Introduction
Acromegaly is a rare, yet serious disorder resulting
from the chronic hypersecretion of growth hormone (GH) and
insulin-like growth factor-1 (IGF-1), most commonly due to
pituitary adenomas (1).
Historically, patients with acromegaly were often viewed as
attractions due to their unusual physical appearance (2). The disease develops insidiously, and
clinical manifestations include the enlargement of the hands and
feet, coarse facial features, fatigue, metabolic dysfunction and
cardiovascular complications (3).
Untreated acromegaly is associated with increased morbidity and
mortality, primarily due to cardiometabolic and respiratory
sequelae (4). The standard of care
for GH-secreting adenomas is transsphenoidal resection, often
followed by medical therapy, such as somatostatin analogs, dopamine
agonists, or GH receptor antagonists, as well as radiotherapy when
necessary (5).
Reports of the spontaneous regression of pituitary
adenomas are exceedingly rare, particularly in hormone-secreting
tumors. Regression, when it occurs, is typically attributed to
pituitary apoplexy, ischemic infarction, or hemorrhage within the
adenoma (6). Reports of GH-secreting
adenomas undergoing spontaneous shrinkage are limited (7). Notably, thyroid disease, including
multinodular goiter, is relatively common in acromegaly (78%)
compared to other pituitary tumors (27%). However, the occurrence
of toxic multinodular goiter with superior vena cava obstruction
(SCVO) in such patients is unusual (8).
The present study describes the case of a
middle-aged male patient with acromegaly who developed
thyrotoxicosis due to a toxic multinodular goiter, complicated by
SVCO. Following thyroidectomy, the patient experienced the
regression of his pituitary adenoma and the normalization of his
IGF-1 levels. To the best of our knowledge, such an association has
not been previously reported in the literature.
Case report
The present study reports the case of a 51-year-old
male patient with acromegaly who presented to the Azadi Teaching
Hospital (affiliated with the College of Medicine at University of
Duhok), Duhok, Iraq in November, 2023. He noted the progressive
enlargement of his hands and feet, accompanied by changes in facial
appearance, which began when he was 44 years of age. He required
larger shoe sizes and clothing and his wedding band no longer fit.
His family observed a gradual deepening of his voice. The patient
experienced easy fatigability; however, he had no headaches,
diaphoresis or fever, and did not experience any weight gain. He
was yet to meet a specialist at this time. Subsequently, at the age
of 46 years, he developed a worsening shortness of breath, poor
sleep quality and frequent nocturnal dyspnea relieved by sitting
upright. He also reported excessive daytime somnolence and
irritability, with no cough, chest pain or palpitations. He was
first evaluated for acromegaly at the age of 48 years through
laboratory and imaging analyses. The GH suppression test revealed
high GH levels (62.5 ng/ml) that could not be suppressed, with
levels remaining unaltered at 1 and 2 h following a 75 g oral
glucose tolerance test (in a normal response, GH is suppressed to
<1 ng/ml). His IGF-1 level was 467 ng/ml [2.33-fold above the
upper limit of the normal range; reference range (RR), 84-200
ng/ml)] and his HbA1c level was 6.4% (RR, <5.7%). A pituitary
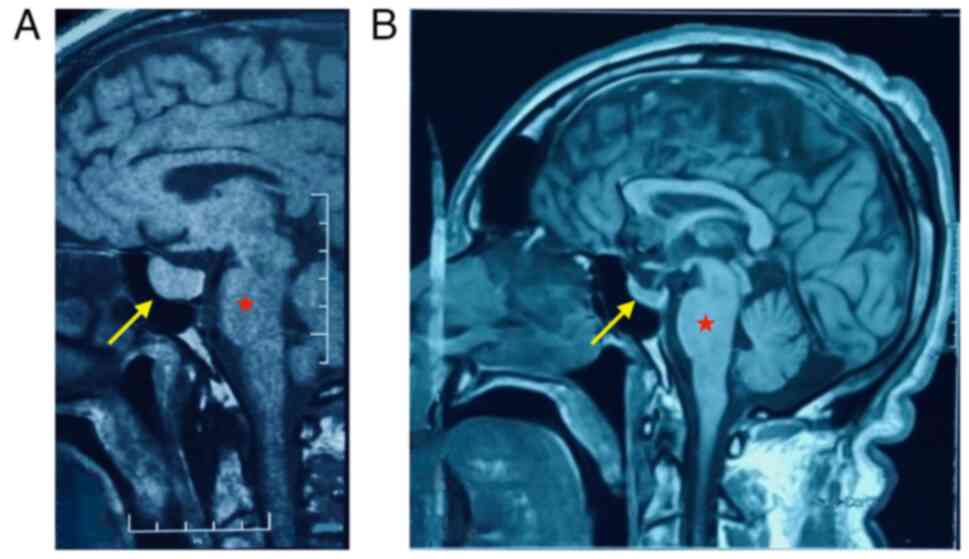
MRI revealed a pituitary macroadenoma measuring 19x17x16 mm on the
right side of anterior pituitary gland (Fig. 1A). Treatment was initiated with a
somatostatin analog (Sandostatin LAR at 30 mg every 4 weeks) and
metformin (750 mg once daily) for uncontrolled blood glucose
levels.
