Introduction
Breast cancer is one of the most common cancers in
females and one of the main causes of cancer-related mortality
worldwide (1). In China, the
incidence and mortality rates of breast cancer have continuously
increased (2,3). Chinese patients with breast cancer
exhibit a more invasive ductal carcinoma with larger tumor sizes
and higher human epidermal growth factor receptor 2 (Her-2)
overexpression than patients from the West (4).
Her-2 regulates cell growth, survival and
differentiation via interlinked signal transduction. Her-2
amplification and overexpression have been reported in 15–30% of
all breast cancer cases and are associated with a poorer prognosis
and more aggressive clinical manifestations (5,6). The
exact mechanism of Her-2 overexpression remains unclear.
The nuclear-associated antigen Ki67 protein may be
detected in the active phases of the cell cycle in late
G1, S, G2 and M phases, but not in the
resting phase (7). The
overexpression of Ki67 corresponds to the high proliferation rate
of tumor cells. Ki67 is used as the main marker to distinguish
between luminal A (Ki67 <14%) and luminal B (Ki67 ≥14%) breast
cancers. Luminal B indicates that the tumor is more aggressive and
requires chemotherapy (8).
Studies have identified that hormones other than
estradiol (E2) may be associated with an increased risk of breast
cancer. High serum prolactin (PRL) levels have been reported in
pre-menopausal females with breast cancer (9) and circulating PRL levels are
positively correlated with the risk of breast cancer (10). Although gene scans have shown that
the expression of luteinizing hormone/choriogonadotropin receptor
(LH/CGR) in breast cancer is either undetectable or very low
(11), studies have identified that
LHCGR may be detected in breast cancer cells (12–14)
and that LH participates in the tumor progression of breast cancer
using LHCGR. Nearly 40% of patients with breast cancer exhibit an
increased human chorionic gonadotropin (hCG)-immunoreactivity in
the serum (15,16). However, few studies have focused on
the association between follicle-stimulating hormone (FSH) and
breast cancer.
FSH stimulates follicle growth and development in
the ovaries and produces the maximum amount of mature spermatozoa
in the testes. FSH and its corresponding receptor (FSHR) have an
important function in various cancers, including prostate (17), endometrial (18) and ovarian (19) cancer. FSH-FSHR induces cancer cell
proliferation, differentiation and metastasis by activating
adenylyl cyclase, thereby resulting in increased cAMP levels
(20,21). The overexpression of FSHR may be
associated with Her-2 overexpression in ovarian cancer (22). Although FSHR expression has not been
identified in primary tissues of breast cancer (23), high FSH levels have been associated
with a significantly poor prognosis in patients with premenopausal
breast cancer (24). FSH has also
been linked to breast cancer cell proliferation and an increased
risk of breast cancer development in females who have undergone
infertility treatments (25).
However, few studies have focused on the association between the
serum level of FSH and the expression status of Her-2 and Ki67.
The present study hypothesized that gonadotropic
hormone has a function in the proliferation of breast cancer cells.
The association between serum hormonal levels and the expression
status of two relative breast cancer proliferation molecular
markers, Her-2 and Ki67, was retrospectively analyzed in 187
post-menopausal females with breast cancer.
Materials and methods
Patients
The data of 187 post-menopausal breast cancer
patients were collected from The Women's Hospital of Zhejiang
University (Zhejiang, China) between January 2007 and October 2012.
The post-menopausal standard was based on the National
Comprehensive Cancer Network Guidelines of 2012. The serum hormonal
levels of FSH, LH, progesterone (P) and PRL were evaluated at the
initial admission of the patients. The patients who were
administered chemotherapy, radiotherapy or hormonal replacement
therapy prior to the surgery were excluded, as the therapies may
have affected their hormonal levels. The study was approved by The
Women's Hospital of Zhejiang University Ethics Committee. Written
informed consent was obtained from the patients.
