Introduction
Solitary fibrous tumor (SFTs) are rare spindle cell
tumors arising from the visceral pleura (1) that are rarely located in the central
nervous system and even more rarely in the sella turcica. To the
best of our knowledge, only 5 cases have been reported in the
literature (2–6). SFTs are often undiagnosed due to the
use of varied imaging techniques pre-operatively and as they are
commonly mistaken for meningiomas or pituitary tumors. Total
resection is difficult and complications often develop
post-surgery.
The current study presents a rare case of an SFT in
the saddle diaphragm, the first in this location. The case report
aims to provide information on the clinical experience, imaging and
pathological features with regards to SFT, to aid in the correct
diagnosis and total resection of tumors in the sella turcica. The
case of a patient who presented with a vision impairment in the
right eye is discussed. Computed tomography of the head revealed a
round, hyperdense mass in the sellar and suprasellar regions.
Pituitary gland magnetic resonance imaging (MRI) revealed
isointensity on T1 and T2 weighted imaging. Tumor enhanced scanning
showed heterogeneous contrast enhancement. The initial diagnosis
was that of meningioma or pituitary tumor. A total tumor resection
was performed using a right pterional approach under general
anesthesia. During surgery, the base of the tumor was located on
the sellar diaphragm of the left anterior pituitary stalk. The
pathological diagnosis was of a SFT. The patient had no
post-operative diabetes insipidus or idiopathic pituitary
hypofunction. Written informed consent was obtained from the
patient for publication of this case report and any accompanying
images
Case report
A 25-year-old male patient with a 5-month history of
aggravated vision through blurring in the right eye was admitted to
the General Hospital of Jinan Military Area Command of Chinese PLA,
Shandong, China, on October 10th, 2011. An examination revealed
sight impairment (vision, right eye, 0.1; left eye, 1.2), a typical
temporal hemianopsia of the right eye and locally decreased vision
sensitivity of the superior nasal aspect of the left eye, without
other positive neurological signs. The serum concentrations of PRL,
GH, T3, T4 and TSH were all within normal limits. The patient
underwent head computed tomography, which revealed a round,
hyperdense mass without clear edges in the sellar and suprasellar
regions that was closely associated with the bilateral vessels.
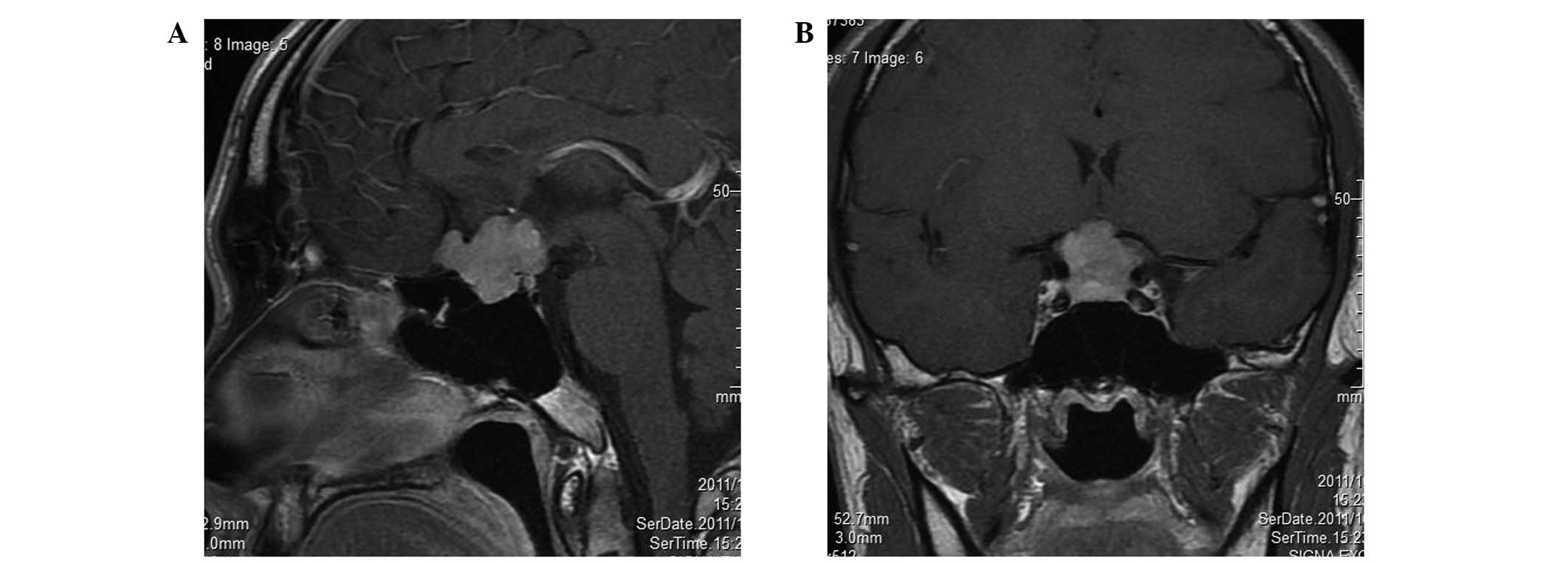
Magnetic resonance imaging (MRI) revealed a lobulated, isointense
mass wrapped around the anterior communicating artery complex in
the sellar-suprasellar region on T1-weighted imaging (T1WI) in the
sagittal view. The tumor was isointense and slightly hyperintense
