1. Introduction
Multifocal epithelial hyperplasia (MEH) is an
uncommon disease characterized by the proliferation on the oral
mucosa of multiple papulonodular lesions, which are smooth, soft on
palpation and generally asymptomatic (1–5). It
has mainly been observed among isolated groups of native Indians in
North, Central and South America and in other very small population
groups in Europe and Africa (6–13).
Although previously described by other authors, the
first case report was published by Dr Heck and his team in 1965,
and it is therefore also known as Heck’s disease (14). In the same year, Witkop et al
reported 11 cases with the same diagnosis among Xavante Indians in
Brazil, a Ladino population in El Salvador and Quiche-Mayan Indians
in Guatemala (13). Single cases
were subsequently reported in Polynesia (15), Puerto Rico (16), in an adult female Caucasian
(17), and in small population
groups in Bolivia, Paraguay, Peru, Colombia and Mexico (12,18–20).
The disease has also been found in primates and in a rabbit, which
presented with macroscopic and microscopic characteristics similar
to those of humans with the disease (21–25).
2. Human papillomavirus and other
etiological factors
The main etiological factor for this disease is the
presence of the human papillomavirus (HPV), which belongs to a
varied group of DNA viruses from the Papillomaviridae
family. Similar to all viruses in this family, it only establishes
productive infections in the stratified epithelium of skin and
mucosa of humans and certain animals (26).
In 1971, Praetorious-Clausen and Willis first
revealed HPV particles in MEH, using an electron microscope to
study five samples from patients in Greenland (27). One year later, Hanks et al
reported the same findings in a 5-year-old child from Cochabamba in
Bolivia (28). This association was
subsequently confirmed by other authors, including Kuffer and Perol
in 1976, in the first reported case in France (29), and Kulhwein et al in 1981
(30).
Approximately 200 different types of HPV have been
identified, mostly asymptomatic (26). In 1983, Pfiser et al related
the disease to HPV-13 after examining a sample from a Turkish
patient (31). Beaudenon et
al confirmed this specific association in 10 patients of
various origins and also observed a correlation with HPV-32
(32). Over the past few years,
immunohistochemical and in situ hybridization studies have
shown MEH to be closely related to HPV-13 and HPV-32, while certain
studies have also demonstrated the presence of HPV-1, HPV-6, HPV-11
and HPV-16 in these patients (33–36).
Genetic predisposition is also frequently mentioned
as an etiological factor for MEH (13,14).
The familial presence of the disease was first highlighted by Gómez
et al in Columbia in 1969 (19). In 1993, Premoli-De-Percoco found
that members of six generations of a Venezuelan family had been
diagnosed with MEH and concluded that the disease has a genetic
basis, noting that all generations were born in a small village
with a very strong American Indian genetic component (37). In 2004, García-Corona et al
assessed the effect of genetics by studying the association of
HLA-DR4 alleles (DRB1*0404) with HPV infection, yielding
results in support of the genetic basis of MEH (4).
Nutritional deficiencies and environmental factors
have been proposed by certain authors (15), including poverty and the lack of
hygiene (38). The role of
immunosuppression is also under investigation. Feller et al
reported the case of a seropositive child undergoing highly active
antiretroviral treatment who was also diagnosed with MEH and
successfully treated by diode laser; the authors suggested that the
anti-HIV therapy may have been responsible for the disease
(39). In another report on an
HIV-positive patient with MEH, Marvan et al concluded that
the correlation between the immune state and HPV infection
warranted further investigation (40).
3. Diagnosis, prognosis and treatment
The diagnosis of MEH is mainly based on the clinical
features of the lesions and a biopsy pathology report. Since the
discovery of HPV particles in these lesions in 1970, there has been
an increase in the diagnostic use of molecular biology techniques,
including in situ DNA hybridization and polymerase chain
reaction, which have proven highly useful in identifying the types
of HPV involved (2,5,27,28,31,41).
The prognosis of the disease is good, given that
most lesions remit spontaneously, but periodical clinical
follow-ups are considered crucial (42,43).
Lesions that do not remit or cause functional and/or aesthetic
problems may be removed by various means (44–48),
including surgery, cryotherapy, electrocoagulation, laser, chemical
agents (e.g., retinoic acid) or immunostimulants (e.g.,
interferon).
