Introduction
Cancer of the head and neck (HNC) refers to a
various types of cancer, predominantly squamous cell carcinomas,
arising from a variety of sites and grouped together under this
category, including oropharyngeal cancer. Worldwide, cancers of the
oropharynx and hypopharynx account for an estimated 123,000 new
cases per year, with an estimated mortality of 79,000 deaths
(1). Surgery and/or radiotherapy
are the standard treatment for oropharyngeal cancer, and these
modalities are frequently complicated by the suboptimal control of
locoregional disease and significant long-term functional deficits
(1).
Paraneoplastic neurological syndromes (PNS) are
defined as remote effects of cancer that are not caused by the
tumor and its metastasis, nor by infection, ischemia, toxicity of
cancer therapy, coagulopathy or metabolic disruptions (2). In the majority of patients,
neurological disorders develop before the cancer becomes clinically
overt. In the last two decades, the finding that certain PNS are
associated with antibodies directed against tumoral antigens
expressed by the tumor and the nervous system suggests that these
disorders are immune-mediated. Numerous onconeural antibodies have
been described, but less than 50% of patients with PNS harbor these
types of proteins.
Therefore, the absence of paraneoplastic antibodies
does not exclude the diagnosis of PNS. The main neurological
syndromes associated with paraneoplastic origin include limbic
encephalitis, subacute cerebellar ataxia, opsoclonus-myoclonus,
retinopathies, chronic gastrointestinal pseudoobstruction, sensory
neuronopathy, Lambert-Eaton myasthenic syndrome and
encephalomyelitis (3).
The majority of tumors associated with PNS are small
cell lung cancer (SCLC), ovarian cancer and hematological diseases,
mainly lymphomas. PNS in HNC is extremely rare. No publications are
currently available on the association between squamous
oropharyngeal cancer and neurological paraneoplastic disease
(4).
Recently, we encountered a patient with a locally
advanced oropharyngeal cancer who simultaneously developed a
PNS-type encephalomyelitis. To the best of our knowledge, a PNS in
a patient with HNC has not previously been reported.
Case report
A 58-year-old male was admitted to the emergency
room. Two to three days earlier, he had experienced weakness in his
left leg resulting in difficulty in walking, which the day prior to
admission had progressed to affect the left arm and the right part
of the face. No prior medical conditions or surgeries were noted.
The patient was a social drinker and he usually smoked one pack of
cigarettes per day.
A number of weeks prior to admission, the patient
experienced hypoesthesia to cold and hot stimuli in his right leg.
He also reported that he occasionally suffered pain in the throat
and noted blood in his spittle.
A general physical examination showed no abnormal
findings. However, a neurological examination revealed right facial
palsy, mild brachiocrural left hemiparesis with increased tendon
reflexes and a Babinski response on the left side. The laboratory
values were within normal limits. A chest X-ray did not show any
relevant findings. The brain and body CT was normal. In the ear,
nose and throat (ENT) examination, a small lesion (<1 cm) in the
right tonsilar bed was found and a biopsy sample was removed.