in the sellar-suprasellar region in the coronal view. There was no
clear border separating the tumor from the peripheral brain
tissues. The tumor was also isointense on T2-weighted imaging
(T2WI). Tumor-enhanced scanning demonstrated heterogeneous contrast
enhancement (Fig. 1). The
preliminary diagnosis was of meningioma or pituitary tumor. A tumor
resection was conducted using a right pterional approach under
general anesthesia on October 15, 2011. Intraoperatively, the base
of the tumor was located on the sellar diaphragm of the left
anterior pituitary stalk. The tumor pushed the pituitary stalk to
the right posterior region, ascended to the suprasellar region,
crossed the optic chiasm, invaded the lamina terminalis cistern and
wrapped the bilateral A1 segment and anterior communicating artery
complex. In the opposite direction, the tumor crossed the
saddle-back and reached the slope, showing no clear demarcation
from the hypothalamus. Severe adhesion to each side of the optic
nerve caused difficulty in the separation of the tissues. The tumor
tissue was tough and had an abundant blood supply. A feeding artery
was present from a branch of the internal carotid artery in the
base of the tumor. A total disparting resection of the tumor was
performed with emphasis on left optic neuroprotection under a
high-power lens. Following tumor resection, the undamaged pituitary
and pituitary stalk were identified; these had been pushed towards
the right posterior hypophyseal fossa by the tumor. The patient had
no post-operative diabetes insipidus or idiopathic pituitary
hypofunction, but had a right eye vision of 0.2, uncorrected and
1.0, corrected. The pathological diagnosis was of a solitary
fibrous tumor (SFT).
Discussion
SFTs are rare spindle cell tumors that arise from
the visceral pleura, according to the earliest studies (1). SFTs are rarely located in the central
nervous system and even more rarely occur in the sella turcica; to
the best of our knowledge, only 5 cases have been reported in the
literature. In 2003, Cassarino et al(2) first reported an SFT that widely
affected the sellar region. A 54-year-old female patient developed
an SFT involving the ephippium, sphenoid sinus, internal carotid,
interior temporal lobe, ethmoid sinus and pterygoid bone and that
extended to the nasopharynx. The tumor was partly removed and the
pituitary was found to be undamaged. Kim et al(3) described 8 patients with SFTs in the
head and neck. Among them, a 56-year-old male patient presenting
mainly with visual disturbances was diagnosed as having a pituitary
tumor with hemorrhage. The patient underwent partial tumor
resection via the transsphenoidal route. A SFT was established by
pathology, and a secondary craniotomy was consequently performed.
