Introduction
Exocrine pancreatic adenocarcinoma is the fourth
most common cause of cancer-related mortality in both genders in
the US (1). Surgery is the only
potentially curative option but is confined to patients with
localized disease. Therapeutic options in patients not eligible for
resection are limited to chemotherapy (CHT) or chemoradiotherapy
(CRT). However, the prognosis is poor, ranging from 6 to 10 months
in locally advanced stage disease.
Locally advanced pancreatic cancer (LAPC) is defined
as a tumour localized in the pancreas, without metastatic spread,
but directly encasing the adjacent arteries, such as the coeliac
axis and superior mesenteric artery, or occluding the superior
mesenteric vein, portal vein or mesenteric-portal vein confluence
(2). The optimal treatment of LAPC
remains to be elucidated. However, enhancement of clinical benefit,
disease control rate (DCR) and survival, and an increase of the
resectability rate in borderline resectable disease are crucial.
Traditionally, CRT was considered to be the treatment of choice for
LAPC. However, despite the known superiority of CRT compared to
radiotherapy (RT) alone and best supportive care (3,4), no
evidence is available to prove that the beneficial effect of CRT is
superior to that of CHT alone (3–9).
Although pancreatic tissue exhibits poor radiosensitivity, the
addition of RT is designed to obtain local disease control and an
early palliation of symptoms. Numerous studies have tested the
sequential schedule of CRT as induction CHT followed by CRT, with
favourable results (10–16). Thus, the association of various
therapeutic techniques including CRT, surgery and locoregional
treatment may be introduced in clinical practice to enhance the DCR
in selected patients in multimodal treatment.
In this study, 2 patients with LAPC received a
