Introduction
Irritable bowel syndrome (IBS) is the most common
functional gastrointestinal (GI) disorder, diagnosed by symptom
questionnaires according to defined criteria (1). The worldwide prevalence of IBS
according to the Rome IV criteria is 4.1% (range 1.3-7.6%) and
varies depending on the country and definition used (2,3).
The majority of the IBS patients are handled at primary healthcare
centers; however, recruitment of these subjects in studies is
performed at tertiary healthcare centers (4). Since only 21% of the patients who
experienced IBS symptoms in the previous year will consult a
physician, the number of unknown cases in the society may be
considerably high (5).
Several research studies have been performed during
the last decades to identify the etiology and pathophysiology of
IBS. The most established risk factors for the development of IBS
are female sex, smoking, and psychological stress (6). Although a low-grade inflammation has
been suggested, this theory is difficult to be confirmed (7). Alterations in gut microbiota have
also been widely discussed; however, different studies have shown
varying results, and no definitive conclusions have been reached
(8). Impaired intestinal barrier
is one of the several hypotheses established to explain functional
GI symptoms. Zonulin has been suggested to be a marker of increased
intestinal permeability (9).
Genetic studies have described associations between IBS and certain
gene variants, such as IKBKAP; these variants are found in
patients with familial dysautonomia and associated GI symptoms
(10,11). Therefore, a hypothesis was
established suggesting that certain forms of IBS may depend on
autonomic dysfunction (12).
Furthermore, the increased survival of premature children exerts a
certain impact on the general health of the affected subjects.
Infants born prior to the 37th completed week of pregnancy, those
with low birth weight (LBW) (<2,500 g), low Apgar scores, or
small for gestational age (SGA), have been associated with negative
health consequences, such as IBS (13–16).
During the last years, a population-based
cross-sectional study, termed the Malmö Offspring Study (MOS), was
performed in the south of Sweden to include participants from the
general population. Several studies have been performed to estimate
risk factors for IBS/GI symptoms. The aim of the present minireview
was to summarize the estimated associations between self-reported
IBS and GI symptoms in the general population and intestinal
permeability, early life factors, gut microbiota, autonomic
homeostasis, sociodemographic characteristics, lifestyle habits,
chronic stress, sleeping habits, concomitant disorders, and drug
treatment.
MOS
The Malmö Diet and Cancer Study (n=28,098) is a
population-based study, which was performed between 1991 and 1996
and invited all subjects born between 1923 and 1950 (17). Subsequently, 6,103 of these
individuals were randomly selected and re-examined for assessing
cardiovascular risk factors. These subjects comprised the Malmö
Diet and Cancer Cardiovascular Cohort (MDC-CC) (18). MOS consists of children and
grandchildren of the participants of the MDC-CC (19). The participants were clinically
examined, their blood and fecal samples were collected and the
study questionnaires were completed. The participants were
categorized to suffer from self-reported IBS if they answered ‘yes’
to the following question: ‘Have you several times during a month
suffered from abdominal pain related to irregular bowel habits,
which is called IBS?’ The formulation was considered to reflect the
Rome III criteria for IBS (20).
They were categorized to suffer from GI symptoms if they answered
‘yes’ to the following question: ‘Have you suffered from any GI
symptoms within the past 2 weeks?’ The two conditions were
associated with each other throughout the study (P<0.001). The
participants who experienced GI symptoms were encouraged to
complete the visual analog scale (VAS) for IBS (VAS-IBS) to assess
the degree of specific symptoms on a VAS scale (21).
