Introduction
Extraskeletal osteosarcomas (OSs) are extremely
rare, malignant neoplasms. In the general population, primary
osteosarcomas constitute <1% of all malignant neoplasms of the
breast. OS of the breast may constitute between 12.5 to 17% of all
breast sarcomas (2,3). In the literature, single cases of OS
have been reported to be located in the thyroid, kidneys, urinary
bladder, colon, heart, testes, gall bladder and cerebellum
(4). Primary osteogenic sarcoma is
an extremely aggressive neoplasm. It is characterised by a high
percentage of early, local recurrences and high metastatic
potential, mostly spreading via the blood. Metastases are most
commonly observed in the lungs and bones (1,5,6). The
current study presents the details of the diagnostic process,
treatment and 18-month follow-up of a 67-year-old patient with
primary OS of the left breast. Written informed consent was
obtained from the patient’s family.
Case presentation
A 67-year-old female patient was admitted to the
Oncology Clinic of the Gdynia Oncology Centre (GCO; Gdynia, Poland)
with a self-detected lump in the left breast. Medical history,
physical examination and additional diagnostic tests, including
mammography, ultrasonography (USG) of the breast, core-needle
biopsy of the palpable breast abnormality, radiological imaging of
chest and laboratory tests, were performed. According to the test
results and the clinical evaluation, a preliminary diagnosis of OS
of the left breast was established.
The mammogram revealed a 5-cm, smooth-contoured
lesion of a regular density in the left breast, located behind the
nipple. On the mammography images of the left breast obtained 5
years earlier, there was no such lesion present, nor were any other
pathological lesions. No lesion was demonstrated in the right
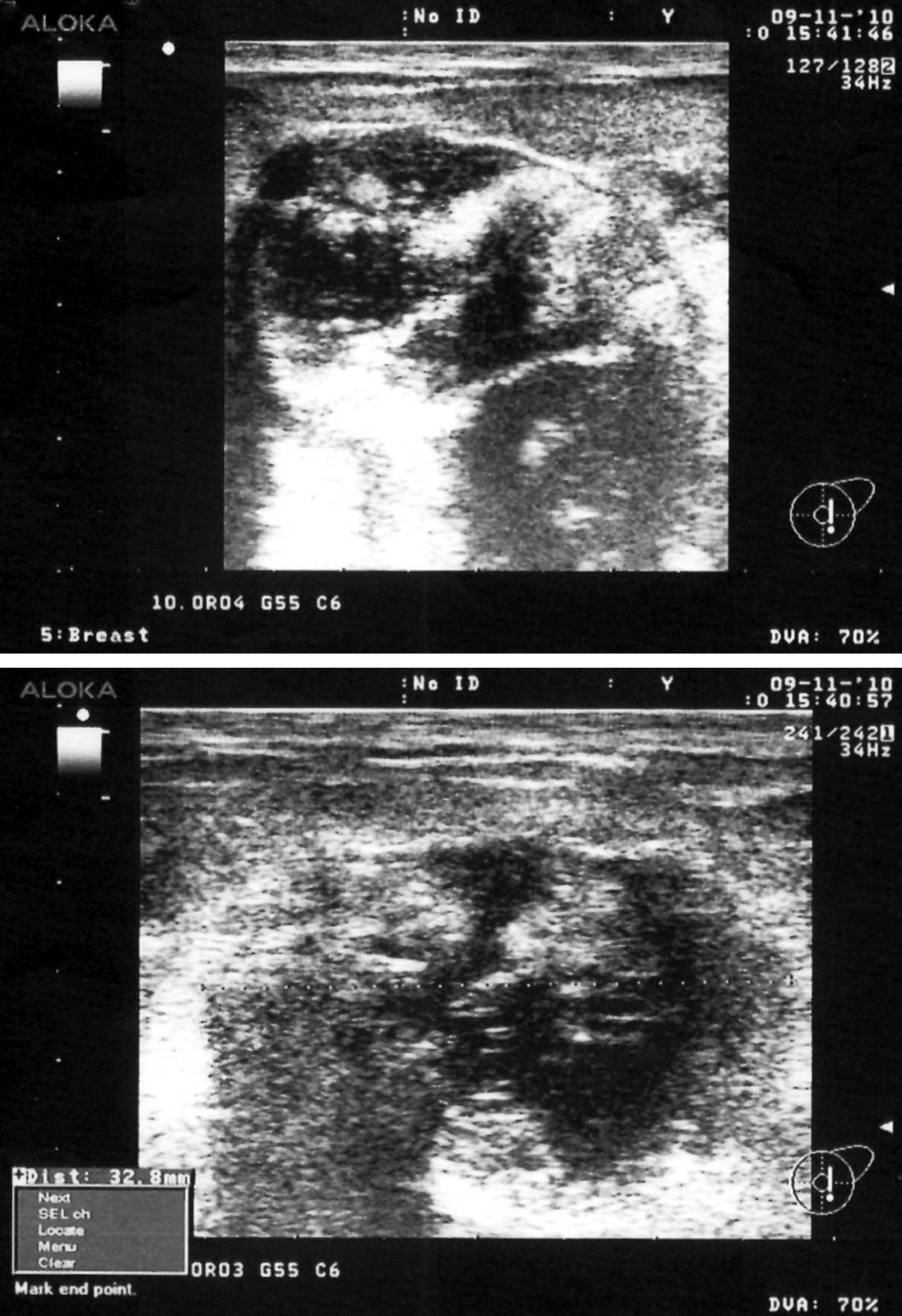
breast. Additional USG of the breast revealed a polycyclic, oval
lesion with heterogeneous echogenicity behind the nipple (Fig. 1). No axillary lymphadenopathy was
