Introduction
Intradural extramedullary (IDEM) tumors are common
types of primary or secondary tumors located in the spinal canal;
neurinoma and meningioma are the most common types of IDEM tumor.
The most effective treatment of IDEM is achieved through early
excision. Laminectomy is the traditional approach used to excise
IDEM tumors; however, the stability of the spine is often affected,
due to impairment of the posterior column. With the development of
microsurgical techniques, to remove the tumor while maintaining the
stability of spinal biodynamics with the least amount of invasion
is raising more and more concerns. In recent years there have been
various studies (1,2) which have investigated the excision of
IDEM tumors through hemilaminectomy. Compared with the traditional
surgical approach, hemilaminectomy is relatively safer with fewer
traumas, and may help maintain the stability of the spine. If
surgical indications are interpreted correctly, satisfactory
results may be expected (3–5) In the present study, 16 cases of IDEM
tumor excision using hemilaminectomy are reported.
Patients and methods
General patient information
Sixteen patients (seven males, nine females), with
IDEM tumors removed by hemilaminectomy between January 2009 and
December 2011, were retrospectively analyzed. The mean patient age
was 49 years, ranging from 34–72 years. The patients’ complete
medical history ranged from 7 months to 3 years, with a mean of
15.7 months. The IDEM tumors were located at different levels of
the spinal canal (at the cervical level in three patients, thoracic
level in four and thoracico-lumbar level in nine). According to
preoperative Frankel classification, there were three cases
classified as grade B, five as grade C, seven as grade D and one as
grade E. All patients exhibited symptoms caused by spinal cord
compression, which were of varying severity. Twelve patients
experienced radicular pain, numbness or zonesthesia; 14 patients
suffered from various degrees of limited mobility, below the level
of the spinal cord compression; and 15 patients exhibited sensory
disturbance of varying severity. All patients were preoperatively
examined using magnetic resonance imaging (MRI; Achieva 3.0T TX,
Royal Philips Electronics, Amsterdam, The Netherlands) which
revealed masses located in the spinal canal. MRI imaging revealed
the precise spinal segments in which the tumors were located. This
study was conducted in accordance with the Declaration of Helsinki
and with approval from the ethics committee of Jilin University
(Changchun, China). Written informed consent was obtained from all
participants.
Procedures
All patients received general anesthetic and were
placed in the prone position. Syringe needle markers were inserted
into spinal processes under the fluoroscope of the C-arm X-ray
machine to assure accurate positioning. A posterior midline
longitudinal incision was made and the subcutaneous tissues and
lumbodorsal fascia of the affected side were divided. The
supraspinal ligaments, interspinal ligaments and tendinous
insertions of the contralateral muscles were retained. The
paraspinal muscles of the affected side were stripped, exposing the
unilateral lamina to the inner edge of the articular process.
Corresponding segments of the lamina were removed by a high-speed
burr. Ligamentum flavum was removed and the dural sac was exposed.