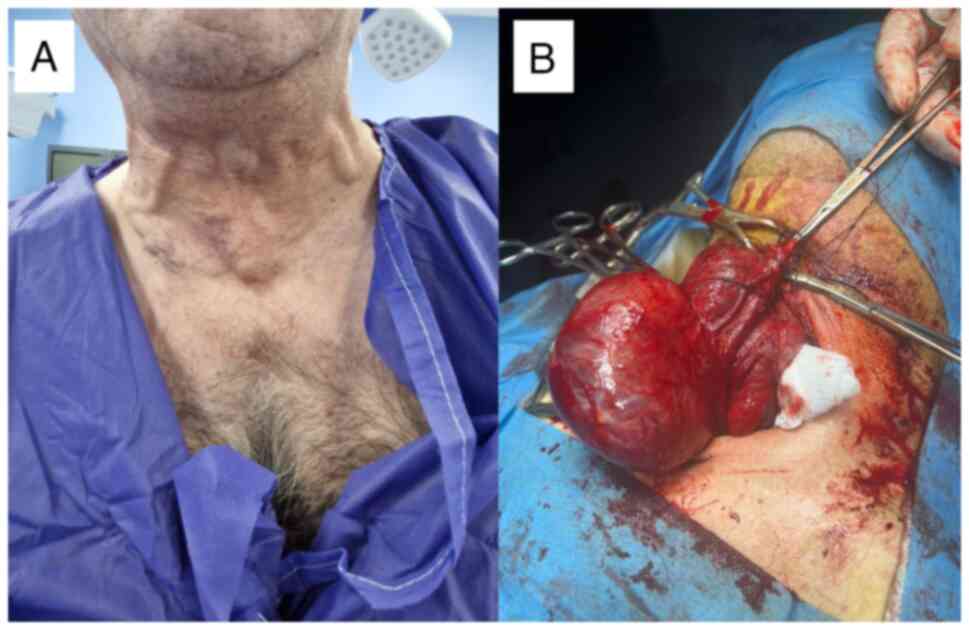
At the age of 49 years, a physical examination
revealed coarse facial features, a prominent nose, interdental
spacing and poor dentition. His thyroid gland was asymmetrically
enlarged, and distended neck veins were noted (Fig. 2A). His extremities revealed large
hands and feet. A laboratory investigation revealed primary
hyperthyroidism with a normal short-Synacthen test result (Table I). However, the short-Synacthen test
may yield false-negative results in the early central adrenal
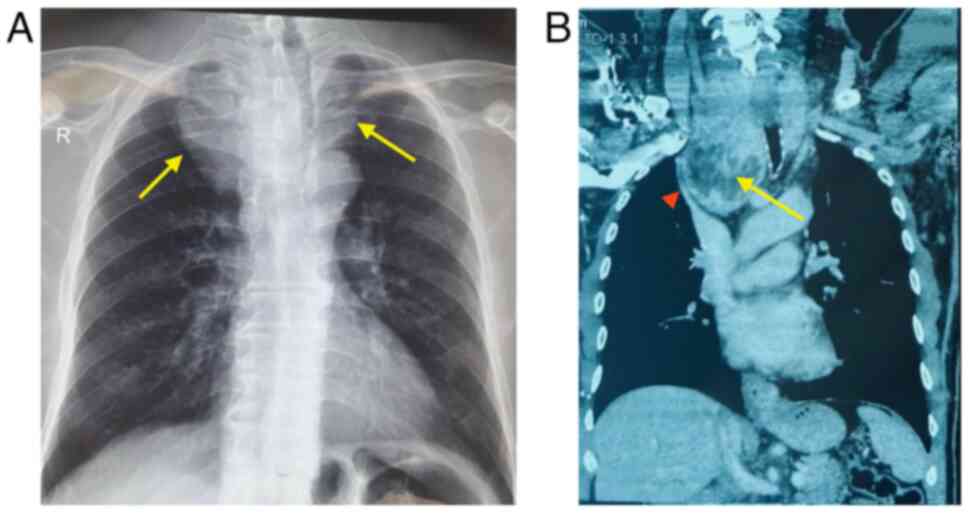
insufficiency. A thyroid ultrasonography revealed an enlarged
thyroid gland with a large nodule in the left lobe (TIRADS 3). Neck
and chest imaging revealed a large thyroid mass extending
retrosternally and compressing the superior vena cava (Fig. 3). An ultrasound-guided fine-needle
aspiration cytology (FNAC) of the thyroid gland confirmed
multinodular goiter (Fig. 4). The
hematoxylin and eosin staining illustrated in Fig. 4 was performed by the Pathology
Laboratory at VIN Specialized Medical Laboratories in Duhok, Iraq.
The patient was commenced on carbimazole therapy at 40 mg daily,
along with propranolol 40 mg daily, to prepare for total
thyroidectomy. Following 4 months of carbimazole dose-adjustments,
his thyroid function test results were normalized
[thyroid-stimulating hormone (TSH), 1.2 µIU/ml; free T4, 12.8
pmol/l)] and he was scheduled for surgery.
 | Table IHormonal profile of the patient prior
to and following thyroidectomy. |
Table I
Hormonal profile of the patient prior
to and following thyroidectomy.
| Hormone | Prior to surgery | Following
surgery | Reference range | Interpretation |
|---|
| GH (ng/ml) | 62.5 | 8.42 | 0.4-10 | Normalized |
| IGF-1 (ng/ml) | 467 (2.33x ULN) | 108 | 84-200 | Normalized |
