40 patients were male (43.4%). Risk factors associated
with a high incidence of rupture included hypertension in 47
(51.0%) patients, cigarette smoking in 39 (42.3%) patients, alcohol
consumption in 20 (21.7%) patients and diabetes mellitus in 2
(2.1%) patients (Table I).
The most common rupture site was the anterior
communicating artery in 49 (53.2%) cases followed by ruptured
middle cerebral artery aneurysms in 22 (23.9%) cases. In total, 11
cases (11.9%) had more than one aneurysm. As regards the aneurysm
diameter, the majority of them were small [0-4.9 mm; 27 patients
(29.3%)] and medium [5-14.9 mm; 60 patients (65.2%)] in size
(Table I).
Upon admission, the majority of cases (60 patients,
65%) presented with favorable Hunt and Hess grading scale scores
(grades 1-3), while the remaining 32 (35%) patients were
categorized as grades 4 and 5. A total of 29 (31.5%) patients had
Fisher grade 2 at the initial presentation, 33 (35.8%) patients had
Fisher grade 3, and the remaining 30 patients had grade 4 (32.6%)
(Table I). In terms of the timing of
surgery, 40 patients underwent microsurgical clipping during the
first 3 days of hospitalization (43.4%) and the remaining 52
(56.6%) patients were operated on after 3 days (Table I).
Association between factors and
clinical outcomes
Univariate analysis revealed that there was a
statistically significant difference in the no complications,
post-operative hemiplegia, diffuse edema/decompressive craniectomy,
re-bleeding, Fisher grading scale, Hunt and Hess grading scale and
mortality between the participants who underwent microsurgical
clipping during the first 3 days of hospitalization (group A) and
those that underwent surgery after 3 days (group B) (P<0.05,
Table II).
 | Table IIUnivariate analysis for good outcomes
(≥2 mRS). |
Table II
Univariate analysis for good outcomes
(≥2 mRS).
| Parameters | Good outcomes (≥2
mRS), n=61 (66.3%) | Poor outcomes
(<2 mRS), n=31 (33.7%) | P-value |
|---|
| Groups, timing of
surgery | 8.2±6.0 | 6.5±5.8 | 0.202 |
| Age, mean ± SD
(years) | 54.4±12.0 | 55.1±10.5 | 0.934 |
| Sex, n (%) | | | 0.117 |
|
Male | 23 (57.5) | 17 (42.5) | |
|
Female | 38(73) | 14(27) | |
| Alcohol
consumption, n (%) | | | 0.500 |
|
Yes | 12 (13.0) | 8 (8.6) | |
|
No | 49 (53.2) | 23(25) | |
| Diabetes, n
(%) | | | 0.622 |
|
Yes | 1 (1.0) | 1 (1.0) | |
|
