Introduction
Chronic low back pain (CLBP) is a pervasive
condition that significantly impairs the quality of life of
patients by limiting daily activities and overall well-being
(1,2). Additionally, anterior column pain, the
cause of CLBP, has been theorized to stem from the pain receptors
of intervertebral discs. However, recent histological data suggest
that the vertebral endplates may play a predominant role, as they
manifest up to four times the number of nerve receptors compared
with intervertebral discs (3-5).
Overall, vertebrogenic low back pain and discogenic
low back pain are considered two entirely dissimilar entities.
Discogenic pain arises from the degeneration of the intervertebral
disc, particularly the annulus fibrosus, and is transmitted via the
sinuvertebral nerve. Discogenic pain accounts for a substantial
portion of cases of CLBP, with estimates ranging from 26 to 42%
(2-5).
It is caused by structural defects, such as annular tears, disc
dehydration and the loss of disc height, leading to inflammation,
nerve ingrowth and altered biomechanics. Clinically, it presents as
axial low back pain worsened by sitting and flexion, with referred
pain above the knees in a non-dermatomal pattern and no
neurological deficits. Magnetic resonance imaging (MRI) may depict
disc desiccation and high-intensity zones, whilst a discography can
confirm diagnosis, although this is considered invasive (3-7).
On the contrary, vertebrogenic pain is a newer concept linked to
the damage and inflammation of the vertebral endplates, innervated
by the basivertebral nerve. It is noteworthy that vertebrogenic
pain is estimated to affect ~1 in 6 individuals with CLBP in the
USA (3-6).
It is associated with Modic type 1 or 2 alterations observed on an
MRI and results from endplate microtrauma, allowing inflammatory
disc material to infiltrate the bone marrow. Symptoms typically
involve midline low back pain, which deteriorates in the morning or
with activity, with possible referral to paraspinal or gluteal
regions. Unlike discogenic pain, it is not aggravated by extension
and may present without significant disc abnormalities on imaging
(5-7).
First-line management for CLBP, including vertebrogenic CLBP,
involves nonpharmacologic therapy such as exercise, physical
therapy, spinal manipulation and acupuncture, while non-steroidal
anti-inflammatory drugs, muscle relaxants etc. are used as
second-line therapy (7); however, in
a significant portion of individuals, those treatments do not
exhibit the desired outcomes (5-7).
The main limitations of the conservative management of
vertebrogenic CLBP are considered limited long-term effectiveness,
the inability to address the source of pain, the risk of dependence
on pain medication and the lack of improvement with certain
therapies such as traction or transcutaneous electrical nerve
stimulation (4-8).
In light of this evidence, interventions have been
employed to manage CLBP by specifically targeting the intradiscal
space and vertebral endplates, including intradiscal steroid
injections (IDSIs) and intraosseous basivertebral nerve
radiofrequency ablations (BVAs) (8,9). IDSI
involves injecting corticosteroids in the center of intervertebral
discs (10), whereas BVA cauterizes
the basivertebral nerve within the vertebral body (11,12).
There is clinical ambiguity as regards which of these two
interventions is superior concerning the treatment of vertebrogenic
CLBP. Targeting the basivertebral nerve may be more effective than
targeting the disc itself for vertebrogenic pain, as the
basivertebral nerve is the primary nerve responsible for
transmitting pain signals from the vertebral endplates, which are
frequently damaged in cases of vertebrogenic pain, and nerve
density is higher in endplates (7-12).
To the best of our knowledge, no study in the existing literature
to date has performed a direct comparison of IDSI and BVA for the
treatment of vertebrogenic CLBP. Thus, the present study aimed to
fill this gap in the literature. The present study aimed to compare
the efficacy of these two interventions in reducing disability and
pain levels in patients with vertebrogenic CLBP, while utilizing
the Oswestry Disability Index (ODI) (13), as it is specific for CLBP and easy to
use. The present study aimed to provide clinicians with insight
into the most effective treatment options for this challenging
condition.
Background information and description
of IDSI and BVA techniques
During intradiscal steroid injections, a single
physician performs each intradiscal injection via the
posterolateral disc access approach. The patient lies in a prone
position, and the targeted intervertebral disc is identified via
fluoroscopy. The overlying skin is prepped surgically and
anesthetized with lidocaine. A 22-gauge spinal needle with guidance
from intermittent fluoroscopy is then advanced towards the center
of the disc via a right or left posterolateral oblique window.
Finally, anteroposterior and lateral visualization ensures the
correct needle position before 2 cc of depo-methylprednisolone is
inserted into the disc space. Depo-methylprednisolone is delivered
directly into the intravertebral space, where it exerts potent
anti-inflammatory and analgesic effects (14). This reduces inflammation, alleviates
pain and improves functional outcomes in patients suffering from
CLBP (15,16). IDSI has shown promising results, with
a number of patients experiencing substantial reductions in
disability levels post-injection (12,14).
