Introduction
The incidence of nasopharyngeal carcinoma (NPC)
varies by region and ethnicity, with the highest incidence in
Southeast China and Southeast Asia (1,2).
Currently, the leading treatment for NPC is radiotherapy. In
addition, a combination of radiotherapy and chemotherapy can
improve the prognosis of patients with advanced NPC. There are
numerous therapeutic strategies for combining radiotherapy with
chemotherapy, and the optimal regimen continues to be explored. In
recent years, epidemiological evidence has shown that the
tuberculosis epidemic situation in China is not optimistic, and
although the incidence has declined, the level remains high
(3,4). In addition, there has been a marked
increase in the prevalence of gout, which highly correlates with
economic development as manifested by dietary and lifestyle changes
(5,6). To the best of our knowledge, there
have been no previous cases reported with regard to patients with
NPC complicated with pulmonary tuberculosis and gout. The current
study presents the case of a patient who was successfully treated
for this condition. Patient provided written informed consent.
Case report
On February 21, 2011, a 59-year-old male was
admitted to the West China Hospital of Sichuan University (Chengdu,
China) with a 5-month history of blood in the nasal mucus. Five
months prior to admission, the patient intermittently experienced a
runny nose with a small amount of dark red blood, which was
occasionally accompanied by dizziness. A physical examination
revealed a rubbery and fixed lymph node on the right side of the
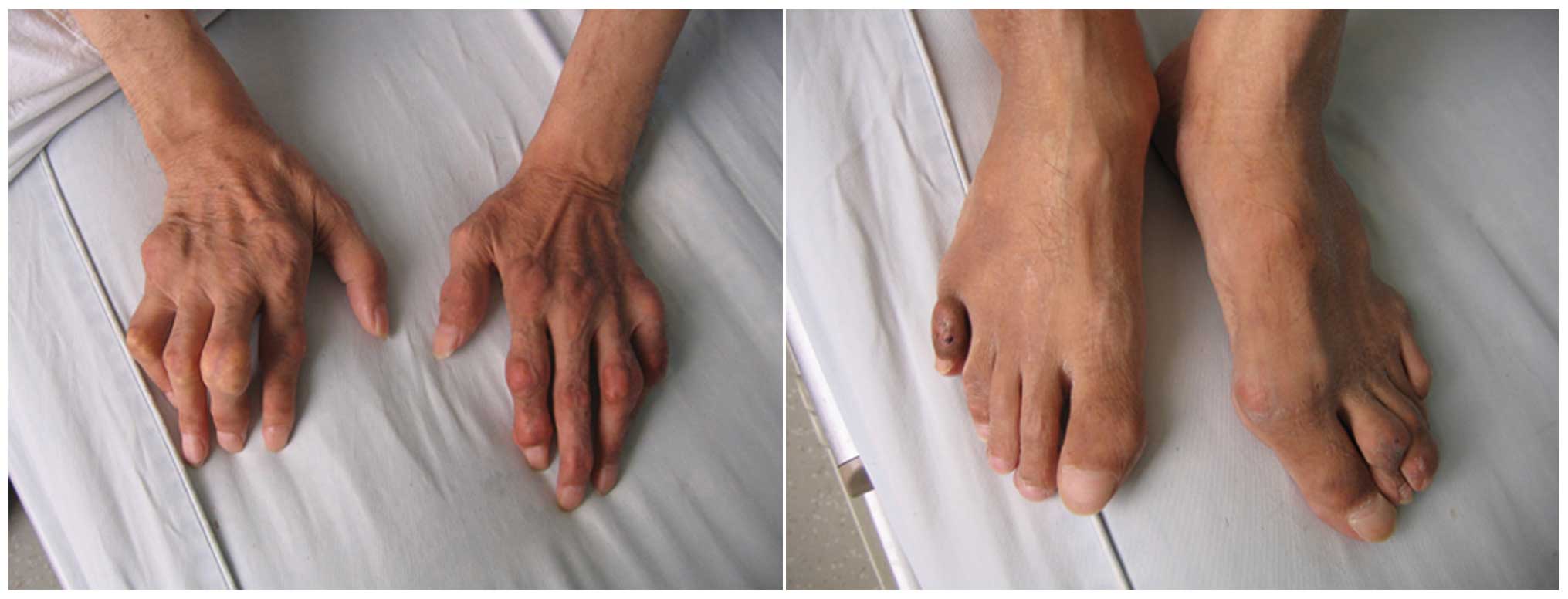
neck, which was 1 cm in diameter. Multiple tophi were found on the