observed. Medical imaging indicated a malignant neoplasm of the
left breast. A thorax radiograph and laboratory test results did
not reveal any abnormalities. Fine-needle biopsy demonstrated a
high density, amorphous protein mass with diffused neutrophils and
shadows of necrotic cells. According to the results of the core
biopsy, there was suspicion of primary extraskeletal OS or a
malignant phyllodes tumour.
One month from the beginning of the diagnostic
procedures, the patient was admitted to the Oncological Surgery
Ward of GCO. Besides tumour of the breast, the patient did not
report any other discomforts. The patient had previously given
birth twice at the ages of 22 and 23 years. The patient breast-fed
her children for 12 and 3 months, respectively and did not
experience any mastitis or mechanical injuries of the breast area.
The patient never received any hormonal therapy medicines,
radiotherapy or treatment for any breast lesion. Several years
earlier, the patient underwent surgery for varicose veins of the
lower extremities, and has suffered from hypoacusis for several
years. The mother of the patient was diagnosed with breast cancer
at 33 years. Upon physical examination, a palpable tumour of 7 cm
in diameter was located behind the nipple of the left breast of the
patient, clinically staged at cT3N0. The lesion did not cause any
pain and there was no leakage from the nipple. Besides hypoacusis,
no other abnormalities were observed.
During the surgery, tumour resection with normal
tissue margins was achieved, confirmed by an intra-operative
histological examination. The frozen section examination led to a
diagnosis of malignant non-epithelial OS. A decision to extend the
surgical margins for a simple mastectomy of the left breast was
made. No complications occurred during the surgery and the patient
was discharged after 2 days. A decision regarding further treatment
was postponed until a full histopathological report was
obtained.