The oblique tilting of the operating table to the contralateral
side (typically 15–20 degrees) ensured an adequate surgical field
for the procedure. A microscope was positioned to begin
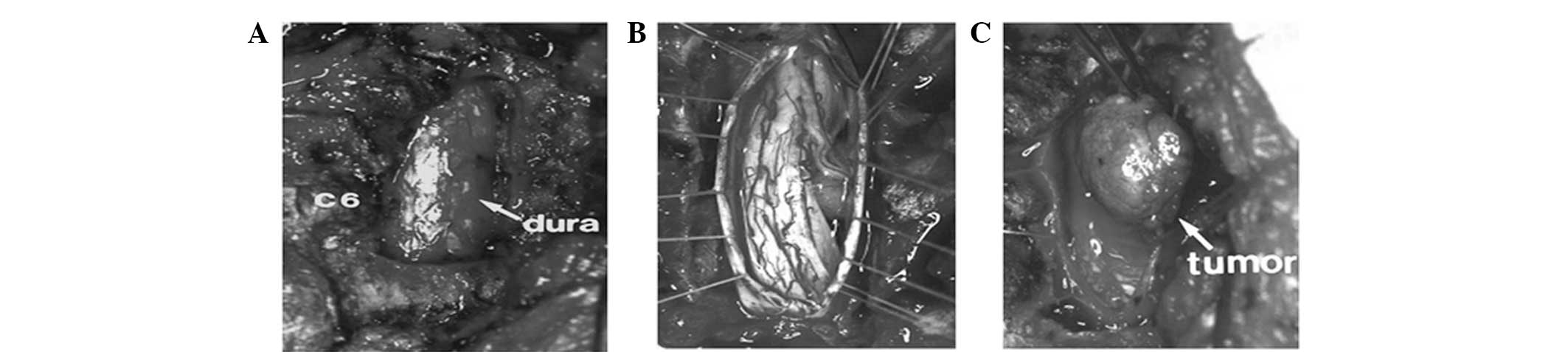
microsurgical excision of the IDEM tumors (Fig. 1). An intracapsule excision was made,
and then finished the removal of the IDEM tumors between the
surrounding normal structures and the tumor. Bipolar coagulation
was used to maintain hemostasis, and the dura mater was tightly
sutured with 5-0 lines using continuous mattress suture, covered
with an absorbable gelatin sponge. Negative pressure drainage was
performed in all the cases.. In two cases, tumors were large and
located to the rear, thus it was difficult to fully reveal the
tumors through hemilaminectomy. Therefore, laminectomy was
performed during surgery with internal fixation of the pedicle
screw and rod system. In the remaining cases, tumors were
successfully removed by hemilaminectomy. Generally,
negative-pressure drains were removed within 24–48 h. All 16
patients were confirmed to have IDEM tumors intraoperatively.
Results
The mean intraoperative bleeding volume was 300 ml
(range, 150–500 ml) and the mean surgery time was 140 min (range,
90–200 min). The mean bleeding volume of patients undergoing
hemilaminectomy and laminectomy was 275 and 475 ml, respectively.
All tumors were resected completely. The maximum tumor volume was
4×1.5×1.5 cm and the minimum was 1.5×1.0×1.0 cm. Neurinoma was
identified in 11 patients, meningioma in four cases and
neurofibroma in one case. Cerebrospinal fluid leakage occurred in
one patient; the fissure was tightly sutured with pressure
bandaging in the Trendelenburg position, infection did not occur
and the wound healed within 10 days. Patients were followed up for
a period of between 6 and 40 months, with a mean follow-up time of
23.7 months. There were no local tumor recurrences or secondary
spinal deformities, and spinal stabilities were determined to be
satisfactory. All patients achieved remission of symptoms. Pre- and
postoperative Frankel grades of the patients are shown in Table I.
 | Table IPre- and postoperative Frankel grades
of patients. |
Table I
Pre- and postoperative Frankel grades
of patients.
| Postoperative Frankel
grade |
|---|
|
|
|---|
| Preoperative Frankel
grade | A | B | C | D | E |
|---|
| A | 0 | 0 | 0 | 0 | 0 |
| B | 0 | 0 | 3 | 0 | 0 |
| C | 0 | 0 | 0 | 5 | 0 |
| D | 0 | 0 | 0 | 0 | 7 |
| E | 0 | 0 | 0 | 0 | 1 |
Discussion
Laminectomy is the traditional approach used to
excise IDEM tumors. However, as the removal of the posterior
lamina, spinous process, supraspinous ligament, interspinous
ligament and ligamentum flavum is necessary, the stability of the
spine is often affected due to impairment of the posterior column
(6–9). Postoperative instability is most
likely to occur in the cervical and lumbar segments of the spinal
canal (10). Lack of the posterior
column and exposure of the dural sac may lead to local fibrosis and
scar formation. Seppälä et al (11) reported 187 cases of intraspinal
neurinoma resection through laminectomy. The rate of total
resection was 90%. However, 10% of patients experienced various
postoperative complications (including pain, spinal instability and
cerebrospinal fluid leakage), and the mortality rate was 1.5%. The
incidence of spinal instability following laminectomy has been
reported to be 20% in adults (12)
and ≤45% (13) in children.