4. Criteria and variables included
Inclusion criteria
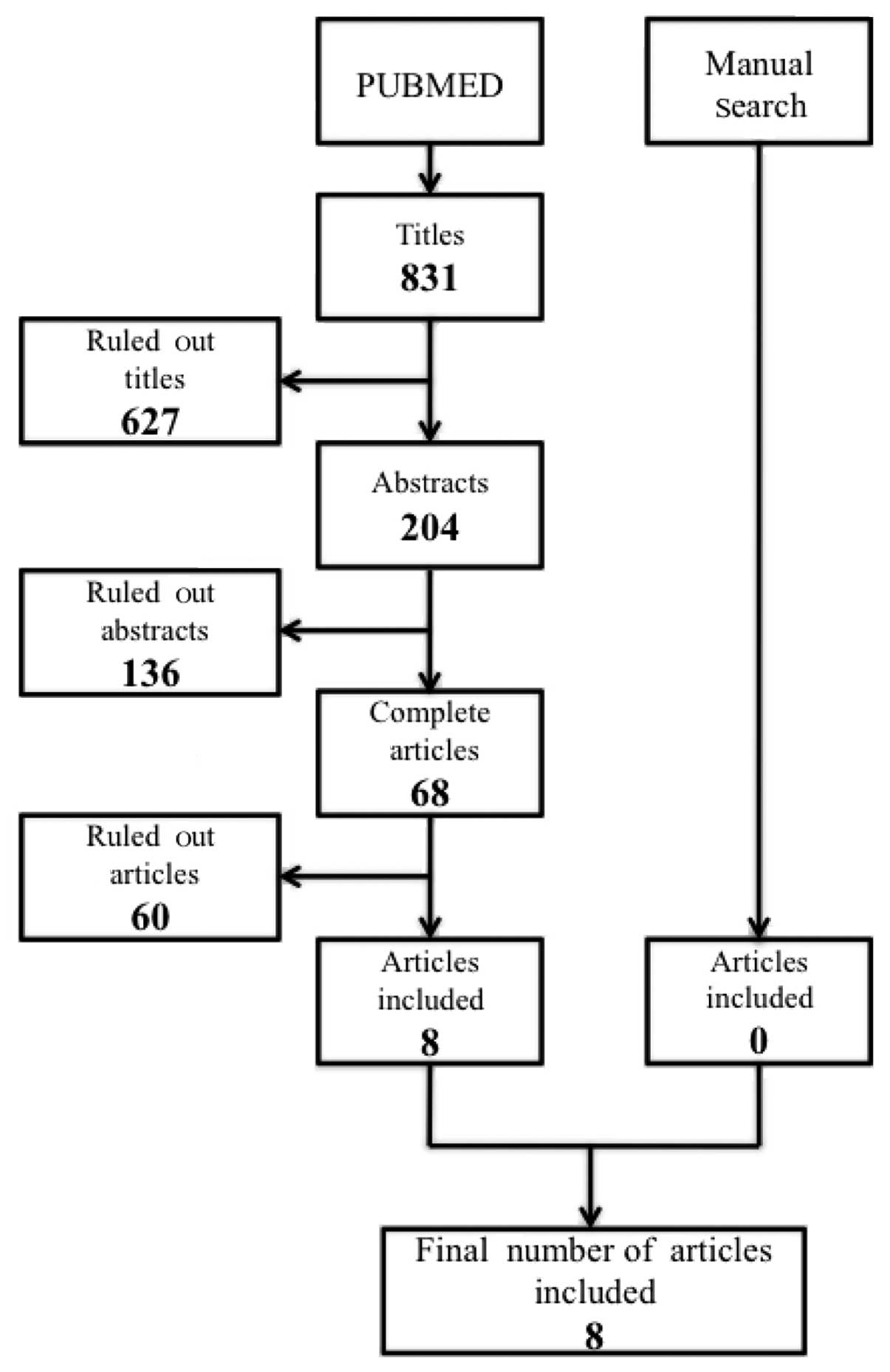
The PubMed database was used to search the
international literature up to April 2011, for the following key
words: Focal epithelial hyperplasia, multifocal epithelial
hyperplasia, Heck’s disease, papillomavirus infections, HPV-13 and
HPV-32. The search was not limited by publication year due to the
scant information on the disease. Out of a total of 831 articles
(in English, German and Spanish), 204 were initially selected for
possible inclusion. After studying the abstracts, 68 relevant
articles that could be downloaded via the Internet were selected,
and a final sample of eight articles was included in the present
review after applying the following inclusion criteria (Fig. 1): i) They could be any type of
publication with the exception of single case reports, ii) they had
to be in vivo studies, iii) the objectives had to include
the description of the clinical characteristics and etiology of MEH
and/or the epidemiology of the disease, iv) they could report on
any clinical situation, including the presence of another disease
with the exception of cancer, v) the complete text of the articles
had to be available, and vi) all publication dates up to April 2011
could be included.
