Introduction
Liposarcoma is the most common type of soft-tissue
sarcoma. However, head and neck liposarcomas are unusual,
accounting for only 1.8–6.3% of cases (1). Furthermore, cases of liposarcoma in
the retropharyngeal space are extremely rare. To the best of our
knowledge, only five cases have been reported previously (1–5).
Unlike previous cases, the present study reports a highly unusual
case of retropharyngeal liposarcoma with rapidly worsening dyspnea
and total dysphagia following an accident and subsequent surgery.
Due to the difficulties of biopsy, radiological examination and
pathohistological examination, a retropharyngeal
well-differentiated liposarcoma may be easily misdiagnosed as a
lipoma. The retropharyngeal space is extremely close to vital
neurovascular structures and the extent of any surgical excision is
restricted to avoid severe complications. These difficulties may
affect the prognosis of patients with retropharyngeal liposarcoma.
In the present study, the diagnosis, treatment and prognosis of
this disease is discussed by analyzing the present case and by
reviewing previously reported cases. This study was approved by the
ethics committee of the Second Affiliated Hospital, School of
Medicine, Zhejiang University. Written informed consent was
obtained from the patient.
Case report
A 58-year-old male patient presented with rapidly
worsening dyspnea and total dysphagia occurring within several
hours. Three years earlier the patient had noted bilateral neck
swelling. The swelling grew slowly and one year later the patient
developed mild dysphagia. As the patient was unaware of the
potential severity of the symptom, a prompt examination and
treatment were not provided. This symptom did not markedly progress
until the occurrence of a traffic accident. Due to this accident,
the patient underwent tibiofibular fracture surgery at a local
hospital. Post-operatively, the patient recovered well and ate as
usual. However, three days subsequent to the surgery, the patient