However, the outcomes can vary, with some patients demonstrating a
complete resolution of symptoms and others exhibiting minimal
improvement (12,14-19).
Reported side-effects known from the literature include transient
pain at the injection site, increased blood sugar levels, and, in
rare cases, infection. These potential side-effects necessitate
careful patient selection and monitoring (17-19).
On the other hand, during intraosseous basivertebral
nerve radiofrequency ablation, the patient is in the prone
position, the C-Arm is prepositioned, the skin is prepped
surgically, and local anesthetization is applied. Multiple
fluoroscopies are employed to ensure that the proper trajectory of
the trocar in pedicle care starts at the superior lateral aspect
until it passes through the posterior vertebral body wall. It is
important to maintain a position superior to the inferior cortex
and lateral to the medial cortex of the pedicle to prevent trocar
entry into the spinal canal or near neural elements. Once the
trocar is inserted into the vertebral body, it is removed, and a
curved stylus is inserted to guide it to the center of the
vertebral body. With proper placement, the stylus is retracted, and
the cautery is placed and used to create a 1 cm spherical lesion
(85˚C for 15 min). BVA involves targeting the basivertebral nerve
within the vertebral body to disrupt pain signals (20). This procedure uses radiofrequency
energy to ablate nerve fibers responsible for transmitting pain,
providing long-lasting pain relief (20-23).
BVA consistently reduces disability and pain levels across patient
cohorts (21-25).
The procedure has been reported to be effective for a significant
proportion of patients, although some outliers do not experience
any change in their disability levels (23,24).
This technique is generally well-tolerated; however, potential
side-effects include temporary discomfort at the treatment site,
infection and nerve damage (23).
These risks underscore the importance of precise techniques and
patient selection (21,22).
Patients and methods
Patients and selection criteria
A retrospective analysis was conducted on patients
who underwent either IDSI or BVA treatment for vertebrogenic CLBP
separated into two groups. The technique employed in each group was
performed exactly as aforementioned. The timeframe in which the
present retrospective study was conducted was ~2 years, from
January, 2022 to December, 2023. The patients in group 1 underwent
IDSI treatment and this group consisted of 12 patients, while those
in group 2 underwent BVA treatment and this group included 10
patients. Patient selection criteria included individuals aged from
18 to 70 years, males or females regardless of sex, who complained
about persistent CLBP over the past ≥3 months at least, and having
undergone lumbar spine MRI scan in which the findings (Modic
changes type 1 and/or 2, vertebral endplate defects and endplate
pathology) confirmed the vertebrogenic nature of the CLBP. In
addition, in terms of inclusion criteria, the patients included had
no notable comorbidities and major health issues, and had undergone
only conservative treatment for their pain with per os
medication and/or physiotherapy and no previous invasive treatment
at any stage of the symptoms. On the contrary, the exclusion
criteria included patients aged <18 years or >70 years of
age, patients with no MRI findings that were associated with
vertebrogenic CLBP and patients with symptoms lasting for <3
months. Furthermore, patients that were excluded from the study
were individuals that had previously undergone any type of invasive
and not conservative-only treatment for CLBP and patients with
considerable comorbidities or major health issues. The patients
were randomly allocated into the two groups, and no group-matching
by age, sex, comorbidities or symptom duration was carried out.
There were no criteria employed to determine whether a patient
received the IDSI treatment or the BVA technique. There were no
variations in the ablation protocol in the second group. ODI scores
before and after treatment were collected to assess the impact of
these interventions on disability and pain levels (16). The procedures were performed by the
same physicians each time. Follow-up duration of the patients was 6
months in total, while patients were clinically evaluated at 1
week, 1 month, 3 months and 6 months following the intervention,
respectively. The ODI score at 3 months post-intervention was
utilized as post-treatment value in the statistical analysis as the
improvement measurement time. No notable adverse events were
observed in all the patients involved in the study during treatment
and follow-up.
All procedures performed in studies involving human
participants were in accordance with the ethical standards of the
institutional and/or national research committee. The present study
was approved by the Ethics Committee of KAT Attica General
Hospital, Athens, Greece (Ref. no. 20869). Written informed consent
was obtained from all patients included in the study.
Statistical analysis
Comparisons of pre- and posttest outcomes for each
treatment method were made using repeated measures ANOVA. The 2
patients who exhibited no improvement were excluded from the
analysis (1 patient from each group). Furthermore, another reason
for the exclusion of theses 2 patients was limited follow-up and
incomplete data. All assumptions for the test were met (26). To improve the statistical power of
the analysis when comparing the efficacy of each intervention
against the other, the two methods were compared with ANCOVA, which
provides the relative improvement of each treatment method compared
with a normalized baseline. As per the prerequisite, all
assumptions were met (27).
Results
Both treatments revealed very promising results in
reducing CLBP to levels practically considered complete resolution.