Determination of circulating levels of
FSH, LH, P and PRL
Venous blood was collected in 6-ml
ethylenediaminetetraacetic acid (EDTA) tubes at 6 a.m. and analyzed
within 24 h. The circulating hormone levels, including those of
FSH, LH, P and PRL, were measured using enzyme immunoassays (Roche
Diagnostics, Mannheim, Germany) on an E170 module.
Evaluation of Her-2 and Ki67 by
immunohistochemistry (IHC)
The tumor grades were assessed using the
tumor-node-metastasis (TNM) staging system. The slides were
re-examined by two expert pathologists to confirm the tumor type,
size and grade and the presence of lymphovascular invasion (LVI).
The classification of Ki67 was determined based on two methods. The
first method divided patients into two groups based on the positive
rates of <14% (IHC, 0 or 1+) or ≥14% (IHC, 2+ or 3+). The second
method divided patients based on the IHC results of 3+ as group 1
and 2+/1+/− as group 2.
Statistical analysis
The statistical analysis was performed using SPSS
19.0 software (SPSS, Inc., Chicago, IL, USA). A Mann-Whitney U test
was performed to determine the association between the hormonal
levels and the expression rates of Her-2 and Ki67. A one-way ANOVA
was performed to evaluate the association between the hormonal
level, LVI and the tumor stage. All of the reported P-values were
two-sided. P<0.05 was considered to indicate a statistically
significant difference.
Results
The clinical and pathological features of the 187
post-menopausal patients with breast cancer are summarized in
Table I. All 187 patients underwent
breast cancer surgery without previous chemotherapy, radiotherapy
or any other hormonal replacement therapy. All patients were