suddenly developed rapidly worsening dyspnea and total dysphagia.
Attempts at intubation failed, so a tracheostomy was performed
under local anesthesia. The patient was then referred to the
Department of Otolaryngology (Second Affiliated Hospital, Zhejiang
University, Hangzhou, China). A physical examination revealed an
extremely large, soft, non-tender mass measuring ∼11×10×8 cm,
involving the bilateral neck. A laryngoscopy showed a
retropharyngeal mass that was reducing the space of the pharynx. A
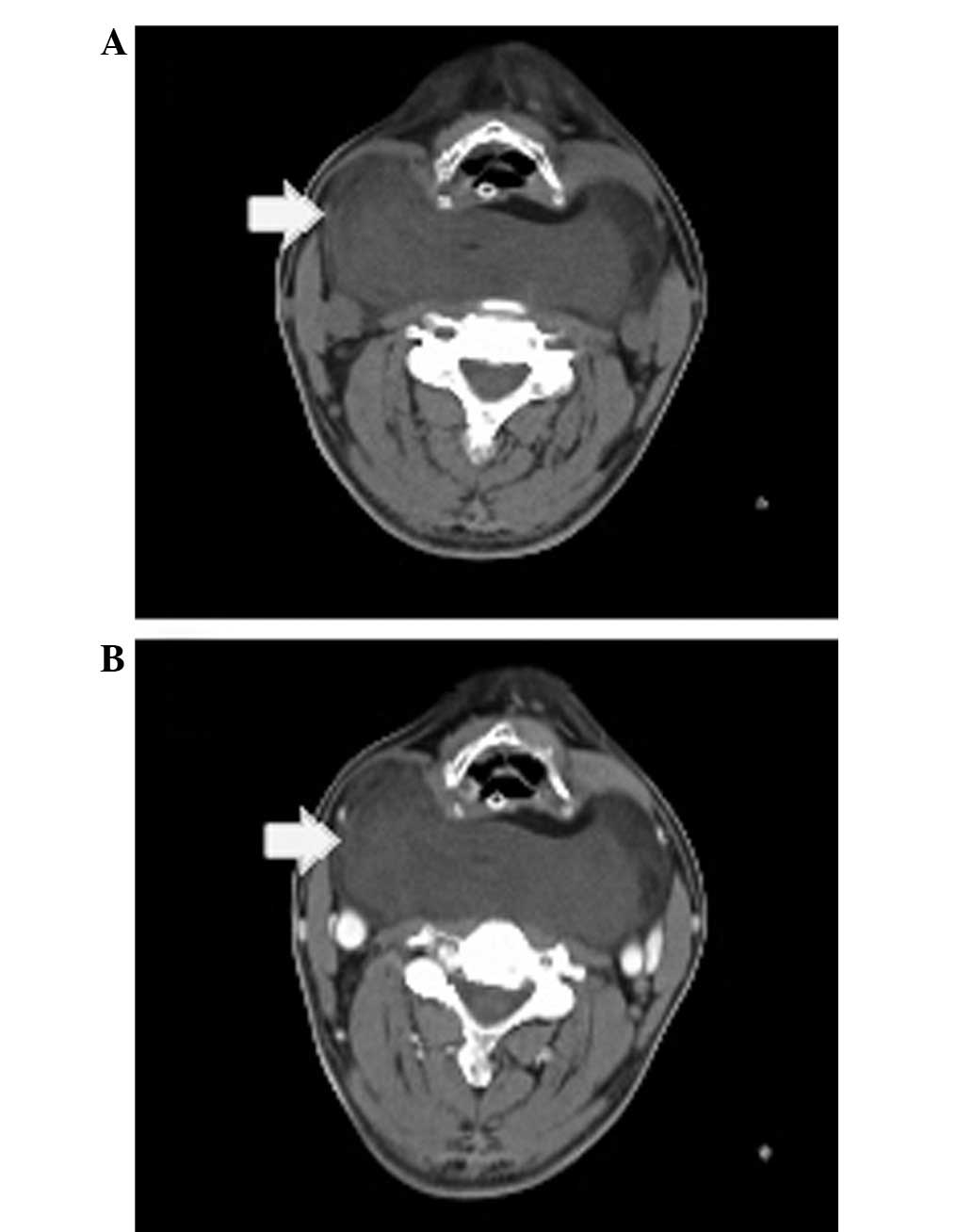
computed tomography (CT) scan of the neck revealed a large,
well-circumscribed, fatty, dense mass measuring 11×11×9 cm, which
extended from the retropharyngeal space to the sides of the neck
and from the level of the hyoid bone to the superior margin of the
mediastinum. The mass displaced the trachea and larynx anteriorly
and the carotid arteries laterally. The mass was not enhanced
following contrast agent administration (Fig. 1A and B). Due to the internal
fixation of the leg, magnetic resonance imaging (MRI) was not an
option. In addition, a CT scan of the chest and abdomen was
performed and no similar mass was observed.
An ultrasound-guided core biopsy of the mass
revealed histological components of fibrous, vascular and fatty
tissues. An incisional biopsy of the lesion was then performed with
the patient under local anesthesia. The histology indicated a
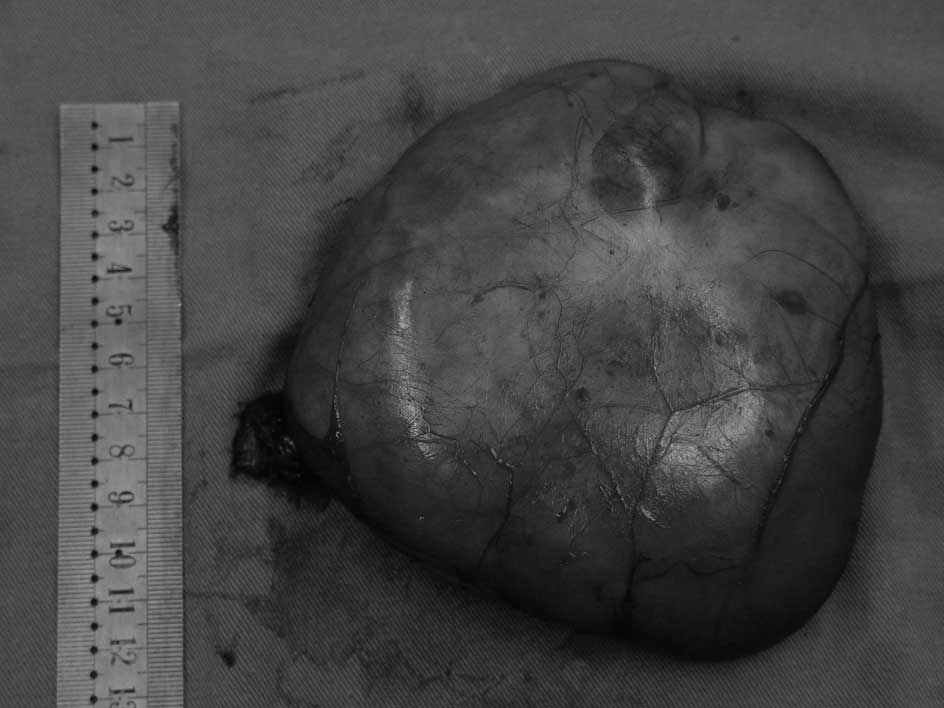
vascular fibrous lipoma. Subsequently, a surgical excision of the
retropharyngeal mass was performed under general anesthesia using
an H-shaped incision. The tumor was well-encapsulated and adhered
to the posterior pharyngeal wall. The tumor was subsequently
resected completely and measured as weighing 401 g (Fig. 2). The posterior pharyngeal and
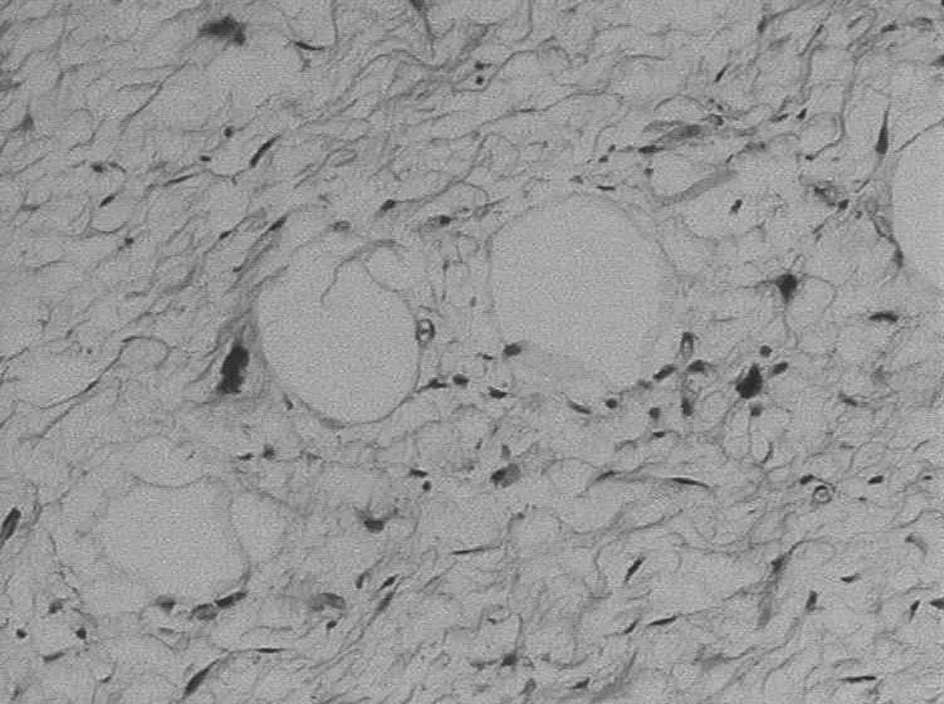
esophageal walls were completely preserved. Microscopically, the
lesion had components of mature adipocytes and lipoblasts with
nuclear atypia (Fig. 3). A
diagnosis of a well-differentiated liposarcoma was confirmed. The
