Introduction
Mucosa-associated lymphoid tissue (MALT)-lymphoma is
a distinctive subtype of non-Hodgkin lymphoma, whose concept was
first put forward by British pathologists, Isaacson and Wright
(1). MALT-lymphoma frequently
occurs in the gastrointestinal tract and rarely occurs in the
salivary gland. The condition is difficult to diagnose using
imaging. Studies have previously reported the imaging features of
gastric and pulmonary MALT-lymphoma (2,3).
However, imaging studies of MALT-lymphomas of the parotid gland
have not yet been published. The present study reviewed and
analyzed the clinical, computed tomography (CT) imaging and
pathological features of eight cases of pathologically confirmed
MALT-lymphomas of the parotid gland in order to improve the imaging
and clinical diagnosis.
Case report
Clinical data
A total of eight patients, one male and 7 females,
with pathologically confirmed MALT-lymphomas were analyzed between
January 2005 and November 2011. The age range of the patients was
14–80 years, with a median age of 52 years and a mean age of 50.9
years. Written informed consent was obtained from the patients.
Methods
All the patients underwent spiral multidetector CT
(MDCT) plain and enhancement scans of the parotid gland using the
GE Lightspeed 16-row MDCT machine (GE Healthcare, Fairfield, CT,
USA). The plain scan covered the area between the hyoid bone and
the base of the skull using the following parameters: Column
voltage, 120 KV; column electric current, 240–260 mAs; slice
thickness, 2.5 mm; interval 0; and matrix, 512×512. A high-pressure
syringe was used to inject 300 mg/ml Ultravist (Shanghai Boyier
Chemical Co., Ltd., Shanghai, China) into the anterior middle vein
of the elbow at a dosage of 50 ml and with an injecting speed of
3.5 ml/sec. A dual-phase scan was also performed. The arterial
phase of the scan began at 25 sec and the venous phase at 75 sec
into the scan. The slice thickness was 2.5 mm, with a 512×512
matrix. A standard algorithm was adopted for the reconstruction.
Follow-up examinations were performed in all eight cases.
Immunohistochemistry
Deparaffinized sections of patient tissue samples
were washed with phosphate-buffered saline (PBS) three times for 5
min each. In order to block the endogenous peroxidase activity, the
sections were dipped in PBS that contained 3%
H2O2 for 10 min, then were immersed with 10%
sheep serum for 30 min and incubated overnight with the specific
antibodies, anti-CD3, CD5, CD19, CD20, CD43 and CD79a (Abcam,
Cambridge, UK). The sections were washed and stained according to
the manufacturer’s instructions.
Imaging data
All the CT images of the patients were analyzed by
two experienced radiologists in the Picture Archiving and
Communication System diagnostic terminal of the Shanghai Daijia
corporation (Shanghai, China) in order to assess the pathological
position, number, morphology, edge, size, density and dual-phase
enhancement features of the lymphomas. Various outcomes were agreed
upon following negotiation. The size was determined by measuring
the two largest diameters of the tumor and adopting the mean value.
The plain CT scan values were measured and the CT enhancement
features were assessed to see whether the enhancement was uniform
and to analyze the increased value of the dual-phase enhancement CT
compared with the plain scan. The CT value was from the target area
of tumor parenchyma ~2 mm in diameter. This was measured three
times and the mean value was calculated.
Clinical data
As shown in Table I,
all the patients presented with painless nodules in the parotid
gland and the course of the disease varied between 20 days and six
years. Of the total cases, seven included symptoms of a dry mouth
and dry eyes, which is similar to the symptoms of Sjögre’s
syndrome. The patients from cases 1 and 3 felt slight pain when the
affected area was palpated and case 4 demonstrated symptoms of
facial nerve involvement. The nodule of case 2 had invaded into the
deep lobe of the parotid gland and linked with the
sternocleidomastoid muscles, and the nodule of case 6 was located
in the lower pole of the parotid gland, with a lymphoid node ~1.5
cm in diameter. The nodules of cases 3–7 were located in the
superficial lobe of the parotid gland and were not well-defined
within the parotid gland tissues. The nodule of case 7 was adhesive
to the facial nerve. Inflammatory changes were observed around the
nodule in one case. All the patients underwent a lump resection and
partial parotidectomy. A total of five patients (cases 1, 2, 4, 5
and 8) were administered post-operative chemotherapy. The follow-up
period ranged between 4 and 48 months. The lymphomas of cases 3 and
8 recurred, but no patients succumbed to their diseases.
