Introduction
Glomus tumors are neoplasms that arise from modified
smooth muscle cells of the glomus body, which is a specialized form
of an arteriovenous anastomosis that plays a significant role in
the regulation of skin circulation (1,2).
Glomus tumors were first described in 1924 by Masson, who compared
the tumors with the normal glomus body and suggested that the
lesion represented hyperplasia or overgrowth of this structure
(3). It is now well accepted that
the lesions are neoplastic.
Glomus tumors have been reported to account for 1–6%
of all soft-tissue tumors and 1–5% of hand tumors (4). The tumors may occur during adult life
at 20–40 years of age and are equally represented in males and
females. In a large series by Beaton and Davis (5), extradigital tumors were more common in
males, while subungual lesions predominantly affected females.
Classic glomus tumors are typically solitary, though they may
rarely occur as multiple nodules (2,6,7).
Multiple lesions have been reported in neurofibromatosis-1
(8). Malignant transformation is
rarely reported (9–11).
Clinical manifestations include paroxysms of pain,
cold sensitivity and point tenderness. In certain patients the pain
is accompanied by additional signs of hyperesthesia, muscle atrophy
or osteoporosis of the affected area (12).
Grossly, the tumor is a small purple nodule that
varies between 2 and 20 mm in diameter, though tumors of >3 cm
have been reported (13).
Histologically, the tumors have variable quantities of glomus
cells, blood vessels and smooth muscle cells. Accordingly, they are
classified as solid glomus tumors, glomangiomas and glomangiomyomas
(14). Solid glomus tumors are the
most common subtype (73%), followed by glomangiomas (25%).
Glomangiomyoma is the rarest variant with a frequency of 8% of all
glomus tumors (15).
The present study reports a case of a glomus tumor
of the shoulder and discusses the histological and
immunohistochemical features.
Case report
Patient and treatment
A 30-year-old female was referred to the Department
of Thoracic Surgery (University of Pisa, Pisa, Italy) with a 1-year
history of shoulder pain and paresthesia of the left arm. Upon
physical examination, the range of motion of the left shoulder was
normal.
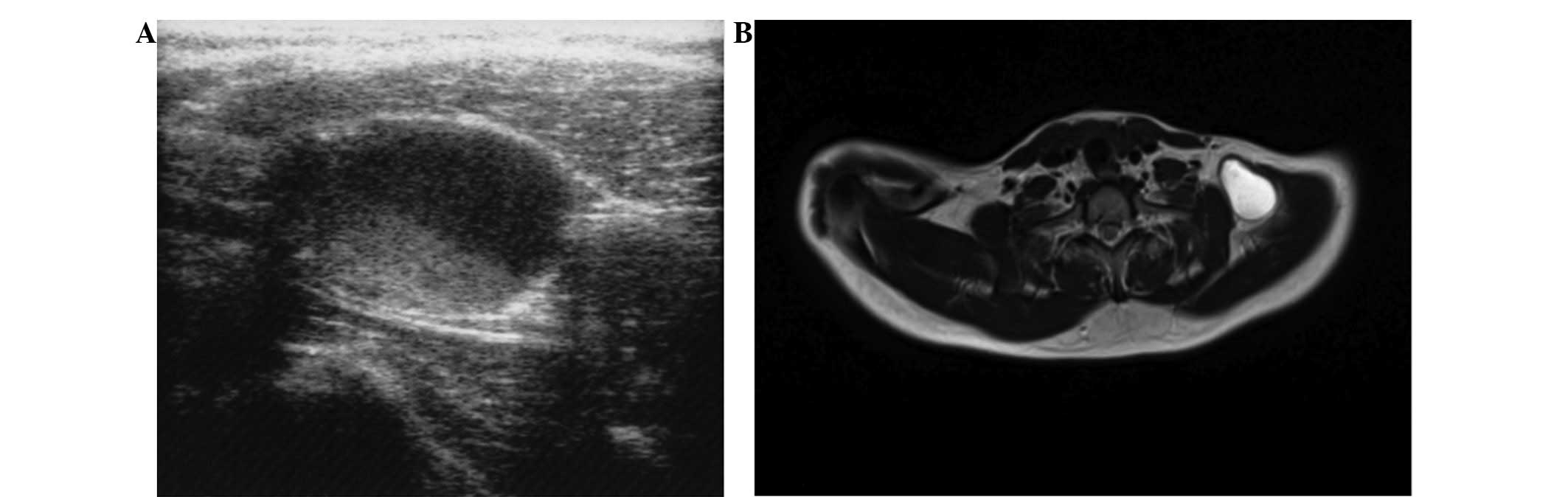
Ultrasonography of the supraclavicular area revealed
a well-defined hypoechoic oval mass measuring ~3.5 cm. MRI of the
shoulder confirmed the presence of a cystic neoformation measuring
~4 cm located between the trapezius and levator scapulae muscles
(Fig. 1).