pathologically diagnosed with breast cancer.
 | Table IClinical and pathological features of
patients (n=187). |
Table I
Clinical and pathological features of
patients (n=187).
| Features | Value |
|---|
| Age, years |
| Median | 62 |
| Range | 47–83 |
| FSH, IU/l |
| Mean | 61.83 |
| Range | 8.82–149.6 |
| LH, IU/l |
| Mean | 27.73 |
| Range | 0.1–77.92 |
| P, mmol/l |
| Mean | 0.673 |
| Range | 0.05–2.84 |
| PRL, ng/ml |
| Mean | 11.38 |
| Range | 0.975–61 |
| Her-2, n (%) |
| Positive | 56 (29.9) |
| Negative | 131 (70.1) |
| Ki67, n (%) |
| Method 1 |
| <14% | 89 (47.6) |
| ≥14% | 98 (52.4) |
| Method 2 |
| negative | 14 (7.5) |
| 1+ | 75 (40.1) |
| 2+ | 61 (32.6) |
| 3+ | 37 (19.8) |
| LVI, n (%) |
| Negative | 111 (59.4) |
| ≤3 | 39 (20.9) |
| 4–9 | 26 (13.9) |
| ≥10 | 11 (5.9) |
| Tumor stage, n
(%) |
| 0 | 13 (7.0) |
| I | 25 (13.4) |
| IIa/IIb | 76 (40.6)/31
(16.6) |
| IIIa/IIIb | 25 (13.4)/15
(8.0) |
| IV | 2 (1.1) |
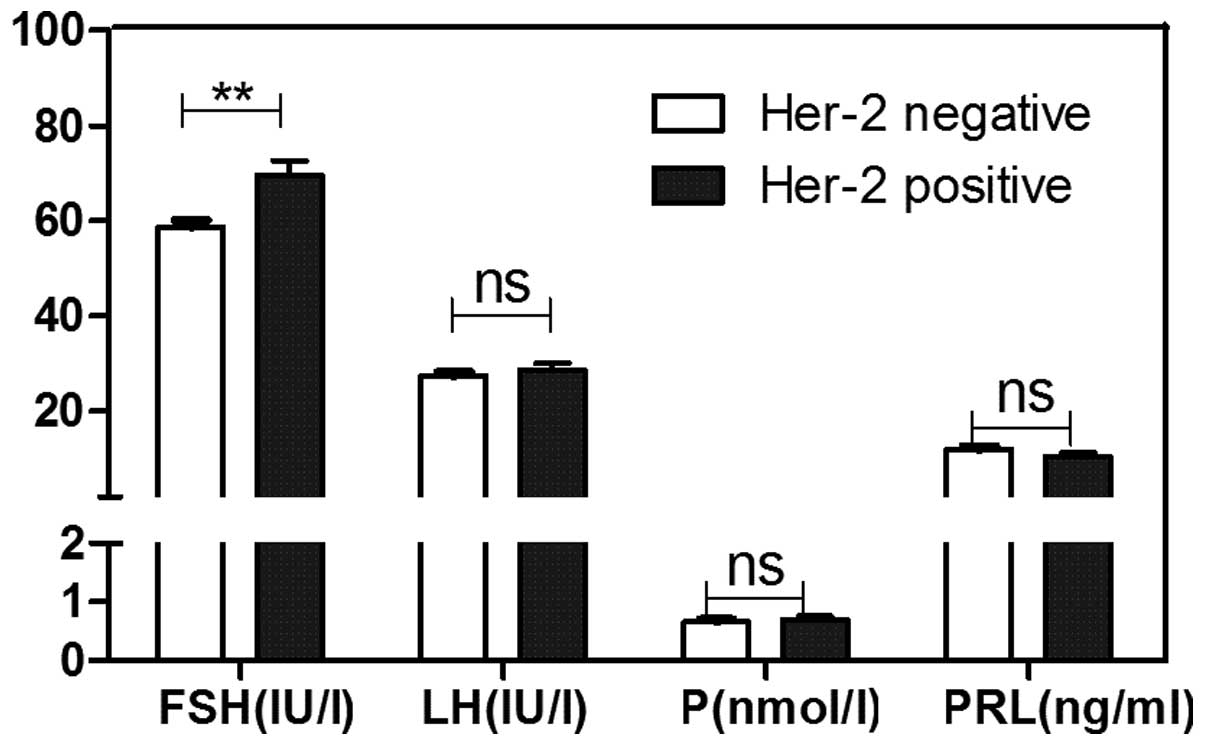
The FSH level was strongly associated with the Her-2
status (P=0.004; Fig. 1). The
Her-2+ patients exhibited higher FSH levels than the
Her-2− patients (69.47±3.219 vs. 58.56±1.516 IU/l). In
contrast, the LH, P and PRL hormone levels were not exhibited with
significant differences between the Her-2+ and
Her-2− patients with post-menopausal breast cancer.
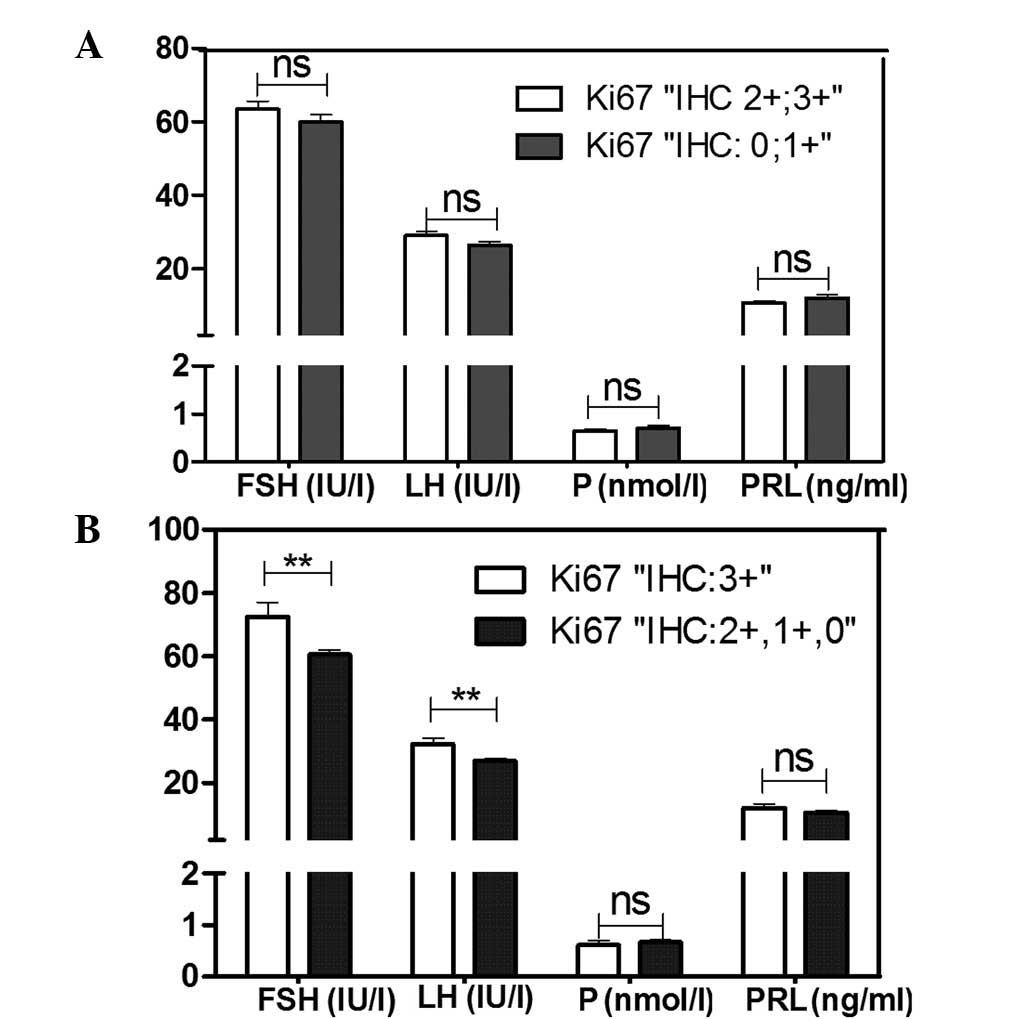
A cut-off point of 14% was selected for Ki67. The
results revealed that FSH, LH, P and PRL were not significantly
different between the two groups (Fig.
2A). In contrast, group 1 exhibited higher FSH (72.51±4.616 vs.
60.53±1.476) and LH (32.33±1.916 vs. 26.98±0.885) levels than group
2 (Fig. 2B).