 | Table IClinical characteristics in eight
cases. |
Table I
Clinical characteristics in eight
cases.
| Case | Gender | Age, years | Sjögre’s
syndrome | Facial nerve
involvement | Range of motion | Malignant neck lymph
nodes | Treatment | Recurrence | Follow-up time,
months |
|---|
| 1 | F | 62 | Y | Y | Poor | N | Surgery and
chemoradiotherapy | N | 48 |
| 2 | M | 14 | Y | N | Poor | N | Surgery and
chemoradiotherapy | N | 24 |
| 3 | M | 80 | Y | N | Good | Y | Surgery | Y | 14 |
| 4 | M | 58 | Y | N | Good | N | Surgery and
chemoradiotherapy | N | 14 |
| 5 | M | 46 | N | N | Good | N | Surgery and
chemoradiotherapy | N | 19 |
| 6 | M | 38 | Y | N | Medium | N | Surgery | N | 19 |
| 7 | M | 68 | Y | N | Medium | N | Surgery | N | 4 |
| 8 | M | 42 | Y | N | Medium | N | Surgery and
chemoradiotherapy | Y | 9 |
Pathological manifestation
The gross appearance of five of the tumor samples
was solid and three were cystic. Cases 5–7 were light yellow in
color, cases 1–3 were yellow and cases 4 and 8 were brown. The
paraffin slice of case 4 displayed high hyperplasia of the
lymphocytes and was identified in the right parotid gland. The
lymphoma and partial small glands were broken by mononuclear B
cells, and the patient was consequently diagnosed with
MALT-lymphoma. Case 8 was diagnosed with MALT-lymphoma by combining
tissue imaging with immunohistochemistry. Case 5 was diagnosed with
bilateral lymphocytic mumps and MALT-lymphoma. Case 6 was diagnosed
with benign lymphoepithelial lesions of the right parotid gland and