suggested adjuvant radiotherapy was not accepted by the
patient.
During the post-operative course, the patient
developed vocal hoarseness. A laryngoscopy revealed right-sided
vocal fold weakness, which the patient recovered from one month
later. The patient was decannulated and the nasogastric tube was
removed. Upon follow-up at 20 months, there were no signs of either
local tumor recurrence or distant metastasis.
Discussion
The retropharyngeal space is the potential space
lying between the prevertebral fascia posteriorly and the
buccopharyngeal membrane covering the constrictor muscles
anteriorly. It extends from the skull base to the mediastinum. The
retropharyngeal space is separated from the parapharyngeal space by
a thin fascial layer and closed by the internal jugular vein,
common carotid artery and vagus nerve. Liposarcomas usually present
as painless enlarging masses and when they arise in the
retropharyngeal space they are difficult to detect early and are
usually discovered incidentally. Patients with a retropharyngeal
mass usually present with dysphagia and foreign body sensation and
when these symptoms are not as clear the patients may become
habituated to their symptoms. Physical findings include bilateral
neck swelling and a reduced anteroposterior diameter of the
pharynx, although these do not appear until the tumors have reached
a large size (1–5). In the present case, as in all five
previously reported cases, prior to the liposarcoma being
identified, it had attained an extremely large size and compressed
the pharynx, causing dysphagia and ultimately dyspnea. However,
unlike previous cases, the present patient presented rapidly
worsening dyspnea and total dysphagia following tibiofibular
fracture surgery. This indicates that stresses, including trauma or
surgery, may stimulate the growth of the tumor. Similarly, stress
and surgical intervention have also been demonstrated to promote
tumor development in another study (6). However, the mechanism remains unclear.