| Prolactin
(ng/ml) | 13.44 | 12.38 | 4.04-15.2 | Normal |
| TSH (µIU/ml) | <0.005 | 3.02 | 0.27-4.2 | Restored |
| Free T4 (pmol/l) | 54.15 | 20.7 | 12-22 | Normalized |
| LH (mIU/ml) | 3.56 | 3.4 | 1.7-8.6 | Normal |
| FSH (mIU/ml) | 2.4 | 2.9 | 1.5-12.4 | Normal |
| Testosterone
(nmol/l) | 11.9 | 14.6 | 8.64-29 | Normal |
| ACTH (pg/ml) | 42 | 20 | 7.2-63.3 | Normal |
| Cortisola (nmol/l) | 393 → 667 → 675 | 262 → 682 → 679 | Baseline, >180; 30
min and 60 min >500-550 | Normal adrenal
response |
The patient underwent an urgent total thyroidectomy
at the age of 50 years to relieve SVCO. The removed thyroid weighed
260 g, with the right lobe measuring 110x70x50 mm with a 65-mm
spherical nodule, while the left lobe was 60x40 mm (Fig. 2B). The post-thyroidectomy course was
uneventful. Immediately following surgery, the patient reported a
marked improvement in dyspnea, the resolution of orthopnea and an
improved sleep quality, with no acute complications or visual
disturbances following surgery. Over the following months, he noted
an improvement in his mood, energy levels, and a partial reduction
in the size of his hands, feet and facial features. Follow-up
laboratory tests revealed the normalization of thyroid function
(TSH, 3.02 µIU/ml; free T4, 20.7 pmol/l) with appropriate
levothyroxine replacement (75 mcg/day) that required dose
adjustment over the course of 5 months until a stable dose of 125
mcg/day. Notably, his IGF-1 levels gradually declined and
normalized (84 ng/ml) within 6 months post-thyroidectomy. An MRI of
the pituitary revealed a marked shrinkage in the size of the
pituitary adenoma, which decreased from 19x17x16 mm prior to the
thyroidectomy (Fig. 1A) to 14x11x9
mm at 5 months post-thyroidectomy, and further to 8x6x5.5 mm at 12
months post-thyroidectomy (Fig. 1B).