The FSH, LH, P and PRL levels did not change
significantly in tumor stage groups I–IV compared with stage 0
(Table II). The serum levels of
the hormones were evaluated between the various LVI stage groups,
however, no significant difference was identified in the
circulating FSH, LH, P and PRL levels in the high LVI groups
compared with the LVI-negative group.
 | Table IICorrelation between the serum
hormonal levels of FSH, LH, P and PRL, tumor status and LVI in
post-menopausal patients with breast cancer. |
Table II
Correlation between the serum
hormonal levels of FSH, LH, P and PRL, tumor status and LVI in
post-menopausal patients with breast cancer.
| Tumor stage | LVI |
|---|
|
|
|
|---|
| Hormone | 0 | I | IIa/IIb | IIIa/IIIb | IV | 0 | ≤3 | 4–9 | ≥10 |
|---|
| FSH | | 0.909 | 1.000 | 0.979 | 0.424 | | 0.976 | 0.730 | 0.999 |
| LH | | 1.000 | 0.624 | 0.817 | 0.839 | | 0.646 | 0.997 | 0.994 |
| P | | 0.377 | 0.286 | 0.282 | 0.530 | | 1.000 | 0.561 | 0.988 |
| PRL | | 0.670 | 1.000 | 0.959 | 0.919 | | 0.995 | 0.555 | 0.979 |
Discussion
The effect of hormones on tumorigenesis and tumor
progression, particularly the function of the estrogen signal
pathway in breast cancer, has been widely discussed. However, the
pathogenesis and progression of breast cancer remains unclear.
Furthermore, the specific functions of other hormones, including
FSH and LH, have not been fully elucidated with regard to the
progression of breast cancer. The present study analyzed 187
post-menopausal breast cancer patients to determine whether or not
the serum hormonal levels of FSH, LH, P and PRL were associated
with the expression of two key molecular markers, Ki67 and Her-2.