The patient was treated by a wide excision of the
mass with a surgical incision in the neck, laterally to the
sternocleidomastoid muscle. The patient did not undergo any further
treatment following the excision and did not have any
recurrence.
Specimens
Excised specimens were fixed in 10% neutral buffered
formaldehyde and embedded in paraffin. Routine hematoxylin and
eosin staining was performed on the microscopic section for
histopathological examination.
Immunohistochemistry
A paraffin block was chosen for immunohistochemical
study. An immunohistochemical evaluation was performed using the
avidin-biotin-peroxidase complex method. Antibodies were purchased
from Ventana Medical Systems (Tucson, AZ, USA). The antibodies that
were used were mouse monoclonal anti-smooth muscle actin, mouse
monoclonal anti-CD34, rabbit monoclonal anti-CD31, polyclonal
anti-factor VIII, mouse monoclonal anti-CK-Pan, mouse monoclonal
anti-CD68, mouse monoclonal anti-S-100, mouse monoclonal anti-CD99,
polyclonal anti-calretinin and mouse monoclonal anti-desmin. All
the antibodies were pre-diluted.
The analysis of the specimens was performed by two
pathologists and the differential diagnosis was widely
discussed.
Results
The specimens were obtained from a 30-year-old
female who underwent an excision of a subcutaneous mass of the
supraclavicular area.
The gross appearance of the specimen was a grayish
fragmented cystic lesion, measuring 4 cm at the maximum. The cut
sections revealed firm tissue without hemorrhagic or necrotic
areas.
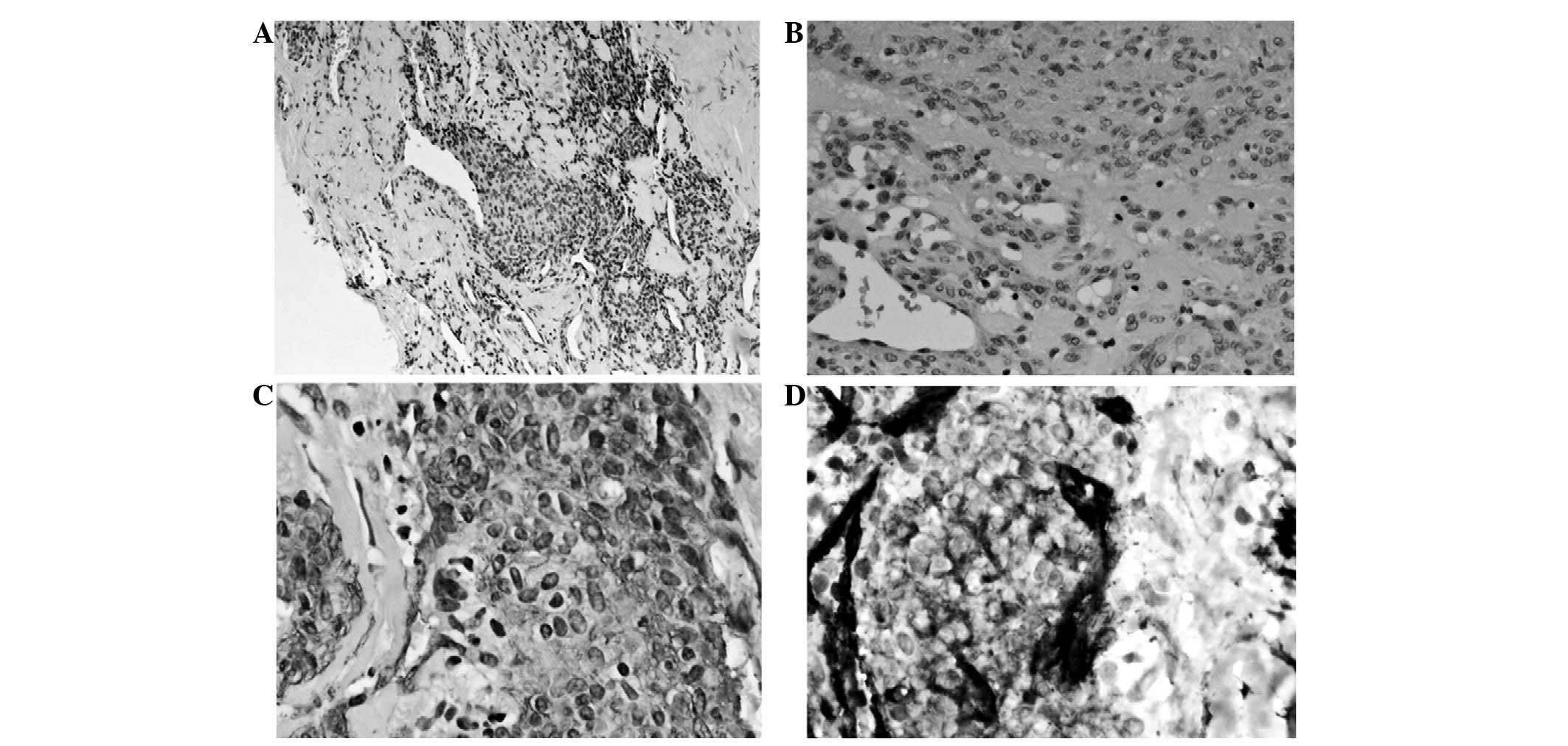
A microscopic examination showed multiple nests of
typical glomus cells surrounded by fibrous tissue with focal myxoid
changes. The glomus cells contained epithelioid elements with
moderate amounts of clear to eosinophilic cytoplasm and round
nuclei with fine chromatin. These cells were closely associated
with small vascular channels and nerves. The cells demonstrated a
low proliferative activity (Ki-67 <5%) and a low mitotic rate of
<1 mitotic figure (MF)/50 high-power fields (HPFs). The lesion
was well-circumscribed and there was no evidence of hemorrhage or
necrosis.
Immunohistochemical staining was positive for SMA
and CD34 and negative for CD31, factor VIII, CK-Pan, CD68, S-100,
CD99, calretinin and desmin (Fig.
2).
Discussion
A glomus tumor is a hamartoma that develops from a
neuromyoarterial glomus body and consists of dilated vascular
channels surrounded by proliferating glomus and nerve cells. It
accounts for 1–6% of all soft tissue tumors and 1–5% of hand tumors
(4). Glomic units are located in
the stratum reticularis of the dermis throughout the body, but they
are highly concentrated in the digits, palms and soles. The units
are most frequently encountered in the subungual region, but also
in the precoccygeal soft tissue (glomus coccygeum). The glomus body
is made of preglomic arterioles derived from the small arterioles
that supply the dermis and is lined by plump cuboidal endothelial
