Introduction
First described by John Fothergill in 1773,
trigeminal neuralgia (TN) is the most common cranial neuralgia
(1,2). The incidence of TN in China has been
reported to be 182.8/100,000, with a predilection age of 37–67
years and a ratio of 1:3 for males and females. Classical
trigeminal neuralgia (CTN) is described by electrical pain
sensations not due to intracranial tumors or bone compression in
the area where one or more branches of the facial nerve distribute.
Pain typically manifests briefly, lasting only a few sec, and
patients do not complain of obvious discomfort between episodes.
Patients primarily report a fixed pain trigger point at the mouth
or nasal wing as well as alleviation or control of pain by oral
medication (3).
Multiple theories concerning the etiology of CTN
have been suggested, including increased excitability of sensory
neurons and abnormal action potentials as a result of neuronal
damage (4). Abnormal action
potentials or external stimulation excite adjacent resting neurons
through direct interneuronal connections, producing abnormally
synchronized discharges and resulting in pain. Another theory holds
that root exit zone compression caused by local axonal
demyelination allows exposed nerve fibers to come into contact,
thus producing abnormal conduction. Transmission of minor stimuli
elicits efferent central nervous system impulses, which change into
afferent impulses via such contact. Such signaling eventually
results in pain (5). To date,
however, little is known about the pathogenesis of CTN despite its
wide prevalence and considerable healthcare burden. However,
increasing evidence has suggested that cerebral abnormalities are
closely related to pain (6). A
prior study which detected brain activity when using an estrogenic
stimulation in CTN patients reported that their gray matter in the
bilateral superior/middle temporal gyrus, thalamus, putamen,
caudate nucleus, forebrain and hindbrain, as well as the primary
somatosensory cortex significantly differed from healthy controls
(7).
Few studies to date have explored altered brain
activity in CTN patients. The aim of the present study was to
investigate whether changes in neuronal activity of related brain
regions can be considered as a therapeutic target which could help
patients alleviate pain and improve their quality of life.
Functional magnetic resonance imaging (fMRI),
offering such advantages as convenience and noninvasiveness, is
widely used for studying brain functions (8). Based on cerebral blood flow and
metabolic analysis, researchers can evaluate specific brain
activity and explore brain structure, elucidating how the brain of
CTN patients is affected by this condition (9). The active state-MRI captures the
brain activity of subjects when they are performing specific tasks,
which has the advantage of directly observing which brain regions
are activated during tasking state and enabling more direct
comparison with psychological behavioral studies. In addition, it
highlights the importance of the relationship between tasks and
activated brain regions (10).
However, this model is greatly influenced by the experimental
design and it is also difficult to control the baseline level.
Furthermore, the subjects need a strong psychological background.
Since certain subjects cannot finish the task or short task time,
this pattern has poor clinical practicability (11). Resting-state functional magnetic
resonance imaging (RS-fMRI) has attracted wide attention in the
field of neuroimaging and is suitable for the study of the central
mechanism. It also has become a useful tool for the study of
functional connections in the human brain (12). RS-fMRI is considered to be the
circuit that forms the information processing and physiological
basis of psychological representation (13). It captures the brain activity of
subjects when they remain at rest without any other activity, which
has the advantage of directly observing the spontaneous
neurological brain activity of subjects. It is closer to the
physiological state and highlights the importance of the
parallelism of human brain neural networks and the interrelation
between different brain regions (14). In addition, the resting state can
last longer which leaves enough time to collect data. Moreover,
this pattern also has the advantage of simple design and easy
baseline control. However, the RS-MRI method can be influenced by a
variety of physiological noises such as the beating heart and
breathing as well as other noises (15).
Amplitude of low-frequency fluctuation (ALFF), a
type of resting state fMRI, can be applied to evaluate intrinsic
fluctuations of bold signals to reveal local spontaneous static
state brain activity (16).
Previous studies have demonstrated that ALFF exhibited good to
moderate test-retest reliability (17,18).
The simple calculation and reliable characterization of the ALFF
measurement makes it a suitable and useful tool for resting-state
fMRI data analysis in order to investigate a disease trait.
Furthermore, it has been demonstrated to be a valuable parameter to
reflect the intensity of spontaneous nerve activity (19). In our previous studies, the ALFF
method was successfully used to evaluate certain eye diseases
(20,21).
The present study, demonstrated that CTN patients
had dysfunction of brain activities. These findings may provide
important information to explain the underlying neural mechanisms
of CTN, which are beneficial to clinical diagnosis. Based on fMRI
and ALFF findings, our aim was to explore the local features of
spontaneous brain activity in patients with CTN and the
relationship between ALFF with the clinical manifestations, thus
possibly helping to elucidate the underlying pathological
mechanisms involved in CTN and agreed to publish their brain scan
images.
Materials and methods
Subjects
The study recruited 28 patients with TN (male, n=12;
female, n=16) from the First Affiliated Hospital of Nanchang
University. Inclusion criteria were: i) Unilateral pain involving
at least one of either the maxillary (V2) or mandibular (V3)
branches of the trigeminal nerve; ii) intense, sharp, burning or
stabbing paroxysmal facial pain precipitated by trigger factors or
zones; iii) conventional MRI T1WI, T2WI sequence examination
revealing no evident abnormal brain signals; iv) no clinically
evident neurological or sensory dysfunction attributed to other
conditions; v) no previous surgical or other invasive treatments
for TN; and vi) no contraindications to magnetic resonance
scanning. Exclusion criteria were: i) headaches, or other
paroxysmal or chronic pain conditions; ii) patient family history
of headache or other pain in first degree relatives; iii) other
somatic or psychiatric conditions; and iv) contraindications to
magnetic resonance scanning. The study was approved by the Ethics
Committee of the First Affiliated Hospital of Nanchang University
(no. CDYFY-E-160802), Jiangxi, China.
A total of 28 healthy controls (HCs; male, n=12;
female, n=16) matched for age, sex and economic status were also
recruited. All subjects were right-handed. The ages of patients and
healthy controls were 51.392±9.372 and 51.357±9.302 years,
respectively. The range of CTN episode duration was 3.73±4.10 years
and visual analogue scale (VAS) scores ranged from 6.32±1.44
(Table I). Inclusion criteria
were: i) No TN symptoms; ii) no diagnosed organic conditions
including chronic pain; iii) not suffering from neurological or
psychiatric disorders; and iv) no contraindications to magnetic
resonance imaging (MRI) scanning.
 | Table I.Demographics and behavioral results
of CTN and HC groups (22). |
Table I.
Demographics and behavioral results
of CTN and HC groups (22).
|
| CTN | HC | T-value | P-value |
|---|
| Male/female | 12/16 | 12/16 | N/A | >0.99 |
| Age (years) | 51.392±9.372 | 51.357±9.302 | 0.297 | 0.769 |
| Handedness | 28 R | 28 R | N/A | >0.99 |
| Duration
(years) | 3.733±4.102 | N/A | N/A | N/A |
| VAS | 6.321±1.442 | N/A | N/A | N/A |
The present study was approved by the Medical
Research Ethics Committee of The First Affiliated Hospital of
Nanchang University. All individuals provided signed informed
consent to participate in the study.
Pain evaluation
Pain in TN patients was assessed using the VAS.
Researchers guided patients in rating their pain on a scale of 0–10
using a 10-cm ruler. A higher score indicated greater pain
intensity. A rating of ‘0’ represented no pain, and a ‘10’ meant
intolerable pain.
MRI parameters
For the MRI scan, a Trio 3.0T MRI machine (Siemens
AG) was used for scanning. All participants were instructed to
close their eyes, stay awake, and breathe quietly until the scan
was completed. 3D damage-gradient echo sequences to collect
functional data were used; parameters were as follows: 176
structural images (repetition time=1,900 msec; echo time=2.26 msec;
thickness=1 mm; gap=0.5 mm; acquisition matrix=256×256; field of
view=250×250 mm; turning angle=9 degrees), and 240 functional
images (repeat time=2,000 msec; echo time=30 msec; thickness=4 mm;
gap=1.2 mm; acquisition matrix=64×64; turning angle=90 degrees;
field of view=220×220 mm, 29 axial). Each scanning process lasted
15 min.
fMRI data processing
To process fMRI images, MRIcro software (https://www.mccauslandcenter.sc.edu/crnl/mricro) was
used to classify functional data and exclude incomplete data. The
first fifteen time-points were discarded to maintain magnetization
equilibrium. Data Processing Assistant for Advanced Edition of
Resting-State fMRI (DPARSF 4.0; http://rfmri.org/DPARSF) software was used for head
motion correction, spatial normalization, slice timing, form
conversion of digital imaging communications in medicine (DICM),
and full-width smoothing with a Gaussian kernel of 6×6×6
mm3 at half-maximum based on the rs-fMRI data analysis
toolkit (REST; http://www.restfmri.net) and the Statistical
Parametric Mapping software (version 8; http://www.fil.ion.ucl.ac.uk/spm). Subjects were
excluded if 1.5 angular motion or an offset exceeding 1.5 mm in
either x, y, or z axes were detected during imaging. Friston
six-head motion parameters (23)
were used to negate any influence of head motion. After correction
for head motion, obtained functional images were standardized using
a standard echo plane image template, conforming to standards set
forth by the Montreal Neurological Institute (MNI).