In the present study sample, there were only two outliers, one for
each method, which reported no difference in symptoms. These
patients were excluded from the analysis due to the possible
misdiagnosis of discogenic pain as the origin of their symptoms. At
this point, it is imperative to underline that excluding 2 patients
who were non-responsive may have led to bias in the outcomes and
may overstate the effectiveness of the treatments. Notwithstanding,
even in the event that those patients were finally included, both
treatments resulted in a >90% reduction in pain and disability.
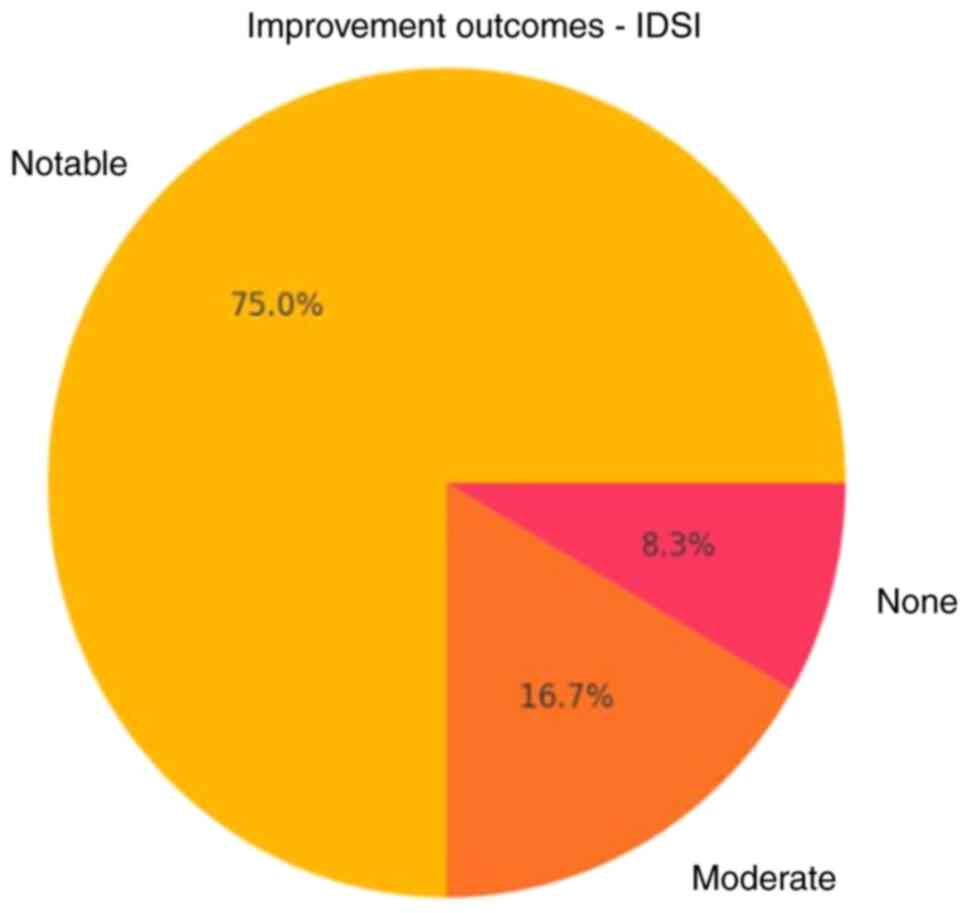
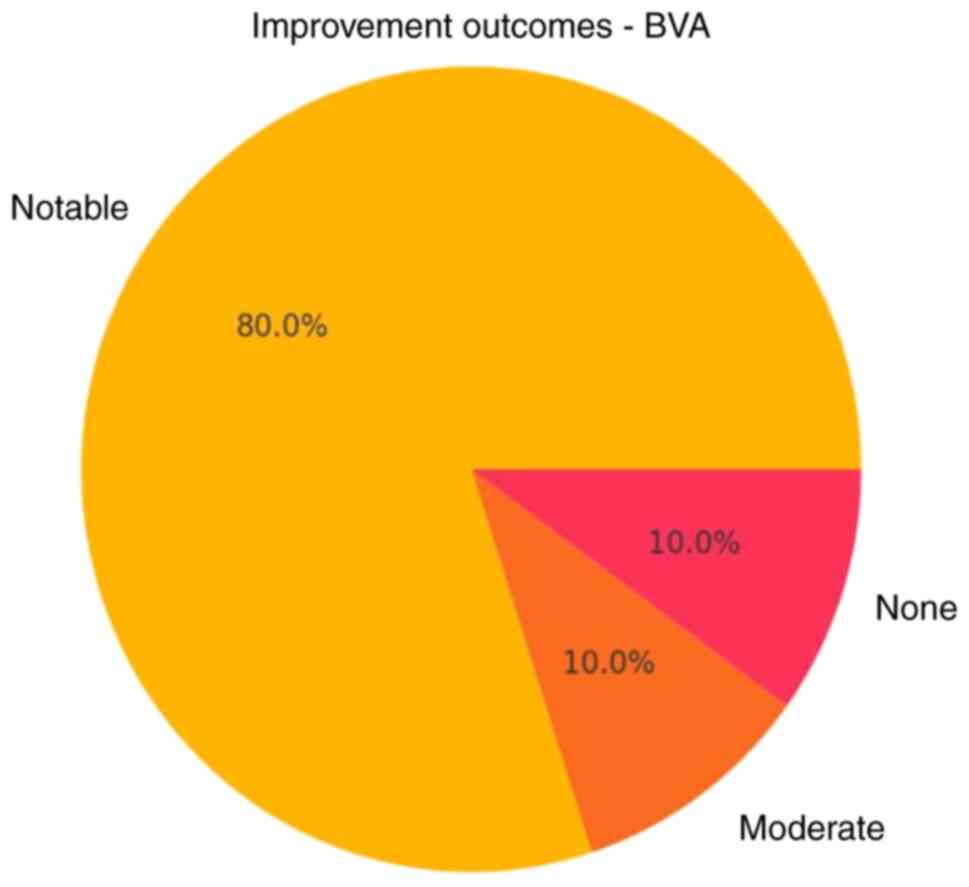
In the analysis in the present study, as demonstrated by the data
in Tables I and II, an improvement of <50% was
considered subjectively moderate. A value >50% was considered
notable, and a value <30% was considered as non-notable.