hands and feet (Fig. 1). The
patient had been suffering from gout for 20 years, and had no
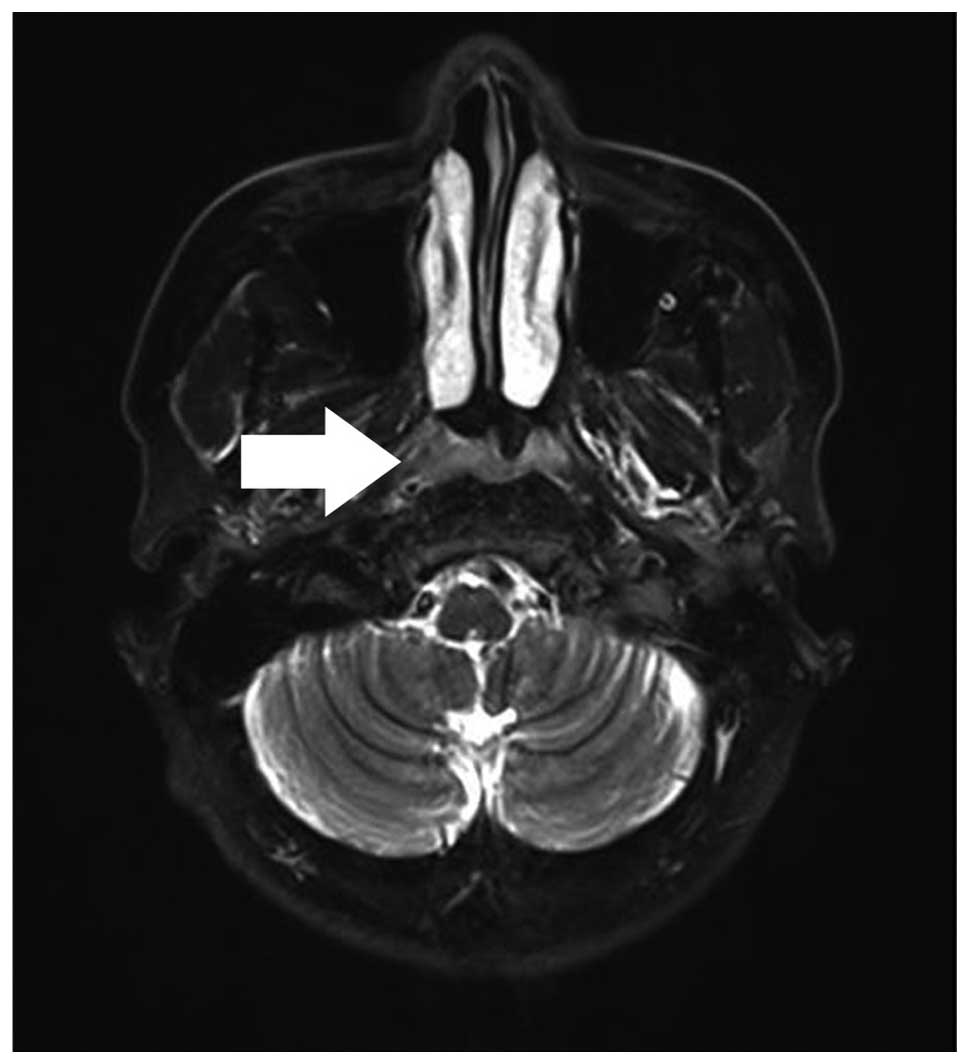
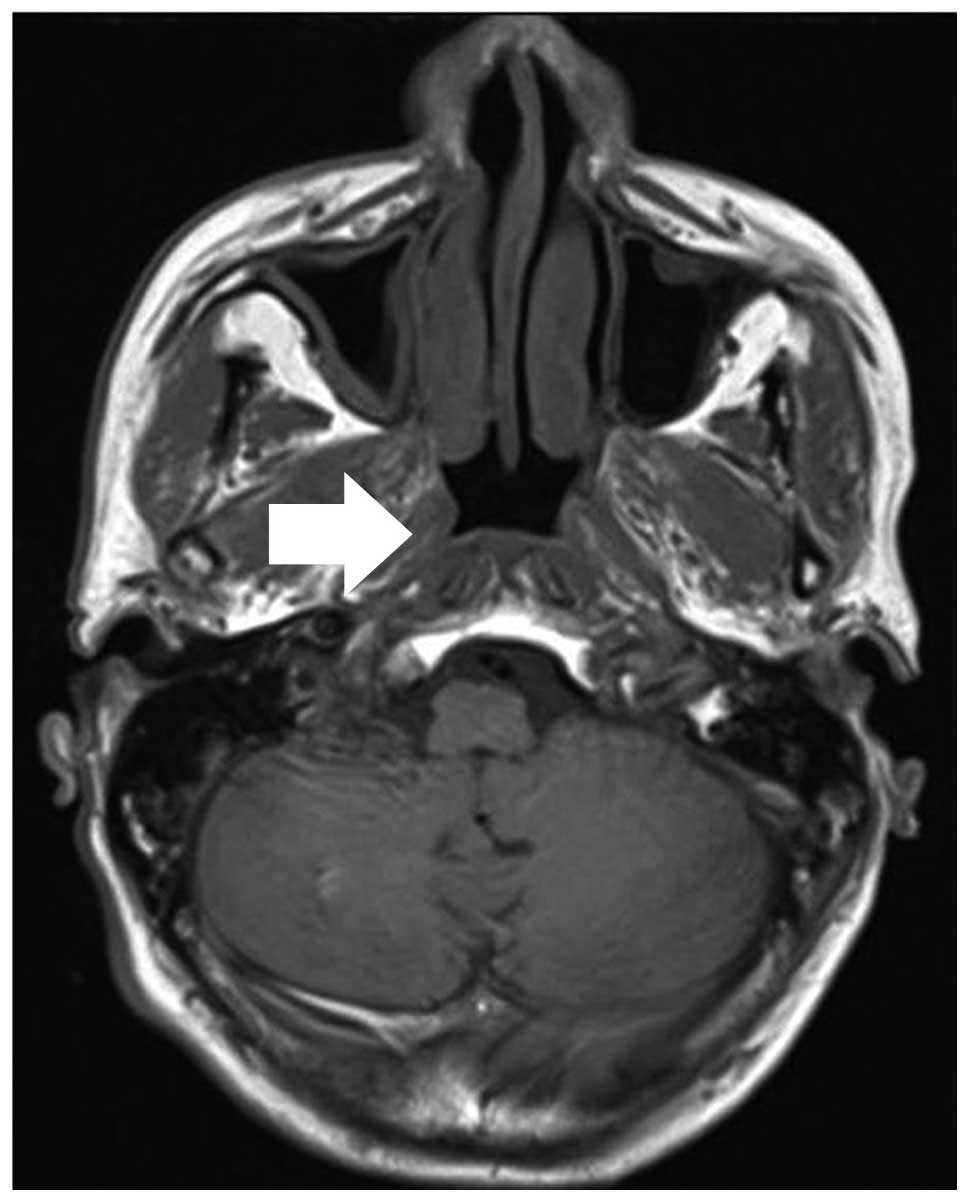
history of tuberculosis. Magnetic resonance imaging (MRI) of the
nasopharynx showed soft-tissue thickening of the top wall of the
nasopharynx (Fig. 2). A
nasopharyngeal fiberoptic laryngoscope examination revealed a
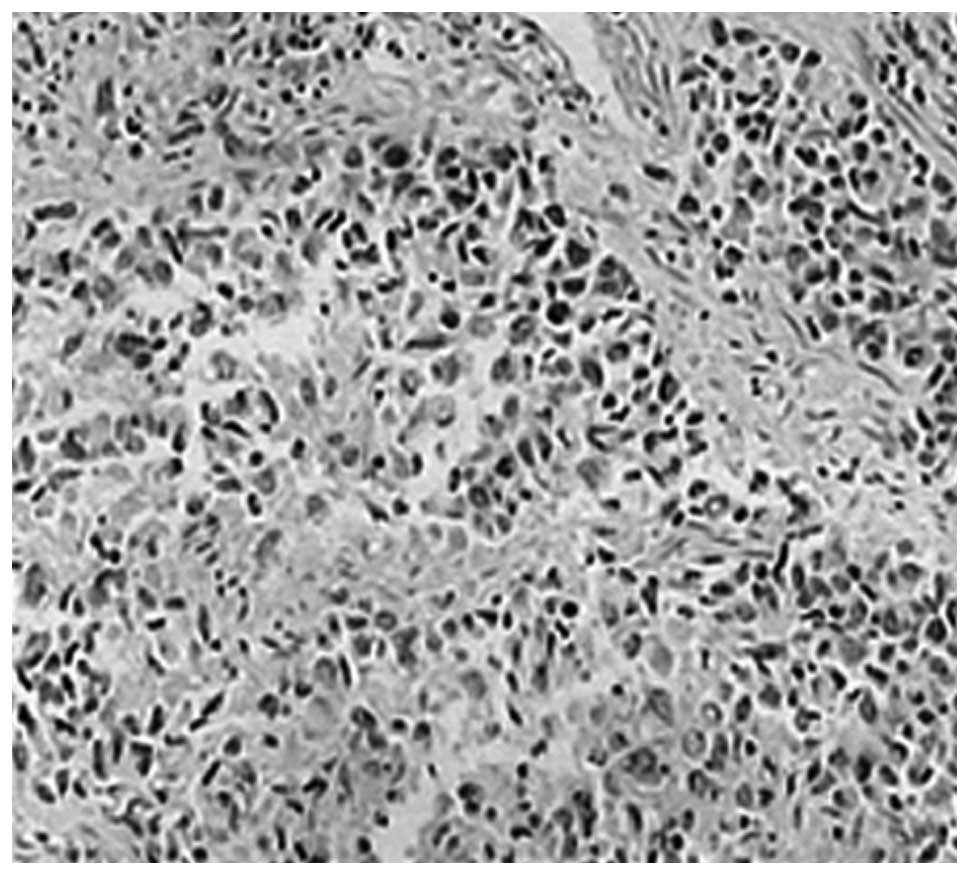
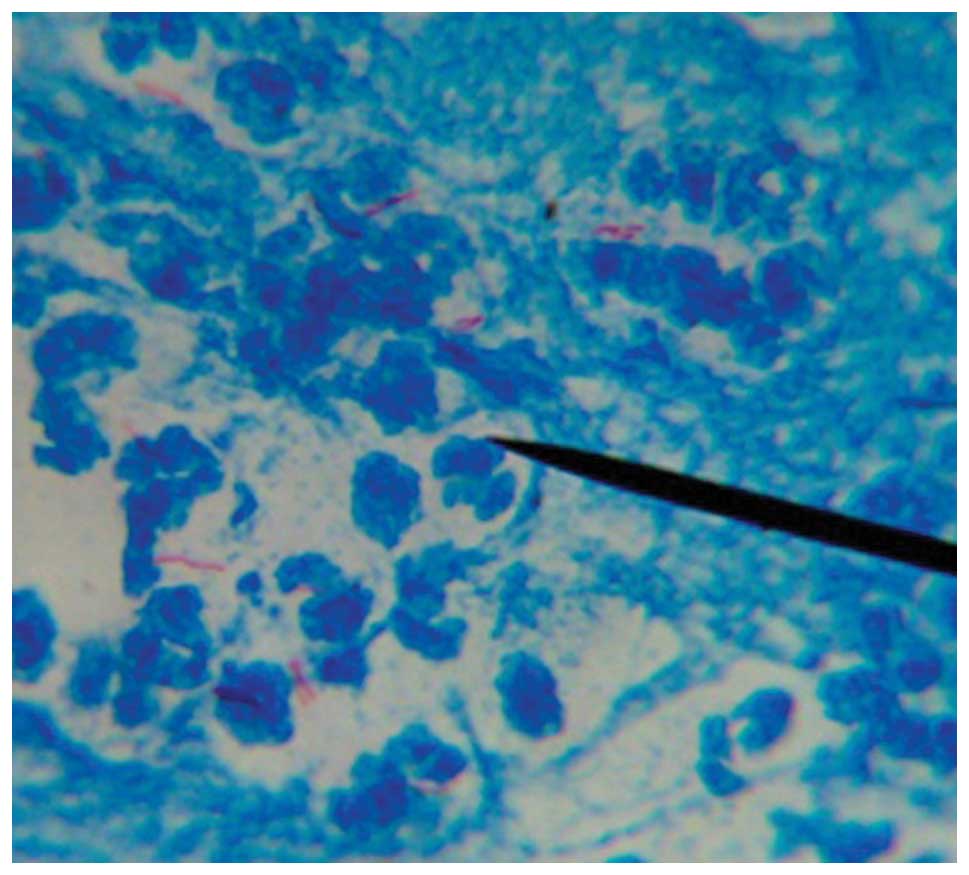
nasopharyngeal neoplasm. Moreover, histopathological examination of
the nasopharynx revealed poorly-differentiated squamous cell
carcinoma (Fig. 3). The
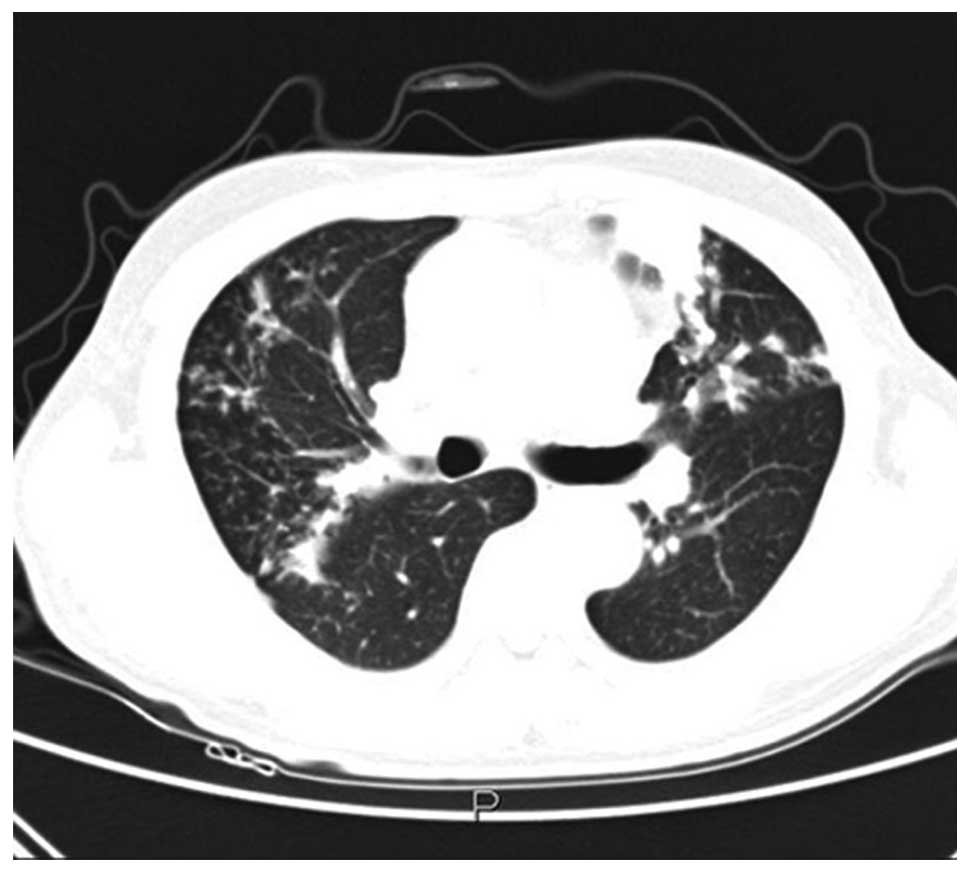
contrast-enhanced computed tomography (CT) chest scan and
thin-slice high-resolution CT findings indicated secondary
tuberculosis, as manifested by increased lung markings, plaques and
