Introduction
Granulocytic sarcoma (GS) is a solid tumor
containing myeloid leukemia cells that appears in a variety of
locations, including the central nervous system, bone and soft
tissue. To the best of our knowledge, GS invading the breast is
rare (1) and may present at the
onset of acute myeloid leukemia (AML) or extramedullary relapse
following bone marrow transplantation. No characteristic
appearances of GS of the breast have been identified by radiography
or ultrasonography. In addition to its rarity, GS of the breast is
easy to misdiagnose as other benign tumors, lymphoma or sarcoma.
Currently, the only method to confirm the diagnosis of GS of the
breast is by pathological examination combined with
immunohistochemistry. Doctors must take GS of the breast into
consideration when the diagnosis is confusing. The standard
therapeutic approach for GS of the breast remains undefined;
therefore, doctors face a dilemma in making a clinical decision.
The current report presents two cases of GS of the breast and a
review of the literature. This study was approved by the Ethics
Committee of Jinhua Central Hospital and was performed according to
the Declaration of Helsinki. Written informed consent was obtained
from each patient’s family.
Case reports
Case 1
A 59-year-old female presented on June 25, 2008,
with a painless mass in the left breast that had been present for
one week and a fever with a temperature of 37.0–37.7ºC. The patient
exhibited no other symptoms or relevant past or family histories. A
physical examination revealed a mobile mass in the left breast
measuring 1.8×1.2 cm, with no palpable auxiliary lymph nodes.
Ultrasound revealed a solid and hypoechoic mass
measuring 1.7×0.9 cm, which had a clear boundary with hypervascular
flow, and the mammography showed an equidensity mass with no areas
of calcification. The chest radiography revealed no abnormal
observations, and abdominal ultrasound revealed no suspected
lesions in the liver or spleen. The complete blood count showed a
white blood cell (WBC) count of 2.9×109/l, a neutrocyte
count of 0.2×109/l, hemoglobin levels of 109 g/l and a
platelet (PLT) count of 104×109/l.
Since the mass in the patient’s breast was
considered to be a benign tumor, a lumpectomy had to be performed