 | Table IClinical outcomes of patients treated
with intraarticular depo-methylprednisolone injection. |
Table I
Clinical outcomes of patients treated
with intraarticular depo-methylprednisolone injection.
| Patient no. | Sex (F/M) | Age (years) | BMI | Anxiety score
(BAI) | Fear-avoidance score
(FABQ) | Follow-up
(months) | Initial disability
level | ODI score before
treatment | ODI score after
treatment | Improvement
outcome |
|---|
| 1 | M | 51 | 22 | 15 | 22 | 18 | Minimal | 14 | 4 | Notable |
| 2 | M | 43 | 28 | 22 | 28 | 22 | Minimal | 18 | 3 | Notable |
| 3 | F | 61 | 30 | 25 | 29 | 6 | Minimal | 18 | 2 | Notable |
| 4 | M | 55 | 25 | 17 | 20 | 12 | Moderate | 22 | 4 | Notable |
| 5 | F | 40 | 21 | 20 | 28 | 20 | Moderate | 22 | 3 | Notable |
| 6 | F | 49 | 26 | 18 | 22 | 24 | Moderate | 24 | 8 | Notable |
| 7 | M | 58 | 20 | 18 | 25 | 10 | Moderate | 24 | 12 | Notable |
| 8 | F | 44 | 22 | 23 | 30 | 18 | Moderate | 27 | 5 | Notable |
| 9 | F | 59 | 31 | 26 | 32 | 12 | Moderate | 34 | 22 | Moderate |
| 10 | M | 46 | 27 | 14 | 26 | 6 | Moderate | 34 | 24 | Moderate |
| 11 | M | 43 | 25 | 15 | 23 | 14 | Moderate | 40 | 6 | Notable |
| 12 | M | 65 | 25 | 17 | 25 | 4 | Crippling | 77 | 77 | None |
 | Table IIClinical outcomes of patients treated
with intra-osseous basivertebral nerve radiofrequency ablation. |
Table II
Clinical outcomes of patients treated
with intra-osseous basivertebral nerve radiofrequency ablation.
| Patient no. | Sex (F/M) | Age (years) | BMI | Anxiety score
(BAI) | Fear-avoidance
score (FABQ) | Follow-up
(months) | Initial disability