Study variables
In an initial analysis, we gathered and analyzed the
main variables related to the epidemiology of EH, including the
place of origin, geographic location, gender and age.
5. Findings pertaining to multifocal
epithelial hyperplasia
There have been few studies on the epidemiology and
incidence of MEH, attributable in part to its low incidence. The
largest number of cases has been observed in Central America, South
America and Mexico. The disease is less prevalent among individuals
in Asia and is even more rare among Caucasian and Black
populations.
In 1965, Witkop and Niswander (13) and Archard et al (14) conducted the first epidemiological
studies on American Indians, finding a predisposition for the
disease in individuals in the first and second decade of life, with
the lower lip being the most frequent localization. However,
whereas they found no significant gender difference, observing a
larger number of males with the disease, Archard et al
reported a female:male ratio of 4:1 (13,14).
In a subsequent study on Eskimos in Greenland,
Clausen et al found no significant gender differences.
Furthermore, in contrast to previous studies, they found that the
disease could also appear in adults, with an overall age range of 2
to 79 years, and that more than 50% of lesions were localized on
the tongue (49). In a similar
study, Henke et al found no significant gender or age
differences and confirmed the possible presence of the disease in
adults, reporting an age range for sufferers of 22 to 85 years
(50).
In 1994, Carlos and Sedano studied a sample of 110
patients diagnosed with MEH over a three-year period in the city
and rural areas of Guatemala (36).
They found that 69% of the patients were female (female:male ratio,
2.2:1).
In Table I, the age
range of these patients was 5 to 38 years, the mean age was 11
years, and 97.5% were in their first or second decade of life.
Although five cases were excluded due to lack of information on
their age, it was concluded that this condition predominantly
affects children and adolescents (36).
 | Table IDistribution by decade of life. |
Table I
Distribution by decade of life.
| Age group | Number of cases | % |
|---|
| First decade | 54 | 50.5 |
| Second decade | 50 | 47.0 |
| Third decade | 2 | 2.0 |
| Fourth decade | 1 | 0.5 |
With regard to the localization of lesions (Table II), the majority were in
non-keratinized mobile mucosa, excluding the soft palate, most
frequently on the lower lip and buccal mucosa. Out of the 110 cases
in this study, only three presented with single lesions (2.8%): two
on the lower lip and one on the tongue (36).
 | Table IIDistribution by localization. |
Table II
Distribution by localization.
| Localization | Number of
cases | % |
|---|
| Upper lip | 68 | 63.55 |
| Lower lip | 103 | 96.26 |
| Right buccal
mucosa | 88 | 83.06 |
| Left buccal
mucosa | 92 | 85.98 |
| Tongue | 73 | 68.22 |
Tongue lesions were usually on the lateral borders,
with only three cases of lesions on the ventral tongue and one on
the dorsal tongue (36).
Socio-economic factors have been related to this
disease. In Table III, cases are
divided into five groups according to monthly family income. In
nine of the 110 cases studied, the income group could not be
established; 90% of the patients assessed were members of a family
receiving less than $200 a month. The only patient with a high
monthly income (>$910) was a 21-year-old female from a native
village in Guatemala in which the presence of MEH has been
reported. There were no cases among the 2,464 children in five
private schools (36). These
findings indicated a correlation between low socio-economic level
and MEH.
 | Table IIIDistribution by monthly income. |
Table III
Distribution by monthly income.
| Monthly income | Number of
cases | % |
|---|
| ≤$100 | 83 | 75.0 |
| $101 to 184 | 10 | 15.0 |
| $185 to 364 | 1 | 0.1 |
| $365 to 910 | 0 | 0.0 |
| >$910 | 1 | 0.1 |
In 2004, García-Corona et al studied American
Indians in 2004 and found no significant differences in gender,
observing that 73% of cases were in the first and second decades of
life, with a mean age of 19 years (4). A later study on Indians from Colombia
by Gonzáles et al (3) found
a predilection for the female gender (63.3%) and a mean age of 9.8
years; the most common localization was the lower lip (66.7% of
cases).