No | 60 (65.2) | 30 (32.6) | |
| Hypertension, n
(%) | | | 0.943 |
|
Yes | 31 (33.6) | 16 (17.3) | |
|
No | 30 (32.6) | 15 (16.3) | |
| Smoking status, n
(%) | | | 0.407 |
|
Yes | 24 (26.0) | 15 (16.3) | |
|
No | 37 (40.2) | 16 (17.3) | |
| Aneurysm size, n
(%) | | | 0.234 |
|
Small (<5
mm) | 21 (22.8) | 6 (6.5) | |
|
Medium (5-15
mm) | 38 (41.3) | 22 (23.9) | |
|
Large
(>15-25 mm) | 2 (2.1) | 2 (2.1) | |
|
Giant
(>25 mm) | 0 (0) | 1 (1.0) | |
|
Complicationsa, n (%) | | | |
|
No
complication | 42 (45.6) | 1 (1.0) | 0.001 |
|
Hydrocephalus | 14 (15.2) | 13 (14.1) | 0.059 |
|
Post-operative
hemiplegia | 2 (2.1) | 5 (5.4) | 0.028 |
|
Pneumonia | 2 (2.1) | 4 (4.3) | 0.077 |
|
Diffuse
edema/DC | 3 (3.2) | 12 (13.0) | 0.001 |
|
Multiorgan
failure | 1 (1.0) | 3 (3.2) | 0.074 |
|
Re-bleeding | 3 (3.2) | 7 (7.6) | 0.010 |
|
Locationa, n (%) | - | - | - |
|
Acom | 34 (36.9) | 15 (16.3) | 0.504 |
|
ICA/Pcom | 12 (13.0) | 5 (5.4) | 0.679 |
|
MCA | 12 (13.0) | 10 (10.8) | 0.181 |
|
ICA-anterior
choroidal | 4 (4.3) | 0 (0) | 0.145 |
|
Multiple
aneurysm | 4 (4.3) | 7 (7.6) | 0.127 |
| Fisher grading
scale, n (%) | | | 0.001 |
|
1 | 0 (0) | 0 (0) | |
|
2 | 29 (31.5) | 0 (0) | |
|
3 | 23(25) | 10 (10.8) | |
|
4 | 9 (9.7) | 21 (22.8) | |
| Hunt and Hess
grading scale, n (%) | | | 0.001 |
|
0 | 0 (0) | 0 (0) | |
|
1 | 30 (32.6) | 1 (1.0) | |
|
2 | 17 (18.4) | 6 (6.5) | |
|
3 | 3 (3.2) | 3 (3.2) | |
|
4 | 9 (9.7) | 17 (18.4) | |
|
5 | 2 (2.1) | 4 (4.3) | |
| Mortality, n
(%) | | | 0.001 |
|
Yes | 0 (0) | 15 (16.3) | |
|
No | 61 | 16 (17.3) | |
Multivariate analysis (Table III) revealed that no complications,
post-operative hemiplegia and mortality were all independent
factors associated with good outcomes (≥2 mRS) (P<0.05 for all
three parameters).
 | Table IIIMultivariate analysis and ROC
analysis of good outcomes (≥2 mRS). |
Table III
Multivariate analysis and ROC
analysis of good outcomes (≥2 mRS).
| A, Multivariate
analysis |
|---|
| | | 95% CI for
Exp(B) |
|---|
| Parameter | P-value | Exp(B) | Lower | Upper |
|---|
| No
complication | 0.005 | 0.300 | 0.086 | 0.482 |
| Post-operative
hemiplegia | 0.007 | -0.210 | -0.647 | -0.104 |
| Diffuse
edema/DC | 0.183 | -0.126 | -0.399 | 0.077 |
| Re-bleeding | 0.757 | 0.025 | -0.209 | 0.286 |
| Fisher grading
scale | 0.099 | -0.224 | -0.289 | 0.025 |
| Hunt and Hess
grading scale | 0.356 | 0.137 | -0.054 | 0.149 |