under local infiltration anesthesia. The patient underwent the
lumpectomy on June 10, 2008, despite a relatively low WBC count.
According to the frozen section, the patient was diagnosed with
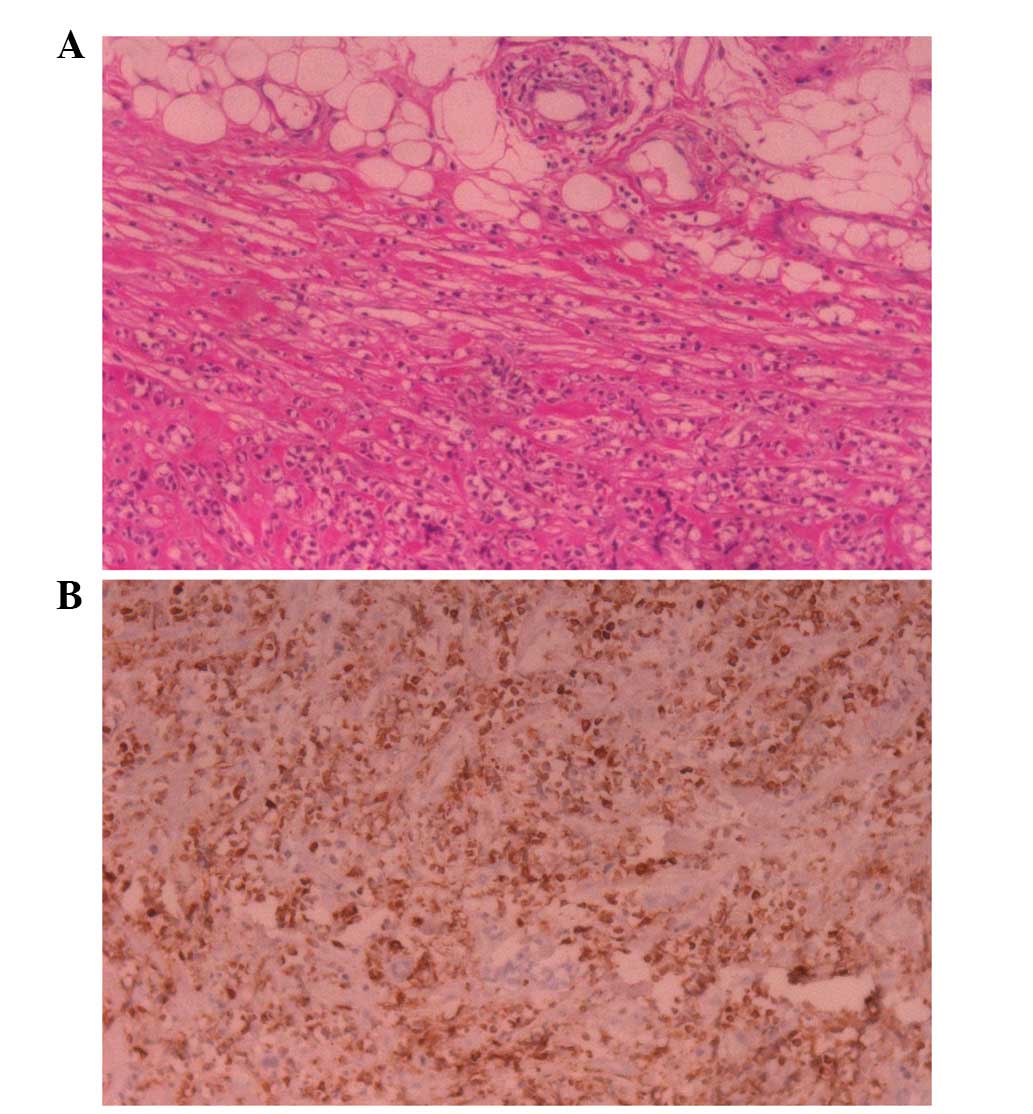
breast mucosa-associated B-cell lymphoma. Post-operative pathology
revealed that the nuclei of the tumor cells were evidently
different in size and shape and scattered among the massive fibrous
tissue. At the edge of the tumor, the tumor cells exhibited a
streamline alignment (Fig. 1A) and
mitotic figures were easily identified. The immunohistochemical
analysis showed that markers of myeloperoxidase (MPO) and CD45RA
were positive and those for carcinoembryonic antigen (CEA), L26 and
CD3 were negative, while CD45RO was weakly positive (Fig. 1B). The patient was confirmed with
AML-M4E0 by bone marrow aspiration, and the final diagnosis was GS
of the breast.
The patient received inducted chemotherapy with the
MA regimen (i.v. injection of 6 mg/m2 mitoxantrone days
1–3 plus i.v. injection of 100 mg/m2 cytarabine day 1–3,
every 3 weeks) and achieved complete remission. The patient
subsequently received consolidation chemotherapy. To date, the
patient has received follow-up for 4 years and no relapse has
occurred.
Case 2
A 37-year-old female was diagnosed with AML-M6 by
bone marrow aspiration and biopsy in April, 2004. The patient
achieved complete remission following inducted chemotherapy with
retinoic acid (45 mg/m2, days 1–28). Following a total
of 8 cycles of consolidation chemotherapy with the MA regimen, the
patient underwent allogeneic bone marrow transplantation in
January, 2006.
In November 2006, the patient was admitted to the
Department of Oncology (Jinhua Central Hospital, Jinhua, China) due
to a painless palpable mass in the left breast that had been
present for 10 days. The patient exhibited no other symptoms and
had no relevant previous or family histories. A physical
examination revealed a mass measuring 2.0×1.5 cm in the lower inner
quadrant of the left breast. Ultrasound revealed a solid and
hypoechoic mass, and fine-needle aspiration (FNA) identified the
mass as a fibroma. No suspicious lesions were located in the
patient’s lungs by chest radiography or in the liver by
ultrasound.