Pathological examination of the sample was consistent with squamous
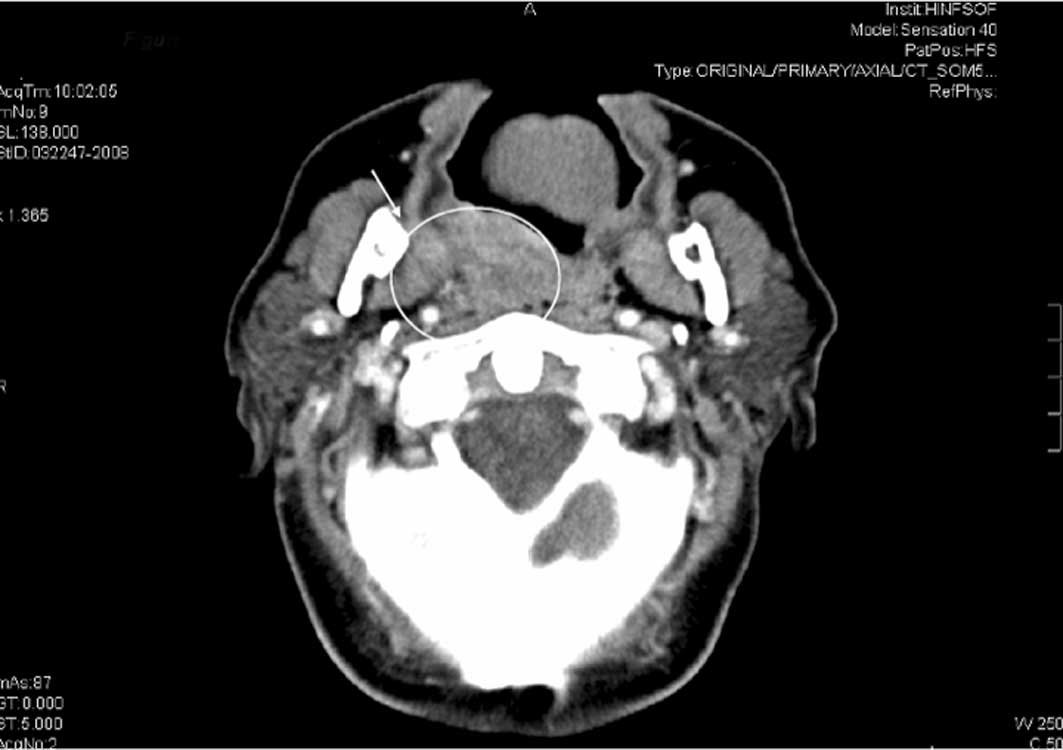
cell carcinoma. The MRI and CT (Fig.
1) of the neck showed a heterogeneous mass located on the right
tonsilar area involving the pterygoideus medial muscle and the
pre-styloid parapharingeus space. This mass grew inside the back
wall of the oropharynx, and presumably involved the long neck
muscle on the right side. Certain cervical lymph nodes were present
in the IIA and IIB spaces, the largest diameter being ~2.5 cm.
According to the endoscopic and radiological findings, the TNM
classification was T4N2bM0 (IVA).
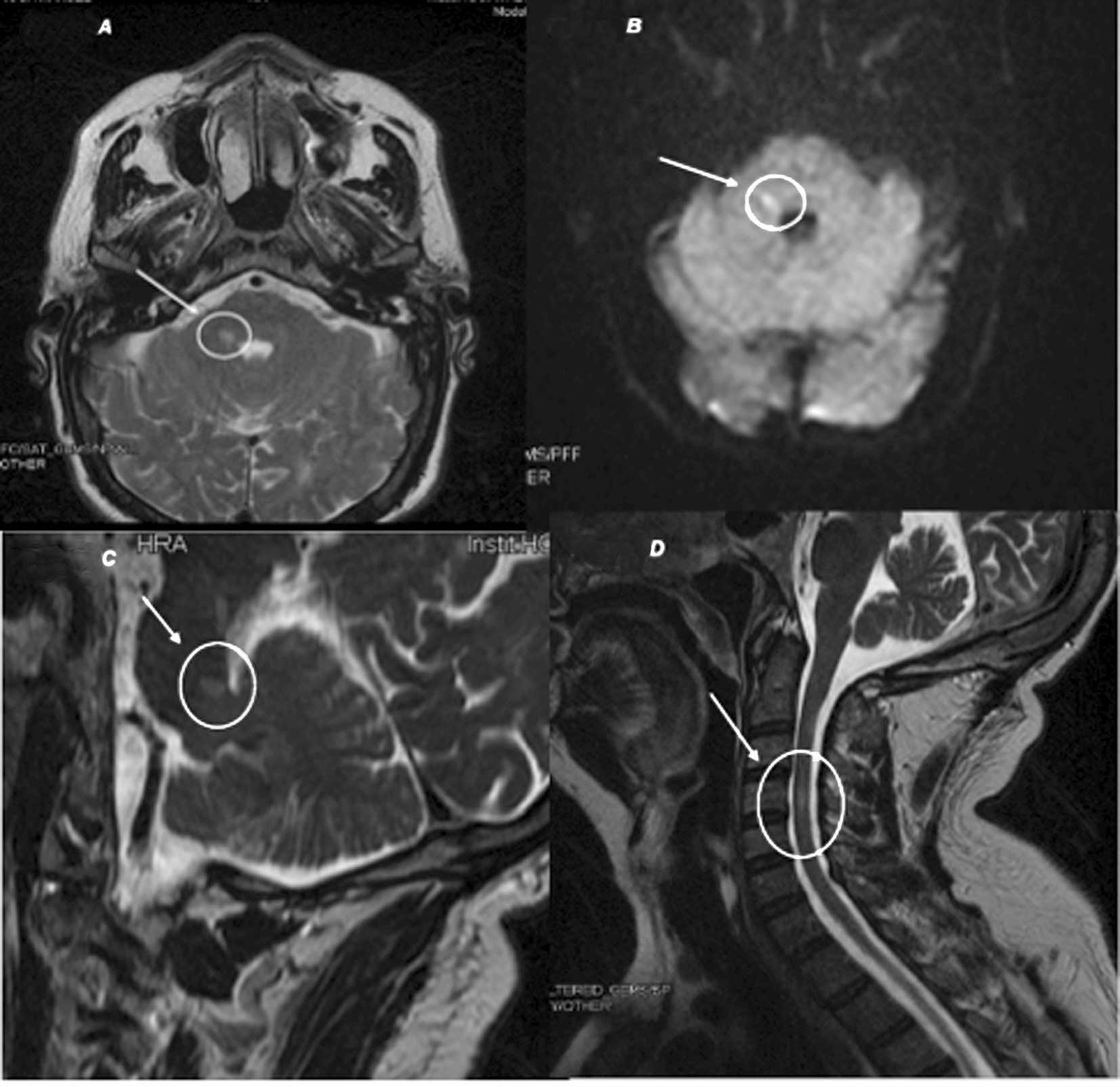
The patient's neurological symptoms became
progressively worse. The brain and spine MRI showed a small lesion
in the right protuberance with subtle changes in the DW sequence
that were enhanced following contrast infusion, and another lesion
in the cervical spinal cord that may explain the neurological