MALT-lymphoma. Case 7 was diagnosed with benign lymphoepithelial
lesions of the left parotid gland and lymphoid node reactive
hyperplasia; a diagnosis of MALT-lymphoma was made through a
consultation with the Peking Union Medical University following the
recurrence of the disease. Cases 1–3 were diagnosed with
MALT-lymphoma only. All the patients underwent immunohistochemical
examinations (Table II).
 | Table IIImmunohistochemistry in eight
cases. |
Table II
Immunohistochemistry in eight
cases.
| |
Immunohistochemistry |
|---|
| |
|
|---|
| Case | Tumor pathological
type | CD3 | CD5 | CD10 | CD20 | CD43 | CD79a |
|---|
| 1 | MALT-L | − | − | − | + | − | + |
| 2 | MALT-L | − | − | − | + | − | + |
| 3 | MALT-L | − | − | − | ++ | − | + |
| 4 | MALT-L | −/+ | − | − | + | − | + |
| 5 | Lymphoblastic
parotitis with MALT-L | − | − | − | + | − | + |
| 6 | Benign
lymphoepithelial lesion with MALT-L | − | − | − | + | + | + |
| 7 | Parotid MALT-L | + | + | − | + | − | + |
| 8 | MALT-L | + | + | − | ++ | + | + |
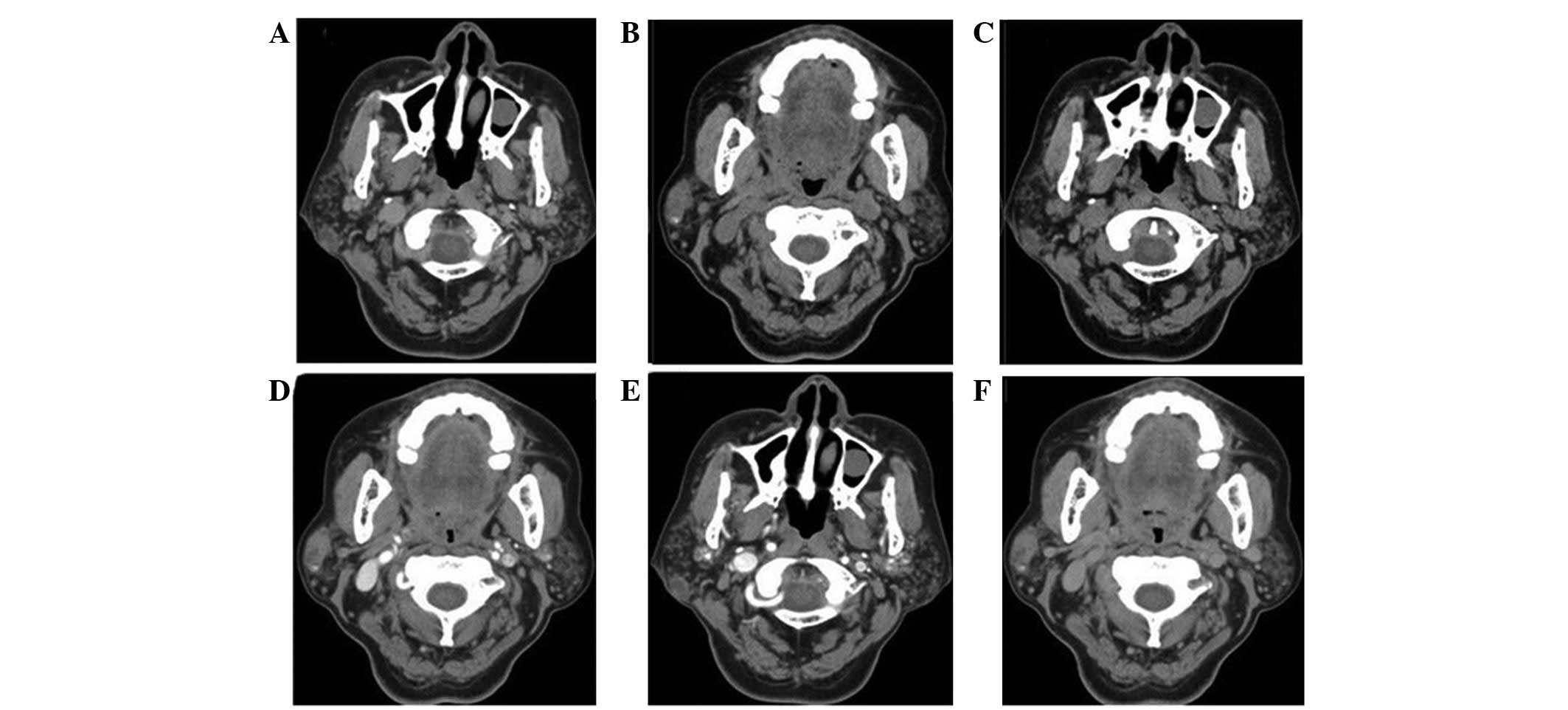
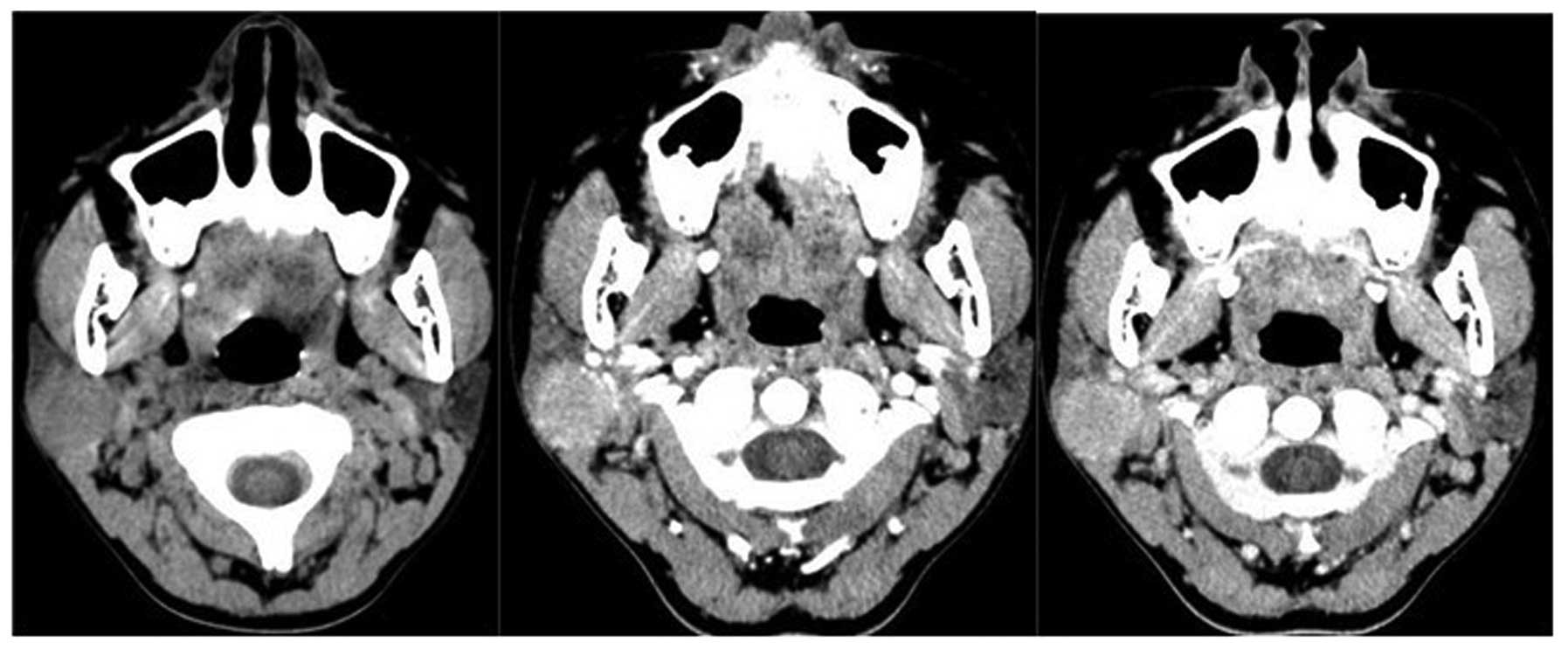
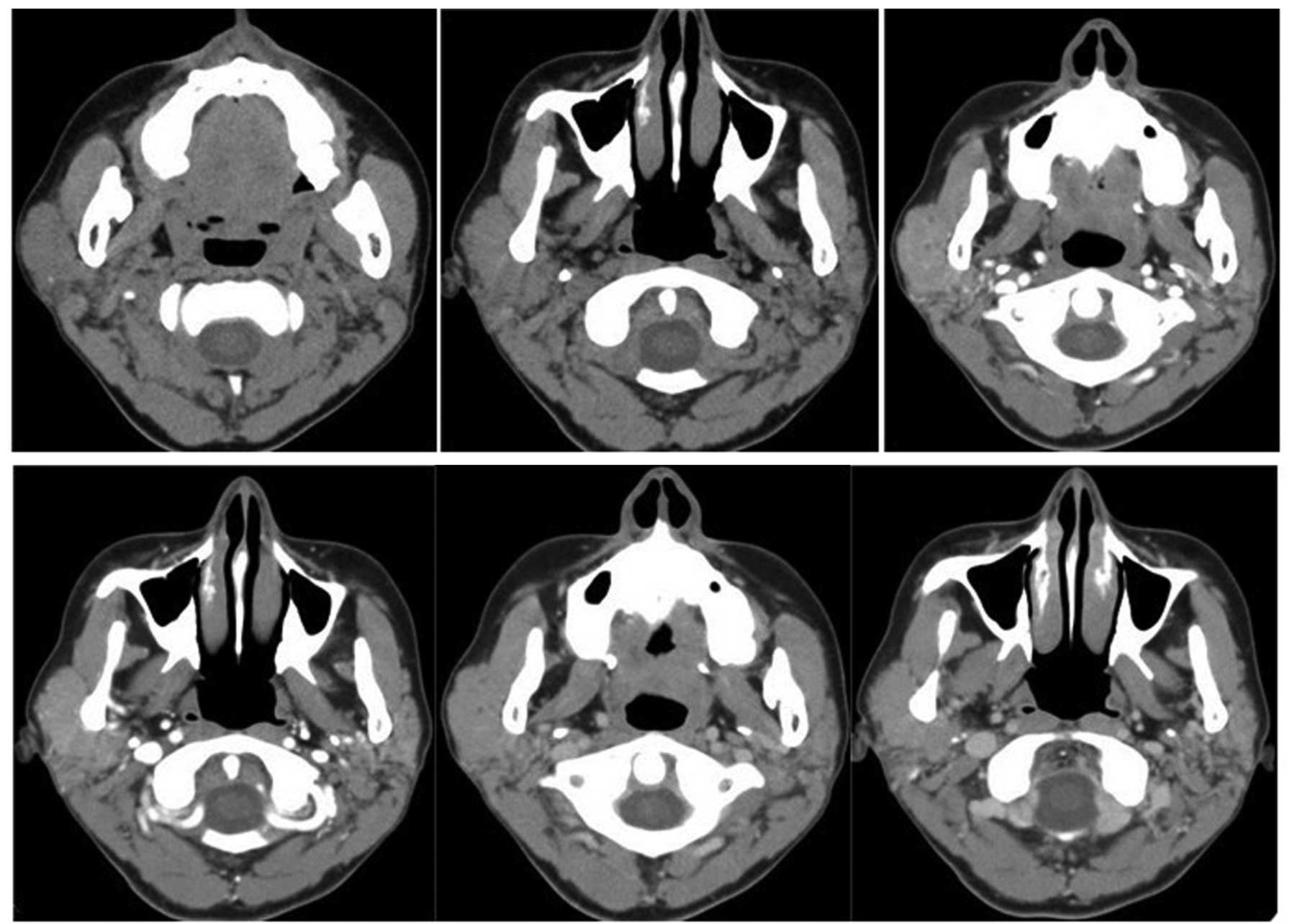
CT imaging features of MALT-lymphoma of
the parotid gland
As shown in Table
II, all the patients were diagnosed with benign lesions. Two
cases were also diagnosed with inflammation, three with mixed
tumors, two with glandular lymphomas and one with a benign tumor. A
total of 14 nodules were identified. Four cases were unilateral