The complete blood count showed a WBC count of
2.9×109/l with 53.4% neutrocytes, a red blood cell count
of 1.94×1012/l with 72.0% HCT and a PLT count of
27×109/l. Since the mass was diagnosed as a benign tumor
by FNA, the patient underwent a lumpectomy under local infiltration
anesthesia, despite having a low PLT count. The tumor was removed
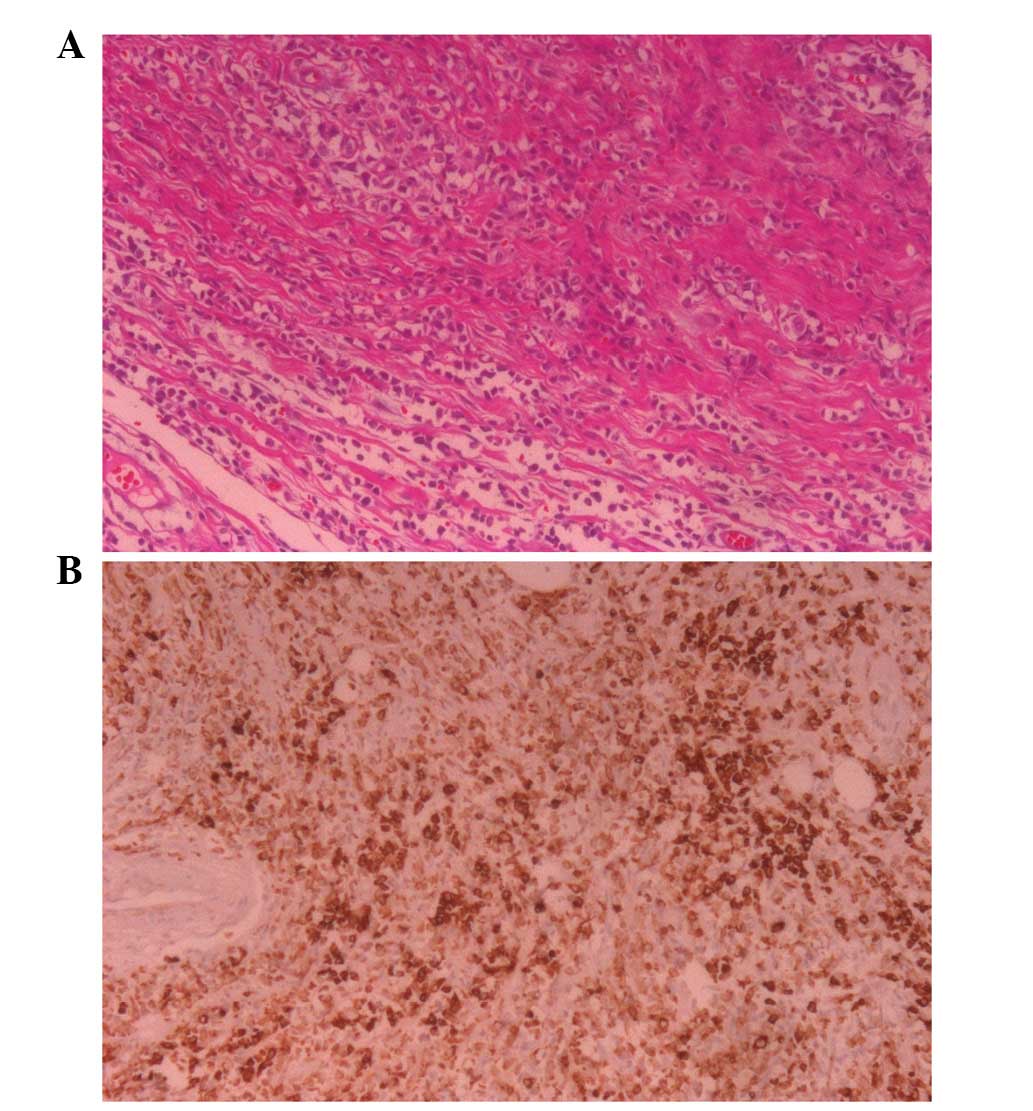
in November, 2006, and the pathological results revealed that the
structure of the breast, which had been invaded by middle-sized
diffuse lymphoid cells and fat tissue, was destroyed (Fig. 2A). Immunohistochemical analysis
revealed that the markers of MPO and LCA were positive and that
those for CD68, CD79a and L26 were negative (Fig. 2B). Following confirmation by
histopathology, the patient was diagnosed with GS of the breast.