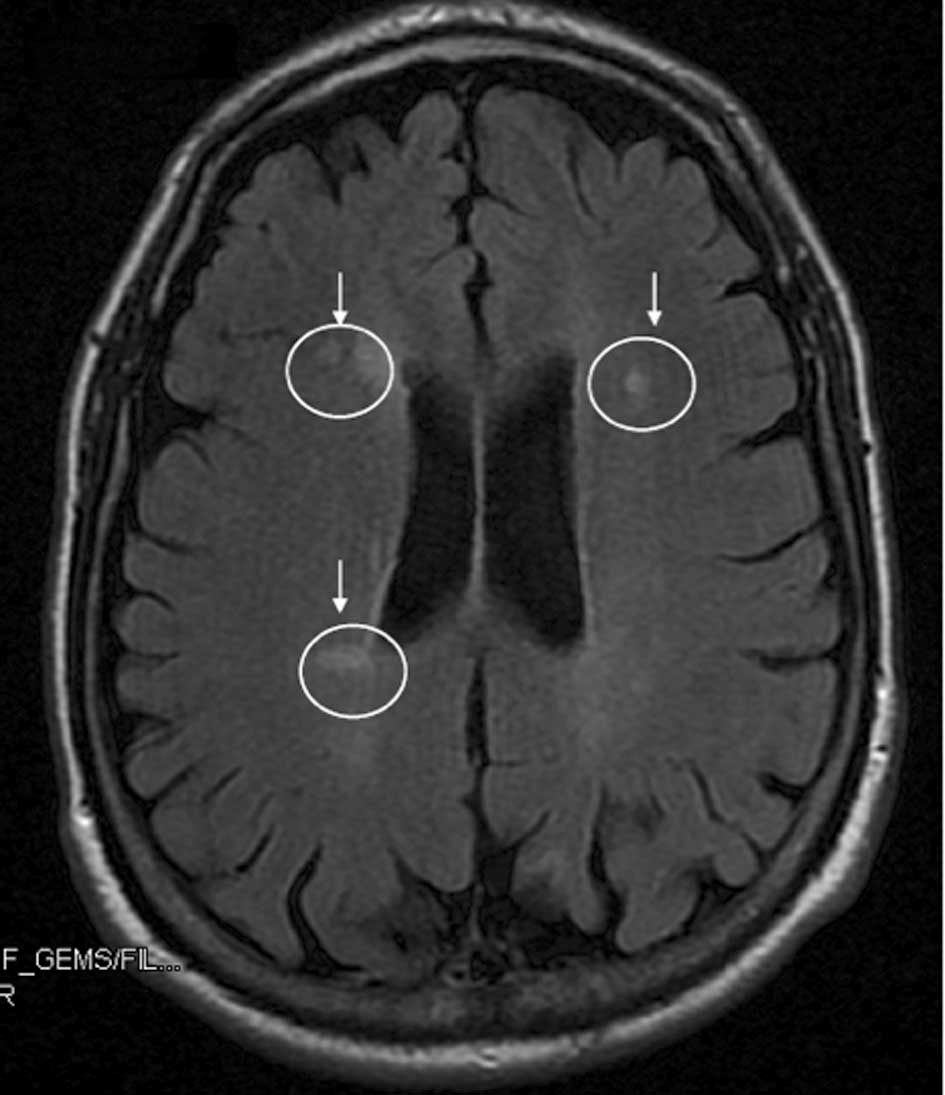
findings (Fig. 2). In addition, a
number of small subcortical lesions were found (Fig. 3). The CSF exam revealed a Tibbling
index of 1.1, protein concentration 66 mg/dl, and normal counts of
glucose and cells. A microbiological examination did not reveal any
signs of infection and three cytologies performed for malignant
cells were negative. Anti-nuclear antibodies, endothelial cytotoxic
activity and serum tests (vitamin B12, IgG, tumoral markers and
thyroid hormones) were normal. The microbiological examination
included serology for RPR and THPA. Hepatitis B virus, human
immunodeficiency virus, toxoplasmosis, citomegalovirus,
herpes-simplex virus type 6 and Varicela zoster virus, Epstein-barr
virus, mycoplasma pneumonia and Borrelia burgdorferi were normal.
Finally, since paraneoplastic encephalomyelitis is occasionally
associated with certain types of cancer, a number of onconeural
antibodies, including anti-Hu, anti-Jo, anti-Ri, anti-MA-1 and
anti-CV2, were examined to eliminate the possibility of a
neurological paraneoplastic syndrome. Presentation of the
antibodies was not demonstrated; however PNS could not be excluded
according to the accepted criteria. Corticoid treatment was
initiated with mild and transitory improvement of neurological
symptoms, which is consistent with our initial hypothesis.
This patient received three courses of cisplatin,
taxotere and 5-fluorouracil (5).
The radiological and ENT examinations showed complete response in
that no residual tumor was found in the biopsy sample. Lymph nodes
were not observed when the MRI was performed. However, the
neurological symptoms persisted, with the addition of numbness of
feet. Cisplatin-related neuropathy was confirmed by an
electromyogram study. Subsequently, administration of this
neurotoxic drug was suspended and an anti-EGFR monoclonal antibody
(Erbitux®), without neurological side effects, was
added.
