Introduction
Laparoscopic nephron-sparing surgery has been
increasingly performed by urologists for patients with renal
tumors, and its complications have received increasing attention
(1). As a rare and potentially
fatal complication, renal artery pseudoaneurysm (RAP) is often
reported in patients undergoing percutaneous nephroscopy, renal
trauma, renal transplantation and kidney biopsy. Recently, two
patients underwent laparoscopic partial nephrectomy for central
renal tumors at The First Affiliated Hospital of Zhejiang
University School of Medicine (Hangzhou, China) who had developed
RAPs following surgery. The aim of the present study was to
introduce a novel therapeutic method, superselective embolization
of the renal artery branches, which was used to cure these two
patients. Written informed consent was obtained from the
patients.
Case report
Laparoscopic surgical procedures
The two patients underwent four-port extraperitoneal
laparoscopic procedures. Preoperative computed tomography (CT)
angiography indicated only one main trunk of the renal artery of
the affected kidney in each patient. Initially, a noninvasive
vascular clip was used to block the main trunk of the renal artery.
The edge of the tumor was identified and scissors were used to
resect the tumor with a 5-mm margin. A 3-0 coated
Vicryl® (polyglactin 910) suture (Johnson & Johnson,
New Brunswick, NJ, USA) was used to close the vascular section with
the hemorrhage and collecting system. Then, 2-0 coated Vicryl
(polyglactin 910) suture (Johnson & Johnson) and an absorbable
clip were used to close the renal parenchyma wound. The noninvasive
vascular clip was released and inactive bleeding was confirmed. The
renal fossa drainage tubes of cases one and two were withdrawn
seven and five days following surgery, respectively.
Case one
A 68-year-old male patient presented to The First
Affiliated Hospital of Zhejiang University School of Medicine with
a previous history of hypertension and diabetes. A 2.5×2.5-cm
space-occupying lesion in the center of the lower pole of the right
kidney parenchyma was identified during the physical examination
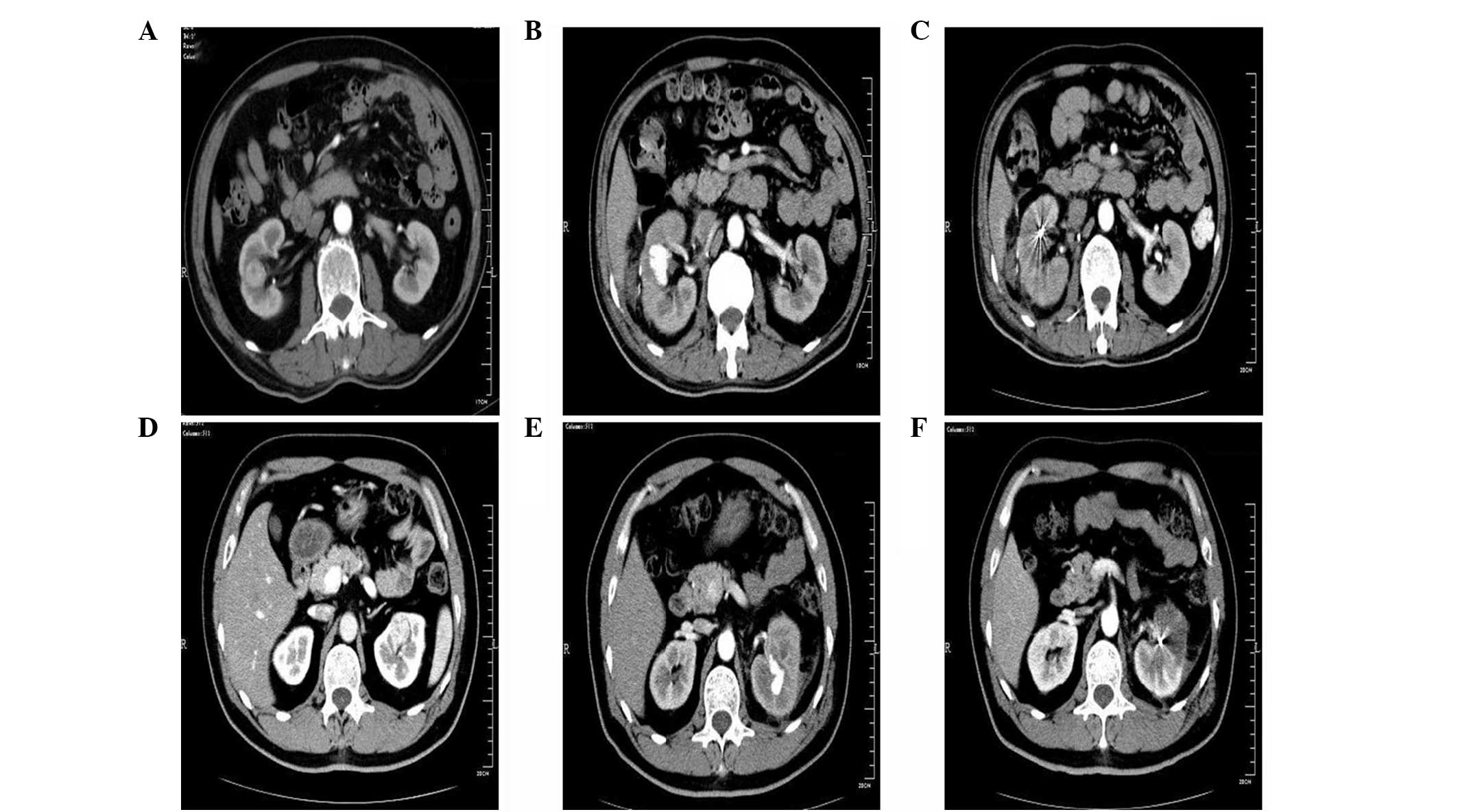
(Fig. 1A). The results of the
preoperative CT angiography indicated that the bilateral renal
arteries had only one main trunk and no abnormal feeding arteries
of the lesion. The results of the preoperative laboratory tests
(liver function, kidney function, routine blood test and clotting
time) were all within normal ranges. Laparoscopic surgery was
performed as previously described. The warm ischemia time of the
right kidney was 28 min and postoperative recovery of the patient
was good. The pathological examination was performed to confirm
renal cell carcinoma (clear cell type) and the negative
margins.
On day 23 following surgery, the patient complained
of gross total hematuria. The enhanced CT scan found a 6-cm
hematoma on the edge of the right kidney and a 2.2-cm cystic shadow
bound to the surgical area of the right kidney with enhancement.
These results suggested the formation of a RAP (Fig. 1B). On day 25 following surgery, the