Natural killer cell activity and β-adrenergic receptors may be
involved in this process (6).
Lipocytes of various shapes and sizes with nuclear
atypia indicate a diagnosis of liposarcoma. The classification
proposed by Enzinger and Weiss is widely accepted and has been
adopted by the World Health Organization. This classification
identifies four subtypes of liposarcoma: well-differentiated,
myxoid, dedifferentiated and pleomorphic (7). The histological appearances of these
vary from well-differentiated neoplasms with scattered atypical
cells to pleomorphic neoplasms resembling high-grade malignant
fibrous histiocytomas (7). CT and
MRI scans aid in establishing a diagnosis. Murphey et al
indicated that well-differentiated liposarcomas are frequently
diagnosed in CT or MRI scans, with a largely lipomatous mass
(>75% of the lesion) and non-lipomatous components in thick
septa or focal nodules (8). The
identification of a nodular dominant focus (>1 cm in size) of
non-lipomatous tissue using CT or MRI suggests a dedifferentiated
liposarcoma (8,9). Myxoid liposarcomas have a high water
content and pleomorphic liposarcomas are high-grade sarcomatous
lesions that typically appear as heterogeneous soft-tissue masses
(8). However, a well-differentiated
liposarcoma is difficult to distinguish from a lipoma by CT or MRI
scans and is commonly misdiagnosed, even with a biopsy. Notably,
all reported cases, including the present case, were
well-differentiated liposarcoma, although 33.3% were misdiagnosed
as lipoma pre-operatively (1–5). In
retropharyngeal liposarcomas, due to the deep location and the
large tumor, a core biopsy or incisional biopsy usually obtains
only a small part of the tumor. This may be one of the reasons
behind the frequent misdiagnoses.
The principal management approach for liposarcoma is
wide surgical excision. However, in the head and neck, the lesion
is usually close to vital neurovascular structures, so the extent
of surgical excision is restricted to avoid severe complications
and the use of adjuvant radiotherapy is increasing. Certain studies
have demonstrated the effect of radiotherapy in reducing the rate
of local recurrence of liposarcomas (10). Eeles et al observed that
adjuvant radiotherapy significantly decreased the rate of local
recurrence of head and neck sarcomas (11). Our previous study also showed that
adjuvant radiotherapy is important in the management of sarcomas of
the parapharyngeal space (12).
However, for well-differentiated liposarcomas of the head and neck,
certain authors have suggested that wide surgical resection is
sufficient (13). The majority of
studies have been confined by the small series of patients used to
assess the value of adjuvant radiotherapy in the treatment of head
and neck liposarcomas (14,15).
Among the various series of retropharyngeal
liposarcomas in the literature, only one patient received adjuvant
radiotherapy in the initial treatment and the follow-up revealed no
evidence of recurrence (2). Among
the other five patients with surgery alone, only one patient
developed recurrence within a year and received re-excision with
adjuvant radiotherapy (1). Six
months after re-excision, there were no signs of recurrence
(1). Additionally, from these five
patients, the follow-up of the present patient was the longest and
there have been no signs of either recurrence or metastasis.
Although the reported periods of follow-up were not long enough,
with two cases with a follow-up of less than one year (2,3), one
case with no follow-up reported (4)
and the other three, including the present case, reporting a
follow-up of between 18 and 20 months (1,5), no
clear benefits of adjuvant radiotherapy were observed.
The major prognostic factor for liposarcoma is the
histological subtype. Well-differentiated liposarcoma is the most
common subtype of all liposarcomas, recurring locally, but rarely
metastasizing (16). Patients with
this type of liposarcoma have an improved prognosis compared with
those with other subtypes (17).
Myxoid tumors, similar to the well-differentiated variety, are
unlikely to metastasize and have a favorable five-year survival
rate. However, these tumors have high local recurrence rates and
are more locally invasive (18).
The other two subtypes are significantly more aggressive and have
worse prognoses (18).
Although all six reported cases of retropharyngeal
liposarcoma were of the well-differentiated subtype, certain
characteristics of this unusual tumor may affect the prognosis due
to its unique localization. Late detection may provide sufficient
time for tumor invasion and metastases to occur. Misdiagnosis may
lead to the diagnosis of a benign lesion, which may result in a
limitation of the extent of surgical excision. In addition,
liposarcomas located in deep anatomical sites, including the
retroperitoneum and mediastinum, have a relatively unfavorable
prognosis (19). This may be due to
the difficulties of using adequate surgical margins. Similarly, in
the head and neck, patients with facial, scalp and laryngeal tumors
have an improved prognosis compared with those with intraoral,
pharyngeal and neck tumors (19).