single lymphomas, one was a unilateral multiple lymphoma with two
nodules, two were bilateral single lymphomas with four nodules and
one case was a bilateral multiple lymphoma with four nodules
(Table III). The sizes of the
nodules ranged between 0.60 and 5.44 cm, with the majority (12
nodules) in the 0.5–3 cm range. The main bodies of the nodules were
located in the superficial lobe. Only three nodules had invaded
into the deep lobe. Two nodules were round and the remaining six
were irregular in shape. Seven cases contained slight lobulation.
The margins in seven cases were unclear and the masses of six cases
were adhered to muscles. One case was cystic, four were with
punctiform necrosis and the remaining three cases contained
calcification. The solid section of the lesion appeared as an
evenly dense soft tissue density on the CT and the range of the CT
values was 35–59 HU. The solid area revealed a pattern of even
enhancement, particularly in the arterial phase. The increased
range of the CT value was 20–56 HU, mostly 20–40 HU. The increased
range of the CT value of the venous phase was 18–34 HU compared
with the plain CT scan. The density of the venous phase was
slightly lower than that of the arterial phase. The decreased CT
value of the venous phase ranged from −1–22 HU, often ≤15 HU,
compared with the arterial phase. Two cases exhibited swelling of
the parapharyngeal space lymphoid node. The density of the
bilateral parotid glands was uneven in five cases and the structure
