Introduction
Epithelial ovarian cancer (EOC) has the highest
mortality of all gynecological cancers and is the fifth leading
cause of mortality due to cancer among women. Despite relatively
low incidence (approximately 1/100 000 new cases per year), EOC
presents a high case-to-fatality ratio. That progression of the
disease is relatively symptomless makes a significant contribution
to the high mortality rates. The 5-year survival rate for EOC is
approximately 45%, largely due to the high proportion of cancer
cases that are not detected until they have spread beyond the ovary
to the pelvis and upper abdomen. Early stages of the disease remain
without symptoms, with the first signs typically occurring at an
advanced stage. Thus, ovarian cancer is commonly known as a ‘silent
killer’. Clinical outcome and survival may be significantly
improved by identifying the disease in its early stages without the
need for altering surgical or chemotherapeutic approaches. Although
certain ovarian cancer screening tests have been shown to decrease
mortality rates, the possibility of efficient screening that may be
used in everyday practice remains elusive. Measurement of serum
CA125 antigen remains the gold standard (1–18).
The best-studied serum marker for ovarian cancer,
CA125, is elevated in less then half of early stage EOC cases and
is not expressed in approximately 20% of ovarian cancers resulting
in a decrease of sensitivity. The lack of specificity of CA125 is
secondary to its levels being elevated in a number of benign
gynecological and non-gynecological conditions. As such, in recent
years over 45 new or already known substances have been verified as
ovarian cancer biomarkers, such as human epididymis protein 4 (HE4)
and soluble mesothelin-related protein (SMRP). Novel biomarkers
alone or combined with CA125 potentially increase the sensitivity
and specificity of CA125. Mesothelin and HE4 protein are the most
intensively studied of the novel biomarkers (19–28).
Mesothelin is a differentiation antigen highly
expressed in mesotheliomas, pancreatic, ovarian and other types of
cancer. Its expression in normal human tissues is limited to
mesothelial cells lining the pleura, pericardium and peritoneum.
Since the widely accepted model of ovarian carcinogenesis is the
tumor origin from the ovarian surface epithelium (OSE) followed by
spread to the pelvic and abdominal cavities afterwards, it appears
that proteins, such as mesothelin may be useful in the early
detection of ovarian cancer. Mesothelin and its soluble isoforms
(SMRP) are synthesized by mesothelial cells but only in a state of
serious pathology such as carcinogenesis. Ovarian cancer is one of
the tumors triggering SMRP synthesis, thus a diagnostic test based
on serum SMRP concentrations may be helpful in the diagnostic
process (4,24,26,29–37).
HE4 protein was first identified in the epithelium
of the distal epididymis and was predicted to be involved in sperm
maturation as a protease inhibitor. This protein has a WAP-type
four-disulphide core (WFDC) domain and is encoded by the
WFDC2 gene. In malignant ovarian neoplasms upregulation of
that gene was observed. In patients with ovarian tumors,
sensitivity of the HE4 protein is similar to CA125 but specificity
for malignancy was increased as compared to benign disease
(4,24,26,38–44).
HE4 is not elevated in common benign gynecological
and other medical conditions, whereas CA125 is elevated. SMRP and
HE4 complement CA125 in ovarian cancer detection and are therefore
of particular interest for the detection of early stage EOC
(26,43,44).
The aim of the present study was to evaluate the
usefulness of the potential biomarkers SMRP and HE4 for ovarian
cancer diagnosis. Additionally, the associations between SMRP, HE4
and CA125 were analyzed to evaluate the role of the two biomarkers
in the early stages of the disease as well as possibilities of
supporting the diagnostics of advanced stages of ovarian cancer. A
further aim of the study was to investigate how the serum
concentration of HE4, SMRP and CA125 varied with age, histological
type and stage of ovarian cancer in women with ovarian cancer and
healthy controls.