| Mortality | 0.000 | -0.422 | -0.766 | -0.321 |
| B, ROC
analysis |
| Parameter | P-value | Area | Std. error | CI (95%)
lower-upper |
| No
complication | 0.000 | 0.828 | 0.043 | 0.744-0.912 |
| Post-operative
hemiplegia | 0.316 | 0.564 | 0.066 | 0.436-0.693 |
| Mortality | 0.000 | 0.742 | 0.062 | 0.621-0.863 |
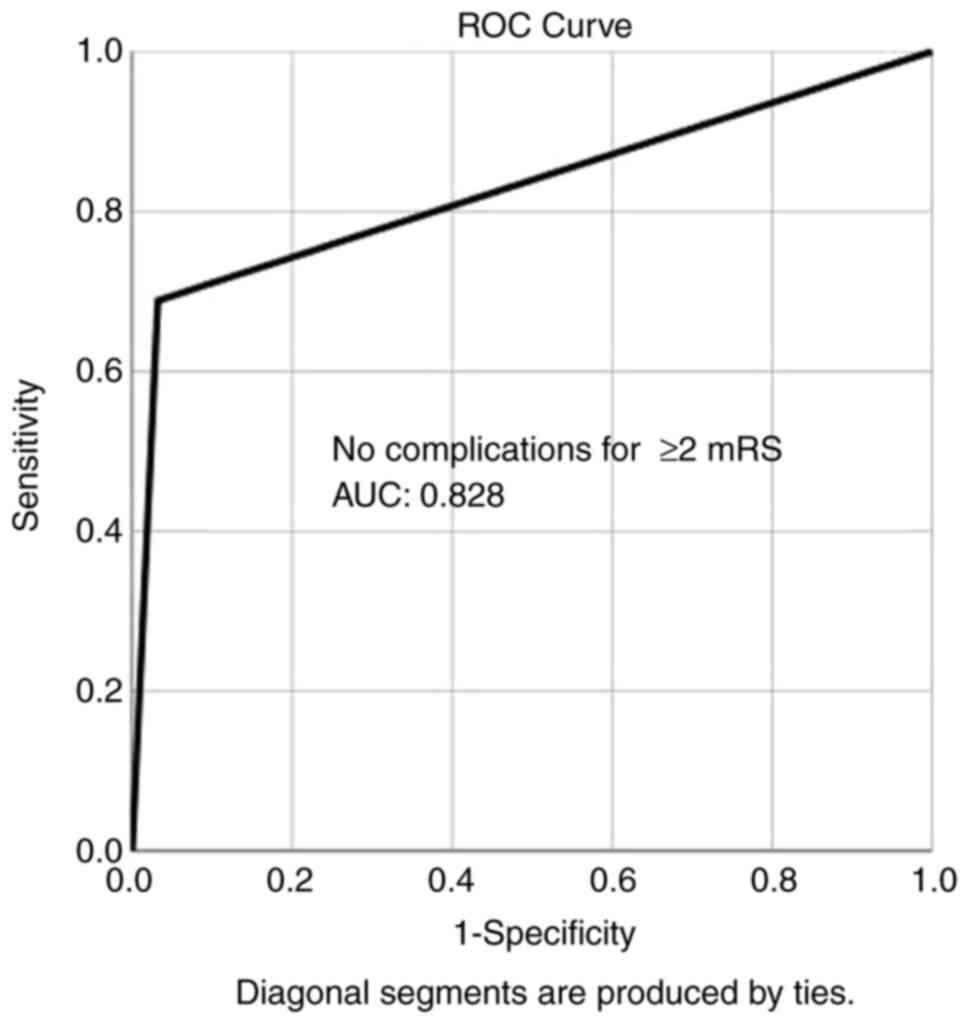
Overall, ROC analysis demonstrated that no
complications exhibited the optimal performance to predict good
outcome (≥2 mRS), as evaluated by an area under the curve standard
error [AUC (SE)] of [0.828 (0.043) and (P=0.000)] (Table III and Fig. 2). In addition, ROC analysis
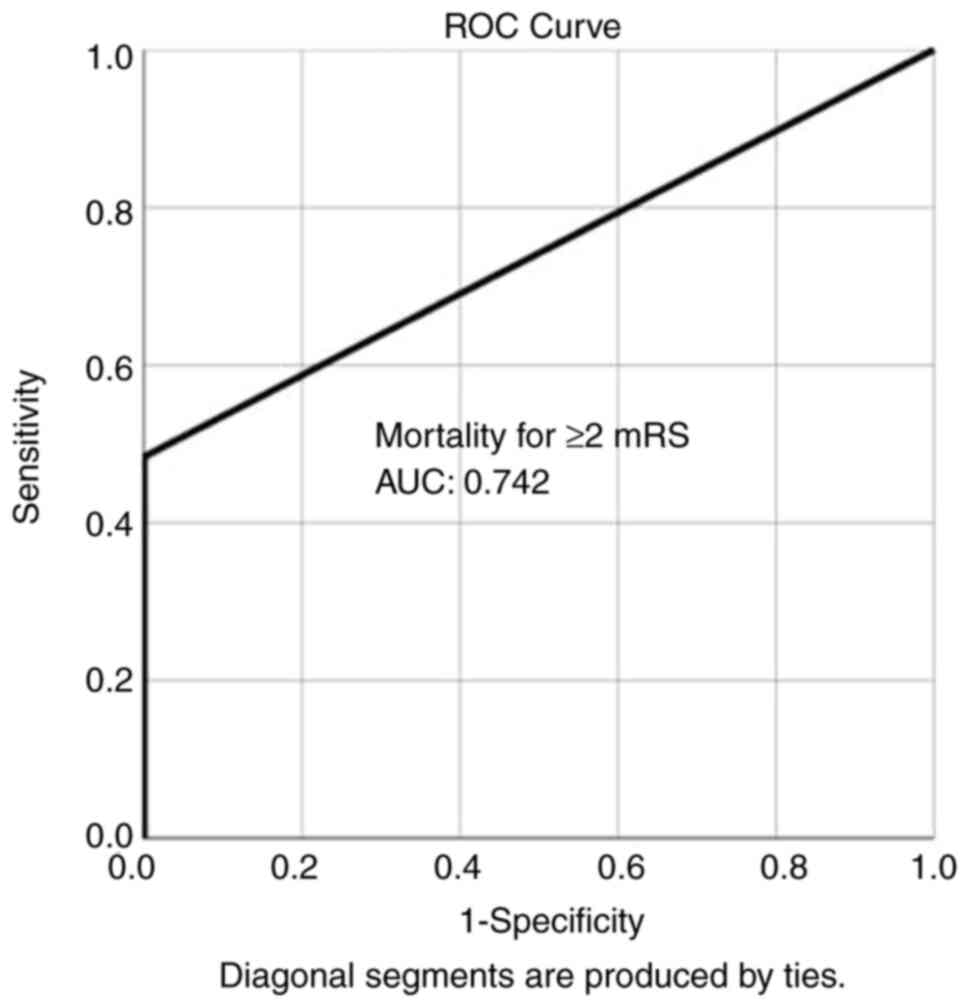
demonstrated that, among the variables, mortality was lower in
group B compared with group A, indicating the superiority of group
B compared with group A, as evaluated by an AUC (SE) of 0.742
(0.062) and P=0.000 (Table III and
Fig. 3).
Discussion
The results of the present study demonstrated that
the outcomes of patients who underwent microsurgical clipping for
ruptured anterior circulation aneurysms ≥3 days after admission or
rupture occurrence, exhibited favorable outcomes compared to
patients operated on during the first 2 days of occurrence. The
good clinical condition concerning SAH-related complications (no
complications); the development of post-operative hemiplegia
related to DCI, and mortality were all independent factors
associated with good outcomes (≥2 mRS). In addition, even though
the majority of the cases (78.4%) were admitted with Fisher grading
scale 3 or 4, in the present study the mortality rate was 16.3%. On
the other hand, risk factors for aneurysm formation and rupture,
including hypertension, diabetes mellitus, hypercholesterolemia and
smoking were not statistically significant parameters reinforcing
the initial hypothesis that the timing of the surgery plays a role
in patient outcomes.
Early surgery, within the first 3 days, seems to be
associated with lower likelihood of a positive outcome, especially
in those patients in good clinical condition on admission [13]. For
this reason, most centers now intend to operate on an aneurysm
within two days of the SAH (20,21).
However, microsurgical management for aneurysmal SAH may be more
dangerous during this two-day interval, and thus treatment