ALFF processing
First, to calculate ALFF, remaining data were
smoothed with a full-width Gaussian kernel of 6×6×6 mm3
at half-maximum. Next, fMRI images were detrended and
bandpass-filtered (0.01–0.08 Hz) to reduce effects of low-frequency
drift and physiological high-frequency respiratory and cardiac
noise. Then, the smoothed signals of each voxel were converted from
time to frequency domains using the fast Fourier transform (FFT)
algorithm and obtained the power spectrum. Finally, all ALFF maps
were divided by the mean value of each ALFF map.
Brain-behavior correlation
analysis
For the purposes of brain-behavior correlation
analysis, areas with significant ALFF changes were selected as
regions of interest (ROIs). Each ROI was calculated by finding each
original ALFF value corresponding to each of the original voxels.
Correlations among ALFF signals of distinct regions within the
cerebrum and clinical manifestations of CTN patients were evaluated
using Pearson's correlation analysis.
Data processing
Demographic and clinical variables of CTN and HC
groups were statistically analyzed using SPSS 20.0 software (IBM
Corp.) and applying an independent sample t-test; P<0.05 was
considered to indicate a statistically significant difference.
Voxel differences between CTN and HC subjects were studied using
REST software and a two-sample t-test. By applying the Gaussian
random field theory, the statistical voxel threshold of multiple
comparisons was set to P<0.05. Calibration was carried out under
the condition of a voxel level of P<0.01 and a cluster size
>40 voxels. Mean ALFF values in different brain regions were
classified by a receiver operating characteristic (ROC) curve.
Pearson correlation coefficient was conducted to assess the
relationships between the ALFF values of different brain regions
and clinical variables (VAS scores and duration of disease) in CTN
using SPSS version 20.0 software.
Results
Differences of ALFF
Compared to HCs, CTN patients had significantly
higher ALLF values in the right inferior cerebellum (RIC), left
fusiform gyrus (LFG), left inferior cerebellum (LIC), left inferior
temporal gyrus (LITG), right fusiform gyrus (RFG), right superior