Citations of three sets of MOS
cohorts
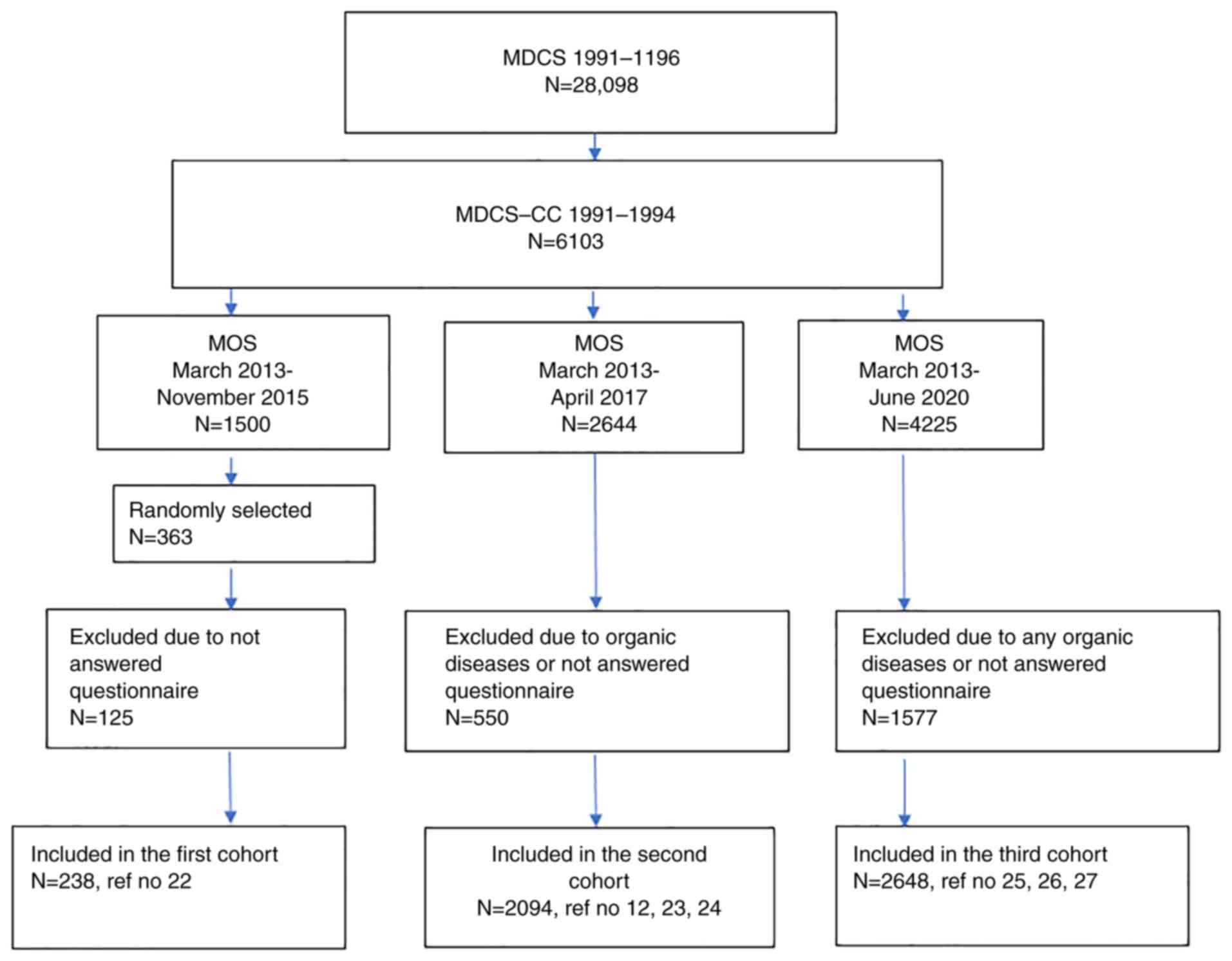
Firstly, 363 of the 1,500 participants attended
between March 2013 and November 2015, of whom 186 were women
accounting for 51.2%. These patients were randomly selected for
serum analysis of zonulin by a commercial ELISA kit. A total of 238
participants of the 363 selected had completed the study questions
regarding GI symptoms (Fig. 1,
Table I) (22). Secondly, 2,644 participants were
included between March 2013 and April 2017. The participants who
reported organic GI diseases, did not answer the questions
regarding GI symptoms, or did not have data regarding autonomic
function tests, gut microbiota, or data from the Swedish Medical
Birth Registry (started 1973) were excluded. In total, 1,013
participants were included in the study of early life factors
(23), whereas 1,988 participants
were included in the study of gut microbiota (24), and 2,094 participants were
included in the studies of autonomic, hemodynamic parameters
(12) (Fig. 1, Table I). Thirdly, 1,577 participants of
the 4,225 participants included between March 2013 and June 2020
(46.7% participation rate) were excluded due to the presence of any
type of organic GI disease or due to their inability to provide an
answer to the questions regarding GI symptoms. Therefore, 2,648
individuals were finally included in the study of sociodemographic
factors (25), chronic stress and
sleeping habits (26),
concomitant diseases, drug use, and family history of any diseases
(27) (Fig. 1; Table I).
 | Table I.Description of the different original
manuscripts published from the Malmö Offspring Study cohorts and
summarized in the minireview. |
Table I.