management must comprise contemplations concerning the risk of
re-hemorrhage (20). In addition,
for these patients, who are only suitable for surgery three days
after SAH, it is significant to identify the most favorable timing
for aneurysm clipping occlusion, i.e. whether it should be until 14
days after SAH (22). In the present
study, surgical morbidity and mortality, between patients submitted
to early, intermediate, or late surgery, was statistically
significant, with patients who underwent surgical aneurysm repair
in an interval ≥3 days indicating a more favorable outcome.
On the other hand, there were studies that the
timing of surgery did not have a significant role in surgical
outcomes, apart from clinical condition on admission (15,23).
Additional subgroup analysis proposed a tendency that recommended
greater advantages with early intervention, which, in other words,
encouraged a policy of surgery as early as possible (23). In addition, based on these results,
it was recommended that clipping between five and ten days after
the event of aneurysmal rupture did not lead to a higher
possibility of DCI (22). Instead,
operating on the swollen and vulnerable brain tissue led to high
rates of perioperative complications (24). The present study demonstrated that
clinical outcomes were improved when aneurysm occlusion was
performed at a later stage after SAH after differences. It is
imperative to understand that patients were not randomized for the
timing of the surgery, and the unfavorable outcome in the group of
patients operated on in the early stages, was possibly associated
with the causes of the post-operative condition, such as a poor
clinical condition on admission, early re-hemorrhage, or early
worsening from other reasons. Notably, in the present study,
re-bleeding did not occur more often in patients operated on after
day 3, and this is a critical factor when deciding on patients'
management.
A previous study on endovascular management report
that the embolization of ruptured intracranial aneurysms can be
applied safely to patients who were admitted between
post-hemorrhage days 4 and 10, with no significant increase in
mortality, and regardless of a higher risk of vasospasm at the time
of treatment (25). In the present
study, the mortality rate was lower in those patients who were
operated on 3 days after aneurysm rupture occurrence.