cerebellum (RSC), left inferior occipital gyrus (LIOG), right
precentral gyrus (RPG) and right superior occipital gyrus (RSOG),
as revealed in Fig. 1 (red) and
Table I. The voxel level
statistical threshold for multiple comparisons using the Gaussian
random field theory was set at a level of P<0.05. Data was
corrected to >40 voxel clusters. The histogram in Fig. 2 details mean altered ALFF values of
both groups. No correlation was noted between mean ALFF values of
relevant brain regions and clinical manifestations in CTN subjects
(P>0.05).
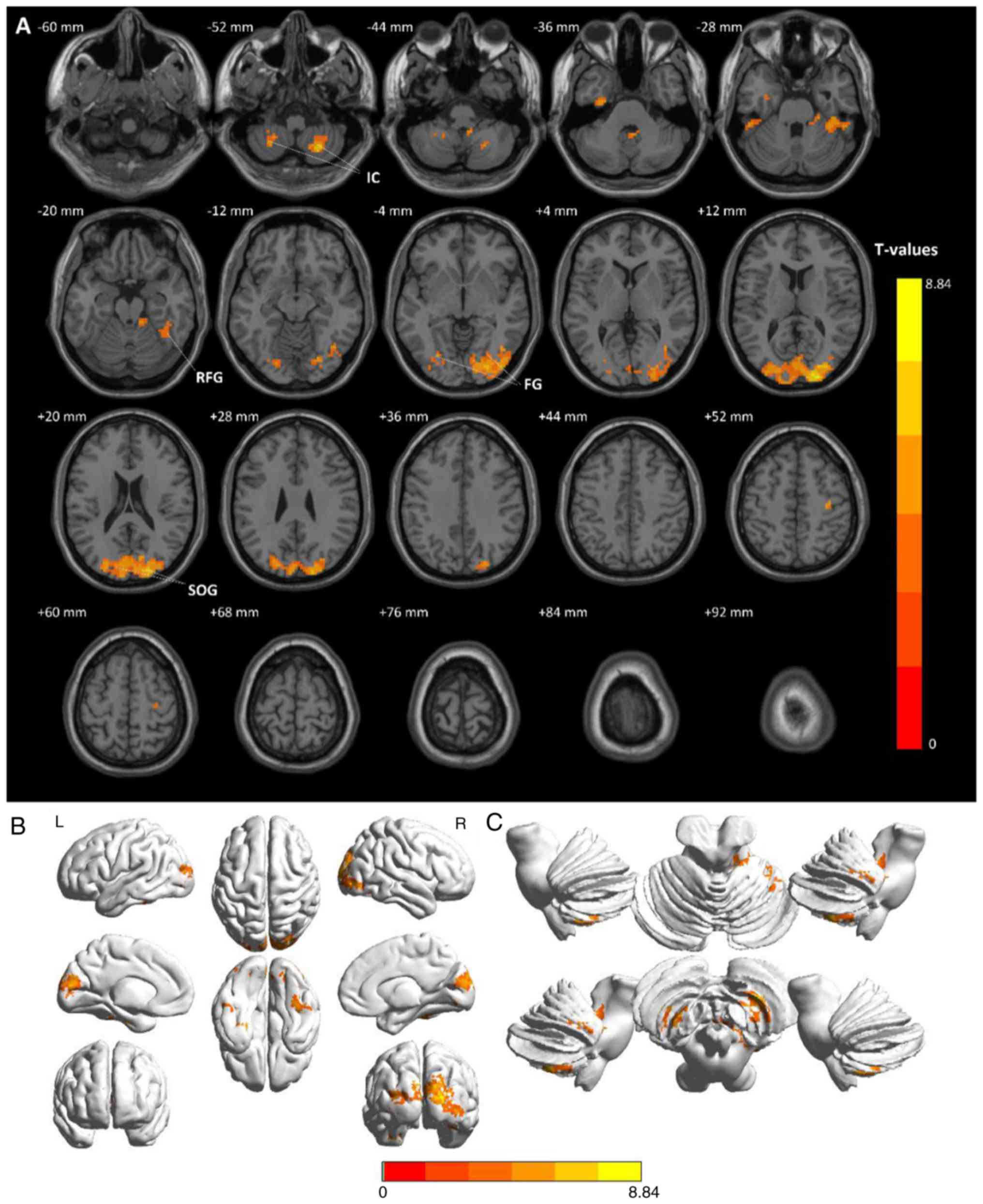
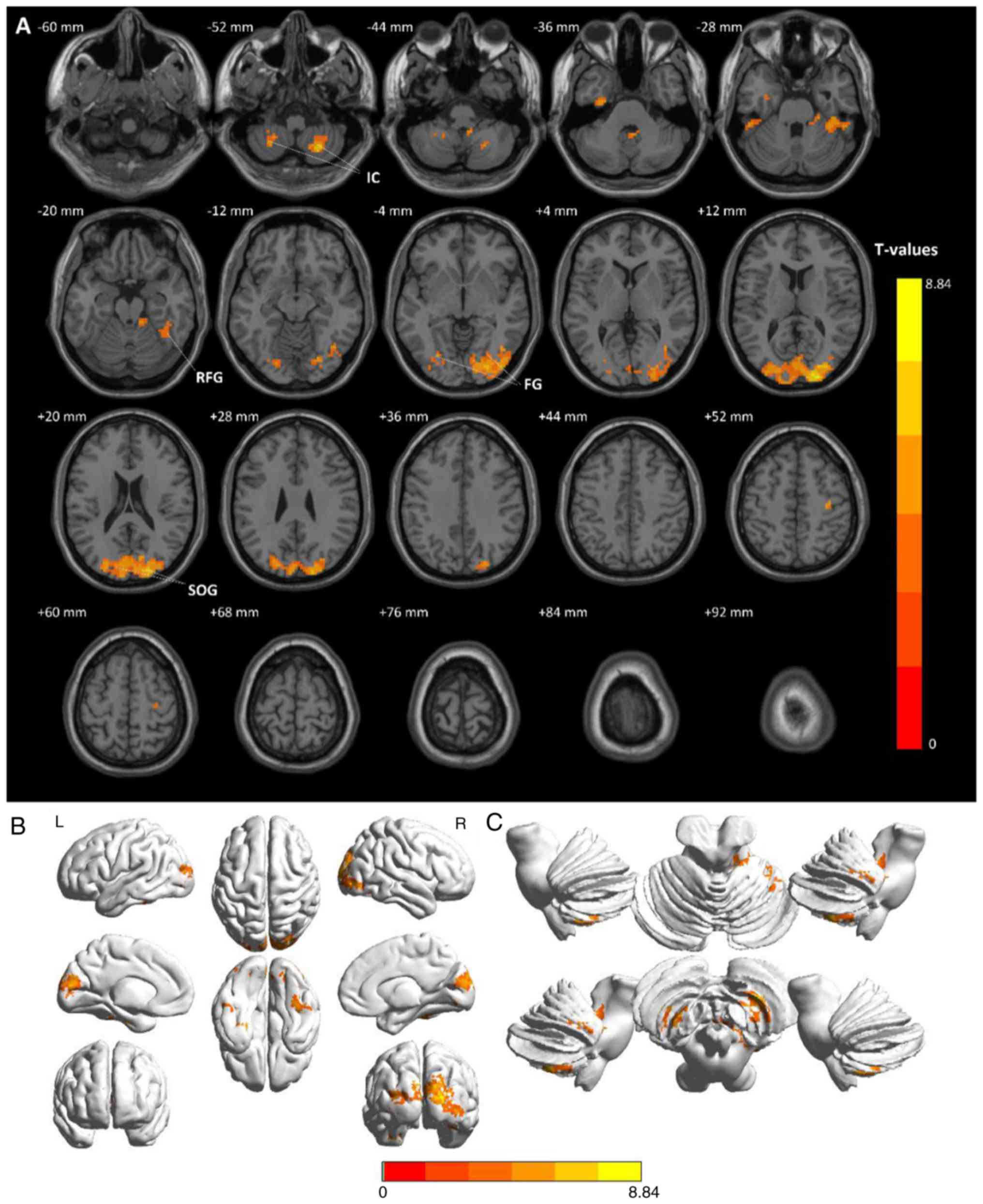 | Figure 1.Comparison of average ALFF values
between the patients with CTN and HCs. (A) Significant differences
in mean ALFF values between CTNs and HCs were recognized in the
bilateral IC, bilateral FG and SOG. The red or yellow regions
indicate higher ALFF values (P<0.01 for multiple comparisons
using the Gaussian random field theory, z>2.3, P<0.01,
cluster >40 voxels, AlphaSim corrected). (B) Stereoscopic form
of the cerebrum. (C) Stereoscopic form of the cerebellum and the
brain stem. CTN, classical trigeminal neuralgia; HCs, healthy
control groups; IC, inferior cerebellum; FG, fusiform gyrus; SOG,
superior occipital gyrus; ALFF, amplitude of low frequency
fluctuation. |
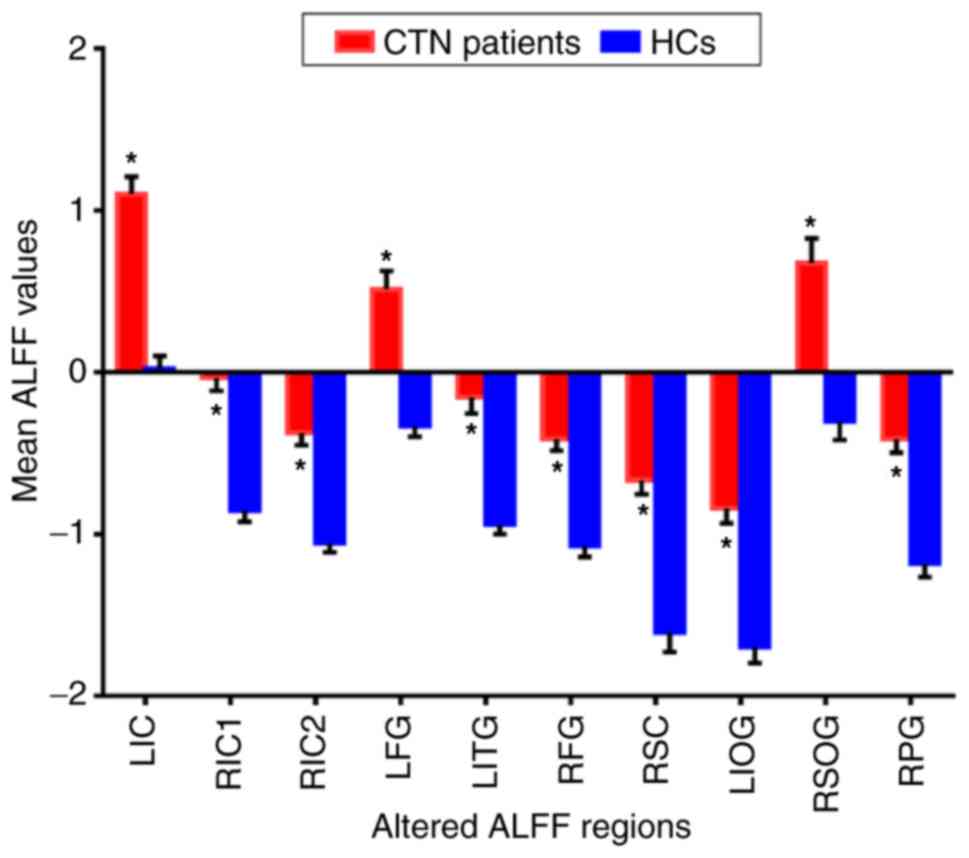
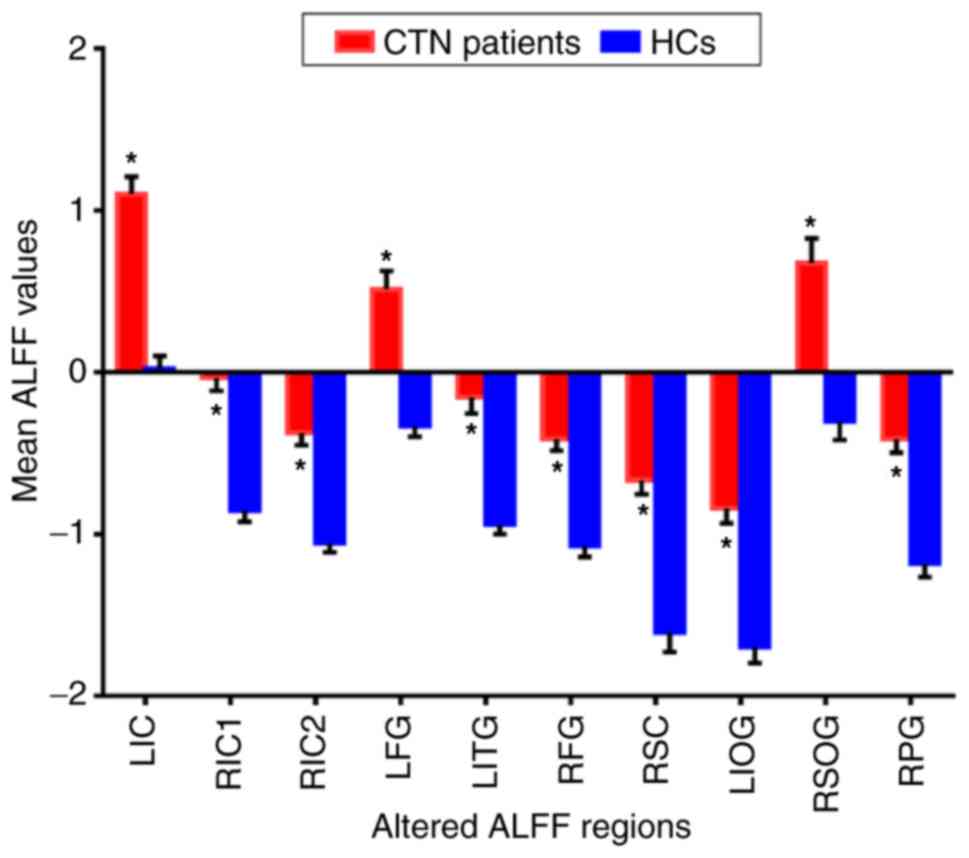 | Figure 2.The mean altered ALFF values between
CTN and HCs. Compared with the HCs, the ALFF of the following
regions were increased to various extents: LIC (t=5.3163); RIC1
(t=5.3491); RIC2 (t=6.6204); LFG (t=6.0603); LITG (t=4.9039); RFG
(t=5.8291); RSC (t=5.9398); LIOG (t=5.3456); RSOG (t=8.8391); RPG
(t=5.7781) in CTN patients. *P<0.05 vs. HCs. Data are presented
as the mean ± standard deviation. ALFF, amplitude of low-frequency
fluctuation; CTN, classical trigeminal neuralgia; HCs, healthy
control groups; LIC, left inferior cerebellum; RIC1, right inferior
cerebellum 1; RIC2, right inferior cerebellum 2; LFG, left fusiform
gyrus; LITG, left inferior temporal gyrus; RFG, right fusiform
gyrus; RSC, right superior cerebellum; LIOG, left inferior
occipital gyrus; RSOG, right superior occipital gyrus; RPG, right