Description of the different original
manuscripts published from the Malmö Offspring Study cohorts and
summarized in the minireview.
| First author/s,
year | Cohorts | No. | Age, years | BMI,
kg/m2 | Female sex, n
(%) | GI symptoms, n
(%) | IBS, n (%) | (Refs.) |
|---|
| Ohlsson et
al, 2017 | Serum zonulin | 238 | 42.6±13.2 | 22.8±4.2 | 127 (53.4) | 44 (18.5) | 40 (16.8) | (22) |
| Wennerberg et
al, 2021 | Early life factors;
excluded celiac disease, IBD and lactose intolerance | 1013 | 29.0±6.8 | 24.9±4.5 | 546 (53.9) | 253 (25.0) | 179 (17.7) | (23) |
| Brunkwall et
al, 2021 | Gut microbiota;
excluded celiac disease, IBD and lactose intolerance | 1988 | 39.8±13.9 | 25.8±4.7 | 1055 (53.1) | 396 (19.9) | 305 (15.3) | (24) |
| Hamrefors et
al, 2019 | Hemodynamic
parameters; excluded celiac disease and IBD | 2094 | 40.1±13.6 | 25.9±4.9 | 1127 (53.8) | 509 (24.3) | 347 (16.6) | (12) |
| Nilsson and
Ohlsson, 2021 | Sociodemography and
lifestyle; excluded any organic GI disease | 2648 | 42.6±14.4 | 25.9±4.7 | 1391 (52.5) | 459 (17.3) | 316 (11.9) | (25) |
| Zejnelagic and
Ohlsson, 2021 | Stress and sleeping
habits; excluded any organic GI disease | 2648 | 42.6±14.4 | 25.9±4.7 | 1391 (52.5) | 459 (17.3) | 316 (11.9) | (26) |
| Ruderstam and
Ohlsson, 2022 | Concomitant
diseases and drugs; excluded any organic GI disease | 2648 | 42.6±14.4 | 25.9±4.7 | 1391 (52.5) | 459 (17.3) | 316 (11.9) | (27) |
Zonulin
The serum concentration of zonulin did not differ
between sexes (21). Zonulin
levels correlated with weight, body mass index (BMI), waist- and
hip-circumference, systolic blood pressure, diastolic blood
pressure, and fasting plasma glucose levels, whereas
sociodemographic factors and lifestyle habits did not influence
zonulin levels. The presence or absence of GI symptoms during the
past 2 weeks (n=44) did not affect zonulin levels. Accordingly, the
degree of GI symptoms or psychological well-being did not correlate
with the serum values of zonulin (22). The participants with any type of
history of organic GI diseases (n=54) exhibited the same zonulin
levels as those without the presence of any disease. The same
finding was also noted in the subjects with functional dyspepsia or
self-reported IBS (n=61) (22).
Early life factors
Age and BMI did not differ between the subjects with
or without IBS or GI symptoms (23). A trend for an association between
GI symptoms and preterm birth was noted compared with the term
birth, which was also noted following estimation of the gestational
age used as a continuous variable. Further calculations stratifying
for the severity of the GI symptoms did not show significant
associations between prematurity and GI symptoms. Lower body weight
at birth, low Apgar score, or SGA did not show significant
associations with the presence of functional GI symptoms or the
degree of symptom severity. However, in contrast to a low Apgar
score, both lower body weight measured as a continuous scale and
SGA were associated with a high degree of symptom influence on
daily life. No association of the early life factors was noted with
self-reported IBS (23).
Gut microbiota
The subjects with IBS and/or GI symptoms were
younger than those without these two conditions, whereas the
parameter BMI did not differ between these groups (24).
Beta-diversity, assessed by the Bray-Curtis
dissimilarity index, was significantly different between
individuals reporting either IBS or GI symptoms compared with those
who did not present with GI complaints. In contrast to these
findings, alpha-diversity did not significantly differ between
these conditions. Following calculations of the different genera
with adjustments for confounders and false discovery rate (FDR), it
was found that IBS was associated with an abundance of
Blautia; GI symptoms were associated with Blautia and
a genus in the order of SHA-98 bacteria. Diarrhea was associated
with Blautia, Prevotella, and a genus in the order of SHA-98
bacteria and Christensellaceae family (24).