level | ODI score before
treatment | ODI score after
treatment | Improvement
outcome |
|---|
| 1 | M | 39 | 20 | 20 | 25 | 6 | Minimal | 7 | 7 | Notable |
| 2 | M | 48 | 26 | 25 | 31 | 18 | Minimal | 17 | 5 | Notable |
| 3 | F | 44 | 25 | 27 | 31 | 10 | Minimal | 18 | 4 | Notable |
| 4 | M | 62 | 25 | 22 | 24 | 22 | Minimal | 20 | 3 | Notable |
| 5 | F | 55 | 23 | 30 | 28 | 16 | Moderate | 33 | 6 | Notable |
| 6 | F | 58 | 30 | 26 | 25 | 4 | Moderate | 34 | 20 | Moderate |
| 7 | M | 44 | 20 | 16 | 22 | 24 | Moderate | 39 | 6 | Notable |
| 8 | F | 51 | 22 | 19 | 24 | 16 | Severe | 43 | 5 | Notable |
| 9 | M | 55 | 29 | 18 | 27 | 6 | Severe | 43 | 43 | None |
| 10 | M | 60 | 26 | 25 | 32 | 12 | Severe | 46 | 1 | Notable |
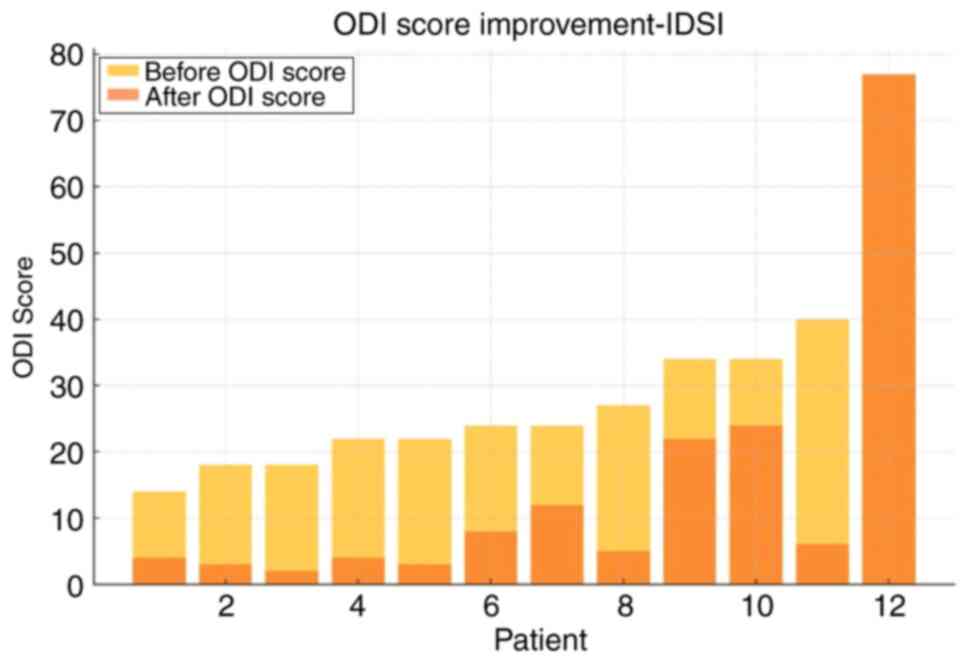
For IDSI (Table I),
the mean pre-treatment ODI was 29.9±16.5, which significantly
decreased to 14.8±20.4 post-treatment (P=0.0001), representing an
absolute reduction of 16.5 and a 66% relative improvement (Figs. 1 and 2). Of note, only 2 patients achieved
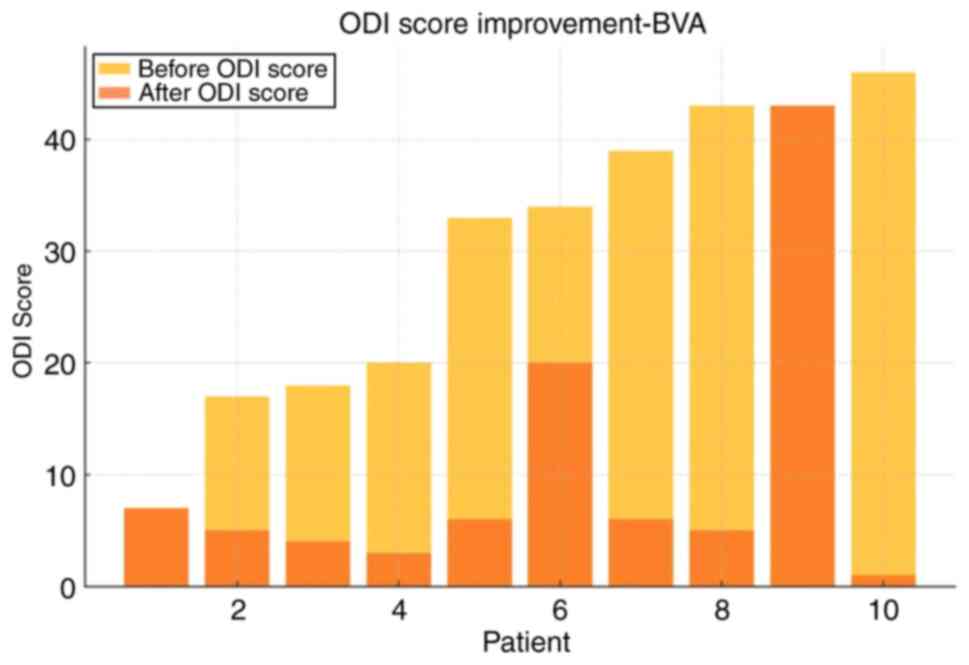
moderate improvement (<50%). BVA treatment also demonstrated
satisfactory results in reducing CLBP (Table II). In the BVA group (n=10), the
mean ODI score significantly decreased from 30.1±13.6 before
treatment to 10.1±12.6 after treatment (P=0.0023). When both groups
were analyzed together, the overall baseline ODI mean was
28.5±15.2, which was reduced to 6.3±8.7 post-treatment,
corresponding to a 78% mean reduction in disability. Notably, 90%
of the patients experienced significant improvement (>50%)
(Figs. 3 and 4).