At the 18-month follow-up, the patient remained asymptomatic, with
well-controlled diabetes (HbA1c 4.7%) on metformin (750 mg once
daily), and stable thyroid and pituitary function on levothyroxine
and somatostatin analog therapy (Table
I). He continues follow-up with an endocrinologist; no
neurosurgical intervention has been required and the planned
transsphenoidal resection of the pituitary adenoma was
cancelled.
Discussion
The present case report illustrates the rare
coexistence of acromegaly due to a GH-secreting pituitary adenoma
with toxic multinodular goiter causing SVCO. Although thyroid
nodular disease is common among patients with acromegaly, the
development of thyrotoxicosis complicated by vascular compression
is unusual (8). The most notable
feature of the case presented herein was the unexpected regression
of the pituitary adenoma following thyroidectomy.
The regression of pituitary adenomas, particularly
GH-secreting tumors, is rare and typically attributed to ischemic
infarction or pituitary apoplexy (7). In the patient in the present study, a
single or a combination of mechanisms may explain the observed
regression. The first possibility is the spontaneous, natural
shrinkage of a macroadenoma, which has been described in large
tumors with limited vascular supply (9). The second mechanism is pituitary
apoplexy induced by sudden perioperative hemodynamic fluctuations,
as the vasculature of pituitary adenomas is fragile and susceptible
to ischemic or hemorrhagic events (9). A third contributing factor may be
elevated levels of thyroid hormones, which enhance GH/IGF-1
secretion and metabolic activity, potentially exacerbating
acromegaly severity, with resolution following thyroidectomy
supporting this hypothesis (10).
The last and most intriguing hypothesis is that the massive
multinodular goiter may have compromised carotid circulation and
hypophyseal arteries supplying the pituitary gland, with surgical
removal altering vascular dynamics and precipitating ischemic
changes within the adenoma. While this mechanism has not
specifically been discussed in the literature, large goiters with
carotid compression are known to cause ischemic stroke in rare
circumstances (11).
The regression of symptoms of acromegaly and the
normalization of IGF-1 levels following thyroidectomy support the
hypothesis of treatment-tumor infarction rather than spontaneous
shrinkage. The biochemical normalization may also be attributed to
somatostatin analogue. If the patient had been subjected directly
to transsphenoidal surgery, the patient may have undergone an
unnecessary invasive procedure. Instead, the improvement following
thyroidectomy highlights how endocrine and vascular interactions
can influence tumor biology. An Italian multicenter study revealed
that in patients with acromegaly, non-toxic nodular goiter was
found in 40% of cases, while toxic nodular goiter was found in
13.4% of cases (8). A previous case
report described the anesthetic challenges encountered in patients
with acromegaly when thyroid disease compromises the airway
(12). Another case report
highlighted the occurrence of acromegaly with multinodular goiter
in a patient with McCune-Albright syndrome, where there was
spontaneous normalization of thyroid function and reduction of
pituitary tumor size with somatostatin analog therapy (13). A different case report documented the
spontaneous shrinkage of a pituitary adenoma in a patient with
hypothyroidism, with the authors of that study proposing the cause
to be autoimmune lymphocytic hypophysitis (14). No prior studies have documented the
shrinkage of GH-secreting tumors following thyroidectomy.
In conclusion, the present case report describes a
rare instance of acromegaly due to a GH-secreting pituitary adenoma
coexisting with toxic multinodular goiter complicated by SVCO.
Following urgent thyroidectomy, the patient experienced clinical
and biochemical improvement with the regression of symptoms of
acromegaly, the normalization of IGF-1 levels and the radiological
shrinkage of the adenoma, without the need for neurosurgical
intervention. The present case report highlights the potential role
of vascular mechanisms in pituitary tumor biology and emphasizes
the importance of carefully reassessing of pituitary lesions before
proceeding with definitive surgical management.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
BAQ evaluated the patient's history and performed
the laboratory tests. HJA was involved in the conception and design
of the case study, and also prepared the article and conducted the
literature review. SHA and AYI evaluated the laboratory test
results of the patient and performed surgery on the patient. RSAK
obtained medical images, analyzed the patient's data, and revised
and edited the manuscript. BAQ and RSAK confirm the authenticity of
all the raw data. All the authors have accepted responsibility for
the entire content of this manuscript and have read and approved
the final manuscript.