The present study had several limitations, such as
that it was a retrospective study of medical records analysis and
was performed in a single center with a limited number of cases. In
addition, the neurological outcomes of patients with SAH is
dependent on the underlying initial pathology and the subsequent
vasospasm. Another limitation was the restrictions concerning the
lack of inclusion of patients presenting with a worse overall
clinical condition.
In conclusion, the present study revealed that the
outcomes of patients who underwent microsurgical clipping for
ruptured anterior circulation aneurysms ≥3 days after admission or
rupture occurrence, exhibited favorable outcomes compared to
patients operated on during the first 2 days of occurrence. The
good clinical condition concerning SAH-related complications (no
complications), the development of post-operative hemiplegia
related to DCI and mortality were all independent factors
associated with good outcomes. In addition, even though the
majority of the cases were admitted with Fisher grading scale
scores of 3 or 4, in the present study, the mortality rate was
16.3%. Although the endovascular treatment of anterior circulation
ruptured aneurysms, during the past years, has been the treatment
of choice following SAH, clipping may be considered a valid
alternative.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
GF and DP conceptualized the study. DP, GF, EK, KP,
IP and NF advised on patient care and medical treatment, and wrote
and prepared the draft of the manuscript. DP, GF, EK, KP, IP and NF
analyzed the patients' data and provided critical revisions. GF and
NF confirm the authenticity of all the raw data. All authors
contributed to manuscript revision and have read and approved the
final version of the manuscript.
Ethics approval and consent to
participate
The study protocol was approved by the Ethics
Committee of the hospital (AHEPA University Hospital Aristotle
School of Medicine, Thessaloniki, Greece) (Ref. no. 1085-2023). In
compliance with the current legislation, the National Data
Protection Authority was notified on its conduction (Ref. no.
985-2024). The study was conducted in accordance with the ethical
standards laid down in the 1964 Helsinki Declaration and its later
amendments. Informed consent was obtained from all individual
participants, prior to their inclusion in the study. All details
that may disclose the identity of the subjects under study have
been omitted.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Steiner T, Juvela S, Unterberg A, Jung C,
Forsting M and Rinkel G: European Stroke Organization. European
stroke organization guidelines for the management of intracranial
aneurysms and subarachnoid haemorrhage. Cerebrovasc Dis. 35:93–112.
2013.PubMed/NCBI View Article : Google Scholar
|
|
2
|
D'Souza S: Aneurysmal subarachnoid
hemorrhage. J Neurosurg Anesthesiol. 27:222–240. 2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Petridis AK, Kamp MA, Cornelius JF, Beez
T, Beseoglu K, Turowski B and Steiger HJ: Aneurysmal subarachnoid
hemorrhage. Dtsch Arztebl Int. 114:226–236. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Fotakopoulos G, Tsianaka E, Fountas K,
Makris D, Spyrou M and Hernesniemi J: Clipping versus coiling, in
anterior circulation ruptured intracranial aneurysms: A
meta-analysis. World Neurosurg. 104:482–488. 2017.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Fotakopoulos G, Andrade-Barazarte H,
Tjahjadi M, Goehre F and Hernesniemi J: Clipping versus coiling in
ruptured basilar apex aneurysms: A meta-analysis. Turk Neurosurg.
31:301–309. 2021.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Tsolaki V, Aravantinou-Fatorou A,
Georgakopoulou VE, Spandidos DA, Papalexis P, Mathioudakis N,
Tarantinos K, Trakas N, Sklapani P and Fotakopoulos G: Early
diagnosis of cerebral vasospasm associated with cerebral ischemia
following subarachnoid hemorrhage: Evaluation of computed
tomography perfusion and transcranial doppler as accurate methods.
Med Int (Lond). 2(34)2022.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Fotakopoulos G, Makris D, Kotlia P,
Kapsalaki E, Papanikolaou J, Georgiadis I, Zakynthinos E and
Fountas K: The value of computed tomography perfusion &
transcranial Doppler in early diagnosis of cerebral vasospasm in
aneurysmal & traumatic subarachnoid hemorrhage. Future Sci OA.