Hemodynamic parameters
BMI did not differ between groups, but the subjects
with IBS or GI symptoms were younger than those without these
conditions (12). No significant
alterations were noted in hemodynamic parameters between IBS and
non-IBS subjects following adjustment for confounders. In contrast
to these findings, lower values of diastolic blood pressure in
supine and standing positions, and mean systolic and diastolic
blood pressures during ambulatory 24-h measurements, demonstrated
significant differences in those with GI symptoms compared with
those without any GI symptoms following adjustments for age, sex,
current smoking, and chronic stress. A total of 142 subjects
(27.9%) reported diarrhea being their most predominant symptom;
this was the only specific symptom, which was associated with
hemodynamic parameters following adjustment of confounders. For the
24-h measurements, concordant positive correlations were noted
between systolic blood pressure, diastolic blood pressure, and
heart rate, and the severity of diarrhea. In accordance with the
correlation analyses, the adjusted linear regression indicated
associations between the 24-h hemodynamic measurements of the
systolic blood pressure, diastolic blood pressure, and heart rate.
Significant associations were also noted for the diastolic blood
pressure in the supine position following comparisons of the fourth
quartile with quartiles 1–3 of diarrhea (12).
Sociodemographic and lifestyle factors
Strong associations were noted between all specific
symptoms and self-reported IBS (P<0.001, except for
constipation, P=0.008). The IBS participants had the same age as
those without IBS, whereas those with GI symptoms were younger than
those without these symptoms. BMI was lower in participants with
IBS and GI symptoms than in those without these conditions
(25).
Self-reported IBS was associated with female sex,
former smoking, and present smoking, and inversely associated with
drinking frequency of 2–3 times a week and drinking 3–4 standard
glasses per occasion (25).
The GI symptoms in the past 2 weeks were associated
with female sex, studying, unemployment, former smoking, and
present smoking, whereas the symptoms were inversely associated
with age 50–59 years and age ≥60 years (25).
The examination of specific GI symptoms, with the
exception of diarrhea and vomiting and nausea indicated that worse
symptoms were associated with female sex and worse psychological
well-being. Present smoking was associated with more severe GI
symptoms and worse psychological well-being. Studying was
associated with a higher degree of abdominal pain, and bloating and
flatulence, but improved psychological well-being. Sick leave and
unemployment were, in comparison to working, associated with more
symptoms and poorer psychological well-being (25).
Following stratification for sex, IBS in male sex
was associated with an age range of 30–39, 40–49, and unemployment.
The GI symptoms in the past 2 weeks were associated with
unemployment. IBS in women was associated with present smoking and
GI symptoms were associated with former smoking and were inversely
associated with age ≥50 years and intermediate physical activity at
work (25).
No significant associations were noted between IBS
or GI symptoms in the past 2 weeks and BMI groups, education,
marital status, snuff use, or physical activity during leisure time
(25).
Chronic stress and sleeping habits
The experience of chronic stress during the past
year was associated with self-reported IBS and GI symptoms, as was
chronic stress during the past 5 years, following adjustment for
sociodemographic factors (26).
Average, bad, or very bad sleeping quality, sleeping
onset difficulties, and ≥3 wake-ups per week were associated with
self-reported IBS, whereas a sleeping duration of 7 h was inversely
associated with self-reported IBS. The only sleeping habit
associated with GI symptoms was a wake-up frequency of 3–6 times
per week.
Following the combined calculation of all the
variables of stress and sleeping disturbances in the full model
adjusted for all confounders, a marked association was noted
between self-reported IBS and sleeping onset difficulties and
chronic stress during the past 5 years, whereas GI symptoms were
associated with chronic stress in the past year (26).
Stress, poor sleeping quality, sleeping onset
difficulties, and IBS/GI symptoms were all associated with poor
psychological well-being (26).
Self-reported IBS or GI symptoms and
comorbidity, medication, and family history of diseases
When examining comorbidity, asthma was associated
with self-reported IBS. The associations between asthma and GI
symptoms in the past 2 weeks and chest pain >30 min and IBS
disappeared following adjustment for FDR (27).
IBS was associated with prescription of drugs in the
past week or the use of a non-prescription drug in the past week.
When calculations were performed with specific medications,
antihistamines, beta blockers, and hypnotics were the drugs
associated with IBS (27).
GI symptoms in the past 2 weeks were associated with
non-prescription drugs prior to FDR correction, as well as the
prescribed drugs beta-blockers and proton pump inhibitors (27).