precentral gyrus. |
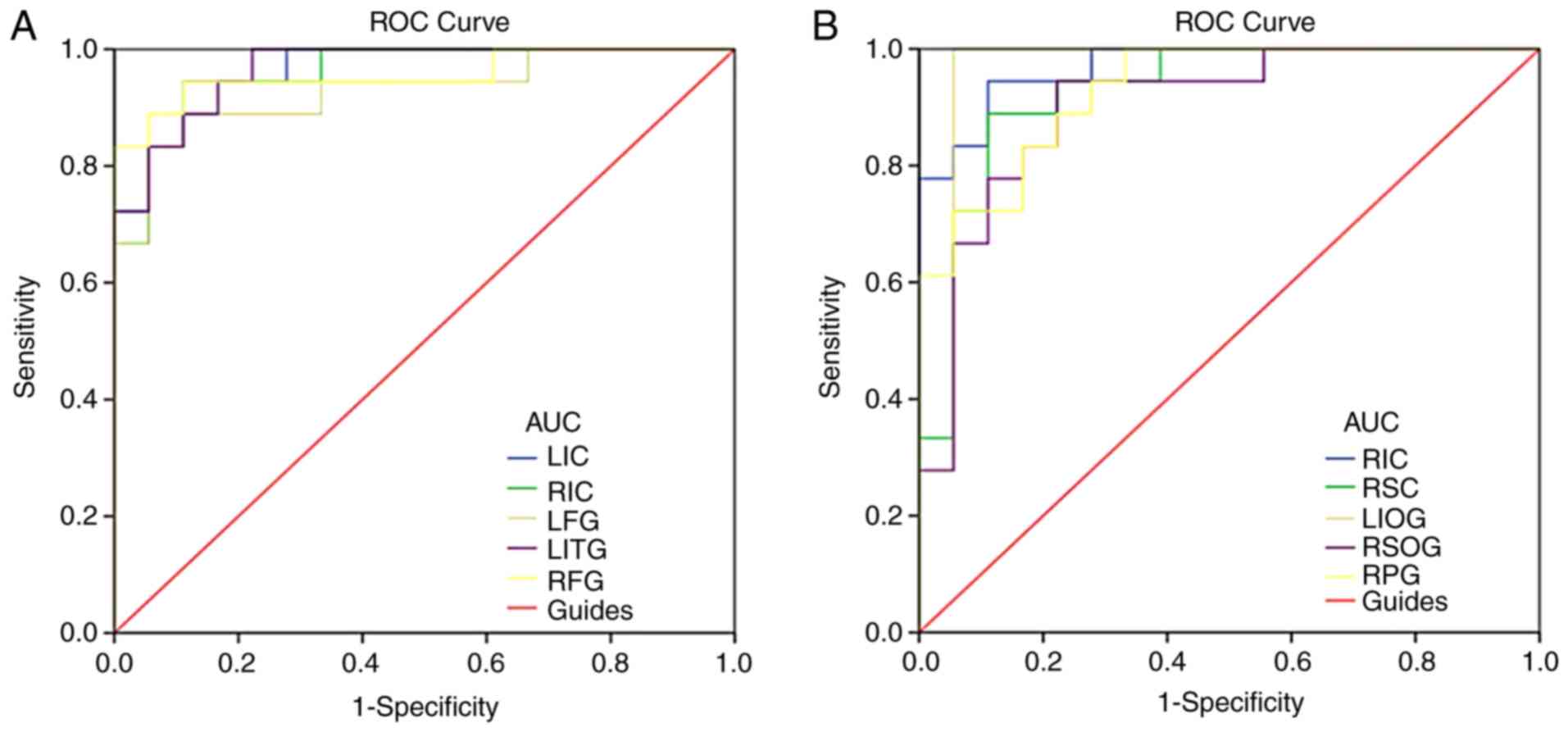
ROC curve
Brain region ALFF values differed between CTN and HC
subjects and were thus recognized as differentiating markers. Areas
under the curve were as follows and are detailed in Fig. 3: LIC (0.966), RIC (0.957), LFG
(0.929), LITG (0.966), RFG (0.957) (Fig. 3A); RIC (0.969), RSC (0.926), LIOG
(0.960), RSOG (0.901), and RPG (0.929) (Fig. 3B).
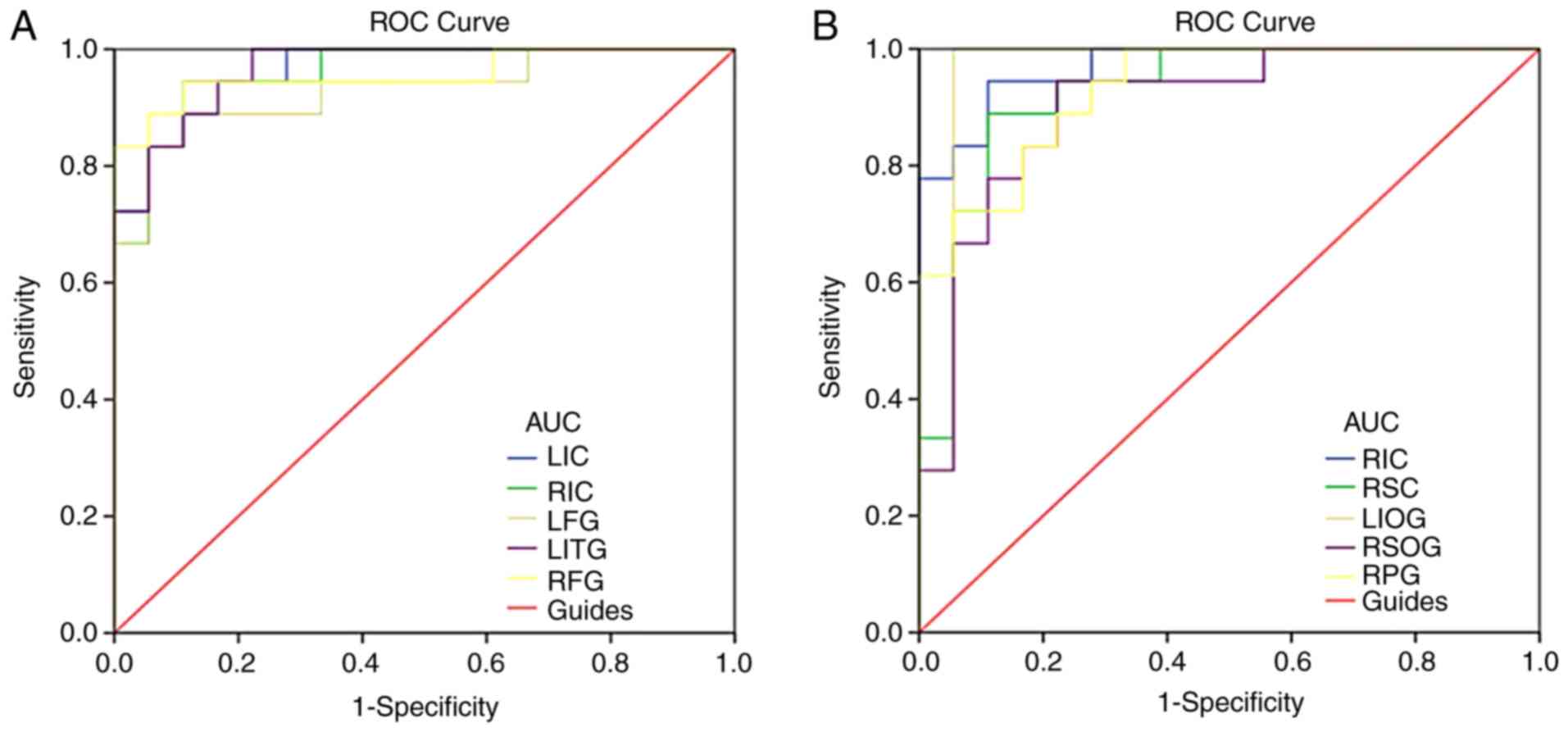 | Figure 3.ROC curve analysis of the mean ALFF
values for altered brain regions. (A) The area under the ROC curve
was 0.966, (P<0.001; 95% CI: 0.917–1.000) for LIC; 0.957
(P<0.001; 95% CI: 0.899–1.000) for RIC; 0.929 (P<0.001; 95%
CI: 0.842–1.000) for LFG; 0.966 (P<0.001; 95% CI: 0.918–1.000)
for LITG; 0.957 (P<0.001; 95% CI: 0.887–1.000) for RFG. (B) The
area under the ROC curve was 0.969 (P<0.001; 95% CI:
0.923–1.000) for RIC; 0.926 (P<0.001; 95% CI: 0.838–1.000) for
RSC; 0.960 (P<0.001; 95% CI: 0.882–1.000) for LIOG; 0.901
(P<0.001; 95% CI: 0.798–1.000) for RSOG; 0.929 (P<0.001; 95%
CI: 0.851–1.000) for RPG. ALFF, amplitude of low-frequency
fluctuation; ROC, receiver operating characteristic; CTN, classical
trigeminal neuralgia; HC, healthy control; LIC, left inferior
cerebellum; RIC, right inferior cerebellum; LFG, left fusiform
gyrus; LITG, left inferior temporal gyrus; RFG, right fusiform
gyrus; RSC, right superior cerebellum; LIOG, left inferior
occipital gyrus; RSOG, right superior occipital gyrus; RPG, right
precentral gyrus. |
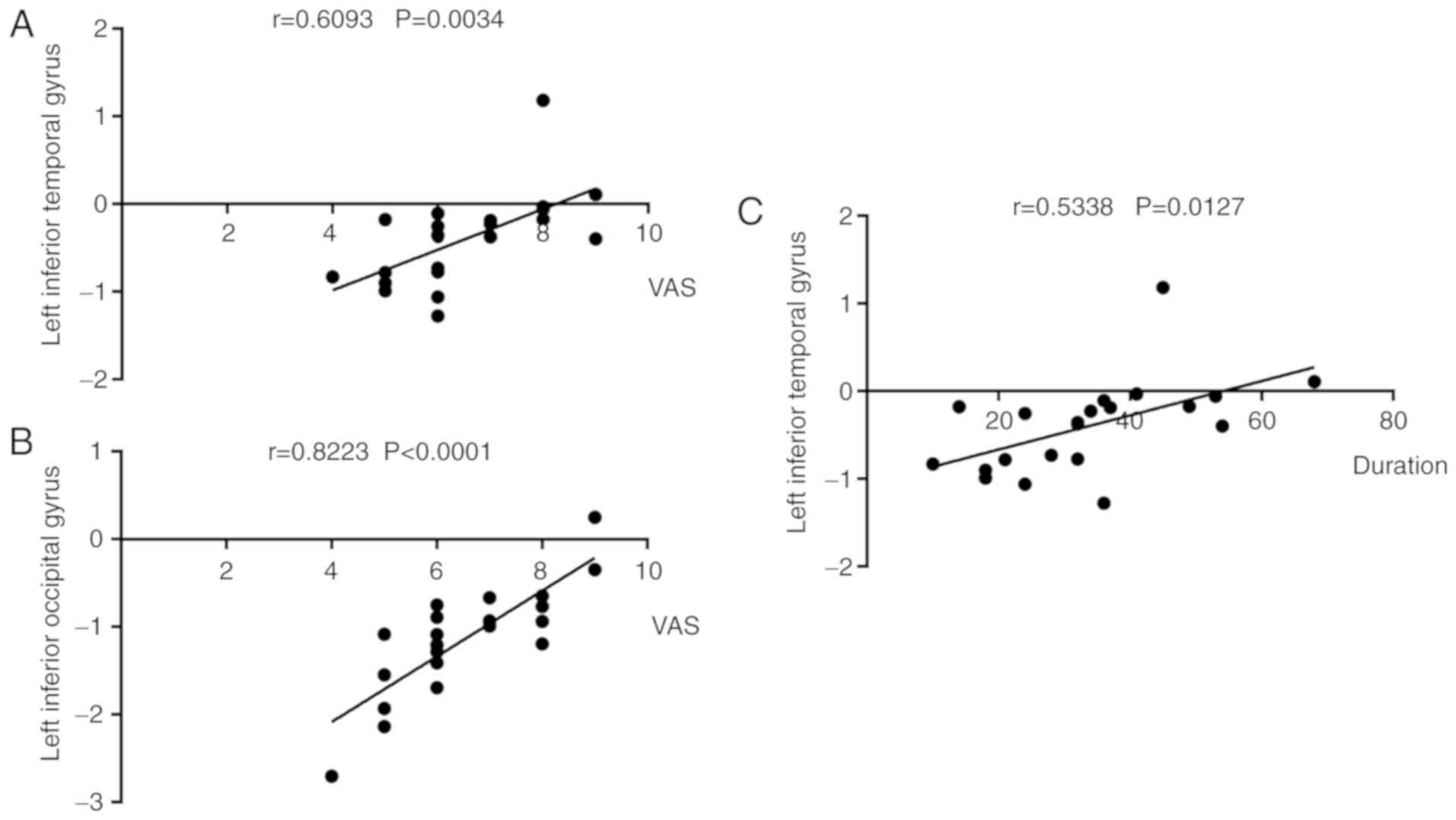
Correlation analysis
Left eye VAS findings were positively correlated
with left inferior temporal gyral ALFF signal values in CTN
patients (r=0.609, P=0.003; Fig.
4A). Likewise, left eye VAS findings was also positively
correlated with left inferior temporal gyral values (r=0.534,
P=0.013; Fig. 4C). Right eye pain
duration positively was correlated with left inferior occipital
gyral values (r=0.822, P<0.0001; Fig. 4B).
Discussion
ALFF has been successfully applied to the study of a
variety of pain-causing conditions (24–29)
(Table II) and holds great
promise in future research. In the present study, for the first