Furlanetto et al(4) reported
the case of a 28-year-old patient who underwent pituitary adenoma
excision via the transsphenoidal approach. The tumor was hard and
involved the sellar diaphragm. Complications, including
cerebrospinal fluid leakage, idiopathic pituitary hypofunction and
meningitis, occurred post-operatively. Yin et al(5) reported a 32-year-old male patient with
a headache and eye discomfort, who underwent partial pituitary
tumor resection and post-operative γ-knife treatment. Cui et
al(6) described the case of a
29-year-old patient who was pre-operatively diagnosed with a right
tuberculum sella meningioma. The pathological diagnosis revealed
that the tumor was a malignant SFT. This lesion was pre-operatively
diagnosed as a pituitary tumor and meningioma. Prior to surgery, it
is almost impossible to achieve a correct diagnosis of SFT in the
saddle area. The diagnosis of SFT of the saddle diaphragm in the
present case was only achieved by ultimate dependence on the
pathological diagnosis, tumor basal position, left anterior
displacement of the left optic nerve and the right posterior shift
of the pituitary stalk observed in surgery. There have been no
previous reports of SFTs of the saddle diaphragm.
However, these tumors have been identified in
various locations outside the thoracic cavity, mostly in the
extracranial head and neck, including the meninges (7–11),
orbit (12), nasal cavity (13), paranasal sinuses (14), soft palate, salivary glands
(15) and parapharyngeal space
(16). Patients aged 30–64 years
are the most commonly affected and there is no gender predilection.
The ages of the six patients in the study by Kim et
al(14) ranged from 46–59
years, with a male to female ratio of 4:2. The 25-year-old male
patient in the present study was the youngest among only six known
cases of SFT in the saddle area. Visual impairment is a common
initial clinical manifestation of SFT caused by the tumor
compressing the surrounding tissues, as occurred in the present
case. Headaches and hypoglycemia are also common manifestations.
However, an endocrine examination disclosed normal pituitary and
target gland hormone secretions. In the present case, the SFT had a
slightly high and heterogeneous density. The present study agrees
with the theory by Kim et al(14) that suggests that the density of the
tumor correlates with its cellular components. In the present
study, the tumor was isointense on the T1- and T2-weighted images.
The contrast enhancement was heterogeneous and lower than for
meningioma.
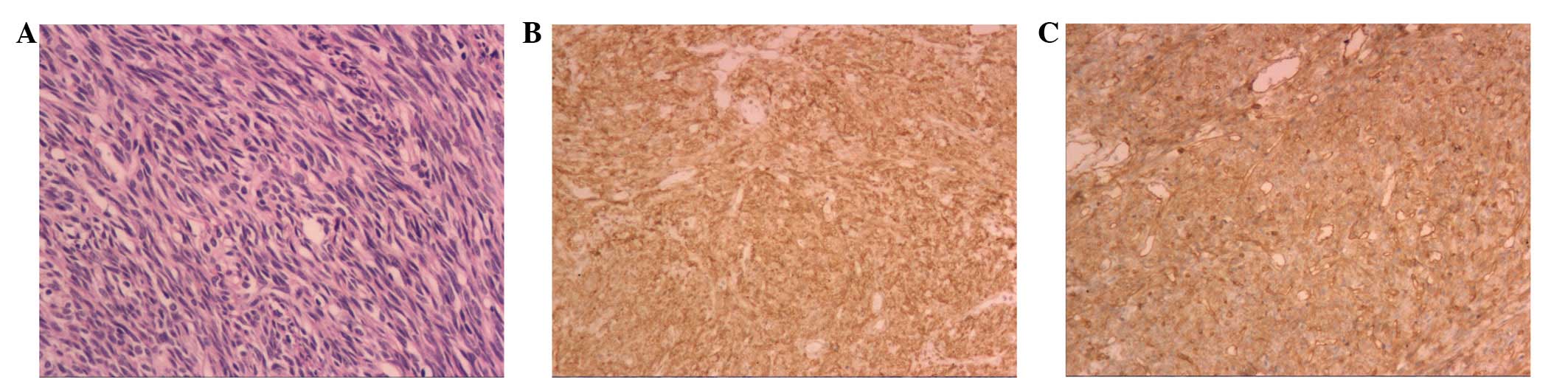
The pathological features of SFTs show that the
tumors are comprised of spindle or short spindle cells and varying
quantities of vascular tissue. Due to the diversity in the number
of blood vessels and the uneven cell density, the organizational
structure varies; it usually includes alternate distributions of
cell-dense and loose areas, and the two areas are often separated
by fibers. The tumor cells are spindle or short spindle cells. The
tumor tissue may be storiform, bundle-like, fishbone-like,
hemangiopericytoma-like (staghorn-like vessels), fence-like or
wavy. In the dense areas and porous intervals, collagen fibers with
various ranges in thickness and shape are observed. At the endpoint
of the disease, the tumor is keloid-like, occasionally with visible
radial asbestos-like collagen fibers, and commonly exhibits
collagen degeneration of the blood vessel walls. The mesenchyme
often shows mucus deterioration and mast cell infiltration with
multinucleated cells. Immunohistochemical examination reveals
diffuse reactivity for CD34 and vimentin and positive expression
for bcl-2 (80–100%) and CD99 (75–100%), but negative expression for
EMA and S-100 proteins. This typical presentation of
characteristics was evident in the present case; the diffuse
reactivity for CD34 and the negative expression of CK, EMA and
S-100 protein were observed (Fig.