nodules of varying sizes (Fig. 4).
The tuberculosis antibody test was positive, and a sputum smear
examination revealed acid-fast bacilli (Fig. 5). Biochemical examination showed
uric acid levels of 610 mmol/l.
Upon admission, the patient was diagnosed with
poorly-differentiated T2N2M0 squamous cell carcinoma of the
nasopharynx, secondary pulmonary tuberculosis (type III), and gout.
Following admission, the patient received anti-tumor,
anti-tuberculosis and anti-gout treatments. The anti-tumor therapy
was chemoradiotherapy combined with concurrent targeted therapy.
The gross tumor volume of the nasopharynx with visible lymph nodes
underwent helical tomotherapy at a dose of 70 Gy in 33 fractions,
the high-risk clinical target volume received helical tomotherapy
at a dose of 60 Gy in 33 fractions and the low-risk clinical target
volume received helical tomotherapy at a dose of 56 Gy in 33
fractions. At the same time, cisplatin and nimotuzumab were
administered intravenously (i.v.) at weekly doses of 40
mg/m2 and 200 mg, respectively. One month after the end
of concurrent chemoradiotherapy, the patient received chemotherapy
combined with concurrent targeted therapy for four cycles: i.v.
infusion of 240 mg liposomal paclitaxel on day 1, i.v. injection of
200 mg oxaliplatin starting on day 1, and every 3 weeks thereafter,
and i.v. infusion of 200 mg nimotuzumab weekly. Anti-tuberculosis
treatment was according to the regimen: Once-daily (q.d.)
administration of 300 mg isoniazid, twice a week administration of
600 mg rifapentine, and q.d. administration of 750 mg ethambutol,
which was continued for 6 months. In addition, the patient
continued to receive 50 mg benzbromarone daily to treat the
gout.