time we studied altered spontaneous brain activity in CTN patients
using the ALFF method. ReHo was used to study patients with TN in
our previous study (23). Both
ReHo and ALFF can be used to study spontaneous brain activity
through BOLD signals. ALFF exhibit fluctuation amplitude of time
course while ReHo describes local synchronization of neighboring
voxels. Therefore, the results obtained by the two methods will be
different. Both of them provide complementary information about the
regional spontaneous brain activity in CTN patients. No other
interventions were imposed and only altered spontaneous brain
activity in the resting state was detected in CTN patients compared
with healthy controls in the present study. LIC, RIC, LFG, RFG,
RPG, LITG, RSC, LIOG and RSOG ALFF values were significantly higher
in CTN patients when compared to HCs (Table III; Fig. 5).
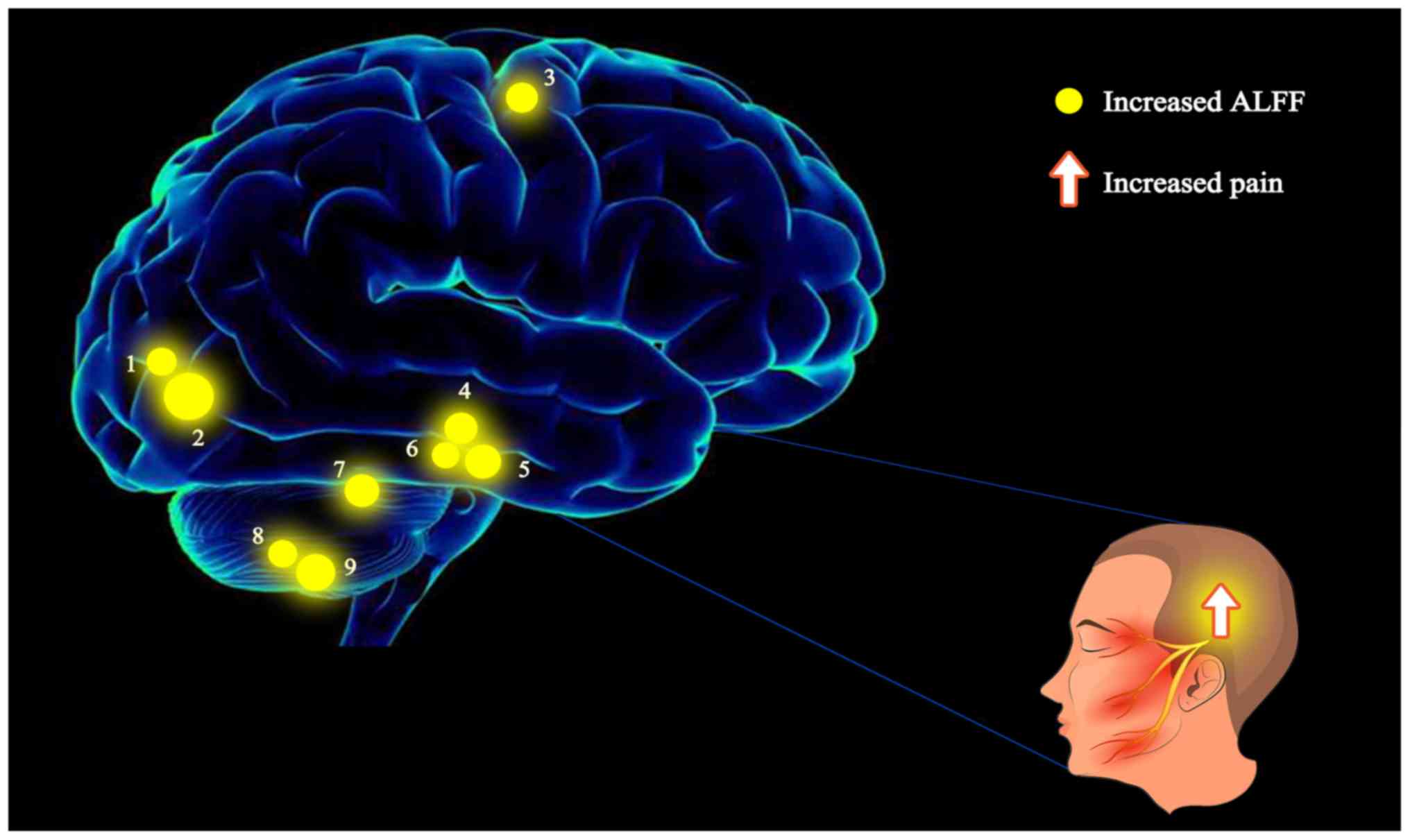
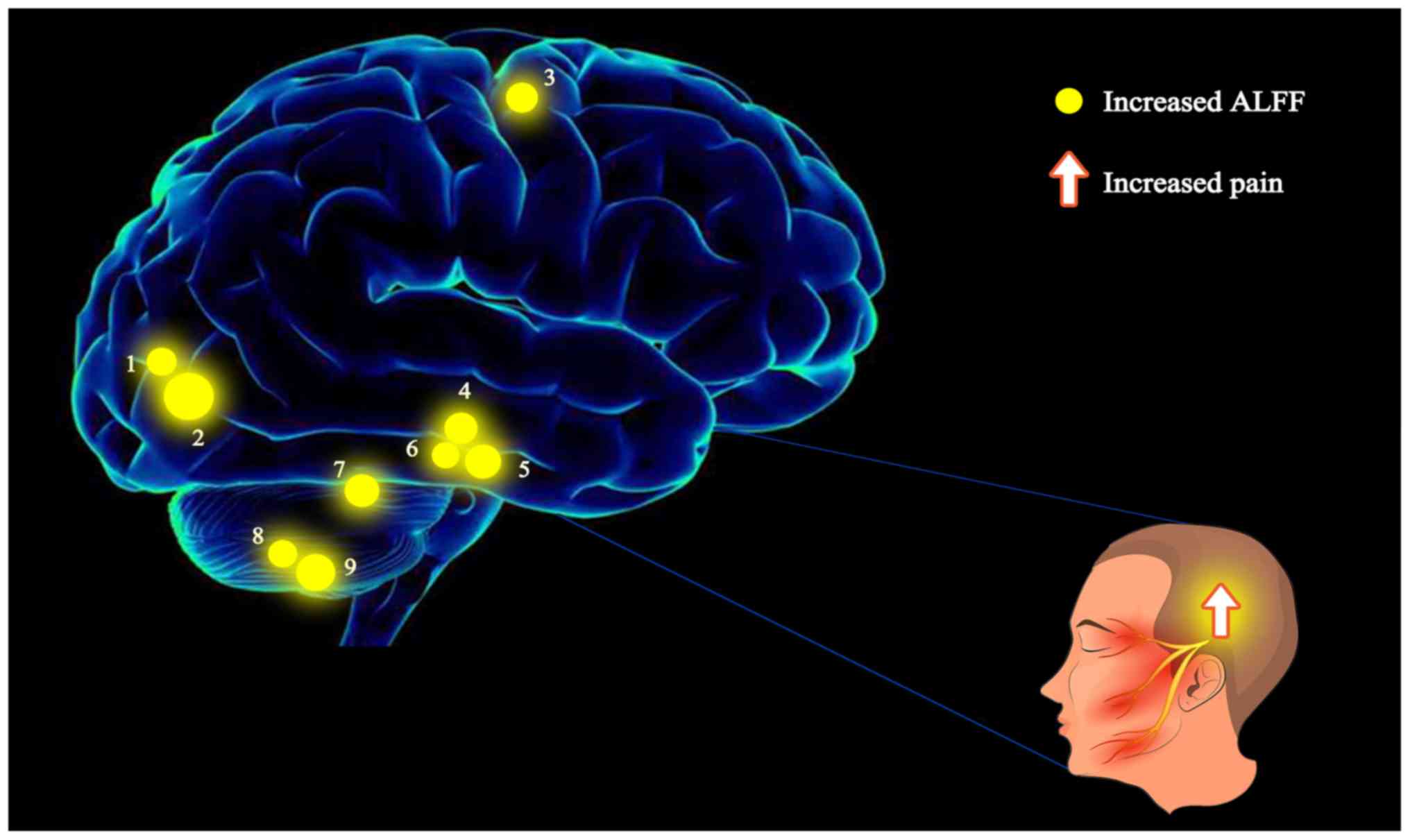 | Figure 5.The ALFF results of the brain
activity in the CTN group. The yellow spots represent brain regions
in which the ALFF value was significantly higher in CTN patients
when compared to HCs: 1-LIOG; 2-RSOG; 3-RPG; 4-RFG; 5-LFG; 6-LITG;
7-RSC; 8-LIC; 9-RIC. The sizes of the spots denote the degree of
quantitative changes. ALFF, amplitude of low-frequency fluctuation;
CTN, classical trigeminal neuralgia; HCs, healthy controls; LIOG,
left inferior occipital gyrus; RSOG, right superior occipital
gyrus; RPG, right precentral gyrus; RFG, right fusiform gyrus; LFG,
left fusiform gyrus; LITG, left inferior temporal gyrus; RSC, right
superior cerebellum; LIC, left inferior cerebellum; RIC, right
inferior cerebellum. |
 | Table II.ALFF method applied in pain-related
diseases. |
Table II.
ALFF method applied in pain-related
diseases.
| Author | Year | Disease | (Refs.) |
|---|
| Xue et
al | 2013 | Migraine | (24) |
| Wang et
al | 2017 | CTN | (25) |
| Pan et
al | 2018 | Acute eye pain | (26) |
| Zhang et
al | 2017 | Low back pain | (27) |
| Ma et
al | 2015 | Visceral pain | (28) |
| Liu et
al | 2017 | Dysmenorrhea | (29) |
 | Table III.Brain regions with differences in
fALFF between CTN patients and HCs. |
Table III.
Brain regions with differences in