Materials and methods
Patient characteristics
Study participants were recruited between 2005 and
2007. The study group consisted of 70 patients with diagnosed
ovarian cancer. The control group consisted of 78 healthy women
without any pathological features of the ovaries. Prior to
collection of biological samples all patients were required to
provide full informed consent. Cases were defined as having
epithelial carcinoma confirmed by a standardized review of the
medical records and pathologist examination of paraffin-embedded
tissue for tumor histology. Patients with an EOC underwent surgical
staging required by protocol or tumor debulking as clinically
indicated. Of the 70 patients with EOC, 52 cases had serous ovarian
carcinoma, 7 cases had mucinous histological type, 5 had
endometrioid EOC and 6 patients had other histological types of
disease. Patient demographics and characteristics are shown in
Table I. The study was approved by
the local ethics committee of the Central Clinical Hospital of
Ministry of Interior and Administration.
 | Table IDemographics and clinical
characteristics of study population. |
Table I
Demographics and clinical
characteristics of study population.
| Characteristics | Study group
(n=70) | Control group
(n=78) |
|---|
| Age (years) |
| Mean (SD) | 57.36 (9.73) | 55.06 (11.21) |
| Range | 20–80 | 32–74 |
| Menopausal
status |
| Premenopausal | 15 (21.4%) | 27 (34.6%) |
| Postmenopausal | 55 (78.6%) | 51 (65.4%) |
| Ovarian cancer stage
(FIGO) |
| I | 15 (21.4%) | NA |
| II | 3 (4.3%) | NA |
| III | 45 (64.3%) | NA |
| IV | 7 (10%) | NA |
| Histology |
| Serous | 52 (74.3%) | NA |
| Endometrioid | 5 (7.1%) | NA |
| Mucinous | 7 (10%) | NA |
| Other subtype | 6 (8.6%) | NA |
Methods
Blood (20 ml) was collected, clotted for 60 min and
centrifuged. The serum fraction was removed and stored at −70°C
until use. Serum levels of CA125, HE4 and SMRP were measured using