Ethics approval and consent to
participate
The present report was carried out in accordance
with the Declaration of Helsinki. The patient provided written
consent for the description of the present case.
Patient consent for publication
The patient described in the present case report
provided written consent for the publication of the present case
report and related images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Fleseriu M, Langlois F, Lim DST, Varlamov
EV and Melmed S: Acromegaly: Pathogenesis, diagnosis, and
management. Lancet Diabetes Endocrinol. 10:804–826. 2022.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Qasim BA: Historical Landmarks in
Endocrinology and Diabetes: The Fascinating World of Hormones.
Cambridge Scholars Publishing, Newcastle upon Tyne, 2024.
|
|
3
|
Lugo G, Pena L and Cordido F: Clinical
manifestations and diagnosis of acromegaly. Int J Endocrinol.
2012(540398)2012.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Hong S, Han K and Park CY: Long-term
prognosis and systemic impact of acromegaly: Analyses utilizing
korean national health insurance data. Endocrinol Metab (Seoul).
40:1–9. 2025.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Ershadinia N and Tritos NA: Diagnosis and
treatment of acromegaly: An update. Mayo Clin Proc. 97:333–346.
2022.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Ghalaenovi H, Azar M and Fattahi A:
Spontaneous regression of nonfunctioning pituitary adenoma. Br J
Neurosurg. 37:769–770. 2023.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Alam S, Kubihal S, Goyal A and Jyotsna VP:
Spontaneous remission of acromegaly after pituitary apoplexy in a
middle-aged male. Ochsner J. 21:194–199. 2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gasperi M, Martino E, Manetti L, Arosio M,
Porretti S, Faglia G, Mariotti S, Colao AM, Lombardi G, Baldelli R,
et al: Prevalence of thyroid diseases in patients with acromegaly:
Results of an Italian multi-center study. J Endocrinol Invest.
25:240–245. 2002.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Muthukumar N: Pituitary apoplexy: A
comprehensive review. Neurol India. 68 (Suppl 1):S72–S78.
2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Mo C, Tong T, Guo Y, Li Z and Zhong L:
Growth hormone-secreting pituitary adenoma combined with Graves'
disease: Retrospective case series and literature review. Endocr
Connect. 13(e230439)2024.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Camacho Y, Jamal Y, Wang A, Chiarolanzio P
and Goswami G: Ischemic stroke: A rare complication of a large
multinodular goiter. Endocrinol Diabetes Metab Case Rep: Jun 1,
2022 (Epub ahead of print).
|
|
12
|
Jamil J, Wan Hassan WMN, Ghani AR and Yeap
TB: Anaesthetic challenges in a patient with acromegaly and
multinodular goitre undergoing endoscopic pituitary surgery. BMJ
Case Rep. 16(e250640)2023.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Abs R, Beckers A, Van de Vyver FL, De
Schepper A, Stevenaert A and Hennen G: Acromegaly, multinodular
goiter and silent polyostotic fibrous dysplasia. A variant of the
McCune-Albright syndrome. J Endocrinol Invest. 13:671–675.
1990.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Jaafar AS, Mohd Shokri SS, Paramasvaran S,
Palaniandy K and Fadzil F: Now you see, now you don't: A case of
spontaneous regression of pituitary tumour. Cureus.
12(e9174)2020.PubMed/NCBI View Article : Google Scholar
|















![Fine-needle aspiration cytology smears
from a 51-year-old male with retrosternal goiter illustrating (A
and B) groups of follicular epithelial cell in a colloid-rich
background [H&E staining; magnification: (A) x5, (B) x20] with
(C) scattered hemosiderin-laden macrophages (H&E staining;
magnification x20). Cytomorphological features are consistent with
a benign thyroid lesion (Thy 2).](/article_images/mi/6/1/mi-06-01-00286-g03.jpg)