was disordered. Multiple punctiform, nodular, striped slightly high
density shadows were observed (Figs.
1, 2 and 3).
 | Table IIICT characteristics in eight cases |
Table III
CT characteristics in eight cases
| Case | Side | Number | Size, cm (width ×
length) | Location | Morphology | Lobular | Margin |
|---|
| 1 | Unilateral | 1 | 1.42×2.49 | Deep | Irregular | Yes | Unclear |
| 2 | Unilateral | 1 | 2.57×2.84 | Deep | Round | Yes | Unclear |
| 3 | Unilateral | 1 | 0.96×1.13 | Superficial | Round | No | Clear |
| 4 | Unilateral | 1 | 0.95×2.42 | Superficial | Irregular | Yes | Unclear |
| 5 | Bilateral | 4 | 0.68×1.27,
0.60×1.00
0.60×0.60, 0.80×1.00 | Superficial | Irregular | No | Unclear |
| 6 | Bilateral | 2 | 1.96×3.52,
0.64×0.88 | Superficial | Irregular | Yes | Unclear |
| 7 | Unilateral | 2 | 1.57×2.58,
1.26×1.99 | Superficial | Irregular | Yes | Unclear |
| 8 | Bilateral | 2 | 2.51×5.44,
1.23×1.28 | Deep | Irregular | Yes | Unclear |
Discussion
MALT-lymphoma, also called the marginal lymphoma, is
a mild malignant tumor of the B lymphocytes that occurs outside the
lymphoid nodes and accounts for 4–13% of all lymphoma (4–6). The
most common site of occurrence is the gastrointestinal tract,
accounting for 45–56% of all MALT-lymphomas. Other commonly
occurring places include the lungs, eyes, conjunctiva, thyroid,
parotid gland, skin and breasts (4). Primary lymphomas of the parotid gland
form 0.6–5% of all the tumors of the parotid gland and tumor-like
lesions. Marginal lymphomas of B lymphocytes form ~30% (7,8).