fALFF between CTN patients and HCs.
|
| CTNs and HCs | MNI
coordinates |
|---|
|
|
|
|
|---|
| Brain areas | BA | T-values | Peak voxels | x | y | z |
|---|
| LFG | 20 | 6.0603 | 48 | −30 | −12 | −33 |
| RFG | 36 | 5.8291 | 93 | 42 | −33 | −27 |
| LITG | 36,20 | 4.9039 | 22 | −51 | −36 | −27 |
| LIOG | 18 | 5.3456 | 77 | −24 | −81 | −6 |
| RSOG | 18 | 8.8391 | 1,310 | 18 | −90 | 15 |
| RPG | 4 | 5.7781 | 27 | 33 | −18 | 51 |
| RSC | – | 5.9398 | 28 | 15 | −39 | −24 |
| RIC1 | – | 5.3491 | 34 | 9 | −45 | −42 |
| RIC2 | – | 6.6204 | 80 | 24 | −63 | −51 |
| LIC | – | 5.3163 | 40 | −24 | −51 | −54 |
The fusiform gyrus is located on the basal surface
of the temporal and occipital lobes, and is associated with
multiple sensory integration and cognitive processing (30). This region is also a vital
component of the marginal system, closely related to psychological
faculties such as emotion, behavior, learning and memory (31–33).
Schwedt et al (34)
revealed that patients suffering migraines exhibited stronger
fusiform gyral pain responses compared to controls. It has also
been reported that the bilateral fusiform gyrus possesses unique
visual processing mechanisms for text and objects, indicating that
this region is affected in CTN patients. Further research, however,
is required to elucidate precise structural and functional
relationships between the fusiform gyrus and CTN. Ter Minassian
et al (35) induced pain in
healthy adults by electrical stimulation, which revealed evident
abnormal activity in the left fusiform gyrus, and was negatively
correlated with the pain response level, which revealed that
fusiform gyrus plays an important role in acute pain response.
Therefore, we inferred that the increase of ALFF signal values and
neuronal activity in the bilateral fusiform gyrus of CTN patients
may be related to pain to a great extent. In addition, the fusiform
gyrus is related to classification and recognition function, which
is integrated by connecting with multiple brain regions (36). Researchers speculated that the
abnormal increase activity of these brain regions may relate to
retrieval of similar feelings in patients with CTN during recurrent
electrical-shock-like pain.