The retropharyngeal space is a deep potential space that is
extremely close to vital neurovascular structures, so the extent of
excision is restricted to avoid severe complications. The
difficulties of surgery may also affect the prognosis of patients
with retropharyngeal liposarcoma.
In conclusion, although well-differentiated
liposarcoma is the most common subtype of liposarcoma and has an
improved prognosis, retropharyngeal liposarcoma has a number of
unfavorable prognostic factors due to its unique localization. No
adequate evidence has demonstrated the value of adjuvant
radiotherapy for treating retropharyngeal liposarcomas. However,
for liposarcomas, adjuvant radiotherapy has been shown to decrease
the rate of local recurrence in a number of literature studies.
References
|
1
|
Yueh B, Bassewitz HL and Eisele DW:
Retropharyngeal liposarcoma. Am J Otolaryngol. 16:331–340. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Gundelach R, Ullah R, Coman S and Campbell
K: Liposarcoma of the retropharyngeal space. J Laryngol Otol.
119:651–654. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Menown IB, Liew SH, Napier SS and Primrose
WJ: Retro- pharyngeal liposarcoma. J Laryngol Otol. 106:469–471.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hermans R, Dewitte B, Delaere P, Feenstra
L and Baert AL: Retropharyngeal liposarcoma. J Belge Radiol.
76:176–177. 1993.PubMed/NCBI
|
|
5
|
Prince ME, Nasser JG, Fung BR and
Broderick I: Liposarcoma of the retropharyngeal space: review of
the literature. J Otolaryngol. 26:139–142. 1997.PubMed/NCBI
|
|
6
|
Lee LW, Shahzad MM, Lin YG, Armaiz-Pena G,
Mangala LS, Han HD, et al: Surgical stress promotes tumor growth in
ovarian carcinoma. Clin Cancer Res. 15:2695–2702. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Enzinger FM and Weiss SW: Soft Tissue
Tumours. 2nd edition. Mosby; St. Louis, MO: pp. 346–382. 1988
|
|
8
|
Murphey MD, Arcara LK and Fanburg-Smith J:
From the archives of the AFIP: imaging of musculoskeletal
liposarcoma with radiologic-pathologic correlation. Radiographics.
25:1371–1395. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang Y and Shi H: Dedifferentiated
liposarcoma of the neck: CT fingdings. AJNR Am J Neuroradiol.
33:E4–E6. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Suit HD, Russell WO and Martin RG: Sarcoma
of soft tissue: clinical and histopathologic parameters and
response to treatment. Cancer. 35:1478–1483. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Eeles RA, Fisher C, A’Hern RP, Robinson M,
Rhys-Evans P, Henk JM, et al: Head and neck sarcomas: prognostic
factors and implications for treatment. Br J Cancer. 68:201–207.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Yang BB, Jiang H and Chang HY: Malignant
triton tumour of the parapharyngeal space: a case arising from the
cervical sympathetic nerve. J Laryngol Otol. 122:531–534.
2008.PubMed/NCBI
|
|
13
|
Nouri H, Hassani R, Aderdour L and Raji A:
The well-differentiated liposarcoma of the hypopharynx. Eur Ann
Otorhinolaryngol Head Neck Dis. 128:143–145. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rogers J, Patil Y, Strickland-Marmol L and
Padhya T: Lipomatous tumors of the parapharyngeal space: case
series and literature review. Arch Otolaryngol Head Neck Surg.
136:621–624. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Makeieff M, Pelliccia P, Poizat F, Arnaud
S, Rat F, Cupissol D, Guerrier B and Costes V: Laryngeal
dedifferentiated liposarcoma. Eur Arch Otorhinolaryngol.
267:991–994. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Enzinger FM and Winslow DJ: Liposarcoma: a
study of 103 cases. Virchows Arch Pathol Anat Physiol Klin Med.
335:367–388. 1962. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Saunders JR, Jacques DA, Casterline PF,
Percarpio B and Goodloe S Jr: Liposarcomas of the head and neck: a
review of the literature and addition of four cases. Cancer.
43:162–168. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Golledge J, Fisher C and Rhys-Evans PH:
Head and neck liposarcoma. Cancer. 76:1051–1058. 1995. View Article : Google Scholar
|
|
19
|
Stout AP: Liposarcoma - the malignant
tumor of lipoblasts. Ann Surg. 119:86–107. 1944.PubMed/NCBI
|