Finally, a study in Mexico by Ledesma-Montes et
al (38) reported that 69.3% of
patients were in their first or second decade of life and that the
overall age range was 4 to 69 years; 71.1% were female. The most
frequent localization was the buccal mucosa (82.6%), followed by
the lips and tongue (67.3%).
None of the studies associated MEH with precancerous
lesions, in spite of its close association with HPV, known to be an
etiological factor in various malignant diseases.
6. Conclusions
MEH is a rare disease and its epidemiology has not
been studied to a great extent. With regard to geographic
localization, the majority of published cases are from the
indigenous populations of the American continent and Eskimos from
Greenland. The lips are the most frequent anatomical site of the
disease. There is a higher prevalence in the first and second
decades of life and a predilection for the female gender.
Socio-economic and genetic factors, among others, have also been
associated with the disease.
No correlation with malignant lesions has been
reported, despite the relationship between MEH and HPV, which is an
etiological agent in various precancerous lesions. However, only
low-risk types of HPV have been related to the etiology of MEH, and
few cases have been reported.
There is a need for further studies in various
populations to permit a wider systematic review and a more updated
meta-analysis of this disease.
References
|
1
|
Saunders NR, Scolnik D, Rebbapragada A, et
al: Focal epithelial hyperplasia caused by human papillomavirus 13.
Pediatr Infect Dis J. 29:550–552. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cuberos V, Perez J, Lopez CJ, et al:
Molecular and serological evidence of the epidemiological
association of HPV 13 with focal epithelial hyperplasia: a
case-control study. J Clin Virol. 37:21–26. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gonzalez LV, Gaviria AM, Sanclemente G, et
al: Clinical, histopathological and virological findings in
patients with focal epithelial hyperplasia from Colombia. Int J
Dermatol. 44:274–279. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Garcia-Corona C, Vega-Memije E,
Mosqueda-Taylor A, et al: Association of HLA-DR4
(DRB1*0404) with human papillomavirus infection in
patients with focal epithelial hyperplasia. Arch Dermatol.
140:1227–1231. 2004.PubMed/NCBI
|
|
5
|
Premoli-de-Percoco G, Galindo I and
Ramirez JL: In situ hybridization with digoxigenin-labelled DNA
probes for the detection of human papillomavirus-induced focal
epithelial hyperplasia among Venezuelans. Virchows Arch A Pathol
Anat Histopathol. 420:295–300. 1992. View Article : Google Scholar
|
|
6
|
Hall C, McCullough M, Angel C and Manton
D: Multifocal epithelial hyperplasia: a case report of a family of
Somalian descent living in Australia. Oral Surg Oral Med Oral
Pathol Oral Radiol Endod. 109:20–24. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mosannen-Mozaffari P, Falaki F,
Amirchaghmaghi M, Pakfetrat A, Dalirsani Z and Saghafi-Khadem S:
Multifocal epithelial hyperplasia, a rare oral infection in Asia:
report of twelve cases in Iran. Med Oral Patol Oral Cir Bucal.
15:591–595. 2009.PubMed/NCBI
|
|
8
|
Falaki F, Amir Chaghmaghi M, Pakfetrat A,
Delavarian Z, Mozaffari PM and Pazooki N: Detection of human
papilloma virus DNA in seven cases of focal epithelial hyperplasia
in Iran. J Oral Pathol Med. 38:773–776. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ledesma-Montes C, Vega-Memije E,
Garces-Ortiz M, Cardiel-Nieves M and Juarez-Luna C: Multifocal
epithelial hyperplasia. Report of nine cases. Med Oral Patol Oral
Cir Bucal. 10:394–401. 2005.PubMed/NCBI
|
|
10
|
Van Wyk W and Harris A: Focal epithelial
hyperplasia: a survey of two isolated communities in the Cape
Province of South Africa. Community Dent Oral Epidemiol.
15:161–163. 1987.PubMed/NCBI
|
|
11
|
Pilgard G: Focal epithelial hyperplasia.
Report of nine cases from Sweden and review of the literature. Oral
Surg Oral Med Oral Pathol. 57:540–543. 1984.PubMed/NCBI
|
|
12
|
Fischman SL: Focal epithelial hyperplasia.