Although MALT-lymphomas occur in structured lymph tissues, numerous
MALT-lymphomas occur in organs or tissues without intrinsic MALT in
normal conditions, including the stomach, salivary gland and
thyroid. Chronic inflammation or autoimmune diseases are the
foundation for these structures to acquire structured lymphoid
tissues. Acquired lymphoid tissues are the premise of
MALT-lymphomas (4). Li et al
revealed that MALT-lymphomas were based on chronic inflammation,
which may transfer for a long distance in the late period and
undergo a transition process from reactive lymphoid hyperplasia to
lymphoma of the B lymphocytes (9).
Certain cases may transform into diffuse large B-cell lymphomas.
MALT-lymphomas of the parotid gland have this pathological feature.
In the present study, five cases demonstrated chronic inflammation
and the infiltration of lymphocytes.
The pathological diagnostic standard of
MALT-lymphoma combines paraffin slices with immunohistochemistry.
The paraffin slice identifies the monoclonal property and the
immunohistochemistry identifies the origin of the B lymphocytes. B
cells express CD20 and CD79a. T cells are negative for CD5, CD10,
CD23 and CD43. The surface immunoglobulins are IgM+,
Bcl-2+ and IgD− (10). In the present study, the cases were
all positive for CD20 and CD79a and negative for CD10. The majority
of the cases were negative for CD3, CD5 and CD43. Two cases were
weakly-positive for CD3, CD5 and CD43, which may be associated with
the reactive T-cell hyperplasia that was observed around the
lesion.
The patients that are affected by MALT-lymphoma are
usually adults with a median age of 60 years and a male:female
ratio of 1.2:1 (11). In the
present study, the male:female ratio was1:7, which was affected by
the number of cases. The median age was 52 years, which was almost
consistent with the literature, however one patient was 14 years
old. MALT-lymphoma may occur unilaterally or bilaterally. In the
present study, five cases were unilateral and three were bilateral.
The course of the disease varied between two months and six years.
The main clinical presentation was a painless lump and no apparent
constitutional symptoms were observed. Symptoms of a dry mouth and
eyes were observed, similar to the symptoms of Sjögre’s syndrome.
One case demonstrated mild facial nerve injury symptoms.
Additionally, the boundary between the lump and the surrounding
tissues may be unclear in MALT-lymphoma. In the present study, the
lumps of six cases were not separate from the surrounding tissues
and exhibited the clinical features of malignant tumors. The lumps
were of moderate hardness and could only be moved slightly if at
all.
The parotid gland contains MALT in normal
conditions. B lymphocytes infiltrate and assemble within the
parotid gland during autoimmune disease, which increases the
succeptibility to MALT-lymphomas. Kassan et al (12) believed that patients with Sjögre’s
syndrome were 44 times more likely to develop MALT-lymphomas
compared with normal individuals. Wang et al (13) revealed that Sjögre’s syndrome is
associated with the occurrence, development and clinical
performance of non-Hodgkin lymphomas of the parotid gland. Certain
patients with Sjögre’s syndrome may develop lymphomas. In the
present study, seven cases had apparent Sjögre’s syndrome symptoms,
including a dry mouth and eyes, which was consistent with the
literature. As a result, strong vigilance is required to avoid
MALT-lymphoma in patients with Sjögre’s syndrome and lumps in the
parotid gland.
Imaging studies with regard to MALT-lymphomas of the
salivary gland have not been previously observed in the literature.
The present study identified that MALT-lymphomas often occur
unilaterally and that they may also occur bilaterally. Wen et
al (14) reported nine cases of
MALT-lymphoma of the salivary gland, one of which was a bilateral
multiple case. Li et al (15) reported three cases of MALT-lymphoma
of the parotid gland and one was a bilateral multiple case. The
size of the nodule is often 0.5–3 cm and is commonly located in the
superficial lobe of the parotid gland. The shape of the nodule may
occasionally be round, but is often irregular. The margin may be
clear or the nodule may be attached to the surrounding muscles with
an unclear margin. The nodule shares common features with malignant
tumors. MALT-lymphoma of the parotid gland is a slightly malignant
tumor. Therefore, the imaging performance is between that of
typical benign tumors and of malignant tumors. In the present
study, the soft tissue density was evenly dense and of slightly
higher density than the surrounding muscles on the plain scan. The
CT value was ~40 HU, although four cases reached >50 HU. Certain
nodules displayed necrosis and calcification and the CT value on
the plain scan was slightly higher than that of other parotid gland
tumors compared with previous studies, which may be associated with
the intensive arrangement of the tumor cells (9,14,16).