Covariate analysis (ANCOVA) was conducted to control
for potential confounding factors. The adjusted pre-treatment means
were 26.7±14.8 for both groups. Covariates utilized in ANCOVA were
baseline ODI scores, anxiety that was assessed using the Beck
Anxiety Inventory (BAI) (mean ± SD: 12.4±3.5), fear-avoidance score
using the Fear Avoidance Beliefs Questionnaire (FABQ) (18.9±5.2),
age (47.2±8.1 years), sex (male:female, 9:13) and BMI (26.8±3.4
kg/m2). The adjusted post-treatment mean values were
8.7±6.1 for IDSI and 5.9±4.8 for BVA, with a statistically
significant between-group difference (P=0.046). Overall, there
appears to be a small improvement in BVA in the present study;
however, owing to the small sample size of our patients, the
statistical power of our research was 40%, which is not
sufficient-enough for highly credible outcomes.
Both interventions in the present study resulted in
a notable improvement for >80% of the patients treated and at
least a moderate reduction in disability (between 30 and 50%) for
>90% of them (Figs. 2 and
3). Furthermore, a minimal, yet
considerable advantage was demonstrated in the analysis for BVA vs.
IDSI, with the obvious caveat of the low statistical power of the
research. Notably, both treatments resulted in post-treatment ODI
scores of <10, 75% for IDSI and 80% for BVA, which translates to
the almost complete resolution of symptoms (Figs. 1 and 2). Another noteworthy element is that 2
patients (1 patient from each group) exhibited no difference pre-
and post-intervention, which may be attributed to unknown factors
or that the treatments themselves could be ineffective in a
percentage of patients (Fig. 1,
Fig. 2, Fig. 3 and Fig.
4); it would be of interest to evaluate this finding in a
larger patient sample.
Consequently, both IDSI and BVA could be considered
viable and highly recommended options for immediate pain reduction
in patients with CLBP; however, due to the methodological
weaknesses of the present study, the findings can be considered as
hypothesis-generating.
Discussion
The comparative analysis of IDSI and BVA for the
treatment of vertebrogenic CLBP can provide several critical
insights. Both treatments have demonstrated efficacy in reducing
pain and disability; however, their mechanisms and clinical
outcomes vary, highlighting the need for a personalized approach in
managing CLBP. The mechanisms of action for IDSI and BVA are
distinct and crucial; although they are used for the same
pathologic entity (CLBP), both demonstrate similar and high
efficacy. IDPI utilizes the anti-inflammatory properties of locally
infused corticosteroids in the body of the intervertebral disc
(9,10).
Contrariwise, BVA targets the nerve pathways
responsible for pain transmission on the vertebral endplates
themselves, providing a more direct approach to pain relief. This
method has exhibited consistent results across a broader range of
patients, making it a reliable option for many patients (21-25).
The direct disruption of pain signals can provide long-lasting
relief, which is crucial for managing chronic conditions (4,5).
The difference in both the area and mechanism of
treatment, compared with the similar effectiveness of IDSI and BVA,
raises the question of which pain receptors are involved and what
exactly the pathologoanatomical substrate of vertebrogenic CLBP is.
If either disc or vertebral pain receptors are prevalent in CLBP,
then the expected result of one of the treatments used herein would
clearly be highly superior to that of the other, which was not the
case reported in the present study or in the existing literature.
As a result, further large-scale studies are warranted to
investigate and differentiate the factors associated with CLBP.
Both treatments may trigger potential side-effects
that need to be carefully managed. The side-effects of IDSIs, such
as transient pain and increased blood sugar levels, require
monitoring, particularly in patients with diabetes (9,10). BVAs,
while generally well-tolerated, carry risks of nerve damage and
infection, necessitating precise techniques and patient education
about potential risks (23-25).
Clinicians should weigh the benefits and risks of each treatment
option, considering patient preferences and the likelihood of
response. The selection between IDSI and BVA should be made by a
comprehensive clinical assessment, ensuring that the selected
treatment aligns with the specific condition and goals of the
patient. The presence of outliers in both treatment groups suggests
that neither IDSI nor BVA is universally effective for all
patients. It should be emphasized that the exclusion of these
patients represents a methodological flaw that can distort the
reported outcomes. The variability in responses highlights the
requirement for careful patient selection on the basis of specific
clinical criteria. Factors, such as the nature of the pain,
previous treatment responses and patient comorbidities should guide
treatment decisions. Personalized treatment plans can optimize
outcomes by matching patients with the most appropriate
intervention. Given the various notable limitations of the present
study, it is not facile to propose a standard treatment algorithm
for vertebrogenic CLBP. Nonetheless, it can be denoted that these
two interventions can be utilized in patients aged 18-70 years with
no considerable comorbidities and persistent LBP for a period of
>3 months where conservative treatment has failed, whist the
selection of employing either IDSI or BVA as treatment of choice
lies in the attending physician as they both seem as viable
fruitful treatment options. In the case of the failure of one
method, the attending physician may consider utilizing the other
treatment method as an alternative; however, this practice can be
the objective of further research.