bead-based immunoassay kits from commercial suppliers according to
manufacturers’ instructions.
Statistical analysis
SPSS statistical software (version 11.5; SPSS Inc.,
Chicago, IL, USA) was used for statistical analyses. The
statistical tests were two-sided and considered to be statistically
significant at p<0.05.
Results
Mean values for the plasma levels of all biomarkers
differed significantly between patients with cancer compared to the
control group. The median serum level of CA125 for ovarian cancer
cases was 503.55±560.7 U/ml vs. 9.28±14.47 U/ml in the control
group (p<0.001). For SMRP, the median serum concentration in the
study group was 5.13±7.64 nM vs. 1.02±0.89 nM in the control group
(p<0.01); and for HE4 these results were 597.95±934.59 pM in the
ovarian cancer group vs. 56.75±43.79 pM in the control group
(p<0.001).
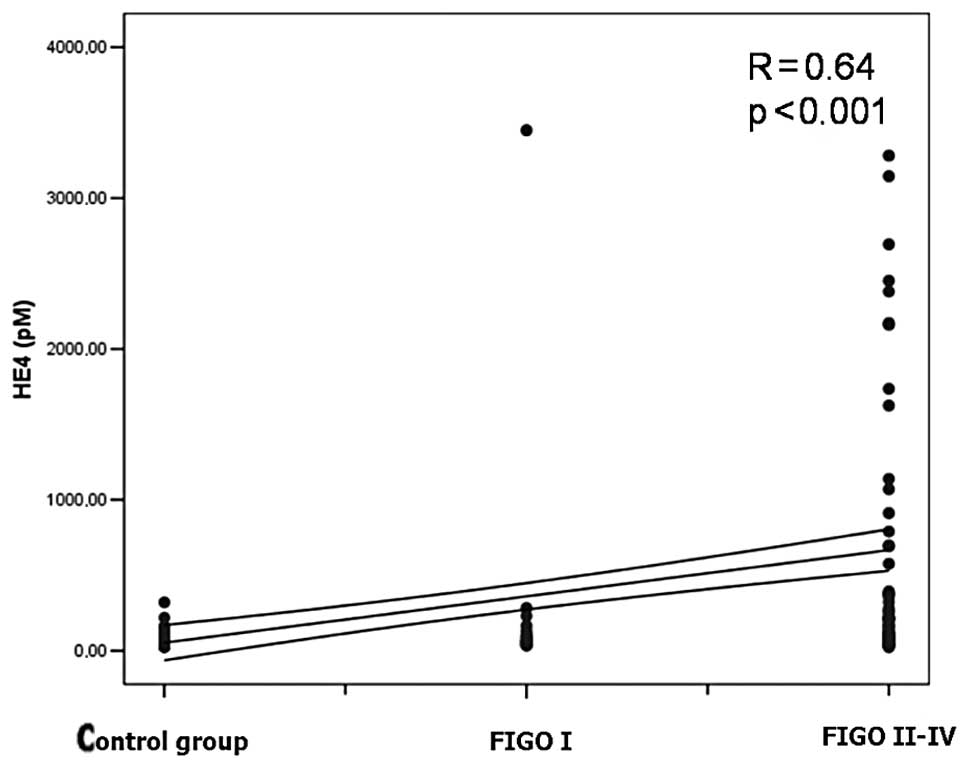
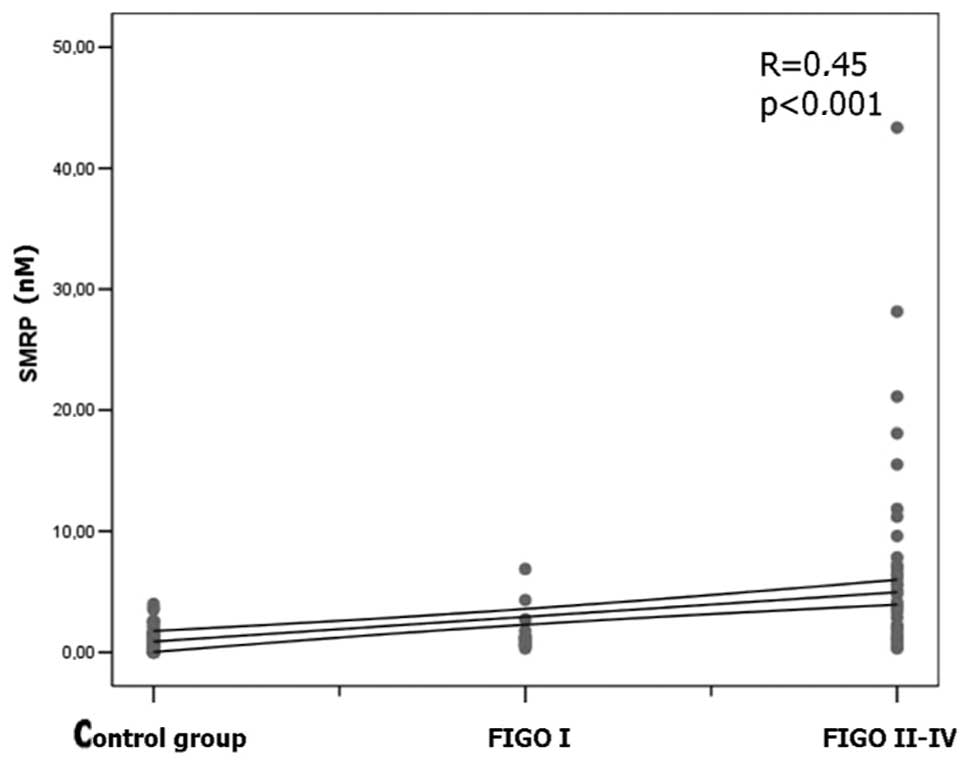
Data analysis also revealed significantly higher
concentrations of CA125, HE4 and SMRP in the late stage ovarian
cancer group (FIGO II–IV) in comparison with the early stage
patients (FIGO I stage) and control group. A positive correlation
between the clinical stage of ovarian cancer and CA125 blood serum
concentration was found (R=0.83; p<0.001). A positive
correlation was found between the HE4 protein serum concentration
and EOC stage (R=0.64; p<0.001) (Fig. 1) and between the SMRP plasma
concentration and stage of ovarian cancer patients (R=0.45;
p<0.001) (Fig. 2).
Data analysis from the study participants also
demonstrated a significant correlation between plasma concentration
of CA125 and HE4 (R=0.45; p<0.001), between CA125 and SMRP
(R=0.38; p<0.001) as well as HE4 and SMRP (R=0.51; p<0.001).
Moreover, in the group of patients with ovarian cancer, similar
significant correlations between serum biomarker concentrations
were observed [CA125 and HE4 (R=0.31; p<0.01); CA125 and SMRP
(R=0.25; p<0.05); HE4 and SMRP (R=0.44, p<0.001)].