A family history of prostate cancer was associated
with IBS, whereas a family history of joint diseases and myocardial
infarction were associated with GI symptoms. In addition, there was
an association between GI disease in the family and self-reported
IBS and GI symptoms. Regarding the subgroups of GI diseases, IBS
was associated with celiac disease, gastric ulcer, functional
dyspepsia, IBS, and reflux; GI symptoms were associated with
functional dyspepsia, IBS, and reflux (27).
Discussion
The main findings from the studies performed in the
general population were that a limited number of objective findings
could be identified in the group of participants with IBS and GI
symptoms (12,22,24). In contrast to this observation,
strong associations between IBS and GI symptoms were noted with
female sex, younger age, smoking, unemployment, stress, poor
psychological well-being, poor sleeping habits as well as drug use,
and family history of GI diseases (25–27).
The findings are in accordance with previous
studies, showing a high prevalence of IBS in the general population
(28). Moreover, the data
indicated that psychosocial and sensory factors contributed to
self-reported pain in IBS (29).
In addition, dietary and lifestyle habits are of importance for
symptom development (30).
Collectively, the included studies support the importance of
performing scientific studies in subjects from the general
population, and not only in subjects from tertiary healthcare
centers (4), where selected
patients are referred who may suffer from enteric dysmotility and
not by IBS, which can obscure the results (31,32).
It has been previously shown that IBS and GI
symptoms are strongly associated with female sex and smoking,
whereas higher age is inversely associated with these conditions
(25). Unemployment was
associated with GI symptoms, notably in men. Sick leave and
unemployment were associated with the presence of GI symptoms and
with more severe symptoms and impaired psychological well-being
(25). This is in accordance with
prior studies that have shown a high degree of unemployment and
absence from work in patients with self-reported IBS (5). Men have been found to have poorer
mental health than women when they are unemployed, possibly due to
traditional beliefs that they should be solely responsible for
providing financial support to their families (33). The subjective social status
relative to other individuals in the same community may mediate the
association between occupational status, psychological well-being,
and stress (34).
Most studies performed have a cross-sectional design
and causality can therefore not be analyzed. Among the limited
number of prospective studies performed regarding sleeping habits,
the parameters poor self-reported sleeping quality, and frequent
waking episodes could predict additional abdominal or other types
of pain, anxiety, and fatigue the following day (35–37). The most important predictor of
poor sleeping quality was pre-sleep cognitive arousal (35). Higher arousal and awakening index
have been described in IBS patients, which can be associated with
sleeping fragmentation (38).
Collectively, low quality of life, depression, and arousal affect
the quality and efficiency of sleeping as well as the experience of
pain and IBS symptoms (35–37).
It has been previously reported that drug treatment
may increase the prevalence of GI symptoms (39). However, this increase may be due
to the disease per se, which requires drug treatment,
leading to the development of GI symptoms. Furthermore, chronic
illness behavior is a learned behavior found to be increased in IBS
patients (40). Children of
parents with IBS had a significantly higher number of ambulatory
care visits; this trend was independent of the presence of GI
symptoms (41). The model of
social learning and behavior may thus explain the associations
found in family history (27),
although genetic components have been found as well, which may lead
to disease development of several members within the same family
(42,43). Perinatal factors were not
associated with the significance of the development of IBS in the
MOS cohort, although previous studies have found an increased risk
to develop IBS when infants are born with LBW (14,42).
Intestinal permeability assessed by zonulin cannot
alone explain the GI symptoms. By contrast, overweight and
metabolic syndromes exhibited a higher association with zonulin
levels (22). Despite these
findings, in a larger population-based study within the same area,
subjects with prevalent inflammatory bowel disease had higher
zonulin levels compared with those without inflammatory bowel
disease (44). The microbiota
changes noted in IBS in the general population were modest and
suggested that gut microbiota was not the major explanation to GI
symptoms (23), which was in line
with a study performed in the general population, indicating no
significant differences in the microbiota from tissue biopsies or
feces of IBS patients compared with those of healthy subjects
(45). Furthermore, autonomic
neuropathy cannot explain IBS in the general population (12) and the findings do not support the
genetic associations with familial dysautonomia found in IBS
(10,11).
The advantage of the performed studies of
self-reported IBS and GI symptoms is the examination of the general
population as opposed to the examination of the tertiary healthcare
centers. The major limitation of the present study was that the
dietary habits were not examined, since the symptom development in
IBS is suggested to depend on the accumulation of unabsorbed
carbohydrates in the bowel leading to gas production and osmotic
diffusion of water (46).