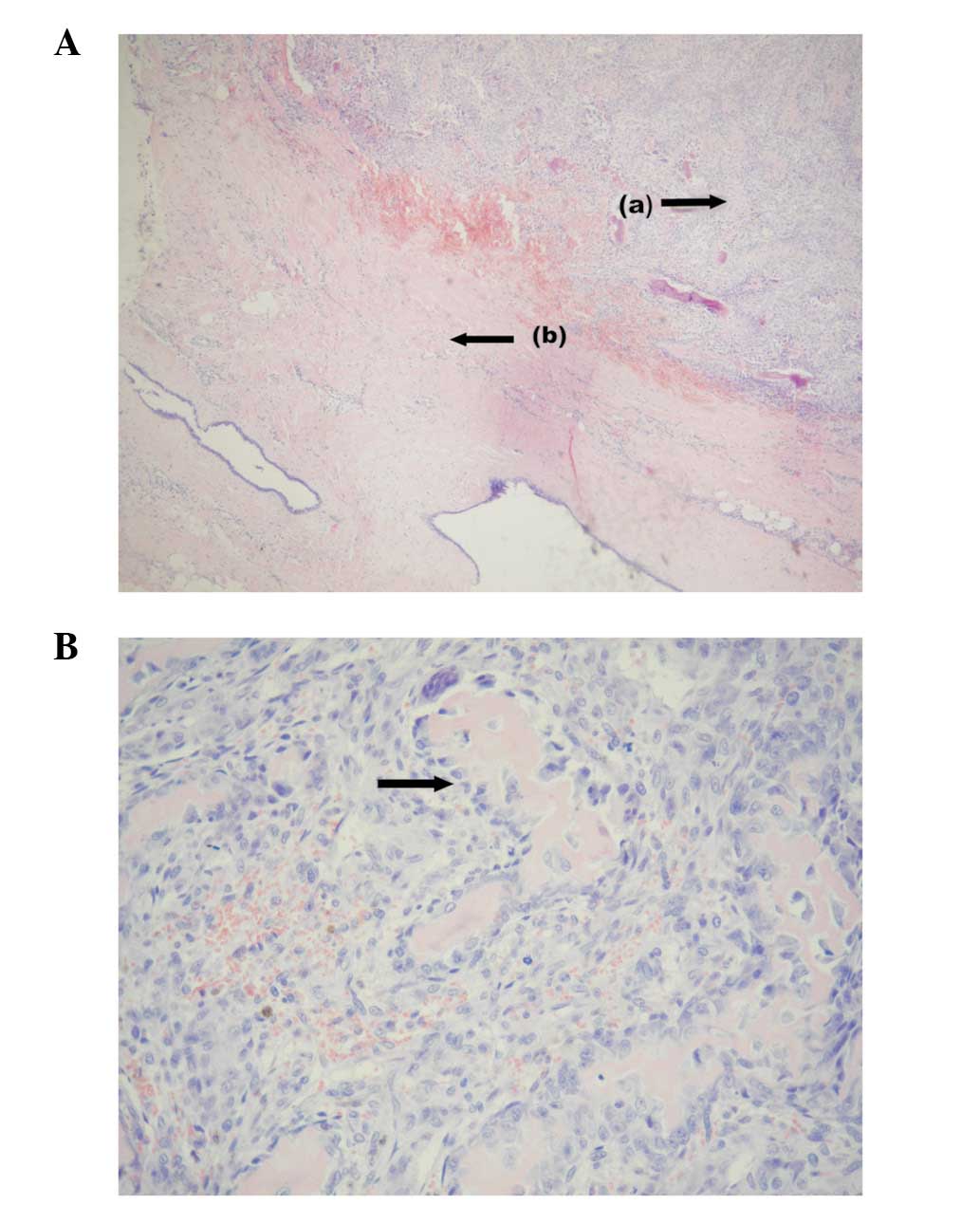
The histopathological report described a solid,
polycyclic, well-circumscribed tumour that was 6 cm in diameter.
Macroscopically, the tumour tissue was grey-pink, hyaline, with
nodules of decay and fibrosis. Microscopic examination showed the
presence of a neoplastic osteoid. Immunohistochemical staining did
not reveal any epithelial component [cytokeratin (CK) AE1/AE3(-),
CK7(-) and epithelial membrane antigen(-)], however, vimentin
immunoreactivity was detected. The mitotic index [Ki-67(+),
>70%]indicated high mitotic activity of the tumour. The
diagnosis of extraskeletal OS was confirmed (Fig. 2A and B). No other tumour nodules
were present in the amputated breast tissue. Surgical margins were
3 cm in distance from the tumour site in all directions. Follow-up
visits every 3 months were recommended to the patient.