cells and surrounded by longitudinal and circular muscle fibers.
Scattered throughout the muscle fibers are rounded, epithelioid
glomus cells (12). The cells are
absent in children under the age of 1 year. With advancing age the
cells begin to atrophy, while the overall number of glomic units
decreases (2).
Glomus tumors are usually located in the deep dermis
of the extremities and in the subungual region of the hands. Other
sites are the shoulder (16), thigh
(17), knee (4) and gastrointestinal tract, including
the stomach (18) and liver
(19).
Malignant transformation is extremely rare, but
possible (10,11). Folpe et al(15) proposed the following classification
criteria for malignant glomus tumors: i) Deep location and a size
of >2 cm; ii) presence of atypical mitotic figures; or iii)
combination of moderate to high nuclear grade and mitotic activity
(5 MFs/50 HPFs).
The typical presentation of a bluish, painful lesion
in either a subungual or digital pulp location is now well
recognized by clinicians. However, when the lesion is extradigital,
the difficulty in forming a diagnosis often leads to delays and
misdiagnosis (20,21).
A review of the literature suggests that the
extradigital distribution along the upper extremity may be more
frequent than is generally assumed. The forearm has been noted to
be the most common extradigital location, while the shoulder and
upper back are the least frequent (12).
A glomus tumor of the shoulder has been reported in
14 cases (Table I). According to
the cumulative data, including that of the present case, the mean
age of the patients was 48.5 years (range, 30–71). There was no
gender predominance (six females and six males). The mean size of
the tumors was 1.9 cm (range, 0.5–4). Seven tumors (50%) were
located in the right shoulder, four (28%) were of the left side and
in two cases (14%), the location of the lesion was not reported. No
data were available for the cases studied by Beaton and Davis
(5) The mean duration of symptoms
was 10.75 years (range, 0.5–20 years). The data indicate that in
the subcutaneous location of the extradigital areas, the tumor only
becomes visible at a late stage, which correlates with the
enlargement of the mass. The majority of lesions are only a few
millimeters in diameter at the onset of symptoms and this limits
the usefulness of palpation in such cases. The absence of objective
findings frequently results in a diagnostic delay, a finding that
is confirmed by the protracted duration of symptoms observed in the
majority of series and case studies. Various diagnostic imaging
techniques have been reported to enhance the ability to detect
these lesions. The are no specific imaging techniques to aid in the
diagnosis. Ultrasonography, despite its low specificity, may aid in
locating the lesion. MRI provides more details of the lesion and
its association with the adjacent structures (12). It must be emphasized that a
diagnosis relies on a high index of clinical suspicion.