During treatment, the patient maintained normal
total, direct and indirect bilirubin levels. The aspartate
aminotransferase and alanine aminotransferase levels increased, but
returned to normal levels in the late stage of treatment. Although
the leukocyte levels in the patient decreased to a minimum of
1.6×109/l during treatment, they quickly increased with
symptomatic treatment. Platelet levels fluctuated between normal
and ceiling levels, and uric acid levels were mostly maintained at
the upper limit of normal. One month after the end of anti-tumor
therapy (September, 2011), an MRI showed a decrease in the
soft-tissue thickening at the roof of the nasopharynx (compared to
results from the MRI taken in February 2011) (Fig. 6). At 11 months post-anti-tumor
therapy (July, 2012) another MRI was performed, which did not
reveal clear thickening of the nasopharyngeal wall (Fig. 7). Two months after the initiation of
the anti-tuberculosis therapy (April, 2011), a contrast-enhanced CT
chest scan demonstrated a decrease in the number of nodules and
intrapulmonary patches of varying sizes (compared to the results
from February, 2011) (Fig. 8). At
11 months post-anti-tuberculosis therapy (July, 2012), repeat CT
scans revealed scattered streaks, plaques and nodules throughout
the lungs, with no evident changes, which was in contrast to the
results from April 2011 (Fig. 9).
Multiple sputum smear examinations did not show acid-fast bacilli.
Currently, the patient’s Eastern Cooperative Oncology Group
performance status is good. There has been no local recurrence and
distant metastasis of the NPC, and the pulmonary tuberculosis and
gout are under control.
Discussion
Currently, the National Comprehensive Cancer Network
Clinical Practice Guidelines in Oncology recommend concurrent
chemoradiotherapy for the treatment of locally advanced NPC
(7,8,9).
Studies of targeted therapies have been encouraging in recent
years. Radiotherapy combined with cetuximab for locally advanced
squamous cell carcinoma of the head and neck has been shown to
reduce the risk of recurrence and improve survival, without
increasing radiation-related adverse effects (10). Recently, an Exercise and Nutritional
Intervention for Cardiovascular Health study found that the
combined treatment of Erbitux with radiotherapy and chemotherapy
for locoregionally advanced NPC was well tolerated, with a local
control rate of 100%. Moreover, no local recurrence occurred
following a median follow-up time of 330 days, and distant
metastasis occurred in only four patients (11). Basavaraj et al (12) reported the results of a phase II
clinical trial in which 92 patients with advanced head and neck
squamous cell carcinoma received standard therapy with or without
nimotuzumab, a humanized monoclonal antibody that recognizes domain
III of the extracellular region of the epidermal growth factor
receptor. The study showed that chemoradiation combined with
nimotuzumab conferred a survival advantage (12). In addition, a controlled,
double-blind, randomized clinical trial by Rodríguez et al
(13) showed that patients with
advanced squamous cell carcinoma of the head and neck who received
a combination of standard therapy and nimotuzumab experienced a
clinical benefit, manifested by a median survival time of 12.5
months compared with 9.47 months in patients receiving radiotherapy
alone. Moreover, the combined treatment was well tolerated
(13). Furthermore, a multi-center
phase II clinical trial found that nimotuzumab combined with
radiotherapy significantly improved the efficacy of treatment in
patients with advanced nasopharyngeal squamous cell carcinoma, with
only mild adverse drug reactions (14).