Case reports from Paraguay and Peru. Oral Surg Oral Med Oral
Pathol. 28:389–393. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Witkop CJ Jr and Niswander JD: Focal
epithelial hyperplasia in central and south american Indians and
Ladinos. Oral Surg Oral Med Oral Pathol. 20:213–217. 1965.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Archard HO, Heck JW and Stanley HR: Focal
epithelial hyperplasia: an unusual oral mucosal lesion found in
Indian children. Oral Surg Oral Med Oral Pathol. 20:201–212. 1965.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hettwer KJ and Rodgers MS: Focal
epithelial hyperplasia (Heck’s disease) in a Polynesian. Oral Surg
Oral Med Oral Pathol. 22:466–470. 1966.
|
|
16
|
Phillips H and Williams A: Focal
epithelial hyperplasia. Report of a case. Oral Surg Oral Med Oral
Pathol. 26:619–622. 1968. View Article : Google Scholar
|
|
17
|
Waldman GH and Shelton DW: Focal
epithelial hyperplasia (Heck’s disease) in an adult Caucasian. Oral
Surg Oral Med Oral Pathol. 26:124–127. 1968.
|
|
18
|
Decker WG and De Guzman MN: Focal
epithelial hyperplasia. Report of four cases in Mestizos from
Cochabamba, Boliva. Oral Surg Oral Med Oral Pathol. 27:15–19.
1969.PubMed/NCBI
|
|
19
|
Gomez A, Calle C, Arcila G and Pindborg
JJ: Focal epithelial hyperplasia in a half-breed family of
Colombians. J Am Dent Assoc. 79:663–667. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tan KN, Medak H, Cohen L and Burlakow P:
Focal epithelial hyperplasia in a Mexican Indian. Arch Dermatol.
100:474–477. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hollander CF and van Noord MJ: Focal
epithelial hyperplasia: a virus-induced oral mucosal lesion in the
chimpanzee. Oral Surg Oral Med Oral Pathol. 33:220–226. 1972.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tate CL, Conti PA and Nero EP: Focal
epithelial hyperplasia in the oral mucosa of a chimpanzee. J Am Vet
Med Assoc. 163:619–621. 1973.PubMed/NCBI
|
|
23
|
Van Ranst M, Fuse A, Sobis H, et al: A
papillomavirus related to HPV type 13 in oral focal epithelial
hyperplasia in the pygmy chimpanzee. J Oral Pathol Med. 20:325–331.
1991.PubMed/NCBI
|
|
24
|
Sa LR, DiLoreto C, Leite MC, Wakamatsu A,
Santos RT and Catao-Dias JL: Oral focal epithelial hyperplasia in a
howler monkey (Alouatta fusca). Vet Pathol. 37:492–496.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chen SY: Focal epithelial hyperplasia in
rabbit oral mucosa. J Oral Pathol. 8:213–223. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Syrjanen S: Human papillomavirus
infections and oral tumors. Med Microbiol Immunol. 192:123–128.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Praetorius-Clausen F and Willis JM: Papova
virus-like particles in focal epithelial hyperplasia. Scand J Dent
Res. 79:362–365. 1971.PubMed/NCBI
|
|
28
|
Hanks CT, Fischman SL and Nino de Guzman
M: Focal epithelial hyperplasia. A light and electron microscopic
study of one case. Oral Surg Oral Med Oral Pathol. 33:934–943.
1972.PubMed/NCBI
|
|
29
|
Kuffer R and Perol Y: Focal epithelial
hyperplasia. 1st French case. Demonstration of a papovavirus by
electron microscopy. Rev Stomatol Chir Maxillofac. 77:318–321.
1976.PubMed/NCBI
|
|
30
|
Kuhlwein A, Nasemann T, Janner M, Schaeg G
and Reinel D: Detection of papilloma virus in Heck’s focal
epithelial hyperplasia and the differential diagnosis of
white-sponge nevus. Hautarzt. 32:617–621. 1981.
|
|
31
|
Pfister H, Hettich I, Runne U, Gissmann L
and Chilf GN: Characterization of human papillomavirus type 13 from
focal epithelial hyperplasia Heck lesions. J Virol. 47:363–366.
1983.PubMed/NCBI
|
|
32
|
Beaudenon S, Praetorius F, Kremsdorf D, et
al: A new type of human papillomavirus associated with oral focal
epithelial hyperplasia. J Invest Dermatol. 88:130–135. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Syrjanen SM, Syrjanen KJ, Happonen RP and
Lamberg MA: In situ DNA hybridization analysis of human
papillomavirus (HPV) sequences in benign oral mucosal lesions. Arch
Dermatol Res. 279:543–549. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Petzoldt D and Pfister H: HPV 1 DNA in
lesions of focal epithelial hyperplasia Heck. Arch Dermatol Res.