The patient then underwent a chemoradiation
treatment (tomotherapy and Erbitux, concomitantly), with cutaneous
toxicity grade II. One month later, the MRI and endoscopic
examination revealed a pathologically complete response, resulting
in the patient undergoing surgery (bilateral lymph nodes
resection). The pathological examination did not reveal metastasis
in the nodes that were removed. Follow-up was conducted every 2
months and comprised an ENT examination, blood test and alternating
image test (MRI and neck CT). No evidence of relapse has been
detected thus far. However, the neurological symptoms became worse,
even after cisplatin suppression. The patient was unable to walk
independently and attended the hospital in a wheelchair.
Additionally, he reported urinary retention 2 weeks prior to the
last appointment.
Corticoides therapy did not improve the neurological
symptoms and the MRI showed an increase in lesion size. It was
concluded that our patient may have a PNS (type, encephalomyelitis)
associated with a HNC. He presented with a neurological syndrome
that is not attributable to the toxicity of cancer therapy,
cerebrovascular disease, coagulopathy, infection or toxic and
metabolic causes. The neurological diagnosis included the criteria
required to define a possible PNS, i.e., non-classical neurological
syndrome (encephalomyelitis) without onconeural antibodies, and the
cancer presents within 2 years of diagnosis.
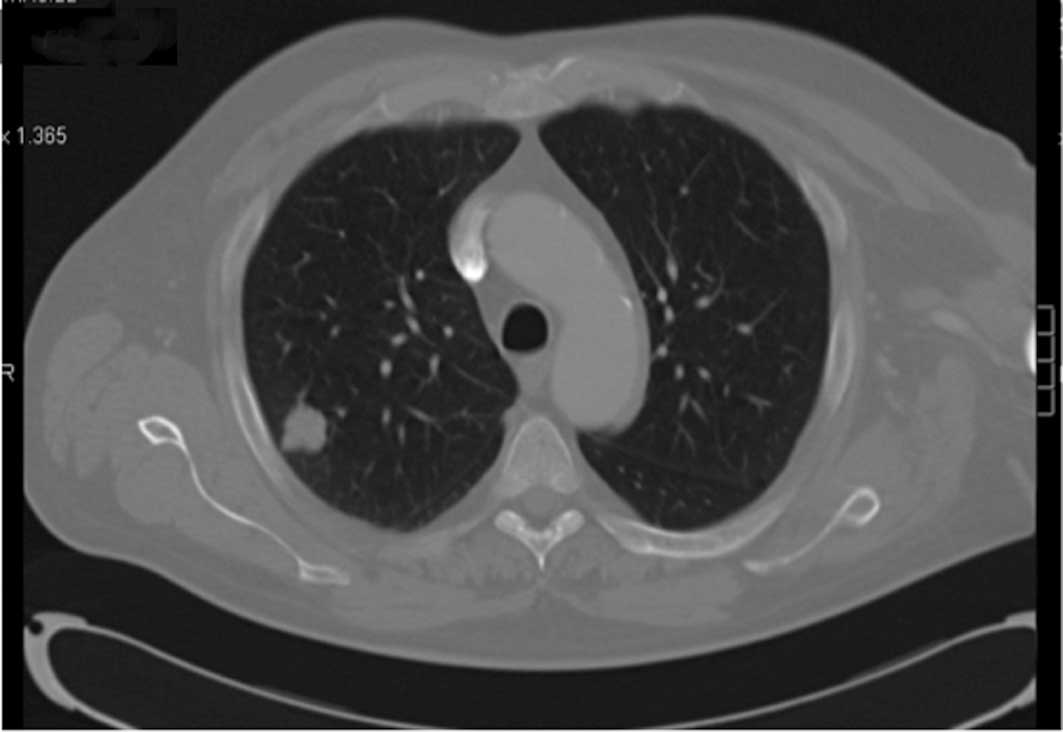
One year later, a chest CT scan showed a 3-cm nodule
in the upper right lobe. A biopsy was performed, the finding of
which were consistent with a SCLC. The work-up did not show
metastasis in any other location. Chemotherapy and radiation
treatment were commenced in another hospital due to relocation. A
partial response to the treatment was noted (Fig. 4).