multimodal treatment starting with gemcitabine (GEM)-CHT followed
by CRT, with concurrent radiosensitizer bi-weekly GEM, in order to
prepare the patients for surgery.
Patients and methods
Case 1
In August 2008, a 63-year-old male was diagnosed
with locally advanced stage and poorly differentiated carcinoma
originating from the head of the pancreas. The Eastern Cooperative
Oncology Group (ECOG) performance status was 2. The tumour markers
[carcinoembryonic antigen (CEA) and CA19.9] were negative. Since
the patient was considered unfit for surgery, the tumour was
treated medically. A sequential CHT followed by CRT was scheduled
in September 2008. However, the treatment was discontinued due to
toxicity, in the form of fever and nausea, during the induction CHT
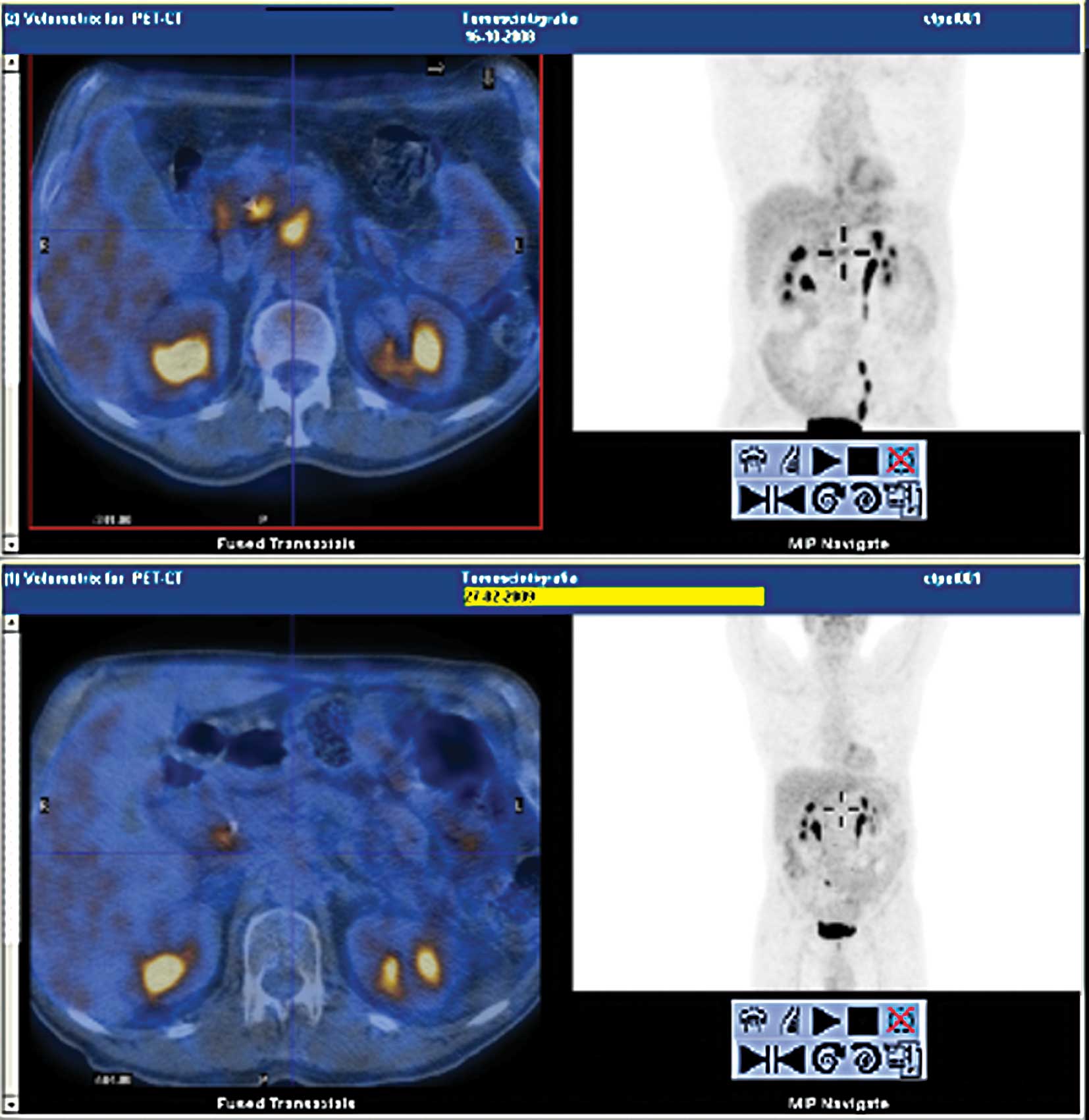
period. In February 2009, an abdominal computed tomography (CT)
scan showed a significant reduction of the pancreatic tumour mass
and a fluorodeoxyglucose positron-emission tomography/CT
(18CT-PET) revealed a complete metabolic response
(Fig. 1). Consequently, the patient
underwent surgery. Since the tumour involved the coeliac axis and
superior mesenteric artery, surgery was confined to explorative
laparotomy. In July 2009, a CT scan showed a further reduction of
tumour size, and 18CT-PET confirmed the complete
metabolic response. The ECOG performance status was 0. In agreement
with the patient, treatment involved the maintenance of GEM at 1000
mg/mq on days 1, 8 and 15 of a 28-day cycle from July 2009 to
February 2010, when a single hepatic metastasis developed, 18
months following the LAPC diagnosis. A slight increase in CEA was
found (6.7 ng/ml). Thus, CHT with gemcitabine and oxaliplatin
(GEMOX schedule) commenced from March 2010. During treatment, a
case of grade 3 neutropenia occurred.