selective embolization of the right renal artery branches failed.
Thus, on day 29, the embolization was performed again and was
successful. The hematuria was controlled and the results of the CT
scan performed two weeks following the embolization indicated that
the RAP had contracted (Fig.
1C).
Case two
A 47-year-old male patient presented to The First
Affiliated Hospital of Zhejiang University School of Medicine with
a previous history of diabetes. A 2.5×3-cm space-occupying lesion
in the center of the upper pole of the left kidney parenchyma was
identified during a physical examination (Fig. 1D). The results of the preoperative
CT angiography indicated that the bilateral renal arteries had only
one main trunk and no abnormal feeding arteries of the lesion. The
results of the preoperative laboratory tests (liver function,
kidney function, routine blood test and clotting time) were all
within normal ranges. Laparoscopic surgery was performed as
previously described. The warm ischemia time of the left kidney was
31 min and postoperative recovery of the patient was good. The
pathological examination was performed to confirm the
angiomyolipoma.
On day 31 following surgery, the patient complained
of gross total hematuria and left lumbago, and received symptomatic
hemostasis at Xinchang Renmin Hospital (Xinchang, China), but the
symptoms were not controlled. On day 36 following surgery, the
patient was admitted to The First Affiliated Hospital of Zhejiang
University School of Medicine. A contrast-enhanced CT scan revealed
a ~3-cm cystic shadow bound to the center of the upper pole of the
left kidney, with enhancement similar to that of the surrounding
renal arteries, which suggested the formation of a RAP (Fig. 1E). On day 37 following surgery, the
patient underwent selective embolization of the left renal artery
branches. This procedure was successful and the patient’s hematuria
was controlled. The results of the CT scan performed one week
following the embolization indicated that the RAP had contracted
(Fig. 1F).
Discussion
In 1993, Winfield et al first reported
laparoscopic partial nephrectomy for benign kidney disease
(2). To date, this surgery has been
increasingly used to treat patients with malignant renal
tumors.
Rupture and hemorrhage of the renal artery or renal
artery branch may lead to a hematoma, which may be wrapped by the
surrounding tissue and form a cystic cavity that connects with the
artery, a condition termed as RAP (3). The cyst does not have a normal
arterial wall structure and its size gradually increases due to
blood flow in the artery. If the collecting system is affected,
hematuria may occur and if the cyst breaks through the renal
capsule, retroperitoneal hematoma may occur, forming a pulsatile
hematoma. RAP rupture may be fatal in severe cases. The reported
incidence rates of RAP following open partial nephrectomy and
laparoscopic partial nephrectomy are 0.43 (4) and 0.97–1.7% (5,6),
respectively. However, the incidence rate of RAP can be as high as
7.5% following laparoscopic partial nephrectomy for central renal
tumors (7).