However, the present findings confirm the multifactorial etiology
of IBS, suggesting that not only dietary factors are of importance
in the development of this disease.
In conclusion, few objective medical findings could
be identified in participants with IBS and GI symptoms from the
general population. The etiology to IBS seems to be multifactorial.
Strong associations were reported with younger age, female sex,
smoking, unemployment, stress, poor psychological well-being,
drugs, and a family history of GI disorders. Therefore,
sociodemographic factors and lifestyle habits must be considered,
and the treatment should be focused on the prevention and
elimination of stressful life factors, and not only on medical
reasons, drug treatment, and dietary advice.
Acknowledgements
The author would like to thank Mr. Anders Dahlin
(Department of Clinical Sciences, Malmö, Lund University, Sweden)
for data management.
Funding
The study was financed by the Development Foundation of Region
Skåne (grant numbers REGSKANE-818781, 2018-Projekt0024).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
BO wrote this minireview and drew the figure. Data
authentication is not applicable. The author has read and approved
the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The author declares that she has no competing
interests.
References
|
1
|
Lacy BE, Mearin F, Chang L, Chey WD, Lembo
AJ, Simren M and Spiller R: Bowel disorders. Gastroenterology.
150:1393–1407.e5. 2016. View Article : Google Scholar
|
|
2
|
Lovell RM and Ford AC: Global prevalence
of and risk factors for irritable bowel syndrome: A meta-analysis.
Clin Gastroenterol Hepatol. 10:712–721.e4. 2012. View Article : Google Scholar
|
|
3
|
Sperber AD, Bangdiwala SI, Drossman DA,
Ghoshal UC, Simren M, Tack J, Whitehead WE, Dumitrascu DL, Fang X,
Fukudo S, et al: Worldwide prevalence and burden of functional
gastrointestinal disorders, results of Rome foundation global
study. Gastroenterology. 160:99–114.e3. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Canavan C, West J and Card T: The
epidemiology of irritable bowel syndrome. Clin Epidemiol. 6:71–80.
2014.
|
|
5
|
Van den Houte K, Carbone F, Pannemans J,
Corsetti M, Fischler B, Piessevaux H and Tack J: Prevalence and
impact of self-reported irritable bowel symptoms in the general
population. United European Gastroenterol J. 7:307–315. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nam SY, Kim BC, Ryu KH and Park BJ:
Prevalence and risk factors of irritable bowel syndrome in healthy
screenee undergoing colonoscopy and laboratory tests. J
Neurogastroenterol Motil. 16:47–51. 2010. View Article : Google Scholar
|
|
7
|
Nilholm C, Larsson E, Sonestedt E, Roth B
and Ohlsson B: Assessment of a 4-week starch- and sucrose-reduced
diet and its effects on gastrointestinal symptoms and inflammatory
parameters among patients with irritable bowel syndrome. Nutrients.
13:4162021. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Singh P and Lembo A: Emerging role of the
gut microbiome in irritable bowel syndrome. Gastroenterol Clin
North Am. 50:523–545. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Fasano A: Zonulin, regulation of tight
junctions, and autoimmune diseases. Ann N Y Acad Sci. 1258:25–33.
2012. View Article : Google Scholar
|
|
10
|
Bonfiglio F, Zheng T, Garcia-Etxebarria K,
Hadizadeh F, Bujanda L, Bresso F, Agreus L, Andreasson A, Dlugosz
A, Lindberg G, et al: Female-specific association between variants
on chromosome 9 and self-reported diagnosis of irritable bowel
syndrome. Gastroenterology. 155:168–179. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Axelrod FB: Familial dysautonomia. Muscle
Nerve. 29:352–363. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hamrefors V, Fedorowski A and Ohlsson B:
Susceptibility to diarrhea is related to hemodynamic markers of
sympathetic activation in the general population. Scand J
Gastroenterol. 54:1426–1432. 2019. View Article : Google Scholar
|
|
13
|
Raju TNK, Buist AS, Blaisdell CJ,
Moxey-Mims M and Saigal S: Adults born preterm: A review of general
health and system-specific outcomes. Acta Paediatr. 106:1409–1437.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Raslau D, Herrick LM, Locke GR, Schleck
CD, Zinsmeister AR, Almazar A, Talley NJ and Saito YA: Irritable
bowel syndrome and the perinatal period: Lower birth weight
increases the risk. Neurogastroenterol Motil. 28:1518–1524. 2016.