 | Table ISummary of the shoulder glomus tumor
cases. |
Table I
Summary of the shoulder glomus tumor
cases.
| First author/s, year
(ref.) | Age, years | Gender | Side | Size, cm | Duration of symptoms,
years |
|---|
| Bailey, 1935
(26) | 48 | M | L | 0.3 | 20.0 |
| Beaton and Davis,
1941 (5) | NA | NA | NA | NA | NA |
| Riveros and Pack,
1951 (27) | 40 | F | NR | 0.5 | NR |
| Heys, 1992 (25) | NR | NR | NR | NR | NR |
| Massey, 1992
(31) | 41 | F | R | 1.0 | Several |
| Yoshikawa, 1996
(29) | 35 | F | L | 4.0 | 20.0 |
| Roberts, 1999
(23) | 67 | M | R | 3.5 | 20.0 |
| Ghaly, 1999 (28) | 62 | M | R | 1.0 | 20.0 |
| Abela, 2000 (16) | 52 | M | R | 1.5 | 10.0 |
| Solivetti, 2002
(30) | 58 | M | R | 0.4 | 1.0 |
| Boretto, 2008
(22) | 54 | F | R | NR | 30.0 |
| Gautam, 2008
(32) | 25 | F | L | NR | 5.0 |
| Karakurum, 2009
(24) | 71 | M | R | 2.5 | 0.5 |
| Present case,
2012 | 30 | F | L | 4.0 | 1.0 |
The present study reports a case of a glomus tumor
in a young patient with a short duration of symptoms in the left
arm. The lesion was located in the left shoulder and despite its
large size, the patient experienced a short duration of symptoms,
including left arm paresthesia. Furthermore, in contrast with data
that has been previously reported in the literature, the lesion was
cystic and perivascular. A correct clinical diagnosis was obtained
from the imaging techniques (ultrasound and MRI). The surgical
excision of the lesion resulted in a complete disappearance of the
symptoms.
In conclusion, glomus tumors of the shoulder are not
as uncommon as previously believed. On this basis, in cases of
unexplained pain in this area, a glomus tumor should be considered
in the differential diagnosis.
Acknowledgements
This study has been supported, in part, by grants
from the Ministry of Education, University and Research (MIUR;
200937N3ME_003). Approval for this study was obtained from the
ethics committee of the University of Pisa. Informed consent for
the use of the tumor samples for the investigation was obtained
from the patient.
References
|
1
|
White CP and Jewer DD: Atypical
presentation of a glomus tumour. A case report. Can J Plast Surg.
14:237–238. 2006.PubMed/NCBI
|
|
2
|
Takei TR and Nalebuff EA: Extradigital
glomus tumour. J Hand Surg Br. 20:409–412. 1995. View Article : Google Scholar
|
|
3
|
Masson P: Le glomus neuromyoartérial des
régions tactiles et ses tumeurs. Lyon Chir. 21:257–280. 1924.
|
|
4
|
Akgün RC, Güler UÖ and Onay U: A glomus
tumor anterior to the patellar tendon: a case report. Acta Othop
Traumatol Turc. 44:250–253. 2010.PubMed/NCBI
|
|
5
|
Beaton LE and Davis L: Glomus tumor. Q
Bull Northwest Univ Med Sch. 15:245–254. 1941.
|
|
6
|
Moor EV, Goldberg I and Westreich M:
Multiple glomus tumor: a case report and review of the literature.
Ann Plast Surg. 43:436–438. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chiang ER and Chen TH: Multiple glomus
tumors in gastrocnemius muscle: a case report. Arch Orthop Trauma
Surg. 128:29–31. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cabral R, Santiago F and Tellechea O:
Multiple glomus tumors and segmental neurofibromatosis: there are
no coincidences. Dermatol Online J. 17:42011.PubMed/NCBI
|
|
9
|
Kayal JD, Hampton RW, Sheehan DJ and
Washington CV: Malignant glomus tumor: a case report and review of
the literature. Dermatol Surg. 27:837–840. 2001.PubMed/NCBI
|
|
10
|
Matsumoto K, Kakizaki H, Yagihashi N and
Yagihashi S: Malignant glomus tumor in the branchial muscle of a
16-year-old girl. Pathol Int. 51:729–734. 2001.PubMed/NCBI
|
|
11
|
Terenda T, Fujimoto J, Shirakashi Y, Kamo
M and Sugiura M: Malignant glomus tumor of the palm: a case report.