During the first year of follow-up, no evidence of
relapse was detected and 14 months following the diagnosis, a
thorax radiograph showed metastatic nodules in the lower site of
the right lung. A thorax computed tomography (CT) scan confirmed
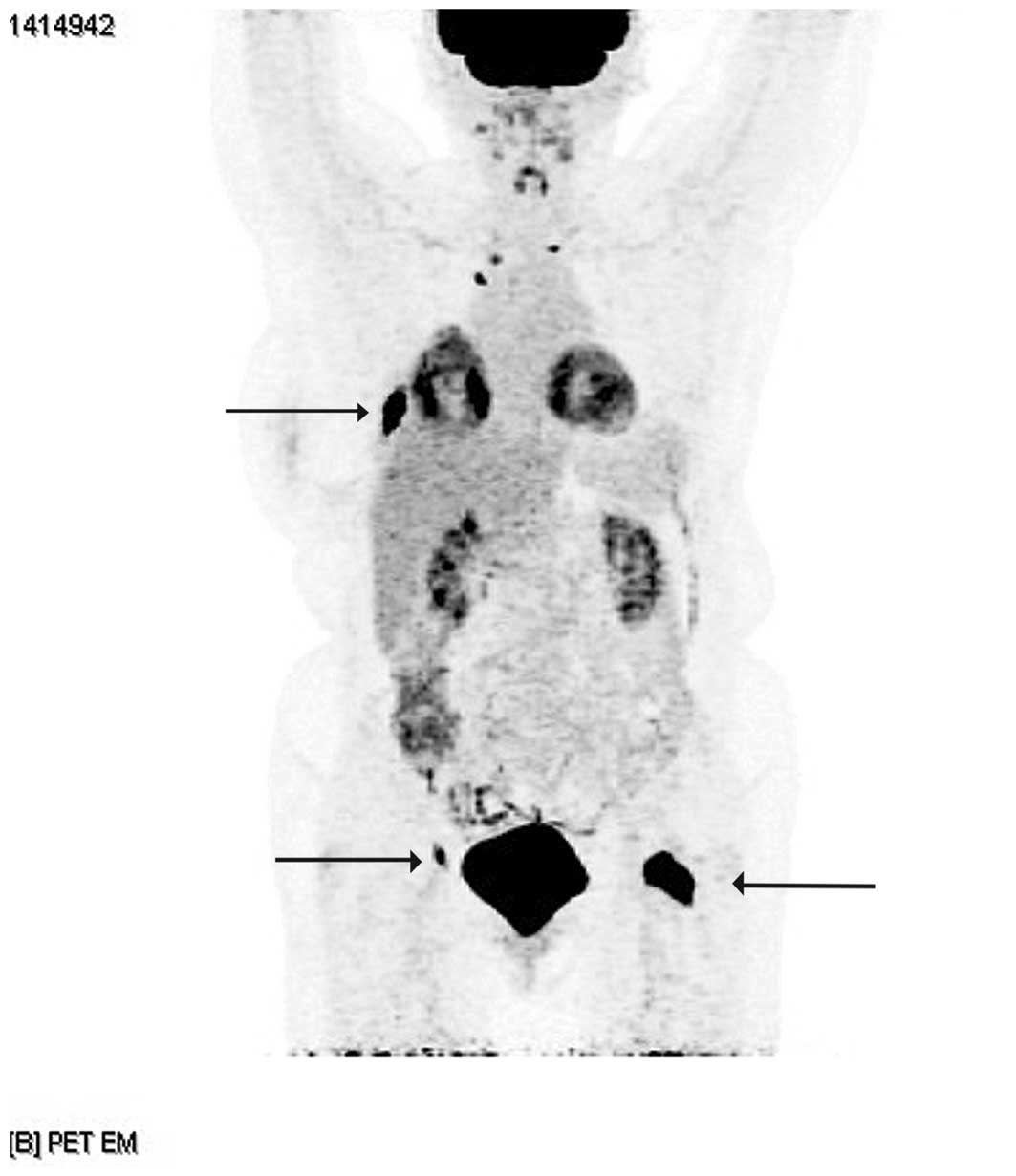
this observation. Due to bone pain, a positron emission
tomography-CT scan was performed, which demonstrated tumour
metastases in the bones (thoracic section of the spine, rib VIII on
the right side, right ischial bone and collum of the thigh bone)
(Fig. 3). Additionally, a
pathological break of the collum of the right thigh bone was
diagnosed. Besides palliative radiotherapy for the collum of the
thigh bone, no other oncological treatment was administered. The
patient succumbed to the disease due to dissemination 18 months
following surgery.
