Introduction
Extramedullary hematopoiesis (EMH), occurring as a
compensatory mechanism for bone marrow dysfunction, is almost
always associated with hemoglobinopathies, including thalassemias,
sickle cell disease and hereditary spherocytosis (HS), and
myelofibrosis, as well as other bone marrow disorders (1). The most common sites of involvement
are the spleen, liver and lymph nodes, however, practically any
anatomical site may be involved (2–4).
Intrathoracic EMH (TEMH) is a rare condition that is often located
in the posteroinferior mediastinum and is usually asymptomatic.
Clinically, it is important to distinguish masses caused by EMH
from other lesions involving the posterior mediastinum.
The current study presents the case of a patient
with HS whose primary complaints were abdominal pain and jaundice.
The chest radiograph and thoracic computed tomography (CT) scan
incidentally revealed posterior mediastinum paravertebral masses,
which were diagnosed as EMH by the CT-guided needle aspiration
biopsy. The patient provided written informed consent.
Case report
A 56-year-old male, with no history of serious
diseases, was admitted to the First Affiliated Hospital, School of
Medicine, Zhejiang University (Hangzhou, China) due to upper
abdominal pain during the previous 10 days. The patient was a
long-term drinker and had a family history of HS. A physical
examination revealed mild pale conjunctivae, icteric sclera, mild
right upper abdominal tenderness without rebound tenderness, a
negative Murphy’s sign and marked splenomegaly. The whole blood
count showed a hemoglobin level of 91 g/l, a red blood cell count
of 2.77×1012/l, a mean corpuscular volume of 98.6 fl, a
mean corpuscular hemoglobin level of 32.9 pg, a total leukocyte
count of 4.3×109/l and a platelet count of
169×109/l. Liver function tests revealed marginally
elevated transaminases, with an aspartate aminotransferase level of
44 U/l and an alanine transaminase level of 55 U/l, and increased
bilirubin levels, with a total bilirubin level of 85 μmol/l and a
direct bilirubin level of 50 μmol/l. The hepatitis serology of the
hepatitis B virus surface antigen and tumor markers were negative.