Case 2
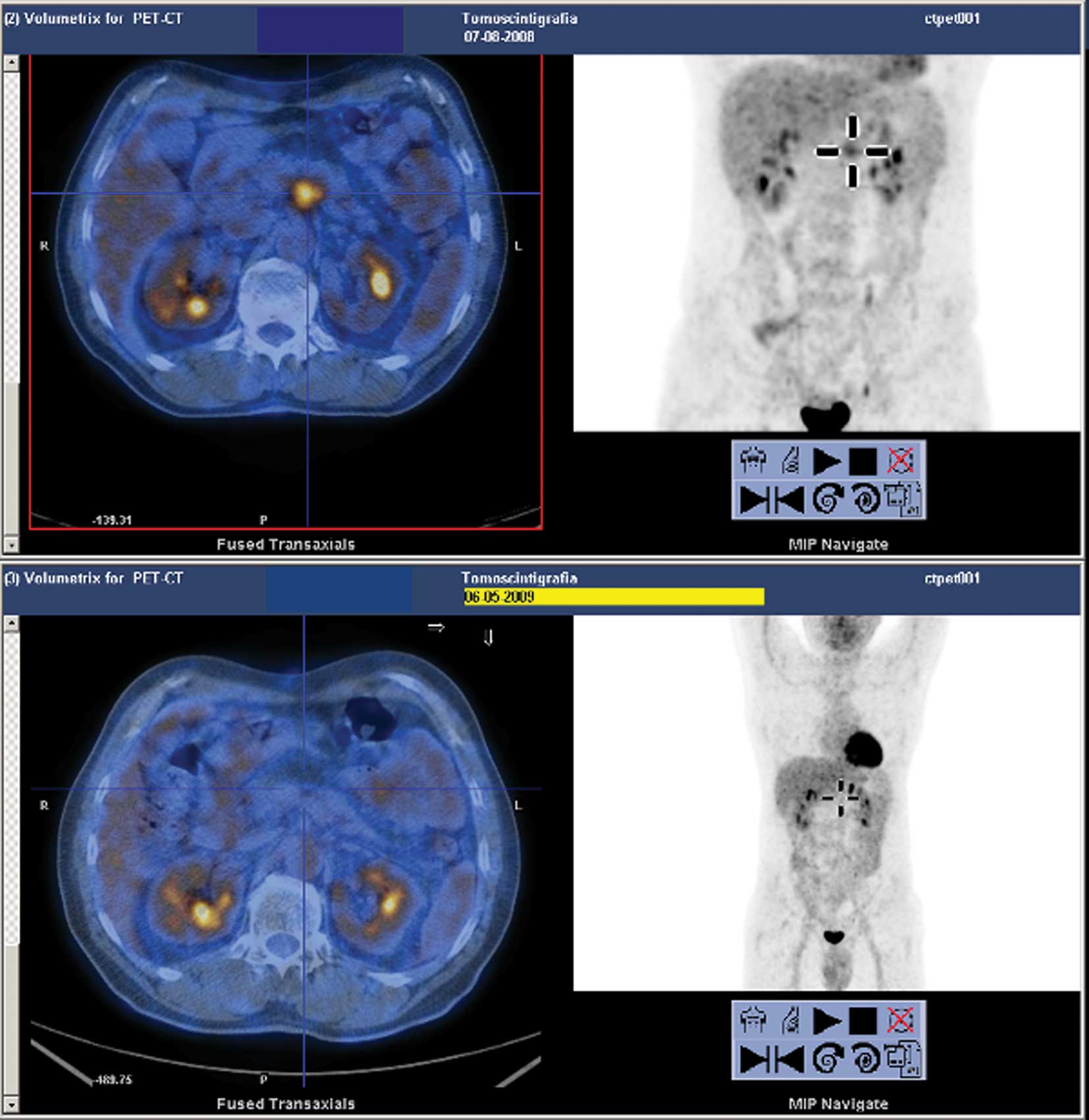
In July 2008, a 63-year-old male was diagnosed with
a locally advanced adenocarcinoma of the pancreatic body. The ECOG
performance status was 2. The tumour marker CA19.9 was 143 U/ml.
The patient was considered unfit for surgery. Consequently, the
tumour was medically treated. From July to October 2008 a
sequential CHT followed by CRT was performed without major
toxicities. In November 2008, a CT scan revealed a slight reduction
in tumour size (30 vs. 39 mm), but coeliac axis tumour involvement
persisted. Since the CA19.9 value remained high, the patient was
treated with CHT according to the GEMOX schedule from January to
September 2009. Further tumour shrinkage (28 vs. 39 mm) and a
complete metabolic response were noted. The CA19.9 value decreased
to 29 U/ml. In November 2009, the patient underwent radiofrequency
ablation (RFA) with a positive locoregional response and a
normalization of CA19.9 serum values. In March 2010, the patient
resumed CHT according to the GEMOX schedule due to an increase in
CA19.9 (345 U/ml), despite negative a 18CT-PET
evaluation. CHT was discontinued in May 2010 and a CT scan revealed
stable disease: serum CA19.9 levels had decreased to 135 U/ml and
18CT-PET showed minimal pathological uptake of the
tracer at the mesenteric node and in the lung nodules.