268:313–314. 1980. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
De Villiers EM, Neumann C, Le JY, Weidauer
H and zur Hausen H: Infection of the oral mucosa with defined types
of human papillomaviruses. Med Microbiol Immunol. 174:287–294.
1986.PubMed/NCBI
|
|
36
|
Carlos R and Sedano HO: Multifocal
papilloma virus epithelial hyperplasia. Oral Surg Oral Med Oral
Pathol. 77:631–635. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Premoli-De-Percoco G, Cisternas JP,
Ramirez JL and Galindo I: Focal epithelial hyperplasia
human-papillomavirus-induced disease with a genetic predisposition
in a Venezuelan family. Hum Genet. 91:386–388. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ledesma-Montes C, Garces-Ortiz M and
Hernandez-Guerrero JC: Clinicopathological and immunocytochemical
study of multifocal epithelial hyperplasia. J Oral Maxillofac Surg.
65:2211–2217. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Feller L, Khammissa RA, Wood NH, Malema V,
Meyerov R and Lemmer J: Focal epithelial hyperplasia (Heck disease)
related to highly active antiretroviral therapy in an
HIV-seropositive child. A report of a case, and a review of the
literature. SADJ. 65:172–175. 2010.PubMed/NCBI
|
|
40
|
Marvan E and Firth N: Focal epithelial
hyperplasia in an HIV positive man. An illustrated case and review
of the literature. Aust Dent J. 43:305–310. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Bombeccari GP, Guzzi GP, Pallotti F and
Spadari F: Focal epithelial hyperplasia: polymerase chain reaction
amplification as a differential diagnosis tool. Am J Dermatopathol.
31:98–100. 2009. View Article : Google Scholar
|
|
42
|
Segura-Saint-Gerons R, Toro-Rojas M,
Ceballos-Salobrena A, Aparicio-Soria JL and Fuentes-Vaamonde H:
Focal epithelial hyperplasia. A rare disease in our area. Med Oral
Patol Oral Cir Bucal. 10:128–131. 2005.PubMed/NCBI
|
|
43
|
Hashemipour MA, Shoryabi A, Adhami S and
Mehrabizadeh Honarmand H: Extensive focal epithelial hyperplasia.
Arch Iran Med Jan. 13:48–52. 2009.
|
|
44
|
Martins WD, de Lima AA and Vieira S: Focal
epithelial hyperplasia (Heck’s disease): report of a case in a girl
of Brazilian Indian descent. Int J Paediatr Dent. 16:65–68.
2006.
|
|
45
|
Dos Santos-Pinto L, Giro EM, Pansani CA,
Ferrari J, Massucato EM and Spolidorio LC: An uncommon focal
epithelial hyperplasia manifestation. J Dent Child (Chic).
76:233–236. 2009.PubMed/NCBI
|
|
46
|
Steinhoff M, Metze D, Stockfleth E and
Luger TA: Successful topical treatment of focal epithelial
hyperplasia (Heck’s disease) with interferon-beta. Br J Dermatol.
144:1067–1069. 2001.PubMed/NCBI
|
|
47
|
Akyol A, Anadolu R, Anadolu Y, Ekmekci P,
Gurgey E and Akay N: Multifocal papillomavirus epithelial
hyperplasia: successful treatment with CO2 laser therapy
combined with interferon alpha-2b. Int J Dermatol. 42:733–735.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Luomanen M: Oral focal epithelial
hyperplasia removed with CO2 laser. Int J Oral
Maxillofac Surg. 19:205–207. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Clausen FP, Mogeltoft M, Roed-Petersen B
and Pindborg JJ: Focal epithelial hyperplasia of the oral mucosa in
a south-west Greenlandic population. Scand J Dent Res. 78:287–294.
1970.PubMed/NCBI
|
|
50
|
Henke RP, Milde-Langosch K, Loning T and
Koppang HS: Human papillomavirus type 13 and focal epithelial
hyperplasia of the oral mucosa: DNA hybridization on
paraffin-embedded specimens. Virchows Arch A Pathol Anat
Histopathol. 411:193–198. 1987. View Article : Google Scholar : PubMed/NCBI
|