The occipital lobe is located in the posterior part
of the parietal and temporal lobes. It is a visual processing
center responsible for visual communication (33). However, a recent study in rats
revealed that the occipital lobe was associated with
pain-descending inhibitory mechanisms (37). The occipital cortex of migraine
patients was reported to possess decreased left infratemporal gray
matter mass and decreased cerebral blood flow (38). In addition, the cortical network
activity of this region was revealed to be negatively correlated
with intensity of diabetic neuropathic pain (39). In addition, in the present study,
increased ALFF signals were revealed in the left supraoccipital
gyrus and the right inferior occipital gyrus, which may be related
to the activation of pain-descending inhibitory mechanisms. It was
also revealed that the ALFF value of the suboccipital gyrus was
positively correlated with VAS, which indicated that the occipital
lobe is associated with CTN. Higher RSOG ALFF signals indicate that
pain may continue to stimulate visual processing networks despite
patients keeping eyes closed during scanning.
Inferior temporal gyrus is an important part of the
default network of the brain, which plays a key role in
self-cognition, emotional processing and regulation. Wang et
al (40) revealed that the
ReHo value of the right inferior temporal gyrus increased in
patients with ITN, indicating that chronic diseases may affect the
function of the aforementioned areas. The Gray matter volume of the
temporal lobe revealed a negative correlation to disease duration
and thus may be an important structure for the development and
maintenance of chronic pain in general and TN in particular
(41). In the present study,
increased ALFF in the inferior temporal gyrus may be associated
with the inhibition of pain induced by negative emotions and
cognitive degradation. In addition, the ALFF value of the LITG was
positively correlated with VAS and duration, and the longer the
pain lasted, the stronger the inhibitory effect was. The observed
ALFF signal changes in the occipital lobe and temporal lobe further
support the assumption that they are related to chronic
manifestation of CTN.
It was also revealed that the ALFF signal values of
the CTN subjects were abnormally decreased in the LIC and RIC
regions. Although the cerebellum has been mainly understood for its
role in motor regulation, it also implicated in a range of movement
disorders (42,43). Although, the cerebellum has been
mainly recognized for its role in motor regulation, a previous
study reported that it can receive extensive somatosensory input,
underscoring its additional role as a sensory organ (44). Changes in intensity of spontaneous
cerebellar and activity in CTN patients provides a basis, on the
contrary. In the present study, the brain areas evoked by pain were
mainly involved in the cognitive aspects of pain perception, such
as pain awareness and memory. Most abnormal brain regions, however,
had elevated ALFF signal values. It was speculated that due to
chronic and frequent pain input, the flow and integration of
information among different brain regions ultimately becomes
affected, and spontaneous cerebral activity is strengthened,
manifesting in response to pain.
The central prefrontal gyrus is located in the
frontal lobe of the cerebral cortex, which is the main movement
area cortex (45). It produces
outgoing axons in the cortical tract and terminates in the motor
neurons of the cranial and spinal cord (45,46).
For patients with TN, even simple non-painful movements can elicit
attacks of pain, while if facial movements are restricted, the pain
would be eased. The precentral gyrus (primary motor cortex) could
therefore mirror sensory pain responses to repeated TN, motor
inhibition of the maxilla and facial muscle tension (47). In the present study, an increased
ALFF value of the RPG was revealed, indicating a link between
intrinsic brain activity and pain modulation.
In fact, the ALFF values may be useful as clinical
markers to reflect pain severity in CTN patients. A study on
obsessive-compulsive disorder (OCD) by Anticevic et al
(48), used a global brain
connective (GBC) analysis method to reveal an increase in GBC in
the cerebellum at rest, indicating an excessive functional
connection between the cerebellum and other brain regions; and an
increase in cerebellar GBC. The effective treatment of the drug
against OCD could alter ligation activity, and break abnormal
functional connection, thereby reducing the OCD symptoms of the
patient. It suggests that the functional connection between the
cerebellum and other important brain regions is related to the
occurrence of OCD symptoms, and the cerebellum may participate in
the OCD abnormal neural circuit. Although the study is not based on
ALFF, it may provide us with inspiration. Perhaps therapeutic goals
can be achieved by reducing the spontaneous activity of the
CTN-related brain regions at a resting state.
In actuality, TN is divided into several categories
according to different criteria, such as, classical and
non-classical TN, primary and secondary trigeminal neuralgia.
However, there may be a crossover between them. It would be of
interest to explore the altered brain activity in patients with
non-classical TN, however the diagnosis of non-classical TN is more
difficult than that of CTN, which makes it harder to recruit
qualified subjects. In future studies, larger sample sizes and
detailed grouping of different types of TN are required, however in
the present study, conditions were limited.
Acknowledgements
Not applicable.
Funding
This study was supported by the National Natural
Science Foundation of China (grant nos. 81660158, 81460092 and
81400372), the Natural Science Key Project of Jiangxi Province
(grant no. 20161ACB21017) and the Health Development Planning
Commission Science Foundation of Jiangxi Province (grant no.
20175116).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YS and LCH conceived and designed the present study.
YC, CQX and WFL were responsible for acquiring the data, designing
the figures and tables and drafting the manuscript. NJ, PWZ and LY
contributed to the acquisition of the data and interpreting the
results. BL and QL assisted in the acquisition of the data and
drafting the manuscript. YLM and TS assisted in the acquisition and
analysis of the data with constructive discussion.
Ethics approval and consent to
participate
The present study was approved by the Medical
Research Ethics Committee of The First Affiliated Hospital of
Nanchang University. Written informed consent was obtained from all
individuals enrolled in the study.
Patient consent for publication
Consent was obtained from all individuals enrolled
in the study.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Heydari M, Shams M, Hashempur MH, Zargaran
A, Dalfardi B and Borhani-Haghighi A: The origin of the concept of
neuropathic pain in early medieval Persia (9th-12th century CE).
Acta Med Hist Adriat. 13:9–21. 2015.PubMed/NCBI
|
|
2
|
Bert C, Engenhartcabillic R and Durante M:
Particle therapy for noncancer diseases. Med Phys. 39:1716–1727.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Maila SK: Clinical outcome following
micro-vascular decompression for trigeminal neuralgia. Int J Res
Med Sci. 3:1741–1744. 2015.
|
|
4
|
Devor M, Amir R and Rappaport ZH:
Pathophysiology of trigeminal neuralgia: The ignition hypothesis.
Clin J Pain. 18:4–13. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Love S and Coakham HB: Trigeminal
neuralgia. Encyclopedia Neuroscience. 124:1173–1177. 2009.
View Article : Google Scholar
|
|
6
|
Wartolowska K and Tracey I: Neuroimaging
in Understanding Chronic Pain Mechanisms and the Development of New
Therapies. Imaging in CNS Drug Discovery and Development. Borsook
D, Beccera L, Bullmore E and Hargreaves R: Springer; New York, NY:
pp. 251–261. 2009
|
|
7
|
Yuan J, Cao S, Huang Y, Zhang Y, Xie P,
Zhang Y, Fu B, Zhang T, Song G, Yu T and Zhang M: Altered
spontaneous brain activity in patients with idiopathic trigeminal
neuralgia: A resting-state functional MRI study. Clin J Pain.
34:600–609. 2018.PubMed/NCBI
|
|
8
|
Tian L, Jiang T, Liang M, Zang Y, He Y,
Sui M and Wang Y: Enhanced resting-state brain activities in ADHD
patients: A fMRI study. Brain Dev. 30:342–348. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Moisset X, Villain N, Ducreux D, Serrie A,
Cunin G, Valade D, Calvino B and Bouhassira D: Functional brain
imaging of trigeminal neuralgia. Neuralgia Eur J Pain. 15:24–131.
2011.
|
|
10
|
Pilgrim LK, Fadili J, Fletcher P and Tyler
LK: Overcoming confounds of stimulus blocking: An Event-Related
fMRI design of semantic processing. Neuroimage. 16:713–723. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Josephs O, Turner R and Friston K:
Event-related fMRI. Hum Brain Mapp. 5:243–248. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Biswal BB, Mennes M, Zuo XN, Gohel S,
Kelly C, Smith SM, Beckmann CF, Adelstein JS, Buckner RL, Colcombe
S, et al: Toward discovery science of human brain function. Proc
Natl Acad Sci USA. 107:4734–4739. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bullmore E and Sporns O: Complex brain
networks: Graph theoretical analysis of structural and functional
systems. Nat Rev Neurosci. 10:186–198. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wu QZ, Li DM, Kuang WH, Zhang TJ, Liu S,
Huang XQ, Chan RCK, Kemp GJ and Gong QY: Abnormal regional
spontaneous neural activity in treatment-refractory depression
revealed by resting-state fMRI. Hum Brain Mapp. 32:1290–1299. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Khalili MN, Chang C, van Osch MJ, Veer IM,
van Buchem MA, Dahan A, Beckmann CF, van Gerven JM and Rombouts SA:
The impact of ‘physiological correction’ on functional connectivity
analysis of pharmacological resting state fMRI. Neuroimage.