Results and Discussion
This study evaluated clinical cases of patients
characterized by long-term DCR and metabolic tumour deactivation,
as noted by a negative 18CT-PET, obtained first by the
early sequential CRT schedule, and followed by further treatment
modality (Figs. 1 and 2). Patient 1 developed a single hepatic
metastasis 18 months after LAPC diagnosis, following upfront
sequential CRT and the first line CHT. The patient remained alive
at 23 months and in good clinical condition. RFA appeared to
prolong disease control in patient 2. This patient developed
metastasis 24 months after the LAPC diagnosis. The two patients
therefore experienced clinical benefits.
It is known that the optimal treatment of patients
with LAPC has yet to be elucidated. CHT alone is the treatment of
choice in the UK, whereas CRT is the standard modality in the USA.
Numerous trials have confirmed the enhanced efficacy of the CRT,
although the survival benefit of combination treatment appears to
be moderate (Table I).
Discrepancies in the results of two phase III studies were noted
(8,9). Loehrer et al showed a slightly
longer survival in patients treated with CRT with concurrent GEM
vs. GEM alone (11 vs. 9.4 months, p=0.044) (8). On the other hand, the Fédération
Francophone de Cancérologie digestive (FFCD) and the Société
Francophone de Radiothérapie Oncologique (SFRO) study proved that
GEM was more favourable than CRT with 5-fluorouracil and cisplatin
followed by GEM (13 vs. 8.6 months, p=0.03) (9).
 | Table IChemotherapy vs. chemoradiotherapy
studies in locally advanced pancreatic cancer. |
Table I
Chemotherapy vs. chemoradiotherapy
studies in locally advanced pancreatic cancer.
| Authors | Refs. | Phase | Patients | Regimen | OS (mo) | p-value
OS | PFS (mo) | p-value
PFS | 1 (ii) y
OS rate |
|---|
| Hazel | (5) | III | 30 (all) | CHT: 5FU 500mg/mq/wk
bolus and methyl CCNU 100 mg/mq/6 wk until progression vs. CRT: 46
Gy and 5FU mg/mq/wk bolus followed by maintenance CHT | 7.8 | | | | |
| 7.3 |
| Klaassen | (6) | III | 47 | CHT: 5FU 600 mg/mq/wk
until disease progression vs. CRT: 4000 rad with concurrent 5FU 600
mg/mq the first three days followed by maintenance 5FU | 8.2 | | | | |
| 44 | 8.3 |
| Gastrointestinal
tumor study group | (7) | III | 43 (all) | CHT: 5FU 600 mg/mq
bolus on days 1, 8, 29 and 36 plus streptomycin 1 g/mq/8 wk plus
MMC 10 mg/mq/8 wks vs. CRT: 54 Gy with concurrent 5FU 350 mg/mq
bolus on days 1–3 and 36–38 followed by maintenance CHT | 7.4 | | | | |
| 9.7 |
| Loehrer | (8) | III | 74 (all) | CHT: GEM 1000
mg/mq/wk on days 1, 8 and 15 vs. CRT: 50.4 Gy with concurrent GEM
600 mg/mq/wk plus maintenance GEM 1000 mg/mq/wk on days 1, 8 and
15 | 9.2 | | 6.1 | | |
| 11 | 0.044 | 6.3 | 0.34 |
| Chauffert | (9) | III | 54 | CHT: GEM 1000
mg/mq/wk for 7 wks vs. CRT: 60 Gy with concurrent 5FU 300 mg/mq/day
days 1–5 for 6 wks and CDDP 20 mg/mq days 1–5 during wks 1 and
5 | 13 | | | | 53% |
| 52 | 8.6 | 0.03 | 32% |
In the last decade, CHT and RT have been tested in a
sequential modality comprising an upfront mono- or
multi-chemotherapy, followed by CRT, or maintenance CHT (Table II). The most significant data on
the efficacy of induction CHT, derived from two large retrospective
analyses and a phase II trial, proved the superiority of the
sequential regimen compared to CRT or CHT. Krishnan et al
(11) showed increased overall
survival (OS) in patients pretreated with GEM-based CHT and CRT
compared to patients who received only CRT (OS: 11.9 vs. 8.5
months, p<0.001; PFS: 6.4 vs. 4.2 months, p<0.001). On the
other hand, the GERCOR analysis showed an OS of 15 months in
patients pretreated with various CHT regimens prior to CRT with
concurrent fluoropyrimidine, whereas OS was only 11 months in the
CHT-only arm (p=0.0009) (12). In a
phase II trial, Hudson et al (15), confirmed the positive effect of
upfront CHT prior to CRT, achieving an OS of 15.3 months compared
to 9.2 months in frontline CRT (p=0.005).