The abdominal ultrasonography and CT scan showed common bile duct
stones, gall stones, cirrhosis and splenomegaly.
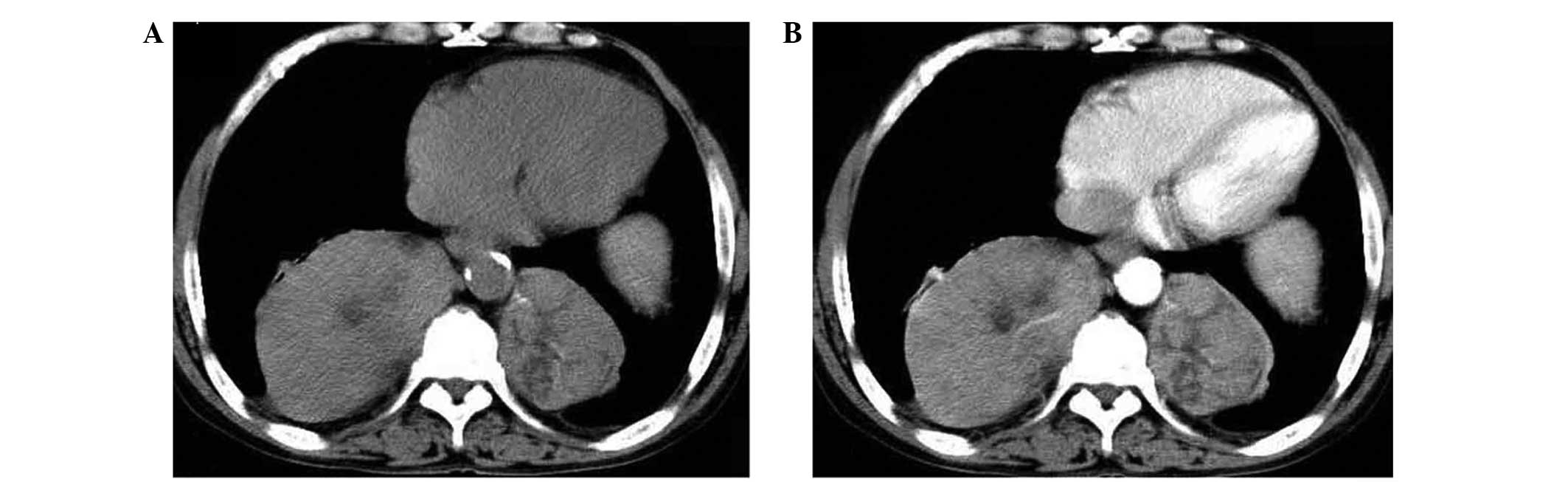
A routine chest radiograph showed bilateral masses
of the mediastinum, and a further thoracic CT scan confirmed
multiple bilateral smoothly-marginated paravertebral massive
tumor-like masses on the posterior mediastinum, with mild
enhancement and without bony erosion of the vertebrae or ribs. The
largest diameter of the masses was ~11 cm (Fig. 1). A peripheral blood smear showed
numerous spherocytes and polychromasia, and the reticulocyte count
accounted for 13.3% of the total erythrocytes. A bone marrow
aspiration and trephine biopsy analysis demonstrated erythroid
hyperplasia only. The osmotic fragility of the red blood cells was
also increased. According to these results, the diagnosis of HS was
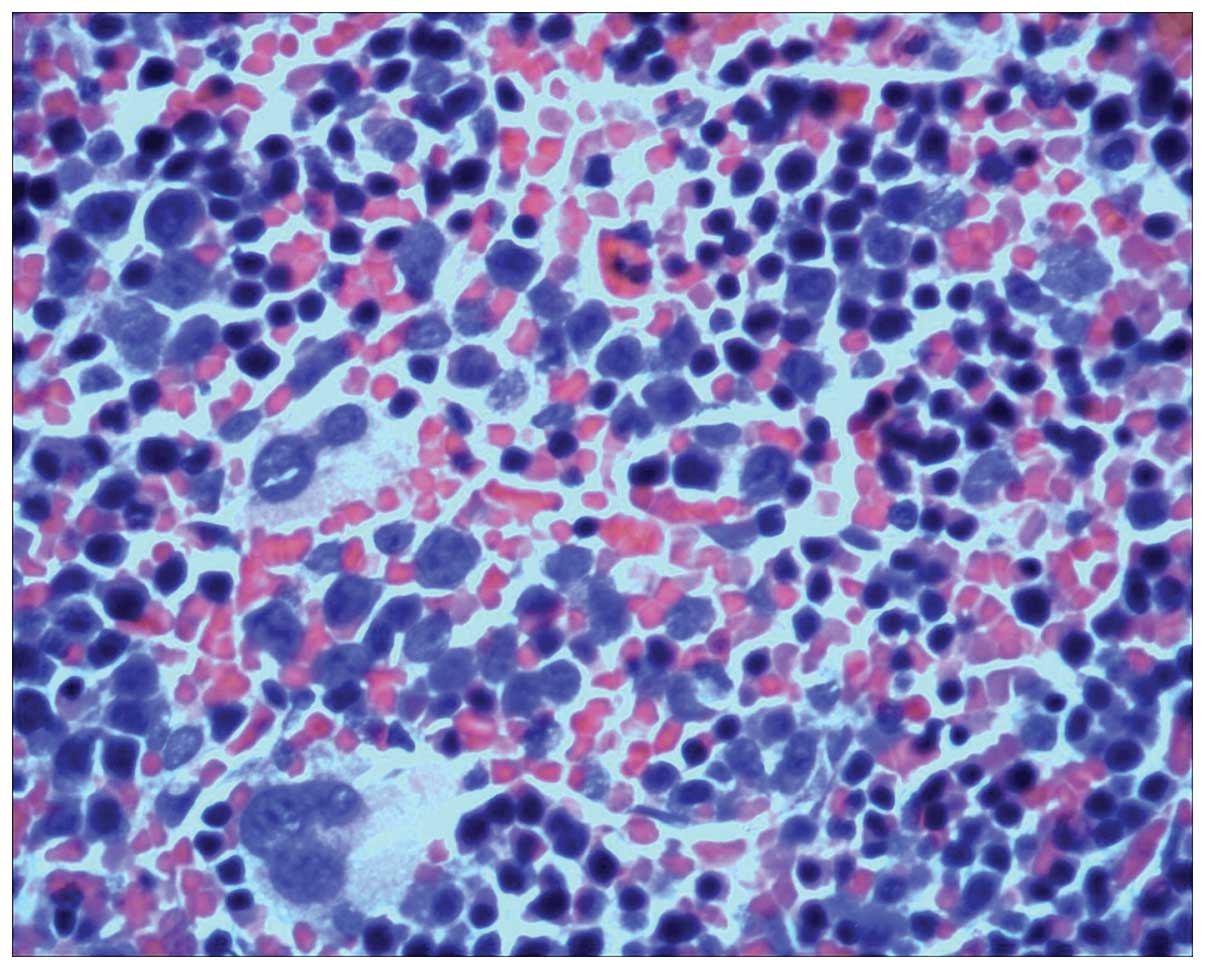
confirmed. For further evaluation, a CT-guided needle aspiration
biopsy of the thoracic masses was performed. The histopathological
examination presented a diagnosis of EMH, revealing hematopoietic
cells with a diffuse distribution, including erythroid, myeloid and
megakaryocytic cells (Fig. 2).
Next, cholecystectomy was performed using a choledoscope via
choledocotomy for exploration. In addition, stone removal, T-tube
drainage and splenectomy were performed. As the TEMH was
asymptomatic, the patient was discharged with the proviso of
regular follow-up examinations being performed.
The patient exhibited improved blood cell counts
following a splenectomy to reduce the hemolysis. The thoracic
masses have been closely followed for one and a half years and
remain stable.
Discussion
EMH occurs rarely and is characterized by
hematopoietic elements that occur outside of the bone marrow. The
disease typically develops as a compensatory response in various
anemias. The liver, spleen and lymph nodes are the usual sites of
EMH, but it may also occur in other sites, including the thymus,
kidneys, retroperitoneum, lungs, breasts, skin, brain, adrenal
glands and paravertebral areas of the thorax (1–5).
TEMH, particularly posterior mediastinal EMH, is a
rare condition that was first described during an autopsy in 1912
(6). The majority of TEMH masses
are usually asymptomatic and can be found by microscopic
examination, however, occasionally they lead to tumor-like masses,
as presented in the current case. Furthermore, TEMH may cause
serious complications, including a massive hemothorax, symptomatic
pleural effusion, chylothorax or spinal cord compression (7–9). As
the manifestation is variable, it is difficult to distinguish EMH
from other mediastinal tumors, mainly when the underlying
hematologic disease is as yet undiagnosed. For posterior
mediastinal masses, such as those identified in the present case,
neurogenic tumors, lymphomas, paravertebral abscesses, extrapleural
cysts, primary and metastatic malignant neoplasms and mediastinal
lymph node hyperplasia must be considered in the differential
diagnosis of TEMH (10).
A number of non-invasive diagnostic procedures have
been recommended to reach a diagnosis of EMH. These include chest
roentgenograms, contrast enhanced CT, magnetic resonance imaging
and technetium-99m sulfur colloid radionuclide bone marrow
scanning. A study by Chute and Fowler (7) reported that the typical radiographic
appearance of TEMH shows unilateral or bilateral, posterior or
lateral, well-circumscribed lobulated paravertebral mass lesions,
which are usually located caudal to the sixth thoracic vertebrae,
without bony erosion and with an absence of calcification. On
magnetic resonance imaging, the appearance of EMH is likely to be
heterogeneous or homogeneous, depending on the presence of adipose
tissue, which is particularly useful in diagnosing intraspinal EMH
(9). A study by Hennessy and
Salanitri (11) indicated that
99mTc-sulfur colloid or human serum albumin millisphere
bone marrow scintigraphy may show increased multiple sites of
ectopic paravertebral tracer uptake in the thorax and abdomen,
corresponding to the sites of EMH. Tissue biopsy or surgical
resection may only be required when the diagnosis of EMH is
suspected or when complications require surgical intervention;
however, these procedures carry a risk of hemorrhagic
complications.
