Introduction
Phyllodes tumors (PTs) of the breast are rare
biphasic fibroepithelial tumors, characterized by the proliferation
of stromal and epithelial cells (1,2). They
account for 0.4–1% of all breast tumors and occur most frequently
between the ages of 40 and 50 years (3). In the majority of cases, the tumor
grows faster than any other tumor would; PT usually presents as a
large lump of 3–5 cm in size when patients visit a doctor. The
current study presents the case of a patient with an ∼11 kg PT
measuring 45 cm at the maximum diameter, who exhibited a composite
of multiple chronic diseases. The study also presents a review of
the literature. We propose that this report may be useful for the
diagnosis and treatment of PT. Written informed consent was
obtained from the patient.
Case report
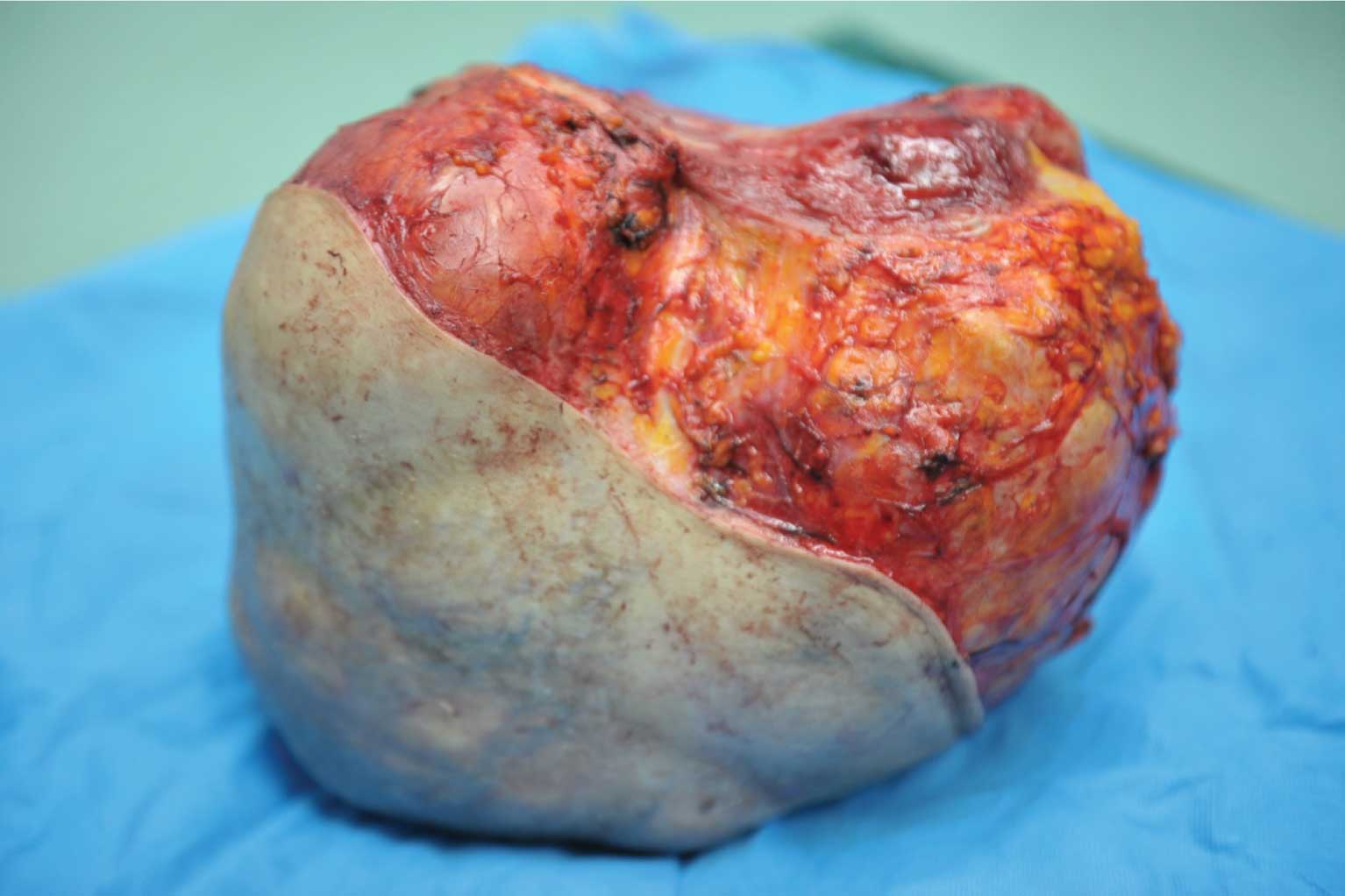
A 63-year-old female patient was admitted to the
Galactophore Department, Bao Ji Central Hospital with a huge lump
in the left breast. The patient stated that they had identified a
thumb-sized lump two years earlier, but that they had ignored it.