The patient in the present case study had
experienced chronic gout for 20 years. Acute uric acid nephropathy
easily occurs under the effect of drugs, and can lead to acute
renal failure. Chemotherapy, anti-tuberculosis and anti-gout drugs
interact in the body, increasing the risk of side-effects. A number
of clinical trials have demonstrated that cisplatin can enhance
radiosensitivity. Platinum-based chemoradiotherapy has a
significant effect in the study of concurrent chemoradiotherapy in
NPC (15,16). In addition, platinum drug toxicity
and radiotherapy toxicity are not superimposed; however, the
optimal dosage of cisplatin to combine with radiation therapy has
not been established. Currently, concurrent chemoradiotherapy in
patients with locally advanced NPC consists of a high dose of
cisplatin (100 mg/m2) and radiotherapy. However, certain
studies have indicated that low and medium doses of cisplatin have
a similar efficacy to high doses of cisplatin, and dividing doses
of cisplatin did not reduce the efficacy, but did decrease the
toxicity (17,18). In the present case study, a
concurrent chemoradiotherapy regimen with 40 mg/m2
cisplatin was used, to avoid induction of renal toxicity as uric
acid levels increased, while at the same time treating the gout.
Oxaliplatin is a third-generation platinum drug that has less toxic
side-effects than cisplatin. A previous study postulated that
oxaliplatin should be used for the treatment of patients with
advanced NPC who are resistant to cisplatin, particularly those
with poor renal function (19). The
patient in the present study was treated with oxaliplatin in order
to avoid increasing the burden on the kidneys. During treatment,
the patient maintained good renal function, and the creatinine and
urea values remained within the normal range.
According to the 2010 global tuberculosis control
report from the World Health Organization (WHO) (20), there are a total of 14 million cases
of tuberculosis worldwide. Although the incidence decreases each
year, the number of cases continues to increase. The treatment of
latent Mycobacterium tuberculosis is the cornerstone of
tuberculosis elimination. However, the hepatotoxicity of
anti-tuberculosis drugs has a great impact on the human body, as it
can cause liver damage, and even result in mortality due to liver
failure and acute hepatic necrosis. Three randomized controlled
trials have shown that the combination of isoniazid and rifapentine
treatment for 3 months was more efficacious than the single use of
isoniazid for 9 months (21). The
combination of isoniazid and rifapentine not only shortened the
treatment time, but also enhanced the treatment efficacy and
decreased the toxicity (22).
Therefore, the patient in the present study received isoniazid,
rifapentine and ethambutol to minimize damage to the liver.
Although the patient experienced third degree bone marrow
suppression, serious complications did not occur during treatment.
At present, the patient’s NPC, pulmonary tuberculosis and gout
remain under control.
In recent years, there has been an increase in the
number of co-existing diseases. When several diseases are being
treated at the same time, clinicians must take into account not
only the efficacy of the treatment, but also the potential
side-effects. Future studies are required on the optimal regimens
for treating patients suffering from co-existing conditions.
Acknowledgements
The authors would like to thank the patients who
participated in this study.
References
|
1
|
Trejaut J, Lee CL, Yen JC, Loo JH and Lin
M: Ancient migration routes of Austronesian-speaking populations in
oceanic Southeast Asia and Melanesia might mimic the spread of
nasopharyngeal carcinoma. Chin J Cancer. 30:96–105. 2011.
|
|
2
|
Wee JT, Ha TC, Loong SL and Qian CN: Is
nasopharyngeal carcinoma really a ‘Cantonese Cancer’? Chin J
Cancer. 29:517–526. 2010.
|
|
3
|
He GX, van denHof S, van der Werf MJ, et
al: Infection control and the burden of tuberculosis infection and
disease in health care workers in china: a cross-sectional study.
BMC Infect Dis. 10:3132010.
|
|
4
|
Sun GM, Gao Q and Peng WX: Progress on
spatial epidemiology of tuberculosis. Zhonghua Liu Xing Bing Xue Za
Zhi. 31:1188–1191. 2010.(In Chinese).
|
|
5
|
Miao Z, Li C, Chen Y, et al: Dietary and
lifestyle changes associated with high prevalence of hyperuricemia
and gout in the Shandong coastal cities of Eastern China. J
Rheumatol. 35:1859–1864. 2008.
|
|
6
|
Li R, Sun J, Ren LM, et al: Epidemiology
of eight common rheumatic diseases in China: a large-scale
cross-sectional survey in Beijing. Rheumatology (Oxford).
51:721–729. 2012.
|
|
7
|
Al-Sarraf M, LeBlanc M, Giri PG, et al:
Chemoradiotherapy versus radiotherapy in patients with advanced
nasopharyngeal cancer: phase III randomized Intergroup study 0099.