 | Table IIInduction chemotherapy followed by
chemoradiotherapy studies in locally advanced pancreatic
cancer. |
Table II
Induction chemotherapy followed by
chemoradiotherapy studies in locally advanced pancreatic
cancer.
| Authors | Refs. | Phase | Patients | Regimen | OS (mo) | p-value
OS | PFS (mo) | p-value
PFS | 1 (ii) y
OS rate |
|---|
| Epelbaum | (10) | II | 20 | CHT: GEM 1000
mg/mq/wk for 7 wks (i) followed by CRT 50.4 Gy with concurrent GEM
400 mg/mq for 2 cys (ii) followed by maintenance GEM (iii) | 8 (median) | | | | 1y:30% (median) |
| Krishnan | (11) | Retrospective
analysis | 323 | CHT: GEM based for
2.5 mo (i) followed by CRT 30 Gy with concurrent 5FU 300 mg/mq/day
or CAPE 1600–1800 mg/mq/day or GEM 350 to 400 mg/mq/wk (ii) | 9 (median) | <0.001 | 5 (median) | <0.001 | 2y:9% (median) |
| 11.9 (i+ii) | 6.4 (i+ii) |
| 8.5 (ii) | 4.2 (ii) |
| Huguet | (12) | Retrospective
analysis | 181 | CHT: Various regimens
for 3 mo (i) followed by CRT 55 Gy with concurrent 5-FU 250
mg/mq/day for 7 wks (ii); or followed by CHT (iii) | 11.4 (median) | 0.0009 | 6.3 (median) | 0.005 | 46% (median) |
| 15 (i+ii) | 10.8 (i+ii) | 65.3% (i+ii) |
| 11 (i+iii) | 7.4 (i+iii) | 47.5% (i+iii) |
| Moureau-Zabotto | | II | 59 | CHT: GEMOX for 4 cys
(i) followed by CRT 45 Gy over 5 wks plus 10 Gy boost with
concurrent 5FU 250 mg/mq as continuous infusion and OHP 60 mg/mq/wk
(ii) | 12.2 (median) | | 7.6 (median) | | 1y:52.1%
(median) |
| GERCOR | (13) | 12.6 (i+ii) | 9.4 (i+ii) | 2y:20.8%
(median) |
| Nakachi | (14) | II | 20 | CHT: GEM and S-1 for
4 cys (i) followed by CRT 30 Gy with concurrent GEM 250 mg/mq (ii)
followed by maintenance GEM for 2 cys (iii) | 14.4 (median) | | 8.1 (median) | | 54.2% (median) |
| Hudson | (15) | II | 43 | CHT: GEM or GEMCAPE
for 3–4 cys (i) followed by CRT 45–50.4 Gy with concurrent GEM 300
mg/mq/wk (ii) | 9.2 (median) | | | | 34.1% (median) |
| 9.2 (i) | | | 30.8% (i) |
| 15.3 (i+ii) | 0.005 | 12.7 (i+ii) | 74.5% (i+ii) |
| Reni | (16) | II | 91 | PEFG/PEXG or PDXG
for 6 mo (i) followed by CRT 50–60 Gy with concurrent 5FU 250
mg/mq/day or CAPE 1250 mg/mq/day or GEM 150–200 mg/mq/wk (ii) | 16.2 (median) | | 9.9 (median) | | |
No consensus exists on an ideal schedule for
sequential treatment. We used GEM-based CHT in the systemic
induction phase as compared to the CRT phase (10,11,13–16),
whereas in the majority of studies the concurrent drug in the CRT
phase was 5-fluorouracil or derivates thereof (11–13,16).
Although the survival improvement was poor, the tumour
resectability rate was increased by RT with concurrent GEM vs
5-fluorouracil in LAPC (17). No
certain dose of GEM with concurrent RT (8,10,11,14–16)
was defined; during conventional radiation the safe weekly dose of
GEM should remain at <400 mg/mq, whereas this dose is not
effective for systemic disease control. Instead, certain studies
tested a lower dosage of GEM twice weekly as a radiosensitizer
enhancer with positive results. For the same purpose, we treated
our patients with bi-weekly 50 mg/mq concurrent to RT (18).