Due to the disadvantages of laminectomy, the use of
hemilaminectomy has been proposed for the treatment of IDEM tumors.
Chiou et al (14) reported
that patients undergoing microsurgical resection of intraspinal
tumors through hemilaminectomy demonstrated fewer postoperative
complications and shorter hospital stays than observed with
laminectomy. Yaşargil et al (15) recommended the use of hemilaminectomy
for the treatment of intraspinal tumors. Oktem et al
(16) reported 20 cases of
resection of intraspinal tumors through hemilaminectomy in 2000,
whereby no spinal instability was exhibited during two years of
patient follow-up. Yu et al (17) reported that excision of tumors by
hemilaminectomy resulted in a shorter duration of surgery and less
bleeding (P<0.01), compared with that by laminectomy. Naganawa
et al (18) reported that
hemilaminectomy could achieve increased neurofunctional recovery
and spinal stability, in 20 patients (mean follow-up period, 85
months) who underwent surgical resection of IDEM tumors through
hemilaminectomy. In the present study, no surgical wound infection
or spinal instability was observed. Patients could have bed
activities (including axial turning and a leg lift) 3 days after
surgery and were able to sit up and walk with the assistance of a
waist support 5 days after surgery; such clinical effects were
similar to those achieved in other reports (8,19).
The spinous process was left in place and therefore
the surgical field was relatively small, so surgery was inevitably
be affected when adopting hemilaminectomy (18). In order to increase the visual
field, damage to facet joints during surgery often occurs.
Therefore, it is necessary to preserve the lateral articular
processes, as damage to the facet joints is an important factor in
spinal instability (20). In the
present study, facetectomy was performed in order to fully expose
the elongated tumor in one patient that underwent hemilaminectomy
with the pedicle screw and rod system.
According to the experience of the authors, when
separating the tumor and spinal cord, the tumor should be stripped
gently. The spinal cords of some cases may become severely
compressed and neither nerve hook nor nerve stripper are permitted
to drag the spinal cord during surgery. Complete resectioning of
the well-encapsulated tumors is relatively facile. As for tumors
that are large, fragile and adhered to the dura mater or located
anterolateral to the spinal cord, decompression is performed by
piecemeal excision in order to avoid spinal cord damage. For tumors
in which the nerve fibers are trapped, it is important to avoid
avulsion of the spinal cord which may be caused by forcible
traction. The expansive growth of IDEM tumors leads to the
dilatation of dura mater, thus, the dura mater may be sutured
tightly without tension. When the dural mater is thin or absent, it
may be repaired with thoracolumbar fascia or artificial dura mater
in order to reduce cerebrospinal fluid leakage. Notably, suturing
of the dura mater in a limited operative view requires an adequate
amount of practice under a microscope.
In order to obtain complete resection of the tumor,
the parent nerve root and tumor could generally be resected
together without apparent postoperative dysfunction. Schuhhiess and
Gullotta (21) reported that 10
cases of relevant nerve root resection were performed for complete
removal of intraspinal neurinomas, whereby no serious or permanent
neurodysfunction was observed. However, Celli (22) reported that 26 patients with
neurinomas underwent relevant nerve root resection (C5-C8 or L3-S1)
whereby four patients exhibited aggravated motor dysfunction and
two patients experienced permanent motor dysfunction. In the
present study, five patients underwent inseparable parent nerve
root resection; two cases in the upper cervical spine and three
cases in the thoracic spine. Of those located in the cervical
spine, only one patient experienced postoperative ipsilateral
shoulder pain, and this gradually improved by itself. Sario-glu
et al (23) described 40
patients that underwent hemilaminectomy for resection of
intraspinal tumors and proposed that hemilaminectomy could be
applied to all intraspinal tumor resections, with the exception of
bilateral widely invading epidural tumors. In the present study,
the majority of the IDEM tumors inclined to one side, thus,
satisfactory surgical exposure was achieved. However, two of the
IDEM tumors were large, located ventrally and were difficult to
fully expose; therefore, laminectomy was performed instead, with
pedicle screw and rod systems.