2). The histological and detailed immunohistological
observations confirmed the diagnosis of sellar diaphragm SFT. Cui
et al(6) stated that
atypical and malignant forms of SFT are diagnosed by the following
characteristics: increased cell density, apparent nuclear atypia,
visible karyokinesis, cell necrosis and resemblance to fibrosarcoma
or malignant fibrous histiocytoma. No such characteristics were
observed in the present case.
The majority of SFTs are benign tumors and may be
cured following radical surgery. SFT in the sellar region has its
own particularity; it is seldomly diagnosed pre-operatively and
surgery may be performed by two approaches. If the initial
diagnosis is of a pituitary tumor, transsphenoidal surgery may be
carried out. This usually causes excessive blood loss and complete
removal of the tumor is not possible. Thus, a secondary craniotomy
is then required. In the present case, the pre-operative diagnosis
was of a pituitary tumor or meningioma, but the two were atypical.
To achieve a total resection, surgery was performed via a right
pterional approach. Block-cutting resection surgery was carefully
conducted through a high-power lens. The tumor base was located on
the sellar diaphragm of the left anterior side of the pituitary
stalk, where the tumor exhibited apparent bleeding. Following total
tumor resection, the anterior communicating artery complex, optic
nerve, optic chiasm, pituitary stalk and pituitarium were clearly
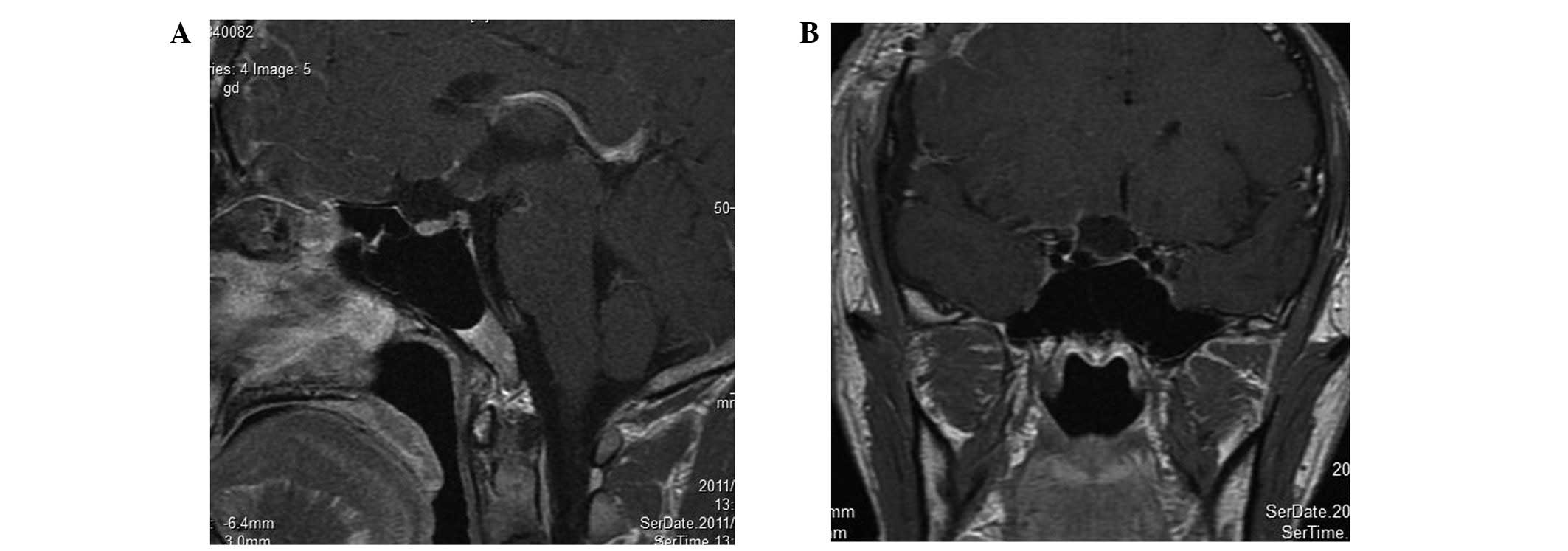
displayed. A one-week post-operative enhanced MRI revealed no tumor
recurrence (Fig. 3).