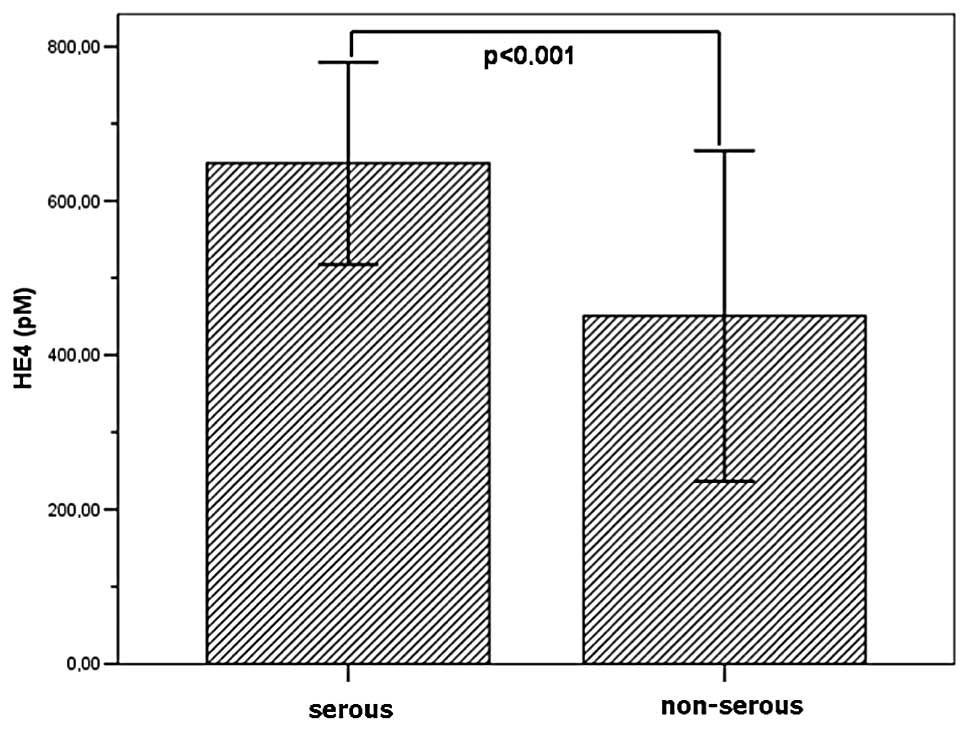
Significant correlations were observed between the
serous histological type of EOC and serum concentration of HE4
observed in the study group in comparison with other non-serous
types of ovarian cancer (p<0.01) (Fig. 3).
To compare the results, SMRP plasma concentrations
in the study group in serous and non-serous histological type of
EOC were also analyzed, but the results turned out not to be
statistically significant (p=0.29). Additionally, data analysis of
the study group participants also revealed a positive correlation
between the age of the patients and HE4 plasma concentration
(R=0.32; p<0.01), whereas the results for CA125 and SMRP were
not statistically significant (p=NS).
Discussion
The novel ovarian cancer biomarkers HE4 protein and
mesothelin have utility for the early detection of ovarian cancer,
but the gold standard for ovarian cancer screening for evaluating
CA125 measurements with a value above 35 U/ml is considered to be
abnormal. The above-mentioned marker is characterized by a
specificity of approximately 80% and a low false positive rate of
less than 1%. Serum CA125 is increased in approximately 50% of
women with the stage I ovarian cancer according to FIGO, which
appears unsatisfactory. However, 80% of women with ovarian cancer
staged from II to IV according to FIGO increased the values of
CA125. Nonetheless, screening based only on CA125 measurements,
results in approximately 20% of cases of ovarian cancer not being
detected (36,37).
Furthermore, in a study by Pauler et al, the
authors reported that CA125 levels in healthy women vary based on
characteristic such as age, race, smoking status, caffeine intake,
age at menarche and menopause status (26,45).
SMRP and HE4 are two of the most promising novel
ovarian cancer biomarkers and are candidates for early detection
markers to replay or complement CA125 (4).
In a study by McIntosh et al, specificity of
CA125 alone was found to be 79%, increasing to 87% when CA125 is
used with the composite marker mesothelin (sensitivity at 98%).
However, the authors concluded that, as a single marker, CA125 is a
better alternative to SMRP (36).
The present study found a significant correlation
between the clinical stage of the ovarian cancer and CA125, HE4 and
SMRP blood serum concentration in the late stage ovarian cancer
group (FIGO II–IV) in comparison with early stage patients (FIGO I
stage) and a control group. This is in accordance with data
presented in the literature (28,43,44,46,47).