The tests for liver function, performed in February, 2007,
demonstrated that the levels for alanine aminotranferase, aspartate
aminotransferase, total bilirubin, direct bilirubin and
r-glutamyltransfarase were 97 IU/l, 186 IU/l, 90.7 μmol/l, 40.8
μmol/l and 1,064 U/l, respectively, with normal reference values of
0–40 IU/l, 0–40 IU/l, 2–25 μmol/l, 0–8 μmol/l and 0–50 U/l,
respectively. The level of the immunoglobulin IgG protein subtype
was 4,240 mg/ml (normal reference value, 723–1,685 mg/ml). The
patient was diagnosed with graft-versus-host-disease (GVHD) and
received immunosuppression therapy to protect the liver. However,
the effect of the treatment was unsatisfactory and the patient
succumbed to fungal pneumonia in June, 2007, without having
received systemic chemotherapy or a second bone marrow
transplantation. The relapse of the GS in the patient’s breasts was
not identified prior to mortality.
Discussion
The prevalence rate of GS is ~8% of all AML cases
(1). GS may occur simultaneously
with leukemia or as the initial symptom of recurrence following
bone marrow transplantation in patients with AML. The mechanism of
GS remains undefined and no definite associations between GS and
bone marrow transplantation have been identified. The
French-American-British classification subtypes of AML, M4 and M5,
and a high WBC count may be predictors of GS (2). However, in the current report, case 1
was diagnosed with M4 and case 2 was diagnosed with M6, and a high
WBC count was not identified in either case, while a low WBC count
was identified in case 1. The results are inconsistent with the
literature (2) and therefore,
further study is required to detect predictors of GS. The mechanism
of extramedullary relapse following allogeneic bone marrow
transplantation remains unclear. There have been numerous cases of
extramedullary relapse and normal donor cells in the bone marrow
and it is possible that extramedullary relapse results from the
graft-versus-leukemia (GVL) effect (3,4). The
graft induces the remaining leukemia stem cells in the marrow to
release into extramedullary sites. The patient in case 2 was
diagnosed with GVHD, and a previous study demonstrated that GVHD
and GVL have the same mechanism (5). However, no reports have analyzed the
correlation between GVHD and the extramedullary relapse of AML.
For patients with GS of the breast, the isolated
nodule, multiple nodules or mass may be observed in the unilateral
or bilateral breasts of patients of any age, even with a diffuse
lesion. Patients do not present specific signs, including nipple
inversion or discharge (6) and do
not have a family history of breast cancer. The two cases in this
report presented with unilateral isolated nodules. The ultrasound
observations for GS of the breast are absent of characteristic
appearances and often present as a hypoechoic and well-defined
mass, with color flow imaging and without areas of calcification
(7). Few case reports have
previously described the mammographic appearance of GS of the
breast (8,9). GS has been commonly described as a
non-calcified mass in the breast. In case 1, the mammogram also
presented a non-calcified, irregular mass, consistent with studies
in the literature (10). The
absence of characteristics in the imaging for GS results in the
difficulty of differentiating GS from other breast diseases.
Therefore, pathological analysis is necessary in order to confirm
the diagnosis of GS. However, without sufficient preparation, due
to the rarity of GS of the breast, the condition is usually
misdiagnosed as a benign tumor or primary carcinoma of the breast
by FNA, as was evident in the two cases of the current study. A
biopsy is the only method to confirm the final diagnosis of GS,
however, hematoxylin and eosin (H&E) staining may reveal
various morphological changes, resulting in the common misdiagnosis
of GS as lymphoma or sarcoma (9).
H&E staining may reveal tumor cells that vary in size and with
evident nuclear atypia (11). At
the edge of the tumor, the vast mesenchymal tissue compresses the
tumor cells into a streamline alignment. The immunohistochemical
detection of MPO-positive cells is useful in order to confirm the
final diagnosis, and primary breast carcinoma may be ruled out by
the detection of cytokeratin-negative cells. B cell and T cell
markers may be useful as further indicators for ruling out the
diagnosis of lymphoma. By combining the history of AML with
observations made in a bone marrow aspiration or biopsy, GS of the
breast may be confirmed.