Further research is essential to refine these
treatments and identify predictors of response. Perusing the
existing literature, no other study could be retrieved comparing
these two treatment methods for CLBP, whilst only a limited number
of review articles could be found presenting the various minimally
invasive treatments for CLBP that already exist. Hence, prospective
studies with larger sample sizes and randomized controlled trials
are vital and could provide more definitive evidence on the
comparative effectiveness of IDSI and BVA. Additionally, exploring
combination therapies and adjunctive treatments may offer new
avenues for patients who do not respond to either intervention
alone.
For a more balanced interpretation of the outcomes,
it is vitally important to acknowledge the copious major
limitations of the present study which include the following: The
retrospective design of the study, the small sample size, the
exclusion of outliers, the absence of a placebo or sham control
group, methodological flaws, reliance on subjective data (ODI
scores), limited follow-up duration and low statistical power. At
this point, the necessity for further larger-scale studies in this
field is accentuated, as the present study can be considered as
thought-provoking material.
In conclusion, both IDSI and intra-osseous BVA
appeared to effectively reduce disability. The IDSIs demonstrated a
higher percentage of complete symptom resolution, whereas BVAs
provided more consistent significant improvements across patients.
Despite potential side-effects, both treatments can provide
substantial pain relief, potentially underscoring the significance
of personalized treatment plans. Notwithstanding, in spite of both
treatments exhibiting potential, taking into account the various
considerable limitations of the present small-scale study, the
findings should be regarded as hypothesis-generating, highlighting
the requirement for further pertinent research in this area.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
ES, EA, VM and PK conceptualized the study. ES, EA,
AK, DT and AG were involved in the study methodology. PK, NP, SP
and DT were involved in data validation. EV, AM and MR were
involved in the formal analysis. ES, AG, AM and EA were involved in
the investigative aspects of the study. ES, EA and AG were involved
in the writing and preparation of the original draft of the
manuscript. ES and EA were involved in the writing, reviewing and
editing of the manuscript, and in visualization. PK, VM and SP
supervised the study. AG and AK were involved in project
administration. ES and NP assisted with the public use of the
hospital materials and operating rooms. AM and PK confirm the
authenticity of all raw data. All authors have read and agreed to
the published version of the manuscript.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were in accordance with the ethical standards of the
institutional and/or national research committee. The present study
was approved by the Ethics Committee of KAT Attica General
Hospital, Athens, Greece (Ref. no. 20869). Written informed consent
was obtained from all patients included in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Hoy D, Bain C, Williams G, March L, Brooks
P, Blyth F, Woolf A, Vos T and Buchbinder R: A systematic review of
the global prevalence of low back pain. Arthritis Rheum.
64:2028–2037. 2012.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Shmagel A, Foley R and Ibrahim H:
Epidemiology of chronic low back pain in US adults: Data from the
2009-2010 National Health and Nutrition Examination Survey.
Arthritis Care Res (Hoboken). 68:1688–1694. 2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Yang G, Liao W, Shen M and Mei H: Insight
into neural mechanisms underlying discogenic back pain. J Int Med
Res. 46:4427–4436. 2018.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Ohtori S, Inoue G, Miyagi M and Takahashi
K: Pathomechanisms of discogenic low back pain in humans and animal
models. Spine J. 15:1347–1355. 2015.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Conger A, Smuck M, Truumees E, Lotz JC,
DePalma MJ and McCormick ZL: Vertebrogenic pain: A paradigm shift
in diagnosis and treatment of axial low back pain. Pain Med. 23
(Suppl 2):S63–S71. 2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Lorio MP, Beall DP, Calodney AK,
Lewandrowski KU, Block JE and Mekhail N: Defining the patient with
lumbar discogenic pain: Real-world implications for diagnosis and
effective clinical management. J Pers Med. 13(821)2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Abel F, Altorfer FCS, Rohatgi V, Gibbs W
and Chazen JL: Imaging of Discogenic and vertebrogenic pain. Radiol
Clin North Am. 62:217–228. 2024.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Tieppo Francio V, Sherwood D, Twohey E,
Barndt B, Pagan-Rosado R, Eubanks J and Sayed D: Developments in
minimally invasive surgical options for vertebral pain:
Basivertebral nerve Ablation-A narrative review. J Pain Res.