With consideration of the stability of the facet
joints, the width of the open surgical window is usually 1.0–1.5
cm, thus, the tumor may not be fully exposed. The authors of the
present study argue that the width of the window of the cervical
canal should be 2 cm. The window located in the cervical segment is
the widest one of the spinal canal, followed by the lumbar segment.
Due to the location of the ribs and costotransverse joints, the
window width of the thoracic canal is the narrowest. In the current
study, since the majority of the IDEM tumors were relatively small
and inclined to one side, the width of the surgical window was
sufficient. The window width of patients was measured during
surgery. Among them, the width of the lower lumbar and upper
cervical segments were the widest, while the lower cervical and
thoracic segments remained relatively limited. The undercut of the
lamina may lead to difficulty in the removal of the tumor and
increase the possibility of spinal cord injury. Therefore,
hemilaminectomy could not applied to all intraspinal tumor
resections. We propose that unilateral IDEM tumors are the most
suitable for hemilaminectomy. Additionally, the transverse diameter
of the tumor should generally be < 2 cm and the span of the
tumor should be limited to a breadth of two vertebra.
In conclusion, microsurgical resection of IDEM
tumors by hemilaminectomy may conserve the stability of spinal
biodynamics with as little invasion as possible. It is of great
importance that the surgical indications are interpreted correctly
and complete tumor resectioning is achieved without aggravating the
spinal cord injury.
References
|
1
|
Naganawa T, Miyamoto K, Hosoe H, Suzuki N
and Shimizu K: Hemilaminectomy for removal of extramedullary or
extradural spinal cord tumors: medium to long-term clinical
outcomes. Yonsei Med J. 52:121–129. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mannion RJ, Nowitzke AM, Efendy J and Wood
MJ: Safety and efficacy of intradural extramedullary spinal tumor
removal using a minimally invasive approach. Neurosurgery. 68(1
Suppl Operative): 208–216. 2011. View Article : Google Scholar
|
|
3
|
Yeo DK, Im SB, Park KW, Shin DS, Kim BT
and Shin WH: Profiles of spinal cord tumors removed through a
unilateral hemilaminectomy. J Korean Neurosurg Soc. 50:195–200.
2011. View Article : Google Scholar
|
|
4
|
Raysi Dehcordi S, Marzi S, Ricci A, Di
Cola F and Galzio RJ: Less invasive approaches for the treatment of
cervical schwannomas: our experience. Eur Spine J. 21:887–896.
2012.
|
|
5
|
Sasani M, Sasani H, Kaner T and Fahir Ozer
A: Resection of a large spinal intradural ependymoma using a
limited unilateral laminectomy approach in the lumbosacral region.
J Neurosurg Sci. 56:55–59. 2012.
|
|
6
|
Canbay S, Hasturk AE, Basmaci M, Erten F
and Harman F: Management of thoracal and lumbar schwannomas using a
unilateral approach without instability: An analysis of 15 cases.
Asian Spine J. 6:43–49. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Bozkus H, Sasani M, Oktenoglu T, Aydin AL
and Ozer AF: Unilateral dynamic stabilization for unilateral lumbar
spinal pathologies; a new surgical concept. Turk Neurosurg.