Premenopausal patients were excluded as their hormonal levels are
affected by their physiological cycle and thus their basic hormonal
level is difficult to determine in the surgery department of the
hospital. The serum FSH levels differed between the
Her-2+ and Her-2− patients, and higher FSH
levels were identified in the Her-2+ patients. A higher
serum FSH level was also identified in patients with high Ki67
expression (IHC, 3+). The serum LH level exhibited no significant
difference based on Her-2 expression, but a higher serum LH level
was observed in the patients with a high Ki67 (IHC, 3+).
FSH and LH belong to a family of glycoprotein
hormones, which also include placental hCG and thyroid-stimulating
hormone (TSH). FSH and LH are key regulators of reproductive
function in the endocrine system and regulate steroidogenesis and
gametogenesis in the ovary and the testis. FSH stimulates
follicular cell activity through FSHR. FSHR expression is
restricted to the sterol cells in the testis and the granulose
cells in the ovary (26,27). FSHR expression has been identified
in cancer cells. However, the exact function of gonadotropin and
its molecular mechanism in the formation and development of tumors
has not yet been fully characterized.
The FSH and LH receptors belong to the super family
of G protein-coupled receptors (GPCRs). However, these hormones are
unique as they have a large ectodomains that contain a leucine-rich
repeat, which is significant for ligand binding. FSHR expression
has been identified in various cancer cells, but rarely in breast
cancer tissues or cell lines. However, numerous leucine-rich GPCRs
(LGRs) have been identified in the human genome (28). In addition to FSHR, other LGR
subgroups are able to transmit signals from gonadotropins (28,29).
The expression of leucine-containing GPCRs should be detected in
breast cancer as FSH is widely distributed in the cytoplasm of
epithelial cells in breast cancer, in which higher levels of FSH
are observed in benign mammary tumors and breast cancer compared
with normal cells (30). Further
studies are required to determine whether or not FSH stimulates
Her-2 expression and cell proliferation by the LGR subgroup. FSH
may function in the malignant transformation of breast cancer via a
specific receptor, but not the traditional FSHR.
Furthermore, the menopause affects Her-2 expression
in breast cancer (31). One study
focused on FSH and Her-2 in breast cancer (32), while certain studies have revealed
that FSH stimulates Her-2 expression via specific signaling
pathways, including cAMP, in ovarian cancer (22,33,34).
In the present study, patients with high Ki67 expression (IHC, 3+)
exhibited higher serum FSH and LH levels. A total of 10 ng/ml FSH
was able to upregulate the expression of Her-2 and Ki67 at the
transcriptional level in 24 h in a breast cancer cell line in
vitro (data not shown). Thus, gonadotropins are able to
directly or indirectly promote cell proliferation in breast
cancer.
To determine whether or not FSH is an independent
prognostic marker, the association between FSH or LH and the
overall survival (OS) or relapse-free survival (RFS) of the
patients was evaluated in the present study. However, the data in
this study was acquired from patients who were diagnosed with
breast cancer within the past 5 years. Thus, OS/RFS could not be
sufficiently evaluated in the study. Future studies with regard to
this topic are required.
In conclusion, in the present cases of
post-menopausal breast cancer, the Her-2+ patients were
observed to have a higher serum FSH level than the
Her-2− patients. The patients with high Ki67 expression
(IHC, 3+) exhibited higher serum FSH and LH levels. In
addition to E2, FSH and LH may have significant functions in breast
cancer progression. Thus, further studies are required to determine
the exact mechanism at the molecular level.
Acknowledgements
This study was supported by the National Natural
Science Foundation of China (grant nos. 30973465 and 81071879).
References
|
1
|
Siegel R, Naishadham D and Jemal A: Cancer
statistics, 2012. CA Cancer J Clin. 62:10–29. 2012. View Article : Google Scholar
|
|
2
|
Yang W and Guan L: Bridging the US and
China together to conquer cancer: report of the 4th annual meeting
of the US Chinese Anti-Cancer Association (USCACA). Chin J Cancer.