Acknowledgements
The authors would like to thank the
clinical research coordinators of the General Hospital of Jinan
Military Area Command of Chinese PLA for their support with the
treatment of the patient.
References
|
1
|
England DM, Hochholzer L and McCarthy MJ:
Localized benign and malignant tumors of the pleura. A
clinicopathologic review of 223 cases. Am J Surg Pathol.
13:640–658. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Cassarino DS, Auerbach A and Rushing EJ:
Widely invasive solitary tumor of the sphenoid sinus, cavernous
sinus, and pituitary fossa. Ann Diagn Pathol. 7:169–173. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Kim HJ, Lee HK, Seo JJ, et al: MR imaging
of solitary fibrous tumors in the head and neck. Korean J Radiol.
6:136–142. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Furlanetto TW, Pinheiro CF, Oppitz PP, de
Alencastro LC and Asa SL: Solitary fibrous tumor of the sella
mimicking pituitary adenoma: an uncommon tumor in a rare location -
a case report. Endocr Pathol. 20:56–61. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yin W, Ma C, Wu J, Cai B and You C: A
primary atypical solitary fibrous tumor of the sella mimicking
nonfuctional pituitary adenoma: a case report. Acta Neurochir
(Wien). 152:519–522. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Cui HJ, Wang ZC, Li TD, et al:
Clinicopathological observation of malignant solitary fibrous tumor
in sellar region. Chin J Min Invasive Neurosurg. 8:340–342.
2011.(In Chinese).
|
|
7
|
Martin AJ, Fisher C, Igbaseimokumo U,
Jarosz JM and Dean AF: Solitary fibrous tumours of the meninges:
case series and literature review. J Neurooncol. 54:57–69. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Johnson MD, Powell SZ, Boyer PJ, Weil RJ
and Moots PL: Dural lesions mimicking meningiomas. Hum Pathol.
33:1211–1226. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Nawashiro H: Intracranial solitary fibrous
tumor of the meninges. Hum Pathol. 31:15362000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ogawa K, Tada T, Takahashi S, et al:
Malignant solitary fibrous tumor of the meninges. Virchows Arch.
444:459–464. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Saceda-Gutiérrez JM, Isla-Guerrero AJ,
Pérez-López C, et al: Solitary fibrous tumors of the meninges:
report of three cases and literature review. Neurocirugia (Astur).
18:496–504. 2007.(In Spanish).
|
|
12
|
Adeleye AO, Ogun OA and Ogun GO: Orbital
solitary fibrous tumor. Another rare case from Africa. Int
Ophthalmol. 30:315–318. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kessler A, Lapinsky J, Berenholz L,
Sarfaty S and Segal S: Solitary fibrous tumor of the nasal cavity.
Otolaryngol Head Neck Surg. 121:826–828. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kim TA, Brunberg JA, Pearson JP and Ross
DA: Solitary fibrous tumor of the paranasal sinuses: CT and MR
appearance. AJNR Am J Neuroradiol. 17:1767–1772. 1996.PubMed/NCBI
|
|
15
|
O’Regan EM, Vanguri V, Allen CM, Eversole
LR, Wright JM and Woo SB: Solitary fibrous tumor of the oral
cavity: clinicopathologic and Immunohistochemical study of 21
cases. Head Neck Pathol. 3:106–115. 2009.PubMed/NCBI
|
|
16
|
Jeong AK, Lee HK, Kim SY and Cho KJ:
Solitary fibrous tumor of the parapharyngeal space: MR imaging
findings. AJNR Am J Neuroradiol. 23:473–475. 2002.PubMed/NCBI
|