The rationale of sequential CRT is based on the
early metastatic spread of LAPC: patients with disease that is
still localized are likely to complete treatment with CRT, whereas
patients with disease progression during the induction CHT may
benefit more from a different CHT regimen. Theoretically the first
CHT phase is utilized to select patients on the basis of their
biological disease malignancy, and adopt the therapeutic strategy
best tailored to the individual patient. The same rationale can be
extended to the neo-adjuvant setting in that despite the failure of
neo-adjuvant intent in our patients, certain authors promote the
sequential schedule since it appears to enhance the selection of
patients with borderline resectable LAPC (10,16,17).
This promotion is crucial in increasing secondary resectability
rate, when the bulk of the disease can be reduced, and avoiding
surgery in patients becoming rapidly metastatic.
Conversely, induction CHT followed by CRT in our
patients appeared to enhance the clinical benefit rate and DCR when
combined with further treatment. In particular, the addition of RFA
appeared to extend the metastasis-free survival time to 24 months
in patient 2, although these data have yet to be elucidated in the
available literature (19,20). To the best of our knowledge, the
multimodal treatment may be considered in selected patients who
obtain a protracted stable disease due to a number of treatment
techniques employed at various stages of disease.
Our cases on sequential CHT and CRT may serve as a
useful starting point for critical consideration. However, numerous
issues have yet to be elucidated. These issues include which
chemotherapeutic scheme is ideal in the induction phase and the
amount of drugs to be administered; the length of time for which
patients should receive frontline CHT to improve the selection for
CRT; which drugs should be administered concurrently with
radiotherapy; as well as the best dosage and purpose. Therefore,
phase III studies are required to better define the role of
sequential CHT and CRT in LAPC patients since patients with
borderline resectable cancer may benefit from better selection for
surgery, whereas patients with unresectable disease may experience
enhanced DCR.
References
|
1
|
Jemal A, Siegel R, Ward E, Hao Y, Xu J and
Thun MJ: Cancer Statistics. CA Cancer J Clin. 59:225–249. 2009.
|
|
2
|
Varadhachary GR, Tamm EP, Abbruzzese JL,
Xiong HQ, Crane CH, Wang H, Lee JE, Pisters PW, Evans DB and Wolff
RA: Borderline resectable pancreatic cancer: definitions,
management, and role of preoperative therapy. Ann Surg Oncol.
13:1035–1046. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yip D, Karapetis C, Strickland A, Steer CB
and Goldstein D: Chemotherapy and radiotherapy for inoperable
pancreatic cancer. Cochrane Database Syst Rev. 3:CD0020932006.
|
|
4
|
Sultana A, Tudur Smith C, Cunningham D,
Starling N, Tait D, Neoptolemos JP and Ghaneh P: Systematic review,
including meta-analysis, on the management of locally advanced
pancreatic cancer using radiation/combined modality therapy. Brit J
Cancer. 96:1183–1190. 2007. View Article : Google Scholar
|
|
5
|
Hazel JJ, Thirlwell MP, Huggins M,
Maksymiuk A and MacFarlane JK: Multi-drug chemotherapy with and
without radiation for carcinoma of the stomach and pancreas: a
prospective randomized trial. J Can Assoc Radiol. 32:164–165.
1981.PubMed/NCBI
|
|
6
|
Klaassen DJ, MacIntyre JM, Catton GE,
Engstrom PF and Moertel CG: Treatment of locally unresectable
cancer of the stomach and pancreas: a randomized comparison of
5-fluorouracil alone with radiation plus concurrent and maintenance
5-fluorouracil – an Eastern Cooperative Oncology Group study. J
Clin Oncol. 3:373–378. 1985.PubMed/NCBI
|
|
7
|
Gastrointestinal tumour study group.
Treatment of locally unresectable carcinoma of the pancreas:
comparison of combined-modality therapy (chemotherapy plus
radiotherapy) to chemotherapy alone. J Natl Cancer Inst.