14:1887–1907. 2021.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Miller S, Caragea M, Carson D, McFarland
MM, Teramoto M, Cushman DM, Cooper AN, Burnham T, McCormick ZL and
Conger A: The effectiveness of intradiscal corticosteroid injection
for the treatment of chronic discovertebral low back pain: A
systematic review. Pain Med. 25:33–46. 2024.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Hashemi M, Poorfarokh M, Mohajerani SA,
Jalili P, Akhyani V, Barikani A and Farivar F: Injection of
intradiscal O2-O3 to reduce pain and
disability of patients with low back pain due to prolapsed lumbar
disk. Anesth Pain Med. 4(e19206)2014.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Khalil JG, Smuck M, Koreckij T, Keel J,
Beall D, Goodman B, Kalapos P, Nguyen D and Garfin S: INTRACEPT
Trial Investigators. A prospective, randomized, multicenter study
of intraosseous basivertebral nerve ablation for the treatment of
chronic low back pain. Spine J. 19:1620–1632. 2019.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Michalik A, Conger A, Smuck M, Maus TP and
McCormick ZL: Intraosseous basivertebral nerve radiofrequency
ablation for the treatment of vertebral body endplate low back
pain: Current evidence and future directions. Pain Med. 22 (Suppl
1):S24–S30. 2021.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Fairbank JC and Pynsent PB: The oswestry
disability index. Spine (Phila Pa 1976). 25:2940–2952.
2000.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Johansson A, Hao J and Sjölund B: Local
corticosteroid application blocks transmission in normal
nociceptive C-fibers. Acta Anesthesiol Scand. 34:335–338.
1990.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Ramesh G, Meisner OC and Philipp MT:
Anti-inflammatory effects of dexamethasone and meloxicam on
Borrelia burgdorferi-induced inflammation in neuronal
cultures of dorsal root ganglia and myelinating cells of the
peripheral nervous system. J Neuroinflammation.
12(240)2015.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Cao P, Jiang L, Zhuang C, Yang Y, Zhang Z,
Chen W and Zheng T: Intradiscal injection therapy for degenerative
chronic discogenic low back pain with end plate Modic changes.
Spine J. 11:100–106. 2011.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Nguyen C, Boutron I, Baron G, Sanchez K,
Palazzo C, Benchimol R, Paris G, James-Belin É, Lefèvre-Colau MM,
Beaudreuil J, et al: Intradiscal glucocorticoid injection for
patients with chronic low back pain associated with active
discopathy: A randomized trial. Ann Intern Med. 166:547–556.
2017.PubMed/NCBI View
Article : Google Scholar
|
|
18
|
Khot A, Bowditch M, Powell J and Sharp D:
The use of intradiscal steroid therapy for lumbar spinal discogenic
pain: A randomized controlled trial. Spine (Phila Pa 1976).
29:833–836. 2004.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Tavares I, Thomas E, Cyteval C, Picot MC,
Manna F, Macioce V, Laffont I, Thouvenin Y, Viala P, Larbi A, et
al: Intradiscal glucocorticoids injection in chronic low back pain
with active discopathy: A randomized controlled study. Ann Phys
Rehabil Med. 64(101396)2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
McCormick ZL, Sperry BP, Boody BS, Hirsch
JA, Conger A, Harper K, Lotz JC and Burnham TR: Pain location and
exacerbating activities associated with treatment success following
basivertebral nerve ablation: An aggregated cohort study of
multicenter prospective clinical trial data. Pain Med. 23 (Suppl
2):S14–S33. 2022.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Becker S, Hadjipavlou A and Heggeness MH:
Ablation of the basivertebral nerve for treatment of back pain: A
clinical study. Spine J. 17:218–223. 2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Fischgrund JS, Rhyne A, Franke J, Sasso R,
Kitchel S, Bae H, Yeung C, Truumees E, Schaufele M, Yuan P, et al:
Intraosseous basivertebral nerve ablation for the treatment of
chronic low back pain: A prospective randomized double-blind
sham-controlled multi-center study. Eur. Spine J. 27:1146–1156.
2018.PubMed/NCBI View Article : Google Scholar
|
|
23
|
DSmuck M, Khalil J, Barrette K, Hirsch JA,
Kreiner S, Koreckij T, Garfin S and Mekhail N: Prospective,
randomized, multicenter study of intraosseous basivertebral nerve
ablation for the treatment of chronic low back pain: 12-month
results. Reg Anesth Pain Med. 46:683–693. 2021.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Truumees E, Macadaeg K, Pena E, Arbuckle
J, Gentile J, Funk R, Singh D and Vinayek S: A prospective,
open-label, single-arm, multicenter study of intraosseous
basivertebral nerve ablation for the treatment of chronic low back
pain. Eur Spine J. 28:1594–1602. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Macadaeg K, Truumees E, Boody B, Pena E,
Arbuckle J, Gentile J, Funk R, Singh D and Vinayek S: A
prospective, single arm study of intraosseous basivertebral nerve
ablation for the treatment of chronic low back pain: 12-month
results. N Am Spine Soc J. 3(100030)2020.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Cohen J: Statistical power analysis for
the behavioral sciences. Hillsdale: L.Erlbaum Associates, 1988.
|
|
27
|
Borm GF, Fransen J and Lemmens WA: A
simple sample size formula for analysis of covariance in randomized
clinical trials. J Clin Epidemiol. 60:1234–1238. 2007.PubMed/NCBI View Article : Google Scholar
|