In the two present cases, RAP occurred several weeks
following surgery. There are two possible reasons for this delay
according to the current analysis (8). Firstly, the degradation of the
absorbable suture may result in decreased tension at the ligation
site in the kidney parenchyma and rehemorrhage of small blood
vessels, such as the renal segmental arteries and arcuate artery,
resulting in the formation of RAP. Secondly, blockage of the renal
artery during surgery may make it difficult to identify the
cross-sections of the small blood vessels. When the renal
parenchyma is closed and the vascular clip on the renal artery is
released, the tension of the suture does not completely block the
blood flow into the small branches of the renal artery. Thus, blood
clots may obstruct the small branches and result in rehemorrhage
and formation of RAP long after patient discharge (6).
In open partial nephrectomy, the cross-sections of
the blood vessels at the kidney wound can be identified and sutured
more easily. However, in laparoscopy, the suturing of single small
blood vessel sections is difficult and time-consuming, and the
kidney is in a state of warm ischemia. Surgeons often close
laparoscopic kidney wounds with continuous absorbable sutures to
reduce renal warm ischemia time, and this may be one of the reasons
why the incidence rate of RAP following laparoscopic partial
nephrectomy is marginally higher than that following open surgery.
With the widespread use of laparoscopic partial nephrectomy, the
skillful surgical procedure and the secure suturing of small blood
vessels at the kidney wound must be emphasized in order to reduce
the incidence of RAP (9). A
previous study also reported that the use of different hemostatic
materials may aid in reducing the occurrence of RAP (10).
Although a patient with RAP may ultimately require
total nephrectomy (11), selective
embolization of the renal artery branch is currently the most
effective treatment. Its achievement ratio is high (>80%) and
has only a small influence on renal function, therefore, it remains
the gold standard for the treatment of RAP (12).
In conclusion, the incidence rate of RAP following
laparoscopic partial nephrectomy is low, but patients undergoing
this surgery must be aware of this complication, particularly those
with central renal tumors. Late onset of gross hematuria and
lumbago on the affected side are the main symptoms of RAP.
According to the results of the current study, the selective
embolization of the renal artery branch is an effective treatment
for RAP.
Acknowledgements
The present study was supported by grants from the
National Natural Science Foundation of China (no. 81000302) and the
Science and Technology Department of Zhejiang Province (no.
2010R10071).
References
|
1
|
Ramani AP, Desai MM, Steinberg AP, et al:
Complications of laparoscopic partial nephrectomy in 200 cases. J
Urol. 173:42–47. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Winfield HN, Donavan JF, Godet AS and
Clayman RV: Laparoscopic partial nephrectomy: initial case report
for benign disease. J Endourol. 7:521–526. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ghoneim TP, Thornton RH, Solomon SB, Adamy
A, Favaretto RL and Russo P: Selective arterial embolization for
pseudoaneurysms and arteriovenous fistula of renal artery branches
following partial nephrectomy. J Urol. 185:2061–2065. 2011.
View Article : Google Scholar
|
|
4
|
Albani JM and Novick AC: Renal artery
pseudoaneurysm after partial nephrectomy: three case reports and a
literature review. Urology. 62:227–231. 2003. View Article : Google Scholar
|
|
5
|
Singh D and Gill IS: Renal artery
pseudoaneurysm following laparoscopic partial nephrectomy. J Urol.
174:2256–2259. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zorn KC, Starks CL, Gofrit ON, Orvieto MA
and Shalhav AL: Embolization of renal-artery pseudoaneurysm after
laparoscopic partial nephrectomy for angiomyolipoma: case report
and literature review. J Endourol. 21:763–768. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nadu A, Kleinmann N, Laufer M, Dotan Z,
Winkler H and Ramon J: Laparoscopic partial nephrectomy for central
tumors: analysis of perioperative outcomes and complications. J
Urol. 181:42–47. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Uberoi J, Badwan KH and Wang DS:
Renal-artery pseudoaneurysm after laparoscopic partial nephrectomy.
J Endourol. 21:330–333. 2007. View Article : Google Scholar
|
|
9
|
Montag S, Rais-Bahrami S, Seideman CA,
Rastinehad AR, Vira MA, Kavoussi LR and Richstone L: Delayed
haemorrhage after laparoscopic partial nephrectomy: frequency and
angiographic findings. BJU Int. 107:1460–1466. 2011. View Article : Google Scholar
|
|
10
|
Pruthi RS, Chun J and Richman M: The use
of a fibrin tissue sealant during laparoscopic partial nephrectomy.
BJU Int. 93:813–817. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shakhssalim N, Nouralizadeh A and Soltani
MH: Renal artery pseudoaneurysm following a laparoscopic partial
nephrectomy: hemorrhage after a successful embolization. Urol J.
7:12–14. 2010.
|
|
12
|
Inci K, Cil B, Yazici S, et al: Renal
artery pseudoaneurysm: complication of minimally invasive kidney
surgery. J Endourol. 24:149–154. 2010. View Article : Google Scholar : PubMed/NCBI
|