4(FSO313)2018.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Zhang Y, Zhu X, Hou K, Zhao J, Gao X, Sun
Y, Wang W and Zhang X: Clinical outcomes of surgical clipping for
intracranial aneurysms in patients with a Hunt and Hess grade 4 or
5. Arq Neuropsiquiatr. 74:478–481. 2016.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Fotakopoulos G, Andrade-Barazarte H,
Alexandros B and Hernesniemi J: A meta-analysis of lateral
supraorbital vs. mini pterional approach in the outcome of rupture
and unruptured noncomplex aneurysms' surgery. Neurocirugia (Engl
Ed). 34:128–138. 2023.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fotakopoulos G, Georgakopoulou VE, Gatos
C, Christodoulidis G and Foroglou N: Microsurgery treatment as an
optimal management of posterior cerebral artery aneurysms: A
systematic review and meta-analysis. Cureus.
17(e77856)2025.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Mohammad F, Horiguchi T, Mizutani K and
Yoshida K: Clipping versus coiling in ruptured aneurysms of the
anterior cerebral circulation. Open J Mod Neurosurg. 10:88–104.
2020.
|
|
12
|
Ahmed SI, Javed G, Bareeqa SB, Samar SS,
Shah A, Giani A, Aziz Z, Tasleem A and Humayun SH: Endovascular
coiling versus neurosurgical clipping for aneurysmal subarachnoid
hemorrhage: A systematic review and meta-analysis. Cureus.
11(e4320)2019.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Dellaretti M, Batista DM, de Almeida JC,
de Souza RF, Ronconi DE, de Almeida CER, Fontoura RR and Júnior WF:
Surgical treatment of ruptured intracranial aneurysms: Timing of
treatment and outcome. Interdiscip Neurosurg. 14:178–182. 2018.
|
|
14
|
Yao Z, Hu X, Ma L, You C and He M: Timing
of surgery for aneurysmal subarachnoid hemorrhage: A systematic
review and meta-analysis. Int J Surg. 48:266–274. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Weil AG and Zhao JZ: Treatment of ruptured
aneurysms: Earlier is better. World Neurosurg. 77:263–265.
2012.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Duangthongphon P, Souwong B, Munkong W and
Kitkhuandee A: Results of a preventive rebleeding protocol in
patients with ruptured cerebral aneurysm: A retrospective cohort
study. Asian J Neurosurg. 14:748–753. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Drake CG: Progress in cerebrovascular
disease. Management of cerebral aneurysm. Stroke. 12:273–283.
1981.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Nieuwkamp DJ, de Gans K, Algra A, Albrecht
KW, Boomstra S, Brouwers PJAM, Groen RJM, Metzemaekers JDM, Nijssen
PCG, Roos YBWEM, et al: Timing of aneurysm surgery in subarachnoid
haemorrhage-an observational study in The Netherlands. Acta
Neurochir (Wien). 147:815–821. 2005.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Broderick JP, Adeoye O and Elm J:
Evolution of the modified rankin scale and its use in future stroke
trials. Stroke. 48:2007–2012. 2017.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Mahaney KB, Todd MM and Torner JC: IHAST
Investigators. Variation of patient characteristics, management,
and outcome with timing of surgery for aneurysmal subarachnoid
hemorrhage. J Neurosurg. 114:1045–1053. 2011.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Chyatte D, Fode NC and Sundt TM Jr: Early
versus late intracranial aneurysm surgery in subarachnoid
hemorrhage. J Neurosurg. 69:326–231. 1988.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Dorhout Mees SM, Molyneux AJ, Kerr RS,
Algra A and Rinkel GJE: Timing of aneurysm treatment after
subarachnoid hemorrhage: Relationship with delayed cerebral
ischemia and poor outcome. Stroke. 43:2126–2129. 2012.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Zhao C and Wei Y: Surgical timing for
aneurysmal subarachnoid hemorrhage: A meta-analysis and systematic
review. Turk Neurosurg. 27:489–499. 2017.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Kassell NF and Drake CG: Timing of
aneurysm surgery. Neurosurgery. 10:514–519. 1982.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Lawson MF, Chi YY, Velat GJ, Mocco JD and
Hoh BL: Timing of aneurysm surgery: The international cooperative
study revisited in the era of endovascular coiling. J Neurointerv
Surg. 2:131–134. 2010.PubMed/NCBI View Article : Google Scholar
|