From July 2011, the patient observed that the lump was growing
rapidly; in February 2012 the lump had become so large that the
patient’s left chest was entirely covered with a solid,
irregularly-shaped, somewhat moveable mass of tremendous size and
the patient was barely able to lie in the prone position. Family
members then finally convinced the patient to seek medical
attention. Upon physical examination, the patient presented with an
elastic hard mass in the left breast that was 45 cm in diameter,
with a circumference of 97 cm (Fig.
1). Rapid growth had resulted in shiny stretched skin that was
translucent, showing underlying extremely enlarged veins with
sections of the circuitous veins about to undergo ulceration,
although no bleeding or discharge was noted. The lymph nodes in the
axillary and other superficial areas were not palpable. The
patient’s previous medical history revealed that they had high
blood pressure, diabetes and atrial fibrillation. Moreover, the
patient had suffered from a cerebral infarction; the patient’s
right side was paralyzed and communicative disorders had appeared
two years previously. The patient was unable to care for herself
due to the cerebral infarction. The patient’s medical history was
negative for allergies, smoking, drinking, contagions and serious
addiction. Furthermore, there was no family history of breast
cancer on either side of the patient’s family.
Due to the non-compressible nature of the mass and
the size of the tumor, regular breast examinations, including
mammography and ultrasound studies, could not be used, while a
computed tomography (CT) scan of the chest revealed a solid mass.
Total body scintigraphy was negative. Comprehensive examinations
and detailed assessments were additionally performed on the patient
due to the presence of high blood pressure, diabetes, atrial
fibrillation and cerebral infarction. In order to ensure the
long-term success of the treatment, a consultation with the
Respiratory Medicine, Vasculocardiology, Neurology and
Anesthesiology departments was organized. Antihypertensive,
glycemic control, oxygen uptake and antiarrhythmic therapies were
administered prior to surgery. The pectoris major and minor had
atrophied and were tightly adhered to the tumor due to long-term
compression, so the surgeon decided to resect the mass along with
these muscles. The mass was resected subsequent to 3 hours of
surgery (Fig. 2). The
post-operative pathology report showed an extremely large grey
mass, weighing 11 kg and measuring 36×40×18 cm, which was covered
by ∼32×35 cm of skin tissue. When the tumor was cut into halves