31:315–318. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yang L, Parkin DM, Ferlay J, Li L and Chen
Y: Estimates of cancer incidence in China for 2000 and projections
for 2005. Cancer Epidemiol Biomarkers Prev. 14:243–250.
2005.PubMed/NCBI
|
|
4
|
Zheng S, Bai JQ, Li J, et al: The
pathologic characteristics of breast cancer in China and its shift
during 1999–2008: A national-wide multicenter cross-sectional image
over 10 years. Int J Cancer. 131:2622–2631. 2012.PubMed/NCBI
|
|
5
|
Slamon DJ, Godolphin W, Jones LA, et al:
Studies of the HER-2/neu proto-oncogene in human breast and ovarian
cancer. Science. 244:707–712. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ross JS, Slodkowska EA, Symmans WF,
Pusztai L, Ravdin PM and Hortobagyi GN: The HER-2 receptor and
breast cancer: ten years of targeted anti-HER-2 therapy and
personalized medicine. Oncologist. 14:320–368. 2009.PubMed/NCBI
|
|
7
|
Lopez F, Belloc F, Lacombe F, et al:
Modalities of synthesis of Ki67 antigen during the stimulation of
lymphocytes. Cytometry. 12:42–49. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Goldhirsch A, Wood WC, Coates AS, et al:
Strategies for subtypes - dealing with the diversity of breast
cancer: highlights of the St. Gallen International Expert Consensus
on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol.
22:1736–1747. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Eliassen AH, Tworoger SS and Hankinson SE:
Reproductive factors and family history of breast cancer in
relation to plasma prolactin levels in premenopausal and
postmenopausal women. Int J Cancer. 120:1536–1541. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tworoger SS and Hankinson SE: Prolactin
and breast cancer risk. Cancer Lett. 243:160–169. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kuijper TM, Ruigrok-Ritstier K,
Verhoef-Post M, et al: LH receptor gene expression is essentially
absent in breast tumor tissue: implications for treatment. Mol Cell
Endocrinol. 302:58–64. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bodek G, Rahman NA, Zaleska M, et al: A
novel approach of targeted ablation of mammary carcinoma cells
through luteinizing hormone receptors using Hecate-CGbeta
conjugate. Breast Cancer Res Treat. 79:1–10. 2003. View Article : Google Scholar
|
|
13
|
Meduri G, Charnaux N, Loosfelt H, et al:
Luteinizing hormone/human chorionic gonadotropin receptors in
breast cancer. Cancer Res. 57:857–864. 1997.PubMed/NCBI
|
|
14
|
Meduri G, Charnaux N, Spyratos F, Hacene
K, Loosfelt H and Milgrom E: Luteinizing hormone receptor status
and clinical, pathologic, and prognostic features in patients with
breast carcinomas. Cancer. 97:1810–1816. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Caffier H and Brandau H: Serum tumor
markers in metastatic breast cancer and course of disease. Cancer
Detect Prev. 6:451–457. 1983.PubMed/NCBI
|
|
16
|
Tsalacopoulos G and Bloch B: Ectopic
production of the beta subunit of human chorionic gonadotrophin by
malignant ovarian neoplasms. S Afr Med J. 62:487–488.
1982.PubMed/NCBI
|
|
17
|
Ben-Josef E, Yang SY, Ji TH, et al:
Hormone-refractory prostate cancer cells express functional
follicle-stimulating hormone receptor (FSHR). J Urol. 161:970–976.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Davies S, Bax CM, Chatzaki E, Chard T and
Iles RK: Regulation of endometrial cancer cell growth by
luteinizing hormone (LH) and follicle stimulating hormone (FSH). Br
J Cancer. 83:1730–1734. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Chen FC, Oskay-Ozcelik G, Bühling KJ, et
al: Prognostic value of serum and ascites levels of estradiol, FSH,
LH and prolactin in ovarian cancer. Anticancer Res. 29:1575–1578.