J Cutan Pathol. 38:381–384. 2011.PubMed/NCBI
|
|
12
|
Enzinger FM and Weiss SW: Perivascular
tumors. Soft Tissue Tumors. 4th edition. Mosby; St Louis: pp.
985–1001. 2001
|
|
13
|
Riddell DH and Martin RS: Glomus tumor of
unusual size; case report. Ann Surg. 133:401–403. 1951. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Rao AG, Indira D and Kamal J: Extra
digital glomangioma. Indian J Dermatol. 55:397–398. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Folpe AL, Fanburg-Smith JC, Miettinen M
and Weiss SW: Atypical and malignant glomus tumors: analysis of 52
cases, with a proposal for the reclassification of glomus tumors.
Am J Surg Pathol. 25:1–12. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Abela M, Cole AS, Hill GA and Carr AJ:
Glomus tumor of the scapular region. J Shoulder Elbow Surg.
9:532–533. 2000. View Article : Google Scholar
|
|
17
|
Negri G, Schulte M and Mohr W: Glomus
tumor with diffuse infiltration of the quadriceps muscle: a case
report. Hum Pathol. 28:750–752. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Bauerová L, Gabris V, Honsová E and
Povýsil C: Glomus tumor of the stomach: a case report and review of
the literature. Cesk Patol. 47:128–129. 2011.
|
|
19
|
Amoueian S, Meibodi NT, Tavoosi H,
Ekramifard VR, Attaranzadeh A and Montazer M: Primary glomus tumor
of the liver. Arch Iran Med. 14:294–295. 2011.PubMed/NCBI
|
|
20
|
Matloub HS, Muoneke VN, Prevel CD, Sanger
JR and Yousif NJ: Glomus tumor imaging: use of MRI for localization
of occult lesions. J Hand Surg Am. 17:472–475. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Leger M, Patel U, Mandal R, Walters R,
Cook K, Haimovic A and Franks AG Jr: Glomangioma. Dermatol Online
J. 16:112010.
|
|
22
|
Boretto JG, Lazerges C, Coulet B, Baldet P
and Chammas M: Calcified glomus tumor of the shoulder. A case
report. Chir Main. 27:183–186. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Roberts SN, Carter C, Brown JN, Hayes MG
and Saies A: Enormous glomus tumor of the shoulder. J Shoulder
Elbow Surg. 8:365–366. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Karakurum G, Tutar E, Pirbudak L and
Mizrak A: Glomus tumour of the deltoid muscle. A case report. Acta
Orthop Belg. 75:681–683. 2009.PubMed/NCBI
|
|
25
|
Heys SD, Brittenden J, Atkinson P and
Eremin O: Glomus tumour: an analysis of 43 patients and review of
the literature. Br J Surg. 79:345–347. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bailey OT: The cutaneous glomus and its
tumors-glomangiomas. Am J Pathol. 11:915–936. 1935.PubMed/NCBI
|
|
27
|
Riveros M and Pack GT: The glomus tumor:
report of twenty cases. Ann Surg. 133:394–400. 1951. View Article : Google Scholar
|
|
28
|
Ghaly RF and Ring AM: Supraclavicular
glomus tumor, 20-year history of undiagnosed shoulder pain: a case
report. Pain. 83:379–382. 1999.PubMed/NCBI
|
|
29
|
Yoshikawa G, Murakami M, Ishizawa M,
Matsumoto K and Hukuda S: Glomus tumor of the musculotendinous
junction of the rotator cuff. A case report. Clin Orthop Relat Res.
326:250–253. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Solivetti FM, Thorel MF, Cota C, Donati P
and Faloni E: Ultrasound pattern of glomus tumor of the shoulder.
Radiol Med. 104:481–483. 2002.PubMed/NCBI
|
|
31
|
Massey EW: Shoulder pain from glomus
tumour. J Neurol Neurosurg Psychiatry. 55:413–414. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Gautam VK, Agarwal PK, Maini L and Prakash
A: Intraosseous glomus tumor in acromion process of scapula.
Orthopedics. 31:4062008. View Article : Google Scholar : PubMed/NCBI
|