along the nipple, it was observed that the majority of the tumor
tissue was a myxoid, lobulated mass with multiple hollow cavities,
thick, yellow, viscous fluid and certain necrotic areas. The
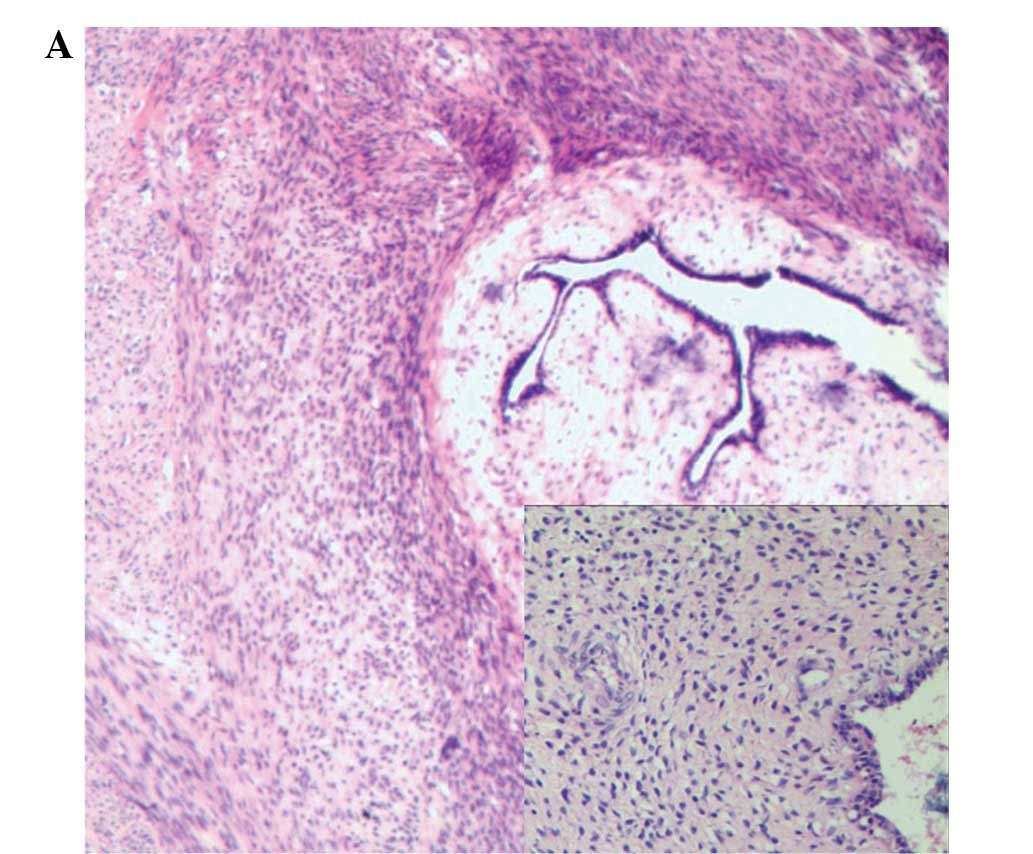
microscopy findings showed extensive necrosis and the majority of
the tumor tissue exhibited an epithelial component with a leaf-like
pattern, but no cellular atypia. The final histopathological
diagnosis was PT of the benign type (Fig. 3).
In view of the benign nature of this tumor, no
chemotherapy or radiotherapy was administered following surgery.
The patient recovered well and to date there has been no evidence
of local recurrence or distant metastasis.
Discussion
PTs, also known as cystosarcoma phyllodes, were
first named by Johannes Muller (4,5).
Muller described cystosarcoma phyllodes as leaf-like masses with a
cyst-like shape and complete envelopes. There were however,
numerous other names used to label this type of case. In 1982, the
World Health Organization (WHO) decided to use the term PT to
describe these cases in the official WHO’s standard classification
of breast diseases (6), and this
term is now commonly used.
PTs are rare tumors of the breast that account for
0.4–1% of all breast tumors, and the average age of the affected
patients is 45 (3). At present, the
exact causes of PTs remain unknown, although the majority of
researchers consider that PTs are likely to have similar epidemic
factors to fibroadenoma of the breast, which is associated with
estrogen secretion and metabolic disorders. With regard to the
clinical and histological aspects, small PTs have apparent
similarity to fibroadenomas (7).
In 1982, PTs were classified by the WHO as benign,
borderline and malignant, on the basis of cell density, atypia,
mitotic figures, tumor borders and hemorrhagic necrosis. Malignant
tumors (either low- or high-grade) are common in elderly females
and exhibit frequent metastasis (lymphatic and blood-borne) with a
high mortality rate (8). Malignant
PTs have a high rate of recurrence and the axillary and
supraclavicular lymph nodes are commonly enlarged (9). However, 70–90% of all PTs are benign
tumors that do not metastasize, although they exhibit continuous
growth and rapidly increase in size in a short time. Due to the
overlapping histological and clinical features between small PTs
and fibroadenomas, there are no known tumor markers or blood tests
to aid in the confirmation of the diagnosis. Consequently, it is
easy to misdiagnose the majority of PTs as fibroadenomas. The
differentiation of PTs from benign fibroadenomas is difficult using
ultrasound, mammograms and magnetic resonance imaging (MRI).