22:718–723. 2012.PubMed/NCBI
|
|
8
|
Iacoangeli M, Gladi M, Di Rienzo A, et al:
Minimally invasive surgery for benign intradural extramedullary
spinal meningiomas: experience of a single institution in a cohort
of elderly patients and review of the literature. Clin Interv
Aging. 7:557–564. 2012. View Article : Google Scholar
|
|
9
|
Zong S, Zeng G, Xiong C and Wei B:
Treatment results in the differential surgery of intradural
extramedullary schwannoma of 110 cases. PLoS One. 8:e638672013.
View Article : Google Scholar
|
|
10
|
Perez-Cruet MJ, Fessler RG and Perin NI:
Review: complications of minimally invasive spinal surgery.
Neurosurgery. 51(5 Suppl): S26–S36. 2002.
|
|
11
|
Seppälä MT, Haltia MJ, Sankila RJ,
Jääskeläinen JE and Heiskanen O: Long-term outcome after removal of
spinal schwannoma: a clinicopathological study of 187 cases. J
Neurosurg. 83:621–626. 1995.
|
|
12
|
Katsumi Y, Honma T and Nakamura T:
Analysis of cervical instability resulting from laminectomies for
removal of spinal cord tumor. Spine (Phila Pa 1976). 14:1171–1176.
1989. View Article : Google Scholar
|
|
13
|
Yeh JS, Sgouros S, Walsh AR and Hockley
AD: Spinal sagittal malalignment following surgery for primary
intramedullary tumours in children. Pediatr Neurosurg. 35:318–324.
2001. View Article : Google Scholar
|
|
14
|
Chiou SM, Eggert HR, Laborde G and Seeger
W: Microsurgical unilateral approaches for spinal tumour surgery:
eight years’ experience in 256 primary operated patients. Acta
Neurochir (Wien). 100:127–133. 1989.PubMed/NCBI
|
|
15
|
Yaşargil MG, Tranmer BI, Adamson TE and
Roth P: Unilateral partial hemi-laminectomy for the removal of
extra- and intramedullary tumours and AVMs. Adv Tech Stand
Neurosurg. 18:113–132. 1991.
|
|
16
|
Oktem IS, Akdemir H, Kurtsoy A, Koç RK,
Menkü A and Tucer B: Hemilaminectomy for the removal of the spinal
lesions. Spinal Cord. 38:92–96. 2000. View Article : Google Scholar
|
|
17
|
Yu Y, Zhang X, Hu F, Xie T and Gu Y:
Minimally invasive microsurgical treatment of cervical intraspinal
extramedullary tumors. J Clin Neurosci. 18:1168–1173. 2011.
View Article : Google Scholar
|
|
18
|
Naganawa T, Miyamoto K, Hosoe H, Suzuki N
and Shimizu K: Hemilaminectomy for removal of extramedullary or
extradural spinal cord tumors: medium to long-term clinical
outcomes. Yonsei Med J. 52:121–129. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ahn DK, Park HS, Choi DJ, et al: The
surgical treatment for spinal intradural extramedullary tumors.
Clin Orthop Surg. 1:165–172. 2009. View Article : Google Scholar
|
|
20
|
Zander T, Rohlmann A, Klöckner C and
Bergmann G: Influence of graded facetectomy and laminectomy on
spinal biomechanics. Eur Spine J. 12:427–434. 2003. View Article : Google Scholar
|
|
21
|
Schultheiss R and Gullotta G: Resection of
relevant nerve roots in surgery of spinal neurinomas without
persisting neurological deficit. Acta Neurochir (Wien). 122:91–96.
1993. View Article : Google Scholar
|
|
22
|
Celli P: Treatment of relevant nerve roots
involved in nerve sheath tumors: removal or preservation?
Neurosurgery. 51:684–692. 2002.
|
|
23
|
Sario-glu AC, Hanci M, Bozkuş H, Kaynar MY
and Kafadar A: Unilateral hemilaminectomy for the removal of the
spinal space-occupying lesions. Minim Invasive Neurosurg. 40:74–77.
1997. View Article : Google Scholar : PubMed/NCBI
|