The results suggest that HE4 and SMRP improved
performance in early stage disease, but since the majority of the
cases (in our study 74.3%) were diagnosed in late stages of the
disease (III or IV FIGO), larger study cohorts are required to
confirm this hypothesis. Study results have shown a significant
correlation between the serous histological type of EOC and serum
concentration of HE4 in the study group in comparison with other
non-serous types of ovarian cancer (p<0.01). However, for SMRP
and CA125, the results turned out not to be statistically
significant (p=0.29; p=0.09). Findings of a study by Palmer et
al showed results for the HE4 protein to be statistically
significant. Those authors concluded that sensitivity and
specificity of single marker HE4 is similar to the combination of
CA125 and HE4 and higher than that of CA125 alone (28).
In a study by Shah et al, mesothelin and HE4
plasma levels were found to be higher for mucinous ovarian cancer
cases. However, those results may have been spurious due to the
small total number of mucinous cancer cases in the cohort (n=6)
(26). In our study, no such
correlation for the mucinous histological type of cancer was found,
but there were only seven cases of this type in our cohort.
Moreover, in the study by Palmer et al extremely low results
were obtained for mucinous type sensitivity and specificity for the
combination of CA125 and HE4 (17 and 98%, respectively) (26,28).
We also observed a correlation between the plasma
concentration of HE4 and age in the cancer subgroup. Similar
results were published in 2008 by Lowe et al whereby levels
of HE4 serum increased with age in a similar manner between women
with ovarian cancer and healthy controls. For SMRP and CA125, the
results were found not to be statistically significant (4).
However, most recent studies undermine the role of
CA125 as a single biomarker in early detection of ovarian cancer.
Investigators have attempted to increase the sensitivity of the
test without decreasing its specificity. It appears that the
combination of CA125 with other blood serum biomarkers such as SMRP
or HE4 may be useful (31,32,48,49).
The main conclusion derived from the present study
and supported by previous studies is that HE4 protein, especially
in combination with CA125 and SMRP, may be used as a marker of
early stage ovarian cancer. Serum SMRP and HE4 may be useful
biomarkers for ovarian cancer screening and detection. Although it
cannot be used alone in early stages of the disease, SMRP and HE4
assessment is a useful screening tool in advanced stages of ovarian
cancer. Serum CA125 antigen is currently the most efficient ovarian
cancer biomarker, especially in early stages of the disease. Data
from the present study suggest that HE4 and SMRP is a potentially
useful in multiple marker screening for the serous type of ovarian
carcinoma. Analysis of the biomarkers also demonstrated
age-dependent differences in the serum concentrations of HE4, as
previously reported (4,44). Further studies are required to
assess this property of HE4 and SMRP alone and confirm their
performance at high specificity before we are able to make
statements concerning the superiority or inferiority of these new
biomarkers over CA125 alone for early detection.
Ongoing efforts using targeted discovery,
combination of markers, and stratification of screening populations
by cancer risk may yet lead to an effective early detection test
for ovarian cancer. However, ovarian cancer is a heterogeneous
disease and it may be difficult for a single marker, even with
serial testing, to achieve a level of robust performance that would
allow cost-effective screening of a general population. It is
conceivable that by incorporating existing or newly discovered
tumor markers one could significantly improve the sensitivity and
specificity of detection of true early signs of ovarian cancer.
Acknowledgements
This study was supported by the Institute of Mother
and Child in Warsaw, Poland by grant number 510-31-82.
References
|
1
|
Jemal A, Murray T, Ward E, et al: Cancer
statistics. CA Cancer J Clin. 55:10–30. 2005.
|
|
2
|
Tortorelo-Luna G and Mitchell M: The
epidemiology of ovarian cancer. J Cell Bioch. 23:200–207. 1995.
View Article : Google Scholar
|
|
3
|
Gupta D and Lis C: Role of CA125 in
predicting ovarian cancer survival - a review of the
epidemiological literature. J Ovarian Res. 2:132003. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lowe K, Shah C, Wallace E, et al: Effects
of personal characteristics on serum CA125, mesothelin and HE4
levels in healthy postmenopausal women at high-risk for ovarian
cancer. Cancer Epidemiol Biomarkers Prev. 17:2480–2487. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Chu C and Rubin S: Screening for ovarian
cancer in the general population. Best Pract Res Clin Obstet
Gynaecol. 20:307–320. 2002. View Article : Google Scholar
|
|
6
|
Canevari S, Gariboldi M, Reid J, et al:
Molecular predictors of response and outcome in ovarian cancer.