The therapeutic approaches for GS of the breast
remain unconfirmed and there have been controversial opinions with
regard to the local treatment of the breast. Mastectomy or
lumpectomy with or without radiotherapy may be acceptable as
treatments, and radiotherapy has been recommended in specific
previous studies, however, the role of surgery remains unclear
(12). The two cases presented in
the current report were treated with lumpectomy alone and the
results of local recurrence in the breast were satisfactory, as no
relapse was identified in either of the patients. A lumpectomy may
be an alternative treatment to consider for breast masses in such
patients. When considering systemic therapy, untreated patients
must receive bone marrow transplantation following induced
chemotherapy, and patients with extramedullary relapse without bone
marrow relapse may undergo strict observation without aggressive
systemic treatment. However, when bone marrow relapse occurs,
patients must receive systemic chemotherapy and/or a second bone
marrow transplantation (9). Case 2
of the current report was diagnosed with GVHD and presented with GS
of the breast as the initial symptom following allogeneic bone
marrow transplantation. This case is the first such case to be
reported and therefore, there were no successful treatments to
refer to. Patients diagnosed with extramedullary relapse
concomitant with GVHD commonly exhibit liver and renal dysfunction,
which reduces the chance of receiving aggressive chemotherapies or
a second bone transplantation.
The prevalence of GS of the breast in AML is rare,
and a lumpectomy may achieve satisfactory local control and be an
alternative treatment for solitary unilateral nodules in the
breast.
References
|
1
|
Liu PI, Ishimaru T, McGregor DH, Okada H
and Steer A: Autopsy study of granulocytic sarcoma (chloroma) in
patients with myelogenous leukemia, Hiroshima-Nagasaki 1949–1969.
Cancer. 31:948–955. 1973.PubMed/NCBI
|
|
2
|
Byrd JC, Edenfield WJ, Shields DJ and
Dawson NA: Extramedullary myeloid cell tumors in acute
nonlymphocytic leukemia: a clinical review. J Clin Oncol.
13:1800–1816. 1995.PubMed/NCBI
|
|
3
|
Firas AS, Demeckova E, Bojtarova E, Czako
B, Hrubisko M and Mistrik M: Isolated extra-medullary relapse of
acute leukemia following allogeneic bone marrow transplantation.
Bratisl Lek Listy. 109:358–361. 2008.
|
|
4
|
Karbasian-Esfahani M, Wiernik PH, Yeddu M
and Abebe L: Leukemic infiltration of the breast in acute
lymphocytic leukemia (ALL). Hematology. 13:101–106. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Koca E, Goker H, Guven GS, et al: Unusual
extramedullary recurrences and breast relapse despite hepatic GVHD
after allografting in Ph+-ALL. Hematology. 11:105–107.
2006.PubMed/NCBI
|
|
6
|
Thachil J, Richards RM and Copeland G:
Granulocytic sarcoma - a rare presentation of a breast lump. Ann R
Coll Surg Engl. 89:W7–W9. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang WT, Muttarak M and Ho LW: Nonmammary
malignancies of the breast: ultrasound, CT, and MRI. Semin
Ultrasound CT MR. 21:375–394. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Khoury NJ, Hanna Al-Kass FM, Jaafar HN,
Taher AT and Shamseddine AI: Bilateral breast involvement in acute
myelogenous leukemia. Eur Radiol. 10:10312000. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shea B, Reddy V, Abbitt P, Benda R,
Douglas V and Wingard J: Granulocytic sarcoma (chloroma) of the
breast: a diagnostic dilemma and review of the literature. Breast
J. 10:48–53. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pettinato G, De Chiara A, Insabato L and
De Renzo A: Fine needle aspiration biopsy of a granulocytic sarcoma
(chloroma) of the breast. Acta Cytol. 32:67–71. 1988.PubMed/NCBI
|
|
11
|
Traweek ST, Arber DA, Rappaport H and
Brynes RK: Extramedullary myeloid cell tumors. An
immunohistochemical and morphologic study of 28 cases. Am J Surg
Pathol. 17:1011–1019. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mandal S, Jain S and Khurana N: Breast
lump as an initial manifestation in acute lymphoblastic leukemia:
an unusual presentation. A case report. Hematology. 12:45–47. 2007.
View Article : Google Scholar
|