Thus, we have presented the case of a patient, with
a locally advanced tonsilar carcinoma, who underwent chemoradiation
with a complete response, as well as paraneoplastic
encephalomyelitis associated with peripheral neuropathy secondary
to cisplatin administration, is presented. This is potentially the
first case of a possible PNS associated with a HNC or a
complication of a further SCLC reported in the literature.
Discussion
PNS is a rare disease occurring in less than 0.01%
of patients with cancer (1). The
current criteria for PNS were reviewed by an international panel of
neurologists (2). Paraneoplastic
encephalomyelitis is characterized by the involvement of one or
more areas, such as the hippocampus, lower brainstem, spinal cord
or dorsal root ganglia. In 75% of patients, the underlying neoplasm
is a SCLC and a majority of patients present anti-Hu, anti-CV2 or
anti-amphiphysin antibodies.
The field cancerization hypothesis is a key concept
related to the natural history of HNC. This term describes the
diffuse epithelial injury throughout the head and neck, lungs and
esophagus that results from chronic exposure to carcinogens
(3). This lesion may be responsible
for the development of a second tumor in the lungs or oesophagus in
the damaged areas. Therefore, our patient may develop a second
tumor in the lungs or in the oesophagus as a consequence of this
process.
According to the previous criteria defining PNS, the
neurological syndrome that we have presented may be associated with
an underlying lung cancer instead of a HNC. As previously
mentioned, lung cancer is more frequently associated with PNS, in
particular, SCLC. Therefore, the presence of a PNS in our patient
may potentially be explained by the fact that either the second
tumor is a definite PNS associated with a HNC or it is a possible
PNS associated with future lung cancer in a patient with high risk,
according to the ‘field cancerization’ hypothesis. In the case that
we consider the tumor to be a paraneoplastic syndrome associated
with HNC, this would be the first such reported case. HNC outcome
did not show a local or distant recurrence during the 1 year of
follow-up.
One year later, a second primary tumor was noted in
the lung. This tumor was a SCLC, which is frequently associated
with paraneoplastic syndrome tumors. Therefore, this paraneoplastic
syndrome may be explained as a complication prior to the appearance
of SCLC.
In conclusion, we examined a patient who
concurrently presented a neurological syndrome of encephalomyelitis
and a tonsilar mass with a biopsy consistent with carcinoma.
According to the clinical and radiological findings, as well as the
clinical outcome, we conclude that this mass is a possible PNS.
However, we cannot assert whether it is a PNS associated with a HNC
or a possible PNS that resulted in the development of a second
tumor in the lungs as a result of field cancerization.
Acknowledgements
We thank Dr Dominguez from the Pathology Department
in our hospital for her expert contribution.
References
|
1
|
Licitra L, Bernier J, Grandi C, et al:
Cancer of the oropharynx. Crit Rev Oncol Hematol. 41:107–122. 2001.
View Article : Google Scholar
|
|
2
|
Graus F, Delattre JY, Antoine JC, et al:
Recommended diagnostic criteria for paraneoplastic neurological
syndromes. J Neurol Neurosurg Psychiatry. 75:1135–1140. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Honnorat J and Antoine JC: Paraneoplastic
neurological syndromes. Orphanet J Rare Dis. 22:1–8. 2007.
|
|
4
|
Scheid R, Honnorat J, Delmont E, et al:
Neurological disorders in patients with small cell lung cancer.
Cancer. 60:2275–2283. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Vermorken JB, Remenar E, van Herpen C, et
al: Cisplatin, fluorouracil, and docetaxel in unresectable head and
neck cancer. N Engl J Med. 357:1704–1715. 2007. View Article : Google Scholar : PubMed/NCBI
|