Discussion
The mechanism of tumourigenesis of primary breast OS
is unclear. It has been indicated that the tumours arise from
totipotent mesenchymal cells of the breast stroma. Another possible
mechanism is transformation from a pre-existing breast fibroadenoma
or phyllodes tumour (2,6,7).
Radiotherapy may induce the formation of breast sarcomas,
predominantly angiosarcomas and chest wall OS. Such an association
was observed in patients treated with radiotherapy for epithelial
breast neoplasms (8–10). In the reported case, there was no
data indicating histogenesis of OS from a pre-existing fibroadenoma
or phyllodes tumour; lack of previous breast pathology and a
negative result in mammography 2 years earlier. An association with
radiotherapy was also excluded.
As reported in the literature, primary breast OS
mainly occurs in females of >60 years, which is consistent with
the observation in the present case (1,5–7,11–14).
The malignancy has also been observed in younger females (1,4,8,15,16).
A report of male primary breast OS also exists (1). Similar to the current patient, a
physical examination revealed a palpable, firm, mobile mass that
did not cause contraction of the nipple. Usually, it is without
bloody leakage from the nipple and axillary lymph node enlargement
(1,5–8,11,13–15).
The presence of palpable enlarged axillary lymph nodes on the side
of the tumour has only been reported in two primary breast OS cases
(4,12). Similar to the radiology examinations
of the current patient, in mammography imaging, OS presents as a
well-circumscribed, oval and firm calcified mass (6–8,11–15).
In USG imaging, the tumour may be observed with blurred outlines,
heterogeneous echogenicity and focal calcification (8,11,14,15).
Histopathological evaluation is fundamental for the
diagnosis of primary extraskeletal OS. According to the criteria
established in the study by Allan and Soule (17), the basis of the diagnosis of
extraskeletal OS should be as follows: Presence of neoplastic
osteoid or bone tumor in the microscopic section, origination from
the bones excluded and absence of an epithelial component. In the
present case study, these criteria are fulfilled.
The fundamental element of the treatment of primary
breast OS is surgery, which consists of complete tumour resection
with normal tissue margins or a simple mastectomy (1,5,6,13).
Metastases in lymph nodes in breast OS cases are uncommon, as is OS
localised in the bones (1,7,8,15,16,18).
A lymphadenectomy in patients with OS is justified in situations
where axillary lymphadenopathy is observed. In such cases,
palpable, enlarged lymph nodes may be the site of neoplastic
metastases (4,12). In the present case, the simple
mastectomy was performed as no enlarged lymph nodes were observed
during the physical examination.
To obtain an increased survival time in cases of
primary breast OS of the bones, multi-agent chemotherapy, including
doxorubicin, cisplatin, high-dose methotrexate with leucovorin and
ifosfamide, is used (18). Applying
this option is not standard treatment for the management of breast
OS patients due to the limited number of clinical trials where
polychemotherapy has been used in cases of this extremely rare
tumour (1,4–6,11–15).
In a situation where tumour-free surgical margins cannot be
obtained, postoperative radiotherapy is sometimes advisable
(4,5,8,19–20).
Due to the rarity of the described tumour, results
are absent regarding overall survival in primary breast OS. In one
study, the 5-year survival rate was evaluated as <38%. In the
group of 50 patients with primary breast OS, metastases were
observed in 41%, mainly in the lung, and in almost half of these,
metastases were detected >1 year post-diagnosis. The patients
with detected metastases succumbed ≤20 months from diagnosis
(median, 2 months) (1).