View Article : Google Scholar
|
|
15
|
Leybovitz-Haleluya N, Wainstock T, Sheiner
E, Segal I, Landau D and Walfisch A: Low Apgar scores in term
newborns and long-term gastro-intestinal morbidity: A
population-based cohort study with up to 18 years of follow-up. J
Matern Fetal Neonatal Med. 32:1609–1614. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Vayssière C, Sentilhes L, Ego A, Bernard
C, Cambourieu D, Flamant C, Gascoin G, Gaudineau A, Grangé G,
Houfflin-Debarge V, et al: Fetal growth restriction and
intra-uterine growth restriction: Guidelines for clinical practice
from the French college of gynaecologists and obstretricians. Eur J
Obstet Gynecol Reprod Biol. 193:10–18. 2015. View Article : Google Scholar
|
|
17
|
Berglund G, Elmstähl S, Janzon L and
Larsson SA: The Malmo diet and cancer study. Design and
feasibility. J Intern Med. 233:45–51. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Smith JG, Newton-Cheh C, Almgren P, Struck
J, Morgenthaler NG, Bergmann A, Platonov PG, Hedblad B, Engström G,
Wang TJ and Melander O: Assessment of conventional cardiovascular
risk factors and multiple biomarkers for the prediction of incident
heart failure and atrial fibrillation. J Am Coll Cardiol.
56:1712–1719. 2010. View Article : Google Scholar
|
|
19
|
Brunkwall L, Jönsson D, Ericson U,
Hellstrand S, Kennbäck C, Östling G, Jujic A, Melander O, Engström
G, Nilsson J, et al: The Malmö offspring study (MOS): Design,
methods and first results. Eur J Epidemiol. 36:103–116. 2021.
View Article : Google Scholar
|
|
20
|
Longstreth GF, Thompson WG, Chey WD,
Houghton LA, Mearin F and Spiller RC: Functional bowel disorders.
Gastroenterology. 130:1480–1491. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bengtsson M, Ohlsson B and Ulander K:
Development and psychometric testing of the visual analogue scale
for irritable bowel syndrome (VAS-IBS). BMC Gastroenterol.
7:162007. View Article : Google Scholar
|
|
22
|
Ohlsson B, Orho-Melander M and Nilsson PM:
Higher levels of serum zonulin may rather be associated with
increased risk of obesity and hyperlipidemia, than with
gastrointestinal symptoms or disease manifestation. Int J Mol Sci.
18:5822017. View Article : Google Scholar
|
|
23
|
Wennerberg J, Sharma S, Nilsson PM and
Ohlsson B: A possible association between early life factors and
burden of functional bowel symptoms in adulthood. Scand J Prim
Health Care. 39:506–514. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Brunkwall L, Ericson U, Nilsson PM,
Orho-Melander M and Ohlsson B: Self-reported bowel symptoms are
associated with differences in overall gut microbiota composition
and enrichment of Blautia in a population-based cohort. J
Gastroenterol Hepatol. 36:174–180. 2021. View Article : Google Scholar
|
|
25
|
Nilsson D and Ohlsson B: Gastrointestinal
symptoms and irritable bowel syndrome are associated with female
sex and smoking in the general population and with unemployment in
men. Front Med (Lausanne). 8:6466582021. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zejnelagic J and Ohlsson B: Chronic stress
and poor sleeping habits are associated with self-reported IBS and
poor psychological well-being in the general population. BMC Res
Notes. 14:2802021. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ruderstam H and Ohlsson B: Self-reported
IBS and gastrointestinal symptoms in the general population are
associated with asthma, drug consumption and a family history of
gastrointestinal diseases. Scand J Gastroenterol. Feb 1–2022.(Epub
ahead of print). doi: 10.1080/00365521.2022.2031281. View Article : Google Scholar
|
|
28
|
Palma J, Antoniewicz J, Borecki K,
Tejchman K, Skonieczna-Żydecka K, Maciejewska-Markiewicz D,
Ryterska K, Komorniak N, Czerwińska-Rogowska M, Wolska A, et al:
Irritable bowel syndrome prevalence among participants of woodstock
rock festival in Poland based on Rome IV criteria questionnaire.
Int J Environ Res Public Health. 18:114642021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chen J, Barandouzi ZA, Lee J, Xu W, Feng
B, Starkweather A and Cong X: Psychosocial and sensory factors
contribute to self-reported pain and quality of life in young
adults with irritable bowel syndrome. Pain Manag Nurs. Jan
21–2022.(Epub ahead of print). doi: 10.1016/j.pmn.2021.12.004.