2009.PubMed/NCBI
|
|
20
|
Wayne CM, Fan HY, Cheng X and Richards JS:
Follicle-stimulating hormone induces multiple signaling cascades:
evidence that activation of Rous sarcoma oncogene, RAS, and the
epidermal growth factor receptor are critical for granulosa cell
differentiation. Mol Endocrinol. 21:1940–1957. 2007. View Article : Google Scholar
|
|
21
|
Hunzicker-Dunn M and Maizels ET: FSH
signaling pathways in immature granulosa cells that regulate target
gene expression: branching out from protein kinase A. Cell Signal.
18:1351–1359. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Choi JH, Choi KC, Auersperg N and Leung
PC: Overexpression of follicle-stimulating hormone receptor
activates oncogenic pathways in preneoplastic ovarian surface
epithelial cells. J Clin Endocrinol Metab. 89:5508–5516. 2004.
View Article : Google Scholar
|
|
23
|
Huhtaniemi I: Are gonadotrophins
tumorigenic - a critical review of clinical and experimental data.
Mol Cell Endocrinol. 329:56–61. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Pujol P, Daures JP, Brouillet JP, et al: A
prospective prognostic study of the hormonal milieu at the time of
surgery in premenopausal breast carcinoma. Cancer. 91:1854–1861.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zreik TG, Mazloom A, Chen Y, et al:
Fertility drugs and the risk of breast cancer: a meta-analysis and
review. Breast Cancer Res Treat. 124:13–26. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sprengel R, Braun T, Nikolics K, Segaloff
DL and Seeburg PH: The testicular receptor for follicle stimulating
hormone: structure and functional expression of cloned cDNA. Mol
Endocrinol. 4:525–530. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kelton CA, Cheng SV, Nugent NP, et al: The
cloning of the human follicle stimulating hormone receptor and its
expression in COS-7, CHO, and Y-1 cells. Mol Cell Endocrinol.
89:141–151. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Van Loy T, Vandersmissen HP, Van Hiel MB,
et al: Comparative genomics of leucine-rich repeats containing G
protein-coupled receptors and their ligands. Gen Comp Endocrinol.
155:14–21. 2008.PubMed/NCBI
|
|
29
|
Hsu SY, Kudo M, Chen T, et al: The three
subfamilies of leucine-rich repeat-containing G protein-coupled
receptors (LGR): identification of LGR6 and LGR7 and the signaling
mechanism for LGR7. Mol Endocrinol. 14:1257–1271. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Garde SV, Sheth AR, Joseph R, Panchal CJ,
Chinoy RF and Sheth NA: Occurrence and de novo biosynthesis of
follicle stimulating hormone (FSH) in benign and malignant
conditions of human breast. Cancer Lett. 75:1–9. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Wang N, Wang B, Wang Y and Hu J: Estrogen
receptor positive operable breast cancer: does menopausal status
impact on HER2 and progesterone receptor status? Breast.
20:519–524. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Hernández L, Nuñez-Villarl MJ,
Martínez-Arribas F, Pollán M and Schneider J: Circulating hormone
levels in breast cancer patients. Correlation with serum tumor
markers and the clinical and biological features of the tumors.
Anticancer Res. 25:451–454. 2005.PubMed/NCBI
|
|
33
|
Choi JH, Chen CL, Poon SL, Wang HS and
Leung PC: Gonadotropin-stimulated epidermal growth factor receptor
expression in human ovarian surface epithelial cells: involvement
of cyclic AMP-dependent exchange protein activated by cAMP pathway.
Endocr Relat Cancer. 16:179–188. 2009. View Article : Google Scholar
|
|
34
|
Zhang Z, Jia L, Feng Y and Zheng W:
Overexpression of follicle-stimulating hormone receptor facilitates
the development of ovarian epithelial cancer. Cancer Lett.
278:56–64. 2009. View Article : Google Scholar : PubMed/NCBI
|