Following enhancement, the CT scan revealed a pattern of even
enhancement, with the exception of the necrotic and cystic regions.
The CT value of the arterial phase increased by 20–56 HU, while
that of the venous phase increased by 18–34 HU. The degree of
enhancement of the venous phase was slightly lower than that of the
arterial phase. The density of the venous phase was slightly higher
than that of the arterial phase in one case. The general
enhancement pattern was almost consistent with that of
MALT-lymphomas of other organs (2,3,15).
Extranodal lymphomas originate from the organ mesenchyme and the
tumor often grows along the edge of the organ, thus structure
residues of the primary tissue are commonly observed in tumors. In
the present study, the density of the majority of the tumors was
even. Certain tumors were not even due to the residues of the
primary tissue, including those of the organic intrinsic vessels,
the intermuscular space and the renal cortex. The degree of
enhancement is even and often ranges from low to moderate, with the
exception of cerebral tumors. The arterial phase shows a pattern of
slight enhancement, while the venous phase shows a pattern of
moderate enhancement or dynamic enhancement (16). The cases in the present study are
relatively consistent with the literature. The lymphomas were
mostly located in the envelop of the superficial lobe of the
parotid gland and demonstrated an even density on the plain scan or
the enhancement, with the exception of the necrotic regions.
However, in these cases, the arterial phase revealed a pattern of
enhancement, which may be associated with the delayed time.
The present study identified that the MALT-lymphomas
of the parotid gland demonstrated even isodense nodules whose
densities were slightly higher than that of the surrounding muscles
and other tumors of the parotid gland on plain CT scan. The
lymphomas easily became attached to the surrounding muscles. The
background of the parotid gland often showed inflammation of
heterogeneous density and a pattern of moderate enhancement, with
no significant features on the imaging. It is necessary to
distinguish MALT-lymphoma from benign or malignant tumors.
The mixed tumors of the parotid gland were the most
common benign tumors of the parotid gland identified. The CT
performance was the closest to that of MALT-lymphoma as it revealed
even or uneven density nodules of the soft tissue on the CT. The
nodules were nearly-round with clear margins and the density was
slightly lower than that of MALT-lymphoma on the plain scan and
revealed a pattern of slightly delayed enhancement. The amplitude
of the mixed tumor was weak in the early enhancement phase and the
mixed tumor had certain differences compared with MALT-lymphoma in
the moderate enhancement, which may provide a reference for
identification.
Glandular lymphomas of the parotid gland, basal
cytoma and myoepithelioma are another three common benign tumors,
which contain round or near-round nodules with clear margins on the
plain scan, often with cystic necrosis (10). In the present study, the glandular
lymphomas showed a pattern of early rapid enhancement with rapid
clearance of the contrast agent, while the basal cytoma and
myoepithelioma showed a pattern of continuous significant
enhancement. Glandular lymphomas may be bilateral and multiple. The
affected patients in the present study had a clinical history of
long-term smoking. Therefore, it was not difficult to distinguish
glandular lymphoma cases from those of MALT-lymphoma.
Primary epithelioid malignant tumors of the parotid
gland were complex and their CT performances were varied, with
typical features of large nodules, inner necrosis, unclear margins,
adhesion to the surrounding tissues and apparent uneven
enhancement. It was relatively easy to identify the tumors with
typical malignant features, but it was difficult to identify other
relatively small and indistinctive nodules. With the exception of
the imaging performance, the most significant basis for diagnosis
was whether there were the symptoms of a dry mouth and eyes, as in
Sjögre’s syndrome.
The treatment of MALT-lymphomas of the parotid gland
involves the surgical excision of the nodule and the gland, with
post-operative radiotherapy or chemotherapy. Zinzani et al
(4) reported that the recurrence
rate for MALT-lymphomas may be up to 17%. Recurrence includes the
transfer of local or surrounding lymphoid nodes and responds well
to treatment with chemotherapy assisted by a local injection of
interferon-α-II. In the present study, two cases recurred, one of
which was not administered post-operative chemotherapy. Six cases
did not experience recurrence.