View Article : Google Scholar
|
|
30
|
Zhang C, Zhang J, Wang Y, Lang R, Su L, Yu
M, Zhao X, Yang G and Ren Z: Association between breakfast
consumption frequency and the risk of irritable bowel syndrome
among Chinese female college students: A cross-sectional study.
Medicine (Baltimore). 100:e275412021. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hellström PM: Pathophysiology of the
irritable bowel syndrome-reflections of today. Best Pract Res Clin
Gastroenterol. 40–41. 1016202019.
|
|
32
|
Lindberg G: Pseudo-obstruction, enteric
dysmotility and irritable bowel syndrome. Best Pract Res Clin
Gastroenterol. 40–41. 1016352019.
|
|
33
|
Artazcoz L, Benach J, Borrell C and Cortès
I: Unemployment and mental health: Understanding the interactions
among gender, family roles, and social class. Am J Public Health.
94:82–88. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Neubert M, Süssenbach P, Rief W and
Euteneuer F: Unemployment and mental health in the German
population: The role of subjective social status. Psychol Res Behav
Manag. 12:557–564. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Tang NKY, Goodchild CE, Sanborn AN, Howard
J and Salkovskis PM: Deciphering the temporal link between pain and
sleep in a heterogeneous chronic pain patient sample: A multilevel
daily process study. Sleep. 35:675–687A. 2012.PubMed/NCBI
|
|
36
|
Buchanan DT, Cain K, Heitkemper M, Burr R,
Vitiello MV, Zia J and Jarrett M: Sleep measures predict next-day
symptoms in women with irritable bowel syndrome. J Clin Sleep Med.
10:1003–1009. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Patel A, Hasak S, Cassell B, Ciorba MA,
Vivio EE, Kumar M, Gyawali CP and Sayuk GS: Effects of disturbed
sleep on gastrointestinal and somatic pain symptoms in irritable
bowel syndrome. Aliment Pharmacol Ther. 44:246–258. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Rotem AY, Sperber AD, Krugliak P, Freidman
B, Tal A and Tarasiuk A: Polysomnographic and actigraphic evidence
of sleep fragmentation in patients with irritable bowel syndrome.
Sleep. 26:747–752. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Fosnes GS, Lydersen S and Farup PG:
Constipation and diarrhoea-common adverse drug reactions? A cross
sectional study in the general population. BMC Clin Pharmacol.
11:22011. View Article : Google Scholar
|
|
40
|
Whitehead WE, Winget C, Fedoravicius AS,
Wooley S and Blackwell B: Learned illness behavior in patients with
irritable bowel syndrome and peptic ulcer. Dig Dis Sci. 27:202–208.
1982. View Article : Google Scholar
|
|
41
|
Levy RL, Whitehead WE, Von Korff MR and
Feld AD: Intergenerational transmission of gastrointestinal illness
behavior. Am J Gastroenterol. 95:451–456. 2000. View Article : Google Scholar
|
|
42
|
Bengtson MB, T Rønning T, Vatn MH and
Harris JR: Irritable bowel syndrome in twins: Genes and
environment. Gut. 55:1754–1759. 2006. View Article : Google Scholar
|
|
43
|
Waehrens R, Ohlsson H, Sundquist J,
Sundquist K and Zöller B: Risk of irritable bowel syndrome in
first-degree, second-degree and third-degree relatives of affected
individuals: A nationwide family study in Sweden. Gut. 64:215–221.
2015. View Article : Google Scholar
|
|
44
|
Wang X, Memon AA, Palmér K, Hedelius A,
Sundquist J and Sundquist K: The association of zonulin-related
proteins with prevalent and incident inflammatory bowel disease.
BMC Gastroenterol. 22:32022. View Article : Google Scholar
|
|
45
|
Hugerth LW, Andreasson A, Talley NJ,
Forsberg AM, Kjellström L, Schmidt PT, Agreus L and Engstrand L: No
distinct microbiome signature of irritable bowel syndrome found in
a Swedish random population. Gut. 69:1076–1084. 2020. View Article : Google Scholar
|
|
46
|
Algera J, Colomier E and Simrén M: The
Dietary Management of Patients with Irritable Bowel Syndrome: A
Narrative Review of the Existing and Emerging Evidence. Nutrients.
11:21622019. View Article : Google Scholar
|