Crit Rev Oncol Hematol. 60:19–37. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gilks C, Ionescu D, Kalloger S, et al:
Tumor cell type can be reproducibly diagnosed and is of independent
prognostic significance in patients with maximally debulked ovarian
carcinoma. Hum Pathol. 39(8): 1239–1251. 2008. View Article : Google Scholar
|
|
8
|
Pettersson F: Annual report on the results
of treatment in gynecological cancer. Stockholm: International
Federation of Gynecology and Obstetrics; 1994
|
|
9
|
Lu K, Patterson A, Wang L, et al:
Selection of potential markers of epithelial ovarian cancer with
gene expression arrays and recursive descent partition analysis.
Clin Cancer Res. 10:3291–3300. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hoskins W: Prospective on ovarian cancer:
why prevent? Cell Biochem Suppl. 23:189–199. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Pettersson F, Kolstad P, Ludwig H, et al:
Annual report on the results of treatment in gynecological cancer.
International Federation of Gynecology and Obstetrics. 1998.
|
|
12
|
Nguyen H, Averette H, Hoskins W, et al:
National survey of ovarian carcinoma VI. Critical assessment of
current International Federation of Gynecology and Obstetrics
staging system. Cancer. 72:3007–3011. 1993. View Article : Google Scholar
|
|
13
|
Bast RC Jr, Brewer M, Zou C, et al:
Ovarian cancer prevention and early detection: mission impossible?
Recent Results Cancer Res. 174:91–900. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang Z, Yu Y, Xu F, et al: Combining
multiple serum tumor markers improves detection of stage I
epithelial ovarian cancer. Gynecol Oncol. 107:526–531. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Havrilesky L, Whitehead C, Rubatt J, et
al: Evaluation of biomarker panels for early stage ovarian cancer
detection and monitoring for disease recurrence. Gynecol Oncol.
110:374–382. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Scholler N, Crawford M, Sato A, et al:
Bead-based ELISA assays for validation of ovarian cancer early
detection markers. Clin Cancer Res. 1:2117–2124. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Nosov V, Feng S, Malaika A, et al:
Validation of serum biomarkers for detection of early-stage ovarian
cancer. Am J Obstet Gynecol. 200:639 e1–5. 2009.PubMed/NCBI
|
|
18
|
Oikonomopolou K, Li L, Zheng Y, et al:
Prediction of ovarian cancer prognosis and response to chemotherapy
by a serum-based multiparametric biomarker panel. Br J Cancer.
99:1103–1113. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Pauler D, Menon U, McIntosh M, et al:
Factors influencing serum Ca125II levels in healthy postmenopausal
women. Cancer Epidemiol Biomarkers Prev. 10:489–493.
2001.PubMed/NCBI
|
|
20
|
Bast R and Knapp R: Use of CA125 antigen
in diagnosis and monitoring of ovarian carcinoma. Eur Obset Gyncol
Reprod Biol. 19:354–356. 1995. View Article : Google Scholar
|
|
21
|
Fishman D: The present and future of
biomarkers for the early detection of epithelial ovarian carcinoma.
CME J Gynecol Oncol. 4:33–36. 1999.
|
|
22
|
Jacobs I and Bast R: The Ca125
tumor-associated antigen: a review of literature. Human Reprod.
4:1–12. 1989.
|
|
23
|
Wollas R, Xu F, Jacobs I, et al: Elevation
of multiple serum markers in patients with stage I ovarian cancer.
JNCI. 85:1748–1751. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bast R: Status of tumor markers in ovarian
cancer screening. J Clin Oncol. 21:200–205. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Skates S, Xu F, Yu H, et al: Toward an
optimal algorithm for ovarian cancer screening with longitudinal
tumor markers. Cancer. 76:2004–2010. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Shah C, Lowe K, Paley P, et al: Influence
of ovarian cancer risk status on the diagnostic performance of the
serum biomarkers mesothelin, HE4 and CA125. Cancer Epidemiol
Biomarkers Prev. 18:1365–1372. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jacobs I and Menon U: Progress and
challenges in screening for early detection of ovarian cancer. Mol
Cell Proteomics. 3:355–366. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Palmer C, Duan X, Hawley S, et al:
Systematic evaluation of candidate blood markers for detecting
ovarian cancer. PLoS One. 3:e26332008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Chang K and Pastan I: Molecular cloning of
mesothelin, a differentiation antigen present on mesothelium,
mesotheliomas, and ovarian cancers. Proc Natl Acad Sci USA.