80:751–755. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Loehrer PJ, Powell ME, Cardenes HR, Wagner
L, Brell JM, Ramanathan RK, Crane CH, Alberts SR and Benson AB;
Eastern Cooperative Oncology Group. A randomized phase III study of
gemcitabine in combination with radiation therapy versus
gemcitabine alone in patients with localized, unresectable
pancreatic cancer: E4201. J Clin Oncol. 26214s(suppl)2008.
|
|
9
|
Chauffert B, Mornex F, Bonnetain F, et al:
Phase III trial comparing intensive induction chemoradiotherapy (60
Gy, infusional 5-FU and intermittent cisplatin) followed by
maintenance gemcitabine with gemcitabine alone for locally advanced
unresectable pancreatic cancer. Definitive results of the 2000–01
FFCD/SFRO study. Ann Oncol. 19:1592–1599. 2008.PubMed/NCBI
|
|
10
|
Epelbaum R, Rosenblatt E, Nasrallah S,
Faraggi D, Gaitini D, Mizrahi S and Kuten A: Phase II study of
gemcitabine combined with radiation therapy in patients with
localized, unresectable pancreatic cancer. J Surg Oncol.
81:138–143. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Krishnan S, Rana V, Janjan NA,
Varadhachary GR, Abbruzzese JL, Das P, Delclos ME, Gould MS, Evans
DB, Wolff RA and Crane CH: Induction chemotherapy selects patients
with locally advanced, unresectable pancreatic cancer for optimal
benefit from consolidative chemoradiation therapy. Cancer.
110:47–55. 2007. View Article : Google Scholar
|
|
12
|
Huguet F, André T, Hammel P, Artru P,
Balosso J, Selle F, Deniaud-Alexandre E, Ruszniewski P, Touboul E,
Labianca R, de Gramont A and Louvet C: Impact of chemoradiotherapy
after disease control with chemotherapy in locally advanced
pancreatic adenocarcinoma in GERCOR phase II and III studies. J
Clin Oncol. 25:326–331. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Moureau-Zabotto L, Phélip JM, Afchain P,
et al: Concomitant administration of weekly oxaliplatin,
fluorouracil continuous infusion, and radiotherapy after 2 months
of gemcitabine and oxaliplatin induction in patients with locally
advanced pancreatic cancer: a Group Coordinateur Multidisciplinaire
en Oncologie Phase II Study. J Clin Oncol. 26:1080–1085. 2008.
|
|
14
|
Nakachi K, Furuse J, Kinoshita T,
Kawashima M, Ishii H, Ikeda M, Mitsunaga S and Shimizu S: A phase
II study of induction chemotherapy with gemcitabine plus S-1
followed by chemoradiotherapy for locally advanced pancreatic
cancer. Cancer Chemother Pharmacol. 66:527–534. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hudson E, Hurt C, Mort D, Brewster AE,
Iqbal N, Joseph G, Crosby TD and Mukherjee S: Induction
chemotherapy followed by chemoradiation in locally advanced
pancreatic cancer: an effective and well-tolerated treatment. Clin
Oncol. 22:27–35. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Reni M, Cereda S, Balzano G, Passoni P,
Rognone A, Zerbi A, Nicoletti R, Mazza E, Arcidiacono PG, Di Carlo
V and Villa E: Outcome of upfront combination chemotherapy followed
by chemoradiation for locally advanced pancreatic adenocarcinoma.
Cancer Chemother Pharmacol. 64:1253–1259. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Crane CH, Abbruzzese JL, Evans DB, et al:
Is the therapeutic index better with gemcitabine-based
chemoradiation than with 5-fluorouracil-based chemoradiation in
locally advanced pancreatic cancer? Int J Radiat Oncol Biol Phys.
52:1293–1302. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Magnino A, Gatti M, Massucco P, Sperti E,
Faggiuolo R, Regge D, Capussotti L, Gabriele P and Aglietta M:
Phase II trial of primary radiation therapy and concurrent
chemotherapy for patients with locally advanced pancreatic cancer.
Oncology. 68:493–499. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Girelli R, Frigerio I, Salvia R, Barbi E,
Tinazzi Martini P and Bassi C: Feasibility and safety of
radiofrequency ablation for locally advanced pancreatic cancer. Br
J Surg. 97:220–225. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
20
|
Casadei R, Ricci C, Pezzilli R, Serra C,
Calculli L, Morselli-Labate AM, Santini D and Minni F: A
prospective study on radiofrequency ablation locally advanced
pancreatic cancer. Hepatobiliary Pancreat Dis Int. 9:306–311.
2010.PubMed/NCBI
|