The patients with MALT-lymphoma of the parotid gland
in the present study were all diagnosed with benign tumors
pre-operatively, mainly due to the fact that the CT performance was
similar to that of benign tumors and the cognition of its imaging
performance was lacking. MALT-lymphomas of the parotid gland have
certain features, including similar clinical symptoms to Sjögre’s
syndrome, and commonly occur in females. The condition frequently
appears in middle-aged and elderly patients and is often
distributed in the superficial lobes, but may also invade into the
deep lobes and be present as bilateral multiple lymphoma. The
uniform hyperdensity is higher than that of the surrounding muscle
tissues on the plain CT scan, and occasionally calcification and
necrosis is observed. The nodules may be of irregular morphology
and often appear to be slight lobulated with unclear margins and
attached to the surrounding muscles. The parenchyma shows moderate
enhancement and the degree of enhancement of the arterial phase is
close to that of the venous phase. These features may aid the
imaging diagnosis.
References
|
1
|
Isaacson P and Wright DH: Malignant
lymphoma of mucosa-associated lymphoid tissue. A distinctive type
of B-cell lymphoma. Cancer. 52:1410–1416. 1983. View Article : Google Scholar
|
|
2
|
Choi D, Lim HK, Lee SJ, et al: Gastric
mucosa-associated lymphoid tissue lymphoma: helical CT findings and
pathologic correlation. AJR Am J Roentgenol. 178:1117–1122. 2002.
View Article : Google Scholar
|
|
3
|
Zhang WD, Guan YB, Li CX, Huang XB and
Zhang FJ: Pulmonary mucosa-associated lymphoid tissue lymphoma:
computed tomography and 18F fluorodeoxyglucose-positron
emission tomography/computed tomography imaging findings and
follow-up. J Comput Assist Tomogr. 35:608–613. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Zinzani PL, Magagnoli M, Galieni P, et al:
Nongastrointestinal low-grade mucosa-associated lymphoid tissue
lymphoma: analysis of 75 patients. J Clin Oncol. 17:12541999.
|
|
5
|
Harris NL, Jaffe ES, Stein H, et al: A
revised European-American classification of lymphoid neoplasms: A
proposal from the International Lymphoma Study Group. Blood.
84:1361–1392. 1994.
|
|
6
|
Yao ZH, Liu YY, Zhao Y, et al: Analysis of
clinical data and prognosis for 24 patients with primary parotid
malignant lymphoma. J Leukemia Lymphoma. 18:616–618. 2009.
|
|
7
|
Barnes L, Myers EN and Prokopakis EP:
Primary lymphoma of the parotid gland. Arch Otolaryngol Head Neck
Surg. 124:573–577. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Harris NL: Lymphoid proliferations of the
salivary glands. Am J Clin Pathol. 111(1 Suppl 1): S94–S103.
1999.PubMed/NCBI
|
|
9
|
Li Yulin: Pathology. People’s Medical
Publishing House; Beijing: pp. 208–209. 2010
|
|
10
|
Bacon CM, Du MQ and Dogan A:
Mucosa-associated lymphoid tissue (MALT) lymphoma: a practical
guide for pathologists. J Clin Pathol. 60:361–372. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
No authors listed. A clinical evaluation
of the International Lymphoma Study Group classification of
non-Hodgkin’s lymphoma. The Non-Hodgkin’s Lymphoma Classification
Project. Blood. 89:3909–3918. 1997.
|
|
12
|
Kassan SS, Thomas TL, Moutsopoulos HM, et
al: Increased risk of lymphoma in sicca syndrome. Ann Intern Med.
89:888–892. 1978. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Yu C, Zhang ZY, Yang C, et al:
Retrospective study of the relativity of the Sjögren’s syndrome and
non-Hodgkin’s Lymphoma in parotid gland. China Ora Maxillo Surg.
14:227–229. 2004.
|
|
14
|
Wen WS, Hu M, Xu YL, et al: Clinical study
of mucosa-associated lymphoid tissue lymphoma of salivary glands.
Natl Med J China. 81:243–244. 2001.(In Chinese).
|
|
15
|
Li Q, Lai QS, Cui QC and Zhou WX:
Treatment and clinicopathologic analysis of mucosa-associated
lymphoid tissue lymphoma of the salivary glands. Zhongguo Yi Xue Ke
Xue Yuan Xue Bao. 25:214–217. 2003.(In Chinese).
|
|
16
|
Zhou JJ, Ding JG, Zhou KR, et al: The
correlation of general imaging features with the pathology in
extranodal lymphoma. J Clin Radiol. 26:618–622. 2007.
|