93:136–140. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chang K, Pai LH, Batra JK, et al:
Characterization of the antigen (CAK1) recognized by monoclonal
antibody K1 present on ovarian cancers and normal mesothelium.
Cancer Res. 52:181–186. 1992.PubMed/NCBI
|
|
31
|
Blaustein A: Peritoneal mesothelium and
ovarian surface cells-shared characteristics. Int J Gynecol Pathol.
3:361–375. 1984.PubMed/NCBI
|
|
32
|
Okamura H, Katabuchi H, Nitta M, et al:
Structural changes and cell properties of human ovarian surface
epithelium in ovarian pathophysiology. Microsc Res Tech.
69:469–481. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Dubeau L: The cell of origin of ovarian
epithelial tumours. Lancet Oncol. 9:1191–1197. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Okamura H: Detailed morphology of human
ovarian surface epithelium focusing on its metaplastic and
neoplastic capability. Ital J Anat Embryol. 106(Suppl 2): 263–276.
2001.PubMed/NCBI
|
|
35
|
Kurman RJ and Shih IM: Pathogenesis of
ovarian cancer: lessons from morphology and molecular biology and
their clinical implications. Int J Gynecol Pathol. 27:151–160.
2008.PubMed/NCBI
|
|
36
|
McIntosh M, Drescher C, Karlan B, et al:
Combining CA125 and SMRP serum markers for diagnosis and early
detection of ovarian carcinoma. Gynecol Oncol. 95:9–15. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Scholler N, Garvik B, Hayden-Ledbetter M,
Kline T and Urban N: Development of a CA125-mesothelin cell
adhesion assay as a screening tool for biologics discovery. Cancer
Lett. 247:130–136. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Drapkin R, Von Horsten H, Lin Y, et al:
Human epididymis protein 4 (HE4) is a secreted glycoprotein that is
overexpressed by serous and endometrioid ovarian carcinomas. Cancer
Res. 65:2162–2169. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Galgano M, Hampton G and Frierson H:
Comprehensive analysis of HE4 expression in normal and malignant
human tissues. Mod Pathol. 19:847–853. 2006.PubMed/NCBI
|
|
40
|
Hellström I, Raycraft J, Hayden-Ledbetter
M, et al: The HE4 (WFDC2) protein is a biomarker for ovarian
carcinoma. Cancer Res. 63:3695–3700. 2003.PubMed/NCBI
|
|
41
|
Moore R, Brown A, Miller C, et al: Utility
of a novel serum tumor biomarker HE4 in patients with uterine
cancer. J Clin Oncol. 24:18S2006.
|
|
42
|
Berry N, Cho Y, Harrington M, et al:
Transcriptional targeting in ovarian cancer cells using the human
epididymis protein 4 promoter. Gynecol Oncol. 92:896–904. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Moore R, Brown A, Miller M, et al: The use
of multiple novel tumor biomarkers for the detection of ovarian
carcinoma in patients with a pelvic mass. Gynecol Oncol.
108:402–408. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Moore R, McMeekin D, Brown A, et al: A
novel multiple marker bioassay utilizing HE4 and CA125 for the
prediction of ovarian cancer in patients with a pelvic mass.
Gynecol Oncol. 112:40–46. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Pauler D, Menon U, McIntosh M, et al:
Factors influencing serum CA125II levels in healthy postmenopausal
woman at high-risk for ovarian cancer. Cancer Epidemiol Biomarkers
Prev. 17:2480–2487. 2008. View Article : Google Scholar
|
|
46
|
Hellström I, Raycraft J, Kanan S, et al:
Mesothelin variant I is released from tumor cells as a diagnostic
marker. Cancer Epidemiol Biomarker Prev. 15:1014–1020.
2006.PubMed/NCBI
|
|
47
|
Das P and Bast R Jr: Early detection of
ovarian cancer. Biomark Med. 2:291–303. 2008. View Article : Google Scholar
|
|
48
|
Köbel M, Kalloger S, Boyd N, et al:
Ovarian carcinoma subtypes are different diseases: implication for
biomarker studies. PLoS Med. 5:e2322008.PubMed/NCBI
|
|
49
|
Kozak K, Su F, Whitelegge J, et al:
Characterization of serum biomarkers for detection of early stage
ovarian cancer. Proteomics. 5:4589–4596. 2005. View Article : Google Scholar : PubMed/NCBI
|