65:499–510. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xi Q, Zhao X, Wang P, Guo Q, Jiang H, Cao
X, He Y and Yan C: Spontaneous brain activity in mild cognitive
impairment revealed by amplitude of low-frequency fluctuation
analysis: A resting-state fMRI study. Radiol Med. 117:865–871.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Dai XJ, Liu CL, Zhou RL, Gong HH, Wu B,
Gao L and Wang YX: Long-term sleep deprivation decreases the
default spontaneous activity and connectivity pattern in healthy
male subjects: A resting-state fMRI study. Neuropsychiatr Dis
Treat. 11:761–772. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zuo XN, Martino AD, Kelly C, Shehzad ZE,
Gee DG, Klein DF, Castellanos FX, Biswal BB and Milham MP: The
oscillating brain: Complex and reliable. Neuroimage. 49:1432–1445.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Logothetis NK, Pauls J, Augath M, Trinath
T and Oeltermann A: Neurophysiological investigation of the basis
of the fMRI signal. Nature. 412:150–157. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kang HH, Shu YQ, Yang L, Zhu PW, Li D, Li
QH□Min YL and Ye L: Measuring abnormal intrinsic brain activities
in patients with retinal detachment using amplitude of
low-frequency fluctuation: a resting-state fMRI study. Int J
Neurosci. 129:681–686. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tan G, Huang X, Ye L, Wu AH, He LX, Zhong
YL, Jiang N, Zhou FQ and Shao Y: Altered spontaneous brain activity
patterns in patients with unilateral acute open globe injury using
amplitude of low-frequency fluctuation: A functional magnetic
resonance imaging study. Neuropsychiatr Dis Treat. 12:2015–2020.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xiang CQ, Liu WF, Xu QH, Su T, Yong-Qiang
S, Min YL, Yuan Q, Zhu PW, Liu KC, Jiang N, et al: Altered
spontaneous brain activity in patients with classical trigeminal
neuralgia using regional homogeneity: A resting-state functional
MRI study. Pain Pract. 19:397–406. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Li HJ, Dai XJ, Gong HH, Nie X, Zhang W and
Peng DC: Aberrant spontaneous low-frequency brain activity in male
patients with severe obstructive sleep apnea revealed by
resting-state functional MRI. Neuropsychiatr Dis Treat. 11:207–214.
2015.PubMed/NCBI
|
|
24
|
Xue T, Yuan K, Cheng P, Zhao L, Zhao L, Yu
D, Dong T, von Deneen KM, Gong Q, Qin W and Tian J: Alterations of
regional spontaneous neuronal activity and corresponding brain
circuit changes during resting state in migraine without aura. NMR
Biomed. 26:1051–1058. 2013. View
Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wang Y, Xu C, Zhai L, Lu X, Wu X, Yi Y,
Liu Z, Guan Q and Zhang X: Spatial-temporal signature of
resting-state BOLD signals in classic trigeminal neuralgia. J Pain
Res. 10:2741–2750. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pan ZM, Li HJ, Bao J, Jiang N, Yuan Q,
Freeberg S, Zhu PW, Ye L, Ma MM, Huang X and Shao Y: Altered
intrinsic brain activities in patients with acute eye pain using
amplitude of low-frequency fluctuation: A resting-state fMRI study.
Neuropsychiatr Dis Treat. 14:251–257. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zhang SS, Wu W, Yang JM and Wang CH:
Abnormal spontaneous brain activity in acute Low-back pain revealed
by Resting-state functional MRI. Am J Phys Med Rehabil. 96:253–259.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ma X, Li S, Tian J, Jiang G, Wen H, Wang
T, Fang J, Zhan W and Xu Y: Altered brain spontaneous activity and
connectivity network in irritable bowel syndrome patients: A
resting-state fMRI study. Clin Neurophysiol. 126:1190–1119. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Liu P, Liu Y, Wang G, Yang X, Jin L, Sun J
and Qin W: Aberrant default mode network in patients with primary
dysmenorrhea: A fMRI study. Brain Imaging Behav. 11:1479–1485.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Parise M, Kubo TT, Doring TM, Tukamoto G,
Vincent M and Gasparetto EL: Cuneus and fusiform cortices thickness
is reduced in trigeminal neuralgia. J Headache Pain. 15:172014.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Starrfelt R and Gerlach C: The visual what
for area: Words and pictures in the left fusiform gyrus.
Neuroimage. 35:334–342. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lee CU, Shenton ME, Salisbury DF, Kasai K,
Onitsuka T, Dickey CC, Yurgelun-Todd D, Kikinis R, Jolesz FA and
McCarley RW: Fusiform gyrus volume reduction in first-episode
schizophrenia: A magnetic resonance imaging study. Arch Gen
Psychiatry. 59:775–781. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mion M, Patterson K, Acosta-Cabronero J,
Pengas G, Izquierdo-Garcia D, Hong YT, Fryer TD, Williams GB,
Hodges JR and Nestor PJ: What the left and right anterior fusiform
gyri tell us about semantic memory. Brain. 133:3256–3268. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Schwedt TJ, Chong CD, Chiang CC, Baxter L,
Schlaggar BL and Dodick DW: Enhanced pain-induced activity of pain
processing regions in a case-control study of episodic migraine.
Cephalalgia. 34:947–958. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Ter Minassian A, Ricalens E, Humbert S,
Duc F, Aubé C and Beydon L: Dissociating anticipation from
perception: Acute pain activates default mode network. Hum Brain
Mapp. 34:2228–2243. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Damasio AR and Damasio H: Cortical systems
for the retrieval of concrete knowledge: The convergence zone
framework. Large Scale Neuronal Theories of the Brain Cambridge MA:
MIT Press; pp. 61–74. 2011
|
|
37
|
Reis GM, Dias QM, Silveira JW, Del Vecchio
F, Garcia-Cairasco N and Prado WA: Antinociceptive effect of
stimulating the occipital or retrosplenial cortex in rats. J Pain.
11:1015–1026. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Cutrer FM, Sorensen AG, Weisskoff RM,
Ostergaard L, Sanchez del Rio M, Lee EJ, Rosen BR and Moskowitz MA:
Perfusion-weighted imaging defects during spontaneous migrainous
aura. Ann Neurol. 43:25–31. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Cauda F, Sacco K, Duca S, Cocito D,
D'Agata F, Geminiani GC and Canavero S: Altered resting state in
diabetic neuropathic pain. PLoS One. 4:e45422009. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Wang Y, Zhang X, Guan Q, Wan L, Yi Y and
Liu C: Altered regional homogeneity of spontaneous brain activity
in idiopathic trigeminal neuralgia. Neuropsychiatr Dis Treat.
11:2659–2666. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Obermann M, Rodriguez-Raecke R, Naegel S,
Holle D, Mueller D, Yoon MK, Theysohn N, Blex S, Diener HC and
Katsarava Z: Gray matter volume reduction reflects chronic pain in
trigeminal neuralgia. Neuroimage. 74:352–358. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Manto M, Bower JM, Conforto AB,
Delgado-García JM, Gerwig M, Habas C, Hagura N, Ivry RB, Mariën P,
Molinari M, et al: Consensus paper: Roles of the cerebellum in
motor control-the diversity of ideas on cerebellar involvement in
movement. Cerebellum. 11:457–487. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Calderon DP, Fremont R and Kraenzlin F:
The neural substrates of rapid-onset dystonia-parkinsonism. Nature.
14:357–365. 2011.
|
|
44
|
Gao JH, Parsons LM, Bower JM, Xiong J, Li
J and Fox PT: Cerebellum implicated in sensory acquisition and
discrimination rather than motor control. Science. 272:545–547.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Yousry TA, Schmid UD, Alkadhi H, Schmidt
D, Peraud A, Buettner A and Winkler P: Localization of the motor
hand area to a knob on the precentral gyrus. A new landmark. Brain.
120:141–145. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Bigbee J: Precentral Gyrus. Springer; New
York: 2011, View Article : Google Scholar
|
|
47
|
Ellingson LD, Shields MR, Stegner AJ and
Cook DB: Physical activity, sustained sedentary behavior, and pain
modulation in women with fibromyalgia. J Pain. 13:195–206. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Anticevic A, Hu S, Zhang S, Savic A,
Billingslea E, Wasylink S, Repovs G, Cole MW, Bednarski S, Krystal
JH, et al: Global resting-state functional magnetic resonance
imaging analysis identifies frontal cortex, striatal, and
cerebellar dysconnectivity inobsessive-compulsive disorder. Biol
Psychiatry. 75:595–605. 2014. View Article : Google Scholar : PubMed/NCBI
|