Adamietz et al (10)
suggested that real-time elastography may be sufficient to
differentiate between these two lesions. The authors proposed that
all PTs have a similar elastic pattern with an elastic center and
inelastic outer limits, although this pattern was also observed in
5% of all fibroadenomas. A study by Bandyopadhyay et al
(11) attempted to make the
distinction from a cytologists’ perspective. The study suggested
that the size, cellularity of stromal fragments and proportion of
spindle cells in the background are significant features in such
differentiation. Spindle cells appear to be present in large
numbers in PTs compared with fibroadenomas.
The primary treatment for PTs is surgery, although
the most suitable type of surgery is debatable (wide local excision
or total mastectomy). In certain cases, there may be a requirement
to resect the pectoris major and minor. If the mass is >5 cm or
malignant, wide local excision is recommended. Although
chemotherapy, radiotherapy and local lymph node dissection are not
used in conventional treatment modalities for PTs, they may be
useful for patients with aggressive tumors, positive margins and
high mitotic rates, as well as for those with recurrence (12). The recurrence rate in benign tumors
(5–15%) is lower than in malignant tumors (20–30%). Certain studies
have shown that the overall five-year disease-free survival rate
ranges from 78–91% and that the resection margin and size of the
tumor may be key factors (13).
In summary, PTs of the breast are rare and the
present malignant PT is notable due to its large size and weight of
∼36×40×18 cm and 11 kg, respectively, in combination with the
presence of other chronic diseases. We suggest that this report may
be useful for the diagnosis and treatment of future PT
patients.
References
|
1.
|
Guerrero MA, Ballard BR and Grau AM:
Malignant phyllodes tumor of the breast: review of the literature
and case report of stromal overgrowth. Surg Oncol. 12:27–37. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Sabban F, Collinet P, Lucot JP, Boman F,
Leroy JL and Vinatier D: Phyllodes tumor of the breast: analysis of
8 patients. J Gynecol Obstet Biol Reprod (Paris). 34:252–256.
2005.(In French).
|
|
3.
|
El Khouli RH and Louie A: Case of the
season: a giant fibroadenoma in the guise of a phyllodes tumor;
characterization role of MRI. Semin Roentgenol. 44:64–66.
2009.PubMed/NCBI
|
|
4.
|
Sanguinetti A, Bistoni G, Calzolari F, et
al: Cystosarcoma phyllodes with muscular and lymph node metastasis.
Our experience and review of the literature. Ann Ital Chir.
83:331–336. 2012.PubMed/NCBI
|
|
5.
|
Lee BJ and Pack GT: Giant intracanalicular
myxoma of the breast. The so-called cystosarcoma phyllodes mammae
of Johannes Muller. Ann Surg. 93:250–268. 1931.PubMed/NCBI
|
|
6.
|
Stone-Tolin K, Pollak EW, Dorzab W, et al:
Recurring cystosarcoma phyllodes associated with breast carcinoma.
South Med J. 75:881–884. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Grenier J, Delbaldo C, Zelek L, et al:
Phyllodes tumors and breast sarcomas: a review. Bull Cancer.
97:1197–1207. 2010.(In French).
|
|
8.
|
Luini A, Aguilar M, Gatti G, et al:
Metaplastic carcinoma of the breast, an unusual disease with worse
prognosis: the experience of the European Institute of Oncology and
review of the literature. Breast Cancer Res Treat. 101:349–353.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Lenhard MS, Kahlert S, Himsl I, Ditsch N,
Untch M and Bauerfeind I: Phyllodes tumour of the breast: clinical
follow-up of 33 cases of this rare disease. Eur J Obstet Gynecol
Reprod Biol. 138:217–221. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Adamietz BR, Kahmann L, Fasching PA, et
al: Differentiation between phyllodes tumor and fibroadenoma using
real-time elastography. Ultraschall Med. 32(Suppl 2): E75–E79.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Bandyopadhyay R, Nag D, Mondal SK,
Mukhopadhyay S, Roy S and Sinha SK: Distinction of phyllodes tumor
from fibroadenoma: Cytologists’ perspective. J Cytol. 27:59–62.
2010.PubMed/NCBI
|
|
12.
|
Pimiento JM, Gadgil PV, Santillan AA, et
al: Phyllodes tumors: race-related differences. J Am Coll Surg.
213:537–542. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Ben Hassouna J, Damak T, Gamoudi A, et al:
Phyllodes tumors of the breast: a case series of 106 patients. Am J
Surg. 192:141–147. 2006.PubMed/NCBI
|