In the current study, a case of primary breast OS, a
rare, malignant tumour of the breast is presented. The follow-up
confirms that local therapy with assurance of adequate tumour-free
margins may effectively protect a patient against relapse, even in
the situation of a large tumour. Systemic dissemination of breast
OS remains the greatest problem in treatment.
References
|
1
|
Silver SA and Tavassoli FA: Primary
osteogenic sarcoma of the breast: a clinicopathologic analysis of
50 cases. Am J Surg Pathol. 22:925–933. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Jernstrom P, Lindberg AL and Meland ON:
Osteogenic sarcoma of the mammary gland. Am J Clin Pathol.
40:521–526. 1963.PubMed/NCBI
|
|
3
|
Ciatto S, Bonardi R, Cataliotti L and
Cardona G: Sarcomas of the breast: a multicenter series of 70
cases. Neoplasma. 39:375–379. 1992.PubMed/NCBI
|
|
4
|
Ogundiran TO, Ademola SA, Oluwatosin OM,
Akang EE and Adebamowo CA: Primary osteogenic sarcoma of the
breast. World J Surg Oncol. 4:902006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Khan S, Griffiths EA, Shah N and Ravi S:
Primary osteogenic sarcoma of the breast: A case report. Cases J.
1:1482008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bahrami A, Resetkova E, Ro JY, Ibañez JD
and Ayala AG: Primary osteosarcoma of the breast: report of 2
cases. Arch Pathol Lab Med. 131:792–795. 2007.PubMed/NCBI
|
|
7
|
Remadi S, Doussis-Anagnostopoulu I and Mac
Gee W: Primary osteosarcoma of the breast. Pathol Res Pract.
191:471–477. 1995. View Article : Google Scholar
|
|
8
|
Brustugun OT, Reed W, Poulsen JP and
Bruland OS: Primary osteosarcoma of the breast. Acta Oncol.
44:767–770. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Karlsson P, Holmberg E, Samuelsson A,
Johansson KA and Wallgren A: Soft tissue sarcoma after treatment
for breast cancer - a Swedish population-based study. Eur J Cancer.
34:2068–2075. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rudman F Jr, Stanec S, Stanec M, et al:
Rare complication of breast cancer irradiation: postirradiation
osteosarcoma. Ann Plast Surg. 48:318–322. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dragoumis D, Bimpa K, Assimaki A and
Tsiftsoglou A: Primary osteogenic sarcoma of the breast. Singapore
Med J. 49:e315–e317. 2008.PubMed/NCBI
|
|
12
|
Momoi H, Wada Y, Sarumaru S, et al:
Primary osteosarcoma of the breast. Breast Cancer. 11:396–400.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Irshad K, Mann BS and Cambell H: Primary
osteosarcoma of the breast. Breast. 12:72–74. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Brown AL, Holwill SD, Thomas VA, Sacks NP
and Given-Wilson R: Case report: Primary osteosarcoma of the
breast: imaging and histological features. Clin Radiol. 53:920–922.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Fiori E, Burza A, Izzo L, et al: Primary
osteosarcoma of the breast. Breast J. 16:656–658. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Adem C, Reynolds C, Ingle JN and
Nascimento AG: Primary breast sarcoma: clinicopathologic series
from the Mayo Clinic and review of the literature. Br J Cancer.
91:237–241. 2004.PubMed/NCBI
|
|
17
|
Allan CJ and Soule EH: Osteogenic sarcoma
of the somatic soft tissues. A clinicopathologic study of 26 cases
and review of literature. Cancer. 27:1121–1133. 1971. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Ritter J and Bielack SS: Osteosarcoma. Ann
Oncol. 21(Suppl 7): 320–325. 2010. View Article : Google Scholar
|
|
19
|
McGowan TS, Cummings BJ, O’Sullivan B,
Catton CN, Miller N and Panzarella T: An analysis of 78 breast
sarcoma patients without distant metastases at presentation. Int J
Radiat Oncol Biol Phys. 46:383–390. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kaiser U, Barth P, Duda V, Pflüger KH and
Havemann K: Primary osteosarcoma of the breast - case report and
review of literature. Acta Oncol. 33:74–76. 1994. View Article : Google Scholar
|