The pathogenesis of TEMH remains unclear, although
one explanation is that TEMH may be derived from the extrusion of
bone marrow stem cells through the cortex into a subperiosteal
location. An additional hypothesis is that TEMH may be derived from
embryonic rests or totipotential cells under the persistent
stimulus of anemia. In the present case, a few of the necks of the
ribs were extremely thin, which may have been responsible for the
development of TEMH.
It is usually unnecessary to treat patients with
TEMH, with the exception of symptomatic patients. Since
extramedullary hematopoietic tissue is highly radiosensitive at
relatively small doses, radiotherapy has been indicated to be an
effective method for controlling symptomatic spinal cord
compression and hemothorax, while surgical treatment is reserved
for immediate symptomatic relief. It has also been reported that
the surgical resection of EMH may cause further deterioration of
anemia and promote hematopoietic behavior in other areas.
Therefore, it is important to determine a correct pre-operative
diagnosis to avoid unnecessary surgical trauma and improve
prognosis.
In conclusion, TEMH must be considered in the
differential diagnosis of patients who have chronic anemia with
asymptomatic intrathoracic masses. Based on characteristic
radiographic observations and chronic hematological conditions, a
diagnosis of EMH should be strongly considered and a biopsy may not
be necessary.
References
|
1
|
Georgiades CS, Neyman EG, Francis IR,
Sneider MB and Fishman EK: Typical and atypical presentations of
extramedullary hemopoiesis. AJR Am J Roentgenol. 179:1239–1243.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lau HY, Lui DC, Ma JK and Wong RW:
Sonographic features of adrenal extramedullary hematopoiesis. J
Ultrasound Med. 30:706–713. 2011.PubMed/NCBI
|
|
3
|
Işık Balcı Y, Kaya V and Ateşçi MS:
Presacral and intrathoracic extramedullary hematopoiesis: a case
report. Clin Imaging. 36:406–408. 2012.PubMed/NCBI
|
|
4
|
Zherebitskiy V, Morales C and Del Bigio
MR: Extramedullary hematopoiesis involving the central nervous
system and surrounding structures. Hum Pathol. 42:1524–1530. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Choi H, David CL, Katz RL and Podoloff DA:
Case 69: extramedullary hematopoiesis. Radiology. 231:52–56. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Andras C, Klassen KP and Holaday WJ:
Tumor-simulating intrathoracic extramedullary hematopoiesis. Ann
Thorac Surg. 10:75–80. 1970. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chute DJ and Fowler DR: Fatal hemothorax
due to rupture of an intrathoracic extramedullary hematopoietic
nodule. Am J Forensic Med Pathol. 25:74–77. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Aessopos A, Tassiopoulos S, Farmakis D,
Moyssakis I, Kati M, Polonifi K and Tsironi M: Extramedullary
hematopoiesis-related pleural effusion: the case of
beta-thalassemia. Ann Thorac Surg. 81:2037–2043. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Das D, Andi AC, van der Walt JD and
Houghton R: MRI appearances of extramedullary haematopoiesis
presenting with cauda equina syndrome in sickle cell disease. Clin
Radiol. 66:1219–1222. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Castelli R1, Graziadei G, Karimi M and
Cappellini MD: Intrathoracic masses due to extramedullary
hematopoiesis. Am J Med Sci. 328:299–303. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hennessy OF and Salanitri JC: Computed
tomography of intrathoracic extramedullary haematopoiesis occurring
as a complication of osteopetrosis. Australas Radiol. 49:430–432.
2005. View Article : Google Scholar : PubMed/NCBI
|