J Clin Oncol. 16:1310–1317. 1998.
|
|
8
|
Komatsu M, Tsukuda M, Matsuda H, et al:
Comparison of concurrent chemoradiotherapy versus induction
chemotherapy followed by radiation in patients with nasopharyngeal
carcinoma. Anticancer Res. 32:681–686. 2012.
|
|
9
|
National Comprehensive Cancer Network.
NCCN Clinical Practice Guidelines in Oncology: Head and Neck
Cancers. http://www.nccn.org/93c288ea1c3664690434dfff86acacfe/head-and-neck.pdf.
Accessed April 28, 2014
|
|
10
|
Lee NY, Zhang Q, Pfister DG, et al:
Addition of bevacizumab to standard chemoradiation for
locoregionally advanced nasopharyngeal carcinoma (RTOG 0615): a
phase 2 multi-institutional trial. Lancet Oncol. 13:172–180.
2012.
|
|
11
|
Lu T, Zhao C, Chen C, et al: An open,
muticenter clinical study on cetuximab combined with intensity
modulated radiotherapy (IMRT) plus concurrent chemotherapy in
nasopharyngeal carcinoma (NPC): A 2-year follow-up report. In:
2012; ASCO Annual Meeting; J Clin Oncol. 30(suppl): pp. abstr
55352012
|
|
12
|
Basavaraj C, Sierra P, Shivu J, Melarkode
R, Montero E and Nair P: Nimotuzumab with chemoradiation confers a
survival advantage in treatment-naïve head and neck tumors over
expressing EGFR. Cancer Biol Ther. 10:673–681. 2010.
|
|
13
|
Rodríguez MO, Rivero TC, del Castillo Bahi
R, et al: Nimotuzumab plus radiotherapy for unresectable
squamous-cell carcinoma of the head and neck. Cancer Biol Ther.
9:343–349. 2010.
|
|
14
|
Huang XD, Yi JL, Gao L, et al:
Multi-center phase II clinical trial of humanized anti-epidermal
factor receptor monoclonal antibody h-R3 combined with radiotherapy
for Iocoregionally advanced nasopharyngeal carcinoma. Zhonghua
Zhong Liu Za Zhi. 29:197–201. 2007.
|
|
15
|
Huncharek M and Kupelnick B: Combined
chemoradiation versus radiation therapy alone in locally advanced
nasopharyngeal carcinoma: results of a meta-analysis of 1,528
patients from six randomized trials. Am J Clin Oncol. 25:219–223.
2002.
|
|
16
|
Thephamongkhol K, Zhou J, Browman G, et
al: Chemoradiotherapy versus radiotherapy alone for nasopharyngeal
carcinoma: A meta-analysis of 78 randomized controlled trials
(RCTs) from English and non-English databases. In: 2004; ASCO
Annual Meeting; J Clin Oncol. 22(suppl 14): pp. abstr 55222004
|
|
17
|
Shao-jun C, Hai-xin H and Gui-sheng L:
Different dosage cisplatin based concurrent radiochemotherapy in
the treatment for locally advanced nasopharyngeal carcinoma. Zhong
Guo Zhong Liu. 18:597–599. 2009.(In Chinese).
|
|
18
|
Dong-ning H, Hai-xin H and Shao-jun C:
Different administration regimens of cisplatin combined with
concurrent radiotherapy for 65 cases with locally advanced
nasopharyngeal carcinoma. Zhong Liu Xue Za Zhi. 15:836–838.
2009.(In Chinese).
|
|
19
|
Shi W, Zhou Q and Ju W: Observation on
therapeutic effects of chemotherapy involving oxaliplatin in
treatment of advanced nasopharyngeal carcinoma. Zhong Guo Yao Fang.
16:1886–1888. 2005.(In Chinese).
|
|
20
|
World Health Organization (WHO). global
tuberculosis control report. 2010, http://reliefweb.int/sites/reliefweb.int/files/resour-ces/F530290AD0279399C12577D8003E9D65-Full_Report.pdf.
Accessed April 28, 2014
|
|
21
|
Centers for Disease Control and Prevention
(CDC). Recommendations for use of an isoniazid-rifapentine regimen
with direct observation to treat latent Mycobacterium
tuberculosis infection. MMWR Morb Mortal Wkly Rep.
60:1650–1653. 2011.
|
|
22
|
Sterling TR, Villarino ME, Borisov AS, et
al; TB Trials Consortium PREVENT TB Study Team. Three months of
rifapentine and isoniazid for latent tuberculosis infection. N Engl